#763 Bold Beginnings: Community
Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome to episode 763 of the Juicebox Podcast. This episode is another in the bold beginnings series
hopefully, you've been listening to the bold beginning series, and you're all caught up and ready to take on the latest episode, community. If you haven't heard the others, you should check them out. You can find them in your podcast player by typing in Juicebox Podcast bold beginnings. Or you can find them at juicebox podcast.com. They're in your podcast player you understand. But if you're looking for a list, I'm saying juicebox podcast.com. And you'll also be able to find a list in the private Facebook group for the podcast Juicebox Podcast type one diabetes. If you'd like to hire Jenny Smith, you can do that she works at integrated diabetes.com Head over there and you'll be able to figure it out. While you're listening today, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your healthcare plan. Or becoming bold with insulin. No ads in this one, just gonna have a little announcement here after the music and then straight through me and Jenny chiton in chat
I'm just here to ask you for your support. And there's not much you need to do to give it follow the podcast or subscribe to the podcast in an audio app, like Amazon music, Apple podcasts, Spotify, something like that. That's one thing you can do. You could tell someone else about the podcast, that's a big deal, actually. Like you're talking to a friend like I got diabetes like you, you should try Juicebox Podcast. Or maybe you tell your doctor about it. Your doctors like to be your doctor in this scenario. Oh my god, how did you get your agency this good? You say I'll be you know, I listen to the Juicebox Podcast, you should check it out Juicebox Podcast and you start telling them that like in your you plot your app, show them on your phone, or tell him about juicebox podcast.com. You know, I'm saying sure the show is pretty much it actually. So I want to say to you, there's no ads today. So enjoy the podcast. The only ad is for for the show, support it, download it, subscribe to it, tell a friend about it followed on Instagram, check out the private Facebook group. That's pretty much it. I appreciate your time. Enjoy the episode. So Jenny, we are doing well with our bull beginning series, a few more episodes left to record. I am beginning as I told you earlier, but more and more getting nice feedback from people newly diagnosed people who have found it and are joining it finding it to be helpful. Yay. It's it's really been a fulfilling thing. Which you know, if you all know me, like I don't say things like I feel. But I really do. And so interestingly enough, I got a note yesterday from a guy, a young man's probably 20 to 23 years old just graduated from college. And it it's going to fit in nicely with the the topic we're doing today. So today's topic is community. And I'm not the type of person who prior to diabetes would have said to you, you know how you handle problems in your life, you surround yourself with people who understand, like I did not grow up in it that would have seemed granola and crunchy to me prior to all this, if that makes sense. Now I am a firm believer in it. I am a firm believer in the idea that people who understand your situation are in a unique situation themselves, and they're able to offer you support. Even if it's not directly that you can't get anywhere else. I've never right, the experience of seeing a person feel supported with just the knowledge that someone else understands. And they don't even know each other is fascinating. I never thought I would see that. But there are the vast majority of people who listen to this podcast or go on my Facebook group or in another community never say a word. They don't type a message. They don't send me a note to tell me they enjoy the podcast. They're just there. Right? Yeah. And there's something really magical about it.
Jennifer Smith, CDE 5:00
There is it's a feeling of, as you said, I mean, a lot of people I think, are for one example Facebook, they're lurkers, right? They sort of just are there. And what they get out of it is either information or against a sense of like belonging to a group that gets it as well in whatever realm of, you know, chronic condition or lifestyle or whatever you might have. I mean, there are lots and lots of Facebook groups for things. Sure. But diabetes, being such a it's, it's something always that there. And I think you can find posts all the time, something new, this is happening, I had this occur, and there's always somebody who's going to chime in and say, I've had that happen, too. I kind of feel it, I get it.
Scott Benner 5:53
Well, the people who listen to the podcast teach me what the podcast is, which is a weird thing, because I'm the one that makes it, but they're the one who tells me, they're the ones who tell me what it is to them, which is okay. It's an interesting, it's an odd dichotomy, right? Because I think I'm doing one thing, like, if you would have asked me five years ago, and even maybe three years ago, I would have told you the podcast is about managing insulin. That's it. That's how I saw it. And then I, I one day had this, this young girl on in her mid 20s. And she's like, you know, I started listening to the podcast, and my A onesies came down. And I thought, probably a little like, smugly. I was like, oh, yeah, cuz you heard how I talked about insulin fixture wholesaling, right? She does now, I always knew that stuff. She said, I just never did it. Yeah. And I was like, Well, what made you do it? And she goes, I don't know. She's like, Just hearing that other people were doing it. And that, I just thought, well, I probably could, too, you know, and then she just, she just did it. So I knew I didn't know that, like her conversation. And other conversations and notes taught me that it's, it's almost strange, because I don't have it in my life the same way that other people do, because I'm the one making it. So like, I can't, I can't be involved in it the same way. I don't know how that it's a strange position to be in, like my facebook group has at this point. By the time this comes out, there'll be 28,000 people in there. And I see the background metrics between 70 and 110 new posts a day. 24 of the 28,000 people are active in it, which is crazy, because Facebook groups are always like, well, we have 100,000 followers, when you look there's two posts every week, you know, like, right, they that
Jennifer Smith, CDE 7:46
by the same people all the time. Yes.
Scott Benner 7:49
each other, we think they're talking 200,000 people. But what's really amazing about that is, is that people will ask a question, and then you get a wide variety of answers by rack but not screwball answers. There's something about people who listen to the podcast, and then go online and participate they have they have enough information, where they're not saying things that you're like, wow, that's doesn't make any sense it all
Jennifer Smith, CDE 8:18
right. It's not like crackerjack information. And if Yeah, if they're
Scott Benner 8:23
a little off, there's such a great vibe in there, that other people will come in and be like, Hey, I see what you said. But have you considered this and it's all taken well, and I'm, I'm stunned every time I see it, because Facebook is, you know, colloquially it's a place where people argue, but yes, does not happen in this space. Really, really?
Jennifer Smith, CDE 8:43
Yeah, I have not I mean, with you know, all the lurking that I myself do. I don't I don't off in fact, I don't think I've ever seen in your group negativity in a way that's, you know, cutting to other people who've made comments or have offered up this is what's happening, you know, whatever. And I've seen that in other groups. Yeah, of course is unfortunate.
Scott Benner 9:09
So the way I do it is probably it's probably opposite of how people think about it, but I don't over moderate the thing. Right there adults get any mean like if they can't figure it out? How am I going to figure it out? Little things you know, there's obviously there's the rules in the Facebook group are kind of funny, if you go read them. I think it's, you know, like the basically it's the it's the equivalent of like, don't be a dick bait, you know, basically, you know, don't don't talk about politics, you know, that kind of stuff, like just just talk about diabetes with people and and it works and it doesn't just, I at one point thought it was going to be like, in addition to the podcast, and then I started realizing that the Facebook group had such a good it had such good word of mouth online, that people were ending up in the Facebook group, have no idea what the podcast is, like, forget that they haven't heard it. They don't know what it is. They just they were told, like, click on this link, and these people will help you with your diabetes. And you see them come in and ask, they'll ask a question. And other person will say, oh, you should try episode, this podcast. And they'll say what podcast, right? And that's amazing, because now there's these, there's these two entities, and they somehow support each other, but can operate
Jennifer Smith, CDE 10:33
separately independently. Really, really interesting.
Scott Benner 10:37
So some feedback from people, if you know, other type ones, reach out to them, if you don't know them, find a community and build a support system. As an adult diagnosed with type one diabetes, I didn't know anything about diabetes, and I had a lot of misconceptions, I felt very alone, finding support groups like Facebook helped READING A reading helped a lot getting Dexcom helped. I found out about them through Facebook groups, I would have loved to have been assigned and experienced type one to talk things through. So this person is a great idea. Yes, right. Yeah,
Jennifer Smith, CDE 11:13
that's I mean, it's there. I know that there are diabetes, like mentors, especially like I think JDRF used to have, they don't still have it, they used to have like a mentoring kind of program. I know that the college diabetes network has some nice mentors, especially within the college chapters, you know, but that is from a boil down, like, Hey, here's your diagnosis, you know, et cetera. But here's somebody to connect with. This is somebody in your area, this is somebody that, you know, would be really good in terms of age level or lifestyle or whatnot. Because, you know, I, I can imagine the, and I have to imagine, because I don't really remember feeling alone when I was diagnosed, but it was a very different time than we have today with technology. So I think in today's world, there's so much connection on so many levels, whether it's texting, or you know, a Facebook or a some type of online group or whatnot. I think it would be a nice idea, actually be like, Hey, here's somebody connect with them, and they can help you like, feel okay,
Scott Benner 12:31
have conversations. Yeah, I think that's one of the places where the podcast fills a void, because I hear from people a lot. I don't know, another person with diabetes. And I come on here, and the few times a week you put these conversations up with people, and I get to meet an airplane pilot who has type one and a firefighter as type one, or just some person, you know, and where someone comes on and says, Oh, you know, I have Hashimotos, too. And I'm, and they think I have Hashimotos. And then you know, it's just it's, it's an opportunity that just doesn't exist in the real world, unless you're gonna go to a diabetes camp. Right? You know, which they have for adults, and they have for for kids. But that's another thing you have to it's a week or two weeks, and they're not all over the country. And, and camps are an interesting, I like watching people talk about camps, because they're an interesting conversation. People fall on one of two sides of camps. They're either like, Camp is the greatest thing. You know, adults will be like, I still my best friends I met in camp when I was 16. And then there are people like, Arden, who I we wants to do you want to go to diabetes camp, and she was like, oh, no, do not make me do that place. And you know, and she didn't want to go to camp forget that it was about diabetes. Right? Right. You know, I have to skip through these. A lot of these people statements, they're lovely. And I want to thank everybody for them. But a number of them are just like, hey, that's the podcast, I found the podcasts and I don't want to just read all those. This person said, I wish they would have given us more access to a community, but like not not deliver it to us. Just tell us that existed. Like tell me there are groups online that there are podcasts. I had so much fear and anxiety, self doubt and blame no matter how much they say otherwise. But this community of moms and dads and adults with type ones was amazing for me. I think. I think that it's a message for doctors really, you know, it is
Jennifer Smith, CDE 14:27
and I think it shows it shows a degree of sort of a lack of information on the clinicians side. Not because they don't want it but because there's not one that's just a an approved Hey, these are the really quality places that you can go for more information. Here's your rip off card along with your rip off card about how to carb count. Here is your like resources from a community based law Have all and they're they're good places they're not, you know, Johnny's corner shop of information.
Scott Benner 15:07
Here's my I mean, I think my focus is pretty clear. But to put it in this episode, I think good, easy to understand information early is important. Yes, there is an entire segment of people who believe the absolute opposite, keep you not understanding give you small bits of information very slowly. They say don't overwhelm people, we had a real I'm not a very dramatic person. And online, I'm very proud of kind of the pragmatic way that I've run a Facebook group. But there was another Facebook group, that if you mentioned the podcast in the group, your posts would just be deleted. And people would come back to me and say, Do you have any idea what happened here? As if I would know I'm like, I don't know. I don't know these people. But I said, you know, they asked what helps you with diabetes? And I said, Oh, I began to listen to the defining diabetes series of the Juicebox Podcast, and I moved on to the Pro Tip series. Now my son has this a one C. And that's what helped me. And then they deleted it. And I said, Well, it's two things. First of all, people fervently love the podcast. And when they talk about it, they mostly speak very well about it. Except for a person who left a review the other day, Jenny about our bold beginnings thing that said they would be better if I didn't talk as much. And
Jennifer Smith, CDE 16:34
maybe they just like my voice better than yours and hurt
Scott Benner 16:37
my feelings, sir. Sorry. But But, but so I said, so I think there's a little bit of that when people share the podcast over and over and over again, it could probably seem like I put you up to it. And also, it's a weird thing, Jenny, but these Facebook groups become territorial. If sure if you have Face Book Group, a Jenny Facebook group, and you say what helped you, and they say, Scott's Facebook group, well, then you go to Scotts Facebook group and never come back to Jenny's Facebook group. And, and that bothers people, they lose their numbers. And,
Jennifer Smith, CDE 17:14
and I think the unfortunate thing there is that as a, let's call it, whatever you are a moderator of your group or whatnot, you're then limiting, you're limiting the quality that you're seeing that you're trying to put out there. Right, you know, you're limiting access to what might work for one person. Great. I'm happy to have somebody go elsewhere. If I'm not the right provider, or the right caregiver or whatever, for you. Go ahead, I would rather that you get good information and good care. And if you're getting it in a different way from a different place. Awesome. glad about
Scott Benner 17:54
that. I agree. But that's exactly how I run it. Like if when that happens in my space, and somebody's like, what happened, you know, what helped you and they're like, this XYZ Facebook group, I think, okay, good. Like, I think it's a strange thing. From a content. On some level, Jenny, I'm a content creator, right. And I need people to continue to listen to my content and share it or the, it'll just stop, like, it'll just end. It's hard not to be overwhelmed by that feeling. It's difficult to keep up the whatever's best for people's best for people. But I believe that, and that's what I do. Like, I also think that the time you spend online in the community, once you find it and realize that it's very valuable, you will spend a fair amount of time there. But it's usually six months, on the outset, maybe a year, and then people fade away. And that's beautiful. They learn what they need to know. And they go back to their lives, right. It's, it's what you would if you care about people, this is what you would want for them, you know, it's what
Jennifer Smith, CDE 19:00
and or when there's new information, people who feel like they've learned enough, may end up coming back now that there's something new available, something new that there might be information that's again, discussed in a different way, or a completely different technology or something. You know, they'll eventually come back. Yeah, honestly.
Scott Benner 19:21
So I hear from people too, that that happens to them, they cycle, but then they'll watch their a one C start to drift up. And they say, I just went back to listen to the podcast, and it wasn't management stuff anymore, because I knew the management stuff. It was It keeps them engaged, I think, yeah.
Jennifer Smith, CDE 19:38
It's motivating. And I think because there's enough, there's enough posting. I see which is really nice. of both. Like, let's call it the wonderful day, right? The no hitters where you're like, Oh, I'm clearly cured today. All right. All right. And then Next day or whatever, there are also posts of, I don't know what's going on, or, you know, this is what's happening. And people chime in, and they're like, ah, you know, we've had that before too, and whatever. So it's a sense of, when you're trying to get back to your management, sometimes it's a sense of seeing those motivators from other people, like other people have really bad days to or really bad times, or have had something occur in their life that got them off track. This is a way to get back on track to get those, those motivators even if you're just reading and you're not posting anything. It just helps us to stay connected and remind yourself I know, I know all the tools, I just, I just have to put them back in the right places in my life. And it's
Scott Benner 20:44
on you a little bit to be in the right mindset, too. Because if you see someone's success, and you're in the right mindset, their success looks hopeful. Yeah. And if you're in the wrong mindset, their success is like, it makes you think I can bleep this out. It makes you think, Oh. Why don't you Bolus for your blood sugar to over 120 You mother. But you have to be able to you mean you have to be able to let that go. And to step back and say, this is possible. Like I think this podcast as it grows, in my mind, it's mostly about what's possible. At this point, right? It's possible to do this, if that person can do it, then I can do it. They might know something that I don't know right now. But, and I, I'm stopping myself from reading over and over again. By far, this has been the best community Juicebox Podcast on Facebook, starting your podcast, especially defining diabetes in the QuickStart Series. I wish they would have given me your Pro Tip series on day one. Like there are countless comments here about this. And I want to tell you this story. Well, let me finish the other side of this. So we say when people are doing well, you can kind of respond to it a couple of ways. And when people are doing poorly. It also is helpful. I know that sounds crazy. But it's the same idea. You look and you think well, they're having a bad day. I've had bad days. Right? So this is normal to you know, it's not going well. And it takes away a lot of the angst from the whole Right. Right. It really does. Yeah. So so this thing at the beginning that I mentioned, I had a message yesterday from this is a long message. I'm not going to read it to you. But I'll give you the I'll give you the breakdown. diagnosed in high school, I think a senior on his way to college, finds the podcast listens to a couple of episodes, doesn't keep listening, goes away to college, drinking weed smoking, spiraling not paying attention to diabetes whatsoever. Blood sugar because it's college, three hundreds blood sugar's higher, a one C going up crazy. doesn't just doesn't even worry about it. I think COVID hits kind of refocuses the person a little bit person goes to a doctor to their Endo, and says, Hey, I found this podcast and I'm gonna try some stuff. And you can already see my agency starting to come down, I'm seeing some stuff, it's positive, and he starts telling them he's going to try it, doctor, whatever, do whatever you want, because doctors not helping. And then the person has a big success moves the agency really far life is changing, goes back to the doctor tells them I want to tell you about the podcast tells them all about the podcast, the doctor gives them the one of two responses that people tell me about either the doctors are like, This is amazing. It's great. Whenever it's more, whatever you're doing. Yeah, going, or you're just going to spend your whole life staring at your diabetes. And I guarantee you that that guy on that podcast doesn't do anything except watch blood sugars and blood and really amazing. Think about that. Right? The person takes their a one C from double digits into the sevens and the advice the doctor gave them was stop doing that. Just essentially Fascinating, right? So the the kid essentially telling this person,
Jennifer Smith, CDE 24:15
that they're putting too much time and effort into their own health management. Yeah, that's really the cut and dry of what this physician was saying what's
Scott Benner 24:24
in rest of that sentence that doesn't get spoken. So go ahead and have major problems later in your life or sooner maybe, you know, right? Yeah, but hey, at least you'll be drunk as a sophomore. Like what the hell are you saying to the kid right? Because the kid has making a change and is excited about it and then the doctor steps on it fast as fast that happens a lot. You have no idea how many notes I get from people. I went to the doctor, I was super excited. I knew my A once he was going to be lower. I knew my lows were going to be less. And all the doctor told me was to put my one C higher. Right Right. And and this three months of hard work, and you're looking for the pat on the butt at the end. And instead you get, don't do that. And it's hard for people to push through sometimes.
Jennifer Smith, CDE 25:12
Absolutely. I mean, you're not surprising to me, you get people all the time who are frustrated with the fact that not only are they usually being told that the highest can be expected, like high higher than you would want highs, right? And that if your insulin is working, you know, you're, you're to expect this and that's and or just the comment of, well, that's just diabetes i in today's day and age, that is still a common that's being you know, or a message that's being given to people. And that's really, really sad,
Scott Benner 25:49
really sad, especially in a world where I can pick my phone up right now and see that Arden's blood sugar has been somewhere between 80 and 110 for the last 15 hours, right? How can you tell somebody that's just diabetes? Why don't you tell them? Hey, here's this stuff that exists or try that or good job? How about how about good job? How about how about good job? person moved there a one see multiple points and found stability? How about good job, that'd be great. By the way, there's another part of that story I can't tell on here. But I'll tell you afterwards. It's about the doctor. And it's fascinating. I apologize that I can't say it here. When I was diagnosed in 2020, you and Jenny, we're all I had this. This group has been my support and my family. I was kicked out of the ER in DKA with insulin to Use as directed, but had to wait five and a half months for my first endo appointment. Every episode I listened to save my life and my Saturday. Oh, and I'm wonderful.
Jennifer Smith, CDE 26:48
That's wonderful. And it's also an I've said it before, but that's, that's why I love I just love being able to contribute, you know, to what you've put together because well, it makes it makes me just smile. That's super awesome.
Scott Benner 27:01
I am happy when you're happy for certain Yeah, this isn't a
Jennifer Smith, CDE 27:04
show you my I know people can't see this. But this was my day yesterday.
Scott Benner 27:07
Wow. Jenny's Jenny's showing me a graph. That's 24 hours. Oh, yeah, it's 24 hours. Yeah, some of you might look at and be like
Jennifer Smith, CDE 27:22
some of my data to kind of, I have an endo appointment coming up. And I like to take photos and whatnot of like, really busy days, like it included a run and included swimming in the afternoon with my boys and included, like all these things. And you know, not every day is 100% like that. But they're they're pretty days where you're like,
Scott Benner 27:41
I know, I did it. That's exactly right. And you should, by the way, celebrate that stuff. You really should. And it, it just it's very important. So anyway, I put all that I put this in this series, because A, I didn't realize how important it was when I started. And I've learned and B I think it's hard for people to accept, especially in the beginning, like you didn't want to have diabetes. And now what now you're gonna surround yourself with more people with diabetes, right? You're probably like, I wasn't looking to be in this club. Thanks. But it's, it's just like, give into it. I don't care. I don't care if you're one of those people who learns and stays on the Facebook page for years helping other people. Or if you get what you need, and you leave, or if you never say a word and you just read it, it doesn't matter. There's something really valuable about it. And it's it's not completely possible to quantify. But I am 100% Short works. And there's this long, there's this long lesson here that I won't read the entire thing. But this person said they found the podcast, and it felt overwhelming. And I understand that. And that's why something like bold beginnings exists, and why defining diabetes exists and all these other series that are inside of the podcast. So I did something Jenny, the other day that I want to put right in here. Yeah, I used so there's juicebox podcast.com, which is just it's a website where you can go and see most recent episodes, and a few of the series like pro tips and stuff are broken out on the front page. Because there are now 741 episodes of the podcast as of this recording. And podcast apps while they're amazing. They're not. It's not the Dewey Decimal System. It's it's not super easy to find stuff, you have to know what you're searching for if you're going to search. So I've had for a long time, another URL diabetes pro tip.com. And it just used to be an online player of the Pro Tip series and the defining diabetes series. But the other night, let me get it up here so I can make sure I'm saying this correctly. diabetes pro tip.com I revamp our tips Tip Because to Hakan No, really leave off, leave off the list. As for savings Jenny, I at first I thought, oh, diabetes pro tips.com. And then it was taken. So I use diabetes pro tip.com. When you get there, you scroll a little bit, and there is a player, the player has the first one, you'll see defining diabetes 44 episodes of that. And you can scroll right through really do that many doors, there'll be more so like, you just scroll through, and there's a player right there, you can play them in order, you can play them one at a time, or you can see the episode names and numbers and go back into your podcast player and find them there if that's, you know, easier for you. But you scroll a little farther, the bowl beginning series is there, which as of this recording has 11 episodes, we'll have more by the time you get there. 22 episodes of the diabetes variable series 25 episodes of The Pro Tip series after dark is now up to 27 episodes. And the cool thing about this is that as I add new episodes, they automatically populate in these players. So it's great, I don't have to go back in and add them like I put up a protip or excuse me, I put up an after dark episode today. And it's already available there. And then there are the wellness series, which was mostly with Erica Forsythe, and Eric and I are planning on doing a lot more in the coming months and years are asking, you know, when we do ask Scott and Jenny episodes, yeah, that's how many you know how many there are? No,
Jennifer Smith, CDE 31:36
I don't know.
Scott Benner 31:38
18 As of this recording, so really, we'll send in questions and we record episodes answering their questions, there's 18 of them. Algorithm pumping series is up to 17 episodes, defining thyroid series we did is there. I'm about to add some pregnancy episodes. So basically any collection of management type stuff. If you can't find it in your podcast player will always be at diabetes protip.com. And you can get to it through juicebox podcast.com as well. Good organization.
Jennifer Smith, CDE 32:11
That's I like that. Yes, I know. That's the kind of person I like organization.
Scott Benner 32:17
I think we all know that. That's not my wheelhouse. And it's pretty crazy that I even did that. But it just seems it seems important. I mean, listen, from a podcaster standpoint, I just want you listening in a podcasting app. It's the best thing for the show. But at some point, I realized, like this podcast has become it's a compendium of information. And it should be accessible, you know, in multitudes of ways. So that's one of them. I hope it helps everybody. Oh, good job.
Jennifer Smith, CDE 32:45
Awesome. Very nice. Thank
Scott Benner 32:46
you. Once again, if you need help with your diabetes, Jenny works at integrated diabetes.com. And in my opinion, there's no one better go check her out. I'd like to thank you for listening remind you that there is an entire bold beginning series that I hope you check out. The podcast has experienced insane growth in 2022. And that is directly because of all of you. So we're just going to take this opportunity right here before the music stops to say thank you, when you support the show, you're supporting me and the work we're doing. And you're helping other people with type one diabetes to be able to find this material. So thank you very much. Hope you enjoyed this episode of The Juicebox Podcast. I'll be back very soon, with much much more
Test your knowledge of episode 763
1. How should blood sugar levels be monitored in relation to exercise?
2. How should low blood sugar episodes during exercise be handled?
3. What is the impact of stress on blood sugar levels?
4. How should insulin doses be adjusted based on physical activity?
5. Which types of exercises are beneficial for diabetes management?
6. What is the role of consistent physical activity in long-term diabetes management?
7. How should one prepare for exercise to avoid blood sugar fluctuations?
8. What are the benefits of incorporating different types of physical activities, such as aerobic and anaerobic exercises?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#759 Bold Beginnings: Guilt, Fears, Hope and Expectations
Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
Test your knowledge of episode 759
1. Why is recognizing the symptoms of type 1 diabetes early important?
2. What is the role of insulin therapy in managing diabetes?
3. Why is carbohydrate counting important in diabetes management?
4. How should high blood sugar episodes be handled?
5. What psychological aspects of living with diabetes should be managed?
6. Why is regular physical activity beneficial for diabetes management?
7. Why is it important to have a personalized diabetes management plan?
8. How can staying informed about new research and developments in diabetes care help?
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 759 of the Juicebox Podcast.
Jenny Smith is back. And today we are doing another indie bold beginning series. Today's topic is interesting. There were a ton of questions that all revolved around guilt, fears, hope, and expectations. So Jenny, and I just sort of sat back and had a conversation about those ideas. We worked in the questions from you, the listeners, and we shared our own. I don't know remembrances of different things that we thought might help you get more comfortable with type one diabetes. I appreciate if you consider going to T one D exchange.org. Forward slash juicebox. And completing the survey. That's it. I won't give you a big thing you hear about it every day on the podcast he one D exchange.org. Forward slash juicebox. completing the survey will take fewer than 10 minutes. It'll help a bunch of people, including you, me and other people with type one T one D exchange.org. Forward slash juice box. And if you want to hire Jenny, she works at integrated diabetes.com. type that into your browser. Go find out about Jenny
the Omni pod five automated insulin delivery system is here. And they're the sponsor of today's episode. If you'd like to learn more, or get started with Omni pod five, go to Omni pod.com Ford slash Juicebox. Podcast is also sponsored today by Ian pen from Medtronic diabetes. The in pen is an insulin pen that has much of the functionality of insulin pumps. To learn more and get started go to in pen today.com. Jenny, we're just going to do one big thing today. And that's it. Awesome. All right. So for the bold beginnings series, which by the way, I'm starting to see feedback about online, which is very exciting.
Jennifer Smith, CDE 2:15
Yay, we're finally, hopefully it's yay, feedback.
Scott Benner 2:19
Do you think if it was bad feedback, I would have brought it up while we were recording another?
Unknown Speaker 2:23
Well, you know, you have to give honest feedback when other people would really like to hear a little more about this or didn't really agree with that, or what, uh, you know, honesty is
Scott Benner 2:33
that made me laugh. I mean, I would have that conversation. I'm gonna be honest in front of people, I would have that conversation with you privately, privately. Giving feedback, and really no one likes this, I didn't realize that people are finding it useful in the way that he intended. So that's perfect. Very excited. So today, we're going to hit this one doesn't seem like fun at all. It's a Monday morning. But this one is, is titled guilt, fears, hope and expectations. And there are a lot of
Jennifer Smith, CDE 3:07
questions are mostly like comment, oh, let's
Scott Benner 3:10
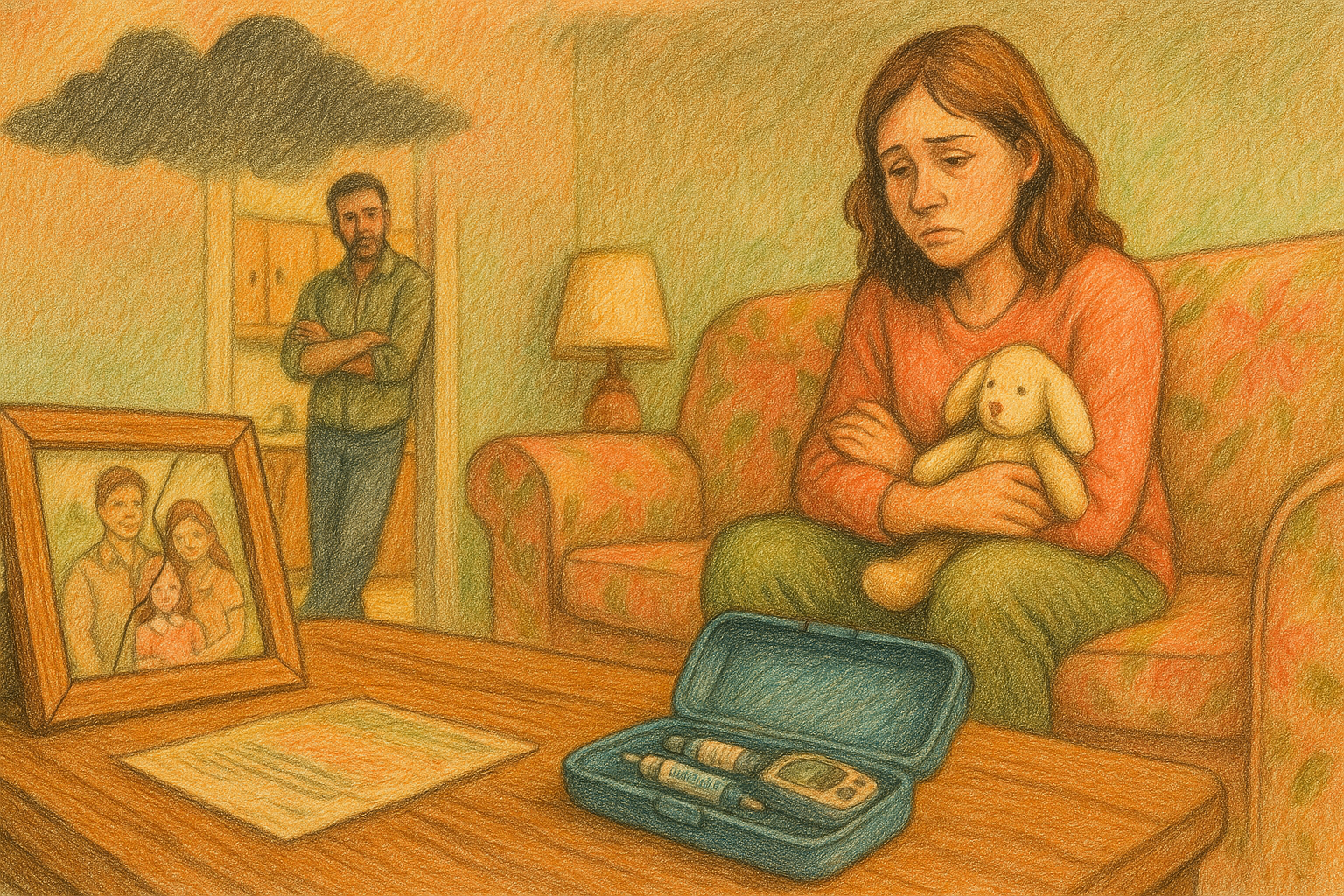
dig right in and find out I'm sure it's full with honestly. So I think, you know, I don't even want to give my opinion yet. Like, let's just talk. So the first person said that they're that they experienced immediate grief around diagnosis. Just immediately, like, like a loss had happened. I've talked about this on the podcast before, I've tried to have therapists on to talk about how you manage grief. Because I don't know from a technical standpoint, but it's so strange, isn't it? We just talked about this before we were recording it. Yeah, we did. Yeah. I guess I'll say it here while we were recording. There is a reaction that you have when you get bad health news and bad health news that isn't going to get cured. You know, it's not like, well, you have the flu, just try not to die for six days, and you'll be okay. Again. That kind of stuff. There was
Jennifer Smith, CDE 4:06
when I go back to being the tennis pro or whatever, you go, go go
Scott Benner 4:11
back to your life, this is all going to be fine. But when I was diagnosed, I remember just thinking, Oh, well, we're not going to have the life I thought we were going to have right like like and then over time that you realize that diabetes isn't as difficult as you imagined it's going to be hopefully you get some things figured out. And that it's not. It's not. I don't know, for us at least it's not like somebody chained to art into a post and we couldn't get her off again. You know, we had to just live our life here in this little space. But it still is true that we're not living the life that like when Arden came out and we were like look, we have a baby like in our symbol. You know what I mean? We're holding the baby up and on the hill. This is not my fault was gonna happen. And so you I think that's the loss. I think, I don't know what you think, though, because you were diagnosed at a different time and a different age.
Jennifer Smith, CDE 5:10
I was. And
Unknown Speaker 5:14
I don't, I
Jennifer Smith, CDE 5:15
don't know that I so much had a sense of loss as a sense of significant change. When I was diagnosed in, in the hospital, the nurse educator, was very quick to tell me, I could do mostly anything that I wanted to do. What she told me I couldn't do, she said was very limited. And boiled down to essentially being was something like a bus driver, a pilot, and I couldn't be in the military. She's like, so think of all the things that you really liked doing, and might want to do at this, you know, age that you're at, and realize that you can still do all of these things. And I was like, Well, I probably was never I was not thinking about being a pilot. I wasn't thinking about being a bus driver, or, you know, whatever. So I just felt like, okay, I guess I just have to do these additional things. So my personal sense wasn't so much of a, obviously, I didn't feel guilty. I mean, I didn't have anything to feel guilty about, I'd have to ask my mom, if she had any guilt, or my dad felt any they'd never voiced it if they if they did. But that guilt and sense of loss, I hear a lot of that in the families that I work with. And it it can stick around.
Scott Benner 6:47
Yeah. So Yeah. For me, I was a stay at home dad at that point. And they, we pretty quickly, even though we didn't understand the link between coxsackievirus and maybe being diagnosed. And even at the moment, in the beginning, I didn't understand that Arden had, you know, markers that made her more likely to get type one, two, I didn't understand any of that at that time, right. But I did see, anecdotally she was sick, she had this Coxsackie virus, and now she has diabetes. And I beat myself up pretty hard about that. Because I kept thinking, like, Did I not wash your hands? Did I not wash my hands?
Jennifer Smith, CDE 7:25
Did I expose her some way that could have been prevented? Kept thinking
Scott Benner 7:29
I took her to the wrong place. Like, like, did I get in my car one day and drive to this place for lunch instead of that place for lunch. And that's why Arden got coxsackievirus. And now we're here at the hospital in Virginia, like, you know, and as it's crazy, because it's twofold. It's not something you can control. And it's obviously not something you have vision for that you could have not done. But yet there's that part of your brain that goes if you What is it instead of zagged maybe this didn't happen. And it's hard not to feel that it's almost like you're gonna have a car accident and think if I would have just left 30 seconds sooner this wouldn't have happened. Yes. You know, absolutely.
Unknown Speaker 8:08
Yes. I've only ever had
Jennifer Smith, CDE 8:10
one car accident in my life. I was coming home from from college and the the roads were clear. Except you know what black ice is? Right? Yes. So driving home. And instead of taking the highway highway, I took a road that cut some of my time off. And it was more of like, let's call it a country road, right? I mean, it was paved. It wasn't like weird back country or anything, right. But I had this little renewal Alliance. That was my very first car. The back tires hit this patch that I thought was snow because it was like lightly covered. And I dashed like across the other side of the street and across the ditch. I hit a mailbox and I ended up in somebody's backyard. Wow. So yes, I did. And at that point, I was like, Well, how could I just like, slow down when I saw that snowy patch in the road, knowing Wisconsin weather and whatever, but you can't go back just have to be like, Okay, now I'm more aware at this point, I realized
Scott Benner 9:14
that you'll black ice out of context. When Kelly and I were very young, she would tell me all the time, be careful of black ice. And one day we were driving. And I just started to wiggle the steering wheel and I yell black ice and she and me and jokes are no wondering how we're together. How she didn't just like say like pull over and let me out now You idiot. I've done you know, it's funny. You were talking about the things that the doctor told you or the the educator told you you couldn't do and you're like, Well, no problem. I don't want to be these things. Anyway. Have you ever heard the lady that came on the show whose husband was a fighter pilot, I think and the person told her kid when the kid was diagnosed, don't worry, the only thing you can't do is fly a jet. And it's the only thing the kid wanted to do because that doesn't you know And of course, you know, I think even in that conversation, the woman's like that poor lady like she was like, so sure she was gonna reinforce to my kid that you can do anything. But there's this one simple thing you can't do,
Jennifer Smith, CDE 10:13
you can't do. And that's exactly what it was. Yeah, they wanted to know, so.
Scott Benner 10:16
So it takes me into these next couple of statements, people said, I really needed a lot of hope in the early days. And that is what people are trying to do. And they say, Don't worry, there's only three things you you know, etc, or you'll live a normal life. Just have to count your I think, I think, oddly, that so much of the poor management information that people get in the beginning stems from someone trying to be kind to them. Does that make sense? Because, like, Don't worry, your carbs and do it like they're trying to make it seem easy? Yes. Right. And maybe that's the maybe that's the only thing you can do in that spot? I don't know.
Jennifer Smith, CDE 10:58
I know, I would agree is and especially boils down to the one comment that, I think is it's hard to understand, once you get further into understanding management is the food tide one, you can just you can eat anything, just take your insulin, right. And that is, it's a way to tell somebody, not much has to change. Look, you can keep doing everything that you have been doing. You have to just add these little extras in to the picture. And there's supposed to be a sense of relief, like thank goodness, I can keep, you know, eating whatever it was for lunch that I love to eat. But it doesn't take away from the feeling of the additional things that are really big additional things that we're teaching somebody they now have to do.
Scott Benner 11:58
These next couple of statements. Kind of they kind of hinged together a little bit. This one person said they kept hoping the doctors were wrong. Like they sent them home. I hear that a lot from people. I only went through it for a day. And I know Arden had some sort of crazy honeymoon Day, which I look back now and think probably wasn't even a honeymoon. She just really just didn't need insulin. This one. Right, right. Like they were wrong. And I know they were wrong. I immediately was I called my friend who's her pediatrician. I was like, Hey, she hasn't needed insulin all day. I think they're wrong. And he was so sad. He was like, oh, Scott, like she has. She has type one. She's he's like this will change. Like, just keep watching. You know? Yeah. There's that. And there's this other part here. This person said that there was so much confusion in the doctor's office. And looking back the way she sees it is they weren't 1,000% Sure the kid had diabetes, but they were sure. And she said I just kept seeing the medical people looking at each other and nodding and kind of like talking to each other with their faces, but not saying anything out loud to me. She said she found it very scary. Like what is in that space?
Jennifer Smith, CDE 13:12
And scary in terms of? Are they confused? Are they actually the right people that I should be talking to? I mean, really, you don't want a confused? Look, or these exchanges of eye movement, facial expression between what you're thinking is an educated professional to get an opinion or a diagnosis from you just want the direct information. Tell me what you think it is. What are you going to do to prove that it is or is not this? Just be honest,
Scott Benner 13:50
it's super interesting that I'm going to tell you something personal has nothing to do with diabetes. My mom's blood pressure started to go up a few days ago. So I get a message from her. Hey, Scott, my blood pressure has been high the last couple of days. I call the nurse where she's living and talking to the nurse. And I said, Hey, my mom's blood pressure has been high for four days. Now, what are we doing? And she said, All the doctors gave her a little more medication. We're waiting to see if that worked. And I was like, Well, what else are we doing? You know, are we just gonna keep medicating or until you know, it's like, and she says, I want to get this word for word. She says, Well, your mom has a heart condition. And those don't get better. They just get worse. And all I could think was what in the hell are you thinking saying that to me? Like, like, Hey, you don't know me? Like I took it. I was like, Yeah, I know. Like, but like, that doesn't mean we're giving up on her right? Like she could see the cardiologists couldn't see. But all I could think afterwards was like, the lack of bedside manner. In that statement is fascinating. Absolutely. He was like, hey, what do you want us to do? That's right. What? Something? Could you do something? You know, it's just it was I just couldn't believe that it occurred to her to speak like that.
Jennifer Smith, CDE 15:11
Absolutely. And I think what we've lost actually, not everybody, but I think what there is a loss of in healthcare is a sense of being human. Right? It's a sense of, how would I want this presented to me? Yeah, imagine you're the person sitting there. And I think doctors, you know, and or other clinicians, not just doctors in general, but other clinicians have become so very just blunt, for lack of a better word about this, is it? And no, it's not going to get better. Well, you may want that information eventually. And you may actually sort of know that, you may understand that as an adult, especially, but to have somebody so very cut and dry be like, Nope, this is it. This is, this isn't going to get any better. And we've put a little bit of empathy in that rather than just being so
Scott Benner 16:15
yeah, Jenny, I don't want her to lie to me. But oh, there had to have been a few better ways to say,
Jennifer Smith, CDE 16:23
I mean, even to be able to say, well, we're going to use these types of medications. And as you understand the medications, we may need to titrate we may need to change them. As things change with this type of a health condition. We do know that it doesn't typically heal. And so we're going to have to try things to keep your mom comfortable to keep her feeling well enough, but it will progress. Yeah, I mean, I think that was much nicer.
Scott Benner 16:52
No kidding. I fascinate anyway, so there's a balance between being told the truth and being slapped in the face with some horror, there's better ways to talk about and I don't, there's one,
Jennifer Smith, CDE 17:06
I think, as you say, slapped in the face, kind of with a diagnosis, oftentimes, in a very immersive, you know, emergency type of diagnosis for type one. Many times it's not that somebody's caught symptoms early enough and just come in to the pedes office or to their typical primary care doctor and said, Yeah, I'm not feeling so great. Could we, you do some tests and have some discussion and whatever many times it's very emergent. And then like mine, I went to the emergency room, and I was right there when the doctor told my mom and myself what was wrong? Yeah, there was no like, time in a nice room someplace with like birds outside the
Scott Benner 17:50
human. That's all like, just yeah, that's all I'm looking for from anybody. I'm going to read this person statements pretty big.
The Omnipod five is the only tubeless automated insulin delivery system that integrates with the Dexcom G six CGM en uses smart adjust technology to automatically adjust your insulin delivery every five minutes, helping to protect against highs and lows without multiple daily injections on the pod five is currently cleared for people with type one diabetes, ages six and older, and you have the option to control it all from a compatible smartphone. On the pod five is also available through the pharmacy, which means you can get started without the four year Durable Medical Equipment contract that comes with most insulin pumps. Even if you're currently in warranty with another system. Wink wink, you know what I'm saying you can switch to get started with Omni pod five, go to omnipod.com forward slash juicebox. If you're not ready for an automated insulin delivery system, go check out the Omni pod dash, a wonderful pump just not automated. And you can do that at my link as well on the pod.com forward slash juice box, you may be eligible for a free 30 day trial the on the pod dash. Did you know that full? Well, it's true. For full safety risk information and free trial terms and conditions. You can also visit omnipod.com forward slash juicebox. Now if you just don't want an insulin pump, but you also don't want to just be using needles or just a regular old pen, you should consider the in pen from Medtronic diabetes. The M pen has some of the functionality that you come to expect with an insulin pump. I'd like to tell you about it right now. But first, let me tell you this in pen today.com. Okay, now now that you remember the link in pen today.com I'll tell you about the N pen. So with the M pen, you get the pen and you get an app. Now here's the thing about the pen, Terms and Conditions apply but It's possible that you'll pay as little as $35. For the pen. That offer is available to people with commercial insurance, you should go check it out. While you're there, take a look at this in pen offers 24 hour Technical Support hands on product training and online educational resources. The M pen is an insulin pen, but it does more. For instance, it has a dosing calculator reminds you of when doses or do carb counting support and a digital logbook. It also has an activity log meal history, your current glucose, a dosing calculator, active insulin remaining glucose history and reports for you and your doctor. Pretty cool, huh? If you're ready to try it, head over to in pen today.com. There's a form there just asks you for your name and your phone number and tell them what kind of insurance you have like private insurance, government insurance, click Submit, somebody gets right back to you. It's pretty easy, and pretty cool. In pen today.com. So whether you're looking for an insulin pump, an insulin pen, glucagon Dexcom, the Contour Next One blood glucose meter, whatever you're looking for, check out my links. They're available at juicebox podcast.com, where they're in the show notes of your audio app. When you click on my links, you're supporting the podcast, and you're being connected with quality, quality devices and products. I'm gonna get you back to Jenny now, thank you for listening to the ads in Penn requires a prescription and settings from your healthcare provider, you must use proper settings and follow the instructions as directed, or you could experience high or low glucose levels for more safety information visit in Penn today.com.
I felt an incredible grief, we had no family history of diabetes, it was a surprise. And I was extremely scared on the way from the urgent care to the hospital, following an ambulance that my daughter was in. Or excuse me, followed by her ambulance ride. My daughter asked what diabetes was. And she said I was like, it's sort of like being allergic to sugar and you need shots. I didn't know a lot. She said she said I wept all night. When she wasn't looking, I thought I can't do this, I really just can't do this. She said I wanted to I wanted someone to come and give me a hug to validate my feelings and my fears, but also that told me that this was going to be okay, that she could live a great life. And that I would be able to do it. A lot of parents have learned to manage well. And you can too, she said that I would have been would have been great if somebody could have said that to me. She can still do everything you hope, etc, and so on, I would have liked someone to tell me that the next few days were going to be hard. And that it would involve sleep deprivation, it would have felt good to know that I could have done it one step at a time, maybe one day at a time that I could have found a Facebook group that I could have shared my struggles with somebody else that somebody else might have known the difference. Sure, yeah.
Jennifer Smith, CDE 23:12
And I think some of that also ties into the rapid nature of discharge upon a diagnosis like this. I mean, in today's world, unless, unless there's something really detrimental within that diagnosis. And they really have to keep you for many, many, many days. Most often. It's an in you might be there one two nights, and you are out and you get rapid fire information. First you get a diagnosis that you had no idea even what it was many times, and now you're getting education, if you will, and you're getting information about all of these things that you're going to have to do again, the factors of life changing, become like a quick like knock on the head. Yeah, here you go. All these things. You know, when I I think that when I was diagnosed, I was in the hospital for an entire week. And day after day, there were new things brought in different pieces of education in a nature that I could swallow and my parents could swallow. Because it wasn't all rapid fire.
Scott Benner 24:24
Yeah. I have a note from a person that just I just randomly got this note a couple days ago and just says Hey, Scott, thanks for everything. You've helped me more in two days than anyone else helped me in the last 20 years. And what I responded back to her was I was like, well, that's really wonderful. Thank you. I appreciate that. I'm glad that the podcast is helping you. But I didn't have to tell you those things while you were sitting in the hospital. And it still felt like somebody hit you in the head with a frying pan. Yeah, I got to tell you when you were relaxed and at home and and I think in
Jennifer Smith, CDE 24:55
a different way though, like there's a slap in the face with something that You never expected again, a type one diagnosis or a type two diagnosis or you know, whatever. But then there's a slap in the face kind of with, well Darn, this information spin around. Why didn't I have access to it? Why did nobody told me about this? Nobody told me I could do this way, or use this product or whatever. So I think they're, they're similar but different enough that you've been already navigating through something. And now you're a little bit more irritated.
Unknown Speaker 25:32
What? Why didn't nobody tell me that?
Scott Benner 25:34
Hers has another layer. And that definitely is that, you know, if she would have found the podcast, you know, six weeks after she was diagnosed, she'd be like, Alright, cool. Six weeks, I didn't understand what I was in 20 years is hard. Because you start doing that reverse math, you're like, I've done damage to my body now that I can't get out of, and you're telling me this all existed? And just no one told me about it? Right. So it's a strange balance. How do I explain type one diabetes to a three year old? And I mean, I don't know. I don't think you can. What
Jennifer Smith, CDE 26:07
did you do with I mean, Arden was to right? Yeah, she was how did you guys talk to her about it?
Scott Benner 26:13
You look her in the face. And you say, I'm sorry, I have to give you this needle. And you try not to cry? Like, I mean, what else are you gonna do? Right? Like, it's, she's two or three years old in this in this person's situation? What are you going to say? Like, correct me? What are they going to understand?
Jennifer Smith, CDE 26:33
Hi. And that's where you have to look at is the understand level. Yeah.
Scott Benner 26:37
I mean, eventually, we told her, there's a thing inside of her body that makes the stuff inside of this needle. It's not making it anymore, and she needs it. And so we're gonna give it to her this way. And she then saw the needle, put a big smile on her face and ran away from us, just like, took off. She just told me. Two nights ago, we were sitting around online, googling what are people's biggest fears. And guessing people's top fears, like by state by country was actually kind of interesting. Yeah. And she said, Oh, this is one of mine. And so we're all like, trying to guess what it is. And she's like needles, she's like, I'm afraid of needles. She's like, I really don't like needles. And I'm gonna try to get on the podcast and to talk about it. But Arden's only ever given herself one shot. One. And it was you did
Jennifer Smith, CDE 27:30
it for such a long time,
Scott Benner 27:31
I switched to a pom pom, and we switched to a pump when she was four. And she gave herself one recently, because she's going to school and I was like, listen, you're going to hit a spot at some point, while you're at school where you're gonna have to clear something, you're gonna need an injection here, do this one. And I'll let her tell the story. But she, I think she took the better part of 90 minutes to put the to put the needle on her thigh. But she had to go into a private room by herself and like psych yourself up to do it. But if you take her she'd gets blood draws constantly sure hates them, but has to watch it happen.
Jennifer Smith, CDE 28:06
And somebody else is doing it though. Yes.
Scott Benner 28:09
But she stares at it. She oh my god and look away she goes, I need to see it happen. I'm like, All right. I don't even know how to explain that. That thing, right? So it's not just as simple as nobody wants to get stuck with a needle, because nobody wants to get stuck with a needle. But she really, she hates it. You know, but how do you explain to a three year old? I don't know. Like, I think the best thing I can say is that after a while, it just becomes commonplace. And a three year old doesn't remember, five months ago, the first day you were like your Give me your arm, you know? Right?
Jennifer Smith, CDE 28:46
Well, and as you teach kids, anything, I think, I think parents who are very verbal and explanation about we're going to do this, because of this, like, I'm gonna go outside and I'm gonna mow the lawn, because the lawn is long, and it needs to be caught. And, you know, we don't want
Unknown Speaker 29:07
bugs growing in our backyard, or whatever it is, I mean, at a level that a
Jennifer Smith, CDE 29:12
kid can understand. And then you continue to progress through. As kids grow, you keep explaining more and more. And oftentimes, they end up coming back to you with the endless flood of questions that over the age of like, four comes into the picture, right? And as they ask more, you get a little bit deeper in, I guess, explanation. You have to start at a really like, dumbed down level. Yeah.
Scott Benner 29:36
And you build on it. You really do because I mean, even even saying, There's something inside of your body that makes this stuff but it's not working anymore. I don't even know if there's context for that. Really. There's stuff inside my body. You don't I mean, like what like this is because for a young person, you're you you're this the village that you see out front you're not your intestines and You know,
Jennifer Smith, CDE 30:00
if the child is interested in books already, and you read often, there are a lot of really good kid based books that are all different levels of knowledge to be able to start with an explanation. And I guess I would probably start there. Yeah.
Scott Benner 30:18
And I think understanding that it's not like you're, you're not talking to a friend, you're not going to explain to them right now. And they're just gonna get it. It's going to be like a process. And, you know, you have to be patient with it. This person said, will my child live a normal life? I know the answer to that now, but I absolutely did not know then. So we covered that. This person said what you said earlier that the simplest advice is still incredibly difficult to comprehend in the early days. It would have been great if somebody would have explained a honeymoon to me. You know that there's one. How about this one? Will I ever sleep again, they just talked about checking every two hours with no end date, and did not discuss CGM with me at the time.
Jennifer Smith, CDE 31:04
That's where with today's technology a you as the parent or caregiver, you go back and you say, You do realize that not only have you loaded me with this thing, not you, you know, by decision, but you've given me this thing to now help me manage for my child, you're telling me you have to do this, I know that this technology is available, you will risk you will write a prescription for this, right? I mean, you will give this to me, there is no reason not to. If I have the ability to sleep, I can make better decisions with all the things you told me to keep track of in the day for my child,
Scott Benner 31:40
but you were thinking about what she said like you're gonna check every two hours. There we go overnight, though. Yeah. Well, what? You know, right. And then there's some doctors who used to say, Don't worry, like, it's very important to check during the day, but overnight, don't worry about it, as well. Because that's what I was told. I was like, how the hell is that reasonable? Like, they told you to not check overnight? Overnight was fine. But during the day, you need to check. And I was like, yeah, and then I stopped. And I didn't do that. And that's how I Well, first I listened to them. And then eventually, I was like, wait a minute, that doesn't make sense. And then, you know, that's how I learned that I was putting Arden to bed at like 180 blood sugar. She was waking up at 90, and I thought I was doing great. I checked overnight and saw she was like 58 At some points.
Jennifer Smith, CDE 32:27
Right? I mean, that's very similar to being like, your newborn baby needs to nurse every two to three hours or get a bottle every two to three hours. But at night, go ahead and sleep about it. They'll be fine until you wake up at nine o'clock the next morning.
Scott Benner 32:44
Exactly right. And it freaked me out. I when I figured it out. It would have been nice. This person says if a medical person would have just talked to me like a human being. And this next person says the favorite thing that an endocrinologist told me early on you see this, people say this all the time online. But there's two things you can no longer eat poison and poisoned cupcakes is what they think. Yeah. It made us realize we could do what we needed to do and succeed. The mental load of it all. For me. My My son was for a diagnosis. And I was able to work from home with him until we became more stable with our sugars. And that helped her with her the mental strain just taking another thing away in life and being able to focus more on that we got super lucky. I was a stay at home dad already
Jennifer Smith, CDE 33:33
already. Yeah. When I think about especially in this I have a number of single parents, you know, single really single like there is no other person father or mother caregiver involved. And or just the sharing families, right? Sometimes you're with mom, sometimes your dad, sometimes you're the grandma and grandpa or whatever it might be. And in a diagnosis setting where there really is only one caregiver. Now you have added when you talk about things changing, you've added another layer of change that they may already be pretty overwhelmed.
Scott Benner 34:13
Yeah. Yeah, no, no, it's not everybody is in my situation where I was like, Oh, well, I don't have a job. I have plenty of time to figure this out. Right. You know, I tell people all the time. They're they, they thank me for the podcast. I was like, thank my wife, like she made enough money when we were younger that I didn't have to work and that's part of my free time. It was around figuring out diabetes. I wouldn't call it free time like you think of but you know,
Jennifer Smith, CDE 34:37
right. Like you're baking cupcakes for the neighborhood.
Scott Benner 34:42
Oh, you know what I'll do with my free time. But I mean, I wasn't at work, where I had to disconnect myself for my family's problems so I could get a thing done so I can collect a paycheck. You know. This person said I needed somebody to tell me it wasn't my fault repeatedly. In the beginning I'm here, this is interesting. We just talked about needle fear. And so I kind of want to come back around to this for a second. This person saying needle fear was really tough for my kid. They figured it out. It's no big deal now, etc. There's this thing that I did that I believe is worked for us. And I think it's worth people paying attention to because in the beginning, you can do this thing. Where you're like, well, we'll use the numbing cream. We'll get a buzzy, we're gonna do this. We'll do that. We're gonna make it easier. Oh, it's time for your shot. Not yet. Okay, buddy. Let's wait like I am more of the School of like, draw the insulin, stick it in push the thing over with like, we're not going to like this one way or the other? Yeah, let me draw it out. Let's not draw it out. I just I learned that lesson very early on when I think my wife and I spent an hour and a half in the middle of the night trying to get my son to swallow a pill. You just like swallow the pill? Just take the please take the pill. I don't want to hold on. Wait a minute, wait a minute, wait a minute, you know, like it's the it was that I'm just aren't used to wait a minute. I was like, God, let's just do it fast and get it over with. Yep. And just get it done. I mean, you'll find what works for you. But I think dragging it out, just extends the panic because it goes away when it's over. It does. Yeah,
Jennifer Smith, CDE 36:22
really. It's even like an argument. You know, with a five year old, essentially, you're having an argument. And you can tell that you're continuing to get more irritated, because they're just not listening to you. It's better as the adult to literally just be like, I'm stepping away. I've told you what needs to be told to you. We're not doing it for this reason. And I'm gonna go over here. And you can just sit because there's, you know, so just deal with it. Now, get it over with and move on. You also have a lot more time in your day.
Scott Benner 36:54
This one person says I was 39 when I was diagnosed, and I kept thinking, What do I do wrong? And she said, or he said, Excuse me one or the other. I still, they said that their mental health is still not where it was before they were diagnosed. And they, they just don't know what to do about it. And speaking of not knowing what to do about it, this next person says, How do you deal with overwhelming emotions? I've never had them before. And now here they are, I don't know what to do. And I don't know where to get help and do the whole thing.
Jennifer Smith, CDE 37:28
Yeah. I mean, the the mental health piece of diabetes management, both for caregivers, as well as the person living with diabetes, thankfully, has gotten more attention, if you will, in the past couple of years. But I think it's still well at the bottom of pile in terms of discussion and asking, how are you doing with all of this? You know, what kinds of things are you doing? To to have joy and to still feel good and to do as much as you can back to the normal, whatever normal is, right? I mean, there are, there are quite a number of mindfulness and meditative types of things that you can kind of do to get back to letting your brain at least work through things in a way that doesn't make you continue to feel stressed all the time. But you have to look for the resources, right? Nobody hands something to you like that at diagnosis.
Scott Benner 38:34
Well, there's a question I asked a lot when I'm interviewing people, and they have really heavy stories, you know, people are like, five, six metal conditions, like a lot of stuff going on, whatever. And they get done. And I try to remember to say to them, Hey, are you okay? You know, like, because I also try to make my interviews fun, and like you're talking about these really serious things and to keep it light hearted. And then I'm like, are you alright? I'm frequently surprised by the number of people who don't know if they're okay or not, or not. They can't say they it's not that they don't want to tell you. They're not okay. It's that they don't even consider if they're okay. Like it's not a concern of theirs. They can I guess they compartmentalize everything to the degree where they don't ever consider Yeah, at all. Yeah, you know, I've had people I'm like, Just take your time. Think about it. Are you alright? They can't say, you know, and that's, that, to me seems like emotion. They're not okay. Yeah. And they're not dealt with emotions. They don't even know how to like, put words to them, you know, right. Right.
Jennifer Smith, CDE 39:41
And I think some of that might come from trying to bring down emotion around diabetes management make right to be able to just see the numbers as numbers and information and be able to navigate through them and move on right. But a lot of that is taking A piece out, that is part of being a human. And, yeah, it's okay. It can go too far in terms of I don't really even know how to analyze whether I feel good or not.
Scott Benner 40:12
Or I don't think I should think about this because I don't, I might fall apart if I think about it. Right. And so everybody's just trying to be I think you're right. Like, there's whatever your situation is. And I'm certainly not, I mean, some people situations are much more manageable than others. But that is your situation. It's not, it's not changing. So you have to accept it, and then put your head down and keep going. And I guess maybe for some people putting their head down and keep going is I can't think about this. Because, hey, because it's yeah, I'm 39 years old, and my pancreas stopped working. Are you okay? I think the answer is no, I'm not okay. This is terrible. You know, like, and there's no, the doctor said they can't fix it. And it's not going to go away. So how am I supposed to be okay. And the answer is, I think you have to change your perspective about what Okay, is. That makes sense? Yeah. I mean, because in the beginning of life, everything just feels free. You know, they mean, like, I'm going to do this and it's going to be fine. And if it doesn't, I'll go do something else. It doesn't matter to me, it doesn't really hit you the first time till school when you're if if the idea of getting good grades is important to you, because then suddenly you're like, Oh, I'm being measured. Right? Yeah. And then you become an adult, and you get measured again, because you want to stay safe and secure and fed. So you got to find a job. And then oh, everything's not so easy. But then you fall into that you're like, hey, all right. I'm an adult, I'm doing it. I got a place to live. Television works. You know what I mean? Like, my vitamins, I'm good. Here's the next problem. And it's medical. And then No, no, it's not okay. I didn't want this to happen to me. I mean, it's
Jennifer Smith, CDE 41:56
well, and medical, I think is really, it's one that may or may not have a quick solution to it, or a fix to it at all. It's something that you learn to navigate with. But it's not like, I'm not okay, because my tire went flat on my car. Okay, well, this is a situational not okay. This isn't a long term. I need to learn how to accept and move forward and realize that this will be here. I know that some days are going to be great. Like I want them and other days are going to be karate. Yeah. And, yeah,
Scott Benner 42:38
I think it's important to know that you are going to go through a lot of the stages of grief, which you know, you can look up online, there's different doctors who think of them differently, but you know, shock disbelief, denial, bargaining, guilt, anger, depression, acceptance, hope, like that stuff is, it's all going to hit you. And it should This one's interesting. Do you know why they call it diabetes? Do you have any idea I'm asking you if you know, like, where they
Jennifer Smith, CDE 43:01
come from the light, I mean, diabetes in and of itself. There are several, obviously, kinds of diabetes in terms of the end like the diabetes we have is diabetes mellitus or mellitus or, you know, whatever how you say that, that last term. In terms of just diabetes. It there are Latin terms, essentially, that go along with it, which is the reason
Scott Benner 43:26
this person statement makes me think that it's, we should call it live a VDS. Because she said her six year old said, why is it that I have babies, that's how the kid heard it. So she thought I'm gonna die, because I got diabetes. She's, she's six. And you know,
Jennifer Smith, CDE 43:46
it is kind of cruddy me. And actually, it's something my husband said to me a long time ago. And we're like doing the diabetes anniversary of their diversity or whatever he's like, why are we not calling this livability? Like, you don't die right away, like, in fact, you, you move forward? Along with it. You're living so what's the, you know, worse than I'm like, Well, here's the Latin meters. Yes, exactly. So
Scott Benner 44:12
it's, I guess, Isabel did a very good job grouping these questions together for me, because I just keep thinking, Wow, it's amazing. They all just relate to each other as I go down the list, but now I realize she did this for me. So that was nice, because this next one is not pleasant. But this list this person said, my baby was diagnosed, and everything felt like that to me. She's like, well, is sugar gonna kill her? Am I gonna kill her with insulin? Is this pump gonna kill her? Will this CGM kill her? She said death just rang through her head in the beginning. Yes, it's a it's a it's there's probably a good spot here for us to point out that Jenny's living very well. diabetes and so are a lot of other people.
Jennifer Smith, CDE 44:54
Many, many other people absolutely are.
Unknown Speaker 44:57
Yes,
Scott Benner 44:58
but I we're doing Next as part of this series, because these are very likely the things that are going to run through your head when this all happens, and I think that should you not go find a therapist, or should you not go find an online group, that it would be very helpful to know that there was another person who thought, I'm gonna kill everybody. I thought I was gonna call Arden constantly. In the beginning, everything I did, I was like, this is definitely gonna kill her. Like, just, you know,
Unknown Speaker 45:27
I'm gonna give this to her. And I don't know that it's right, and I'm gonna snack and well,
Scott Benner 45:33
lunch wasn't lunch anymore. Lunch was just like, I wonder if I didn't screw this up is how it felt. You know? And then, you know, a couple of hours later, she was still looking at me. I was like, hey,
Unknown Speaker 45:43
yay, was when I didn't. Yeah, it isn't. You know,
Jennifer Smith, CDE 45:48
I haven't thought about it in quite a while though. The question about the word. diabetes, I really haven't. I mean, the the first part of it has nothing to do with death at all Daya. diabetes really just means a passing through or a siphoning right. And mellitus or mellitus means sweet. So it's they tested eons ago, when we had nothing. Doctors would literally dip their fingers in like a person's urine and taste it. And if it was sweet, they knew that they had this like sugar sweats, sugar sickness, or honey sickness.
Scott Benner 46:24
You also knew your doctor really cared about you. Because taste in
Jennifer Smith, CDE 46:28
my urine. Urine is pretty sterile. So unless there's like Aki, you know, whatever,
Scott Benner 46:33
how about I don't care, Jimmy, I would not have been a good doctor. In that moment, I would have been like, listen, we could taste this to see if you have diabetes, but I gotta be honest, I'm not doing it. Go find a friend.
Unknown Speaker 46:45
There's lots of stuff that could be in. Good Doctor was like, let's taste this and see what's going on. He signed up for
Scott Benner 46:52
that. This person said to be very careful that they stopped taking care of themselves when they were diagnosed. She said I could start, I got to the point where I could count the times I was showering because I I was just not taking care of myself anymore. She's like, I was fighting with my insurance company, calling companies begging nurses to call me back. She said I was distraught and overwhelmed. And that's where the that's how the grief hit her. She kind of just started to let go of like everyday activities that you would do.
Jennifer Smith, CDE 47:25
Right better now. And I think it brings it in, I mean, that that brings in a layer in terms of what she mentioned, things like calling insurance and fighting for things, right? It brings in a piece to that management, that is the addition of more, right more things to keep track of and do. It's not well, my you know, medication that I take for whatever it is, I pick it up once a month, and it's okay. And I don't really have to think about it. And I want to fight the insurance to cover it and whatever. But all these parts that ended up coming along with diabetes management in today's world, especially mean, you may have to have more interaction, at times, not necessarily every day, but more interaction at times, and especially in the very beginning. When you are asking your insurance to now Hey, cover this and cover this. And we've got this new diagnosis, and they've got all of these protocols and things that they have to follow within their organization. There's a lot of work upfront,
Scott Benner 48:32
ya know, I've yelled the F word into a phone a lot of times the beginning Oh, yeah. I don't know that I've ever used no word. But I've heard Yeah, I used to find that it moves things along very nicely.
Unknown Speaker 48:46
I probably said them after I was off the
Scott Benner 48:49
- i I'm assuming that this customer service rep would say that they don't feel like they're in a safe space. Now I'd hang up the phone. But back then I was like, Hey, you don't know how hard this is? Let's go. You know, it's just interesting. Consequences are real. But I couldn't let that stop me from living my life, the balance. I think that not being a person with diabetes, I can't be sure. But I think that's got to be a bargain that everyone with diabetes makes every day of their life. Like Absolutely. Right.
Jennifer Smith, CDE 49:24
Absolutely. With with everything. I mean, the consequences. And they're not necessarily saying the consequences are real in terms of, let's say bad versus good. I don't love those words. But there can always be a good consequence to your choice. There could also be what you really didn't plan on happening, because it just worked out the other way. Right. So
Scott Benner 49:47
this person says, the fear of complications for my daughter was my biggest worry. And that's all I saw when I look things up online. I have to tell you, my brain works that way too. Like, you know, you have an autoimmune disease, there's a likelihood you might have another one at some point. At what point your brain
Jennifer Smith, CDE 50:08
goes to the world what else could be wrong? Yeah, the worst What else could happen because of this? Yeah.
Scott Benner 50:14
Which by the way, you have to guard against, because you, you have to make sure to look at all your possibilities as things are happening over your lifetime, but do not just see diabetes all the time, too. I see people that happens them all the time, like, hey, my kids got a headache. What's this got to do with diabetes? I was like, I mean, maybe, yeah, maybe the kids just got a headache. But listen, I don't know is your blood sugar bouncing around all over the place? They've been low for a while high for a while. If those things decide people get headaches, still people with diabetes, get headaches and have nothing to do with their headaches. And it's hard sometimes to separate them. You know,
Jennifer Smith, CDE 50:50
and then in kids in terms of headaches, I think a big one is hydration. A lot of the time, quite honestly. And yes, you might see some blood sugars that look funny to hydration being a big piece of overall management. But headaches just alone. Oftentimes, it's drink some water,
Scott Benner 51:07
I want to I want to offer some comfort to the person who wrote this, because they said that they remember thinking that their son would grow up to hate them. Because she saw what she was doing taking care of him as hurting him. I don't think that's how it gets remembered. You don't know? Yeah. I mean, I guess it could, but
Jennifer Smith, CDE 51:31
it could I think in again, that's where some of the discussion goes along with what you're doing, using less of your own, like inner thought as you work through doing an injection or changing a pump site or putting, you know, a new sensor on or all those kinds of things that parents are doing. If you talk through it, like and verbalize it rather than just think it through. Kids absorb. And they start to make connections. And with that, I would expect that the child who's hearing their parents say, we have to do this, and I'm going to do this, and this is why I'm doing it this way. They see it more from a standpoint of caring, rather than the parent. Like being me and yeah,
Scott Benner 52:17
no, I think that hopefully, over time, it shakes out that way. Yeah. This next one, I learned the most important thing I learned from the podcast is that non diabetic blood sugars are actually possible. And no one told me that at first and I did not believe it until I found the podcast. So I'm very glad that that happened for them. I guess they made it on to the Pro Tip series. But that's that's lovely that that for somebody because I do think that when expectations start getting set up and they start telling you like a seven a one C is fine. Don't worry about it, you might start thinking like, oh, I guess I guess what I used to have with my pancreas isn't gonna happen anymore. But it can. Just a quick one lady said, I was told that in the beginning, it will be hard. And I thought in my mind, that's probably means like, two, three weeks. And not a couple of years or do this for three weeks. I got that. It'll be okay. If it's only going to be three weeks. That'll be okay. Yeah, so there's one on here. There's not there's one that's not on here. And I know we're kind of getting up on your time. Am I right? We're okay. Because I'm gonna tell you right now, this list goes on. And on and on and on. Like, I think we've hit the big, the big, you know, ideas, ones, but here's one that just isn't here. And this is all this is perspective from me, because I'm not a I'm not a religious person. But I see people talking online all the time. Why did God do this to us? I see a lot, or this is going to be okay. Because God wouldn't give me something I can't handle. And so I don't have a lot of religious perspective. And I and I understand that. That's how some people might see these things, which is, you know, I have no qualms with, but what I can see from an outsider's perspective is that sometimes sometimes I've seen people not pay as close attention to their health, because they think God's got it. If that's the way to put it, I don't know exactly. And if you believe in God, and you think he's on your side, or she's on your side, or whatever you think I'm down with that. But just remember God is not going to Bolus when your kid is 330 You know, you need to take care of these things. There was just another story recently, I think it was from Australia where these people were put in jail because they let their kids die. Yeah, because they said that God was going to take care of him. And yeah, you know, I just, it's not a commentary about religion to me, it's just you have to realize you're in a, you know, a unique situation that is not going to be in any way taken care of without you facilitating it.
Jennifer Smith, CDE 55:20
Correct. And I think the bigger thing in, in whatever type of faith that you may have. Most, most religions, most faiths have an underlying to God or logos or whatever you believe in kind of out there. It gives us movement forward and information. And the better we utilize that information for the, for the greater good, or for our own health or whatever, we have to know that that knowledge, you know, is coming from somewhere, right. And so I don't think if there is a God, there would be, and I believe in God. But I don't I don't think that God dictates this person gets cancer, this person gets diabetes, this person gets heart disease, that that type of being if there is, isn't so cute into person to person on a grander scale, we've been given free choice, right? We've been given the ability to use our brain to use what we know how to do, or I don't believe that there would be doctors and engineers and plumbers, and, you know, people who are truck drivers or bus drivers or whatever, you know, we've decided along a path. And we are using our brains to make decisions. And one of those things comes in to health management. If you if you have a child or someone you love, you have to do what is been put out there already. To be two years. Right. I mean, that's that's what I believe. I think I in particular, from my faith base, I truly believe there was a reason that I have type one. I believe it's because I had a, I guess, a destiny, if you will, to be able to use what I've been given to help other people. That's what I believe. And I don't know. So I hope I'm Hope I'm achieving that.
Scott Benner 57:47
I appreciate your perspective very much, because I honestly don't have one. First of all, I just know that, from my, from my perspective, looking on to other people's lives. There are times that I want to respond and say, Please stop hoping and Bolus, right. Yeah, like, right, please. I hope. Can you pray for my son, not none of us need to pray right now push the button on the thing, make the blood sugar go down, like like, you know, like that, that kind of thing? Right? I just think sometimes that that can get in the way of you making a good decision. And so I'm going to there's a story, I'm going to get it wrong to some degree. I think it's it's something that's been repeated over and over again for years. But guys walking down the street falls in a hole. A doctor passes by the guy shouts up, hey, can I can I get some help here? The doctor writes prescription throws down in the hole. And the guy's like, well, what am I gonna do with this? And then, you know, a priest comes along, and he says, Hey, can I get some help? And the priest writes out a prayer and throws down the hole. And the guy's like, actually can't get out of this hole and a friend of his walks by, and he says, Hey, man, can I get some help? I'm stuck down in this hole. And the friend jumps in with him. And the guy goes, What are you doing? Like now? We're both stuck down here. And he goes, No, no, I've been down here before. And I know the way out. Let me help you. Right. Yeah. So you, you have to accept that help. Right, right. You can't just you can't then you can't just step back and keep saying like, what's the other story right guys lives on a floodplain. And somebody comes by and the news cameras come by and they say, Hey, aren't you gonna leave? Man, there's a flood, you gotta go. And the guy's like, no, he's like, you know, gotta get me. And the guys like, I really think you should go there saying you should leave here. And then a little while later, a guy comes by on a boat and says, Hey, man, get in. There's a flood common. Let me get you out of here. And a guy goes, no, no, no, no, you know, like, God's got right. And then eventually the guy's house gets knocked over. He's dead. He looks at God. When he opens his eyes. He goes, what happened, guys, like, like I said, the reporter with a whole bunch of hell, I sent the guy with the boat, you know, I mean, it's an old story, obviously. But you really have to. These are just parables because this is how people's minds work. Correct? Right. So take the help that's offered to you and wouldn't help go to somebody who knows what they're doing. Yeah, excuse me find people who have been through this before. Err how you feel, don't hold your emotions in. Understand you didn't do this guilt is I understand it. But I mean, try to have some long perspective, I find that what helps my guilt more than anything is sometimes when I'm talking to a person who's got autoimmune down their family line forever. The other day, this woman said to me, Oh, my grandmother has she's achy all the time. I don't know if she has Ra. She's like, I'm not sure. But her grandmother was in her 90s. And I thought, okay, that sucks. But she still lived her whole life. You know what I mean? Like she like a long, long life. I think sometimes just seeing that other people do, it takes away a lot of the other stuff. And I also think, Jenny, that understand understanding, I don't think anybody gets out of this thing unscathed. Like, you know, I'm a little, maybe we all are a little jaded, because we know so many people with autoimmune diseases that it feels like everyone has an autoimmune disease some days, right. And I'm sure there are some people walking around who are just free and clear. Nothing's ever happened to them. But I think for the most part, that's not most people. So I don't
Jennifer Smith, CDE 1:01:19
think so either. I think most people have something that is not visible to others, similar enough to diabetes. And the only outward visual in terms of diabetes truly are the devices right? Now, the pumps and the CGM that are very visible to but even that doesn't disclose internally what the person has to go through and manage and take consideration of all day long. So yes, and I loved your little boat, and, you know, the news reporter and being like, hello, hello, something's come in, right? Because that is it. Oftentimes, we, if you really are hoping too much hope is a grand thing. It's wonderful. I, you know, we all have to hope for things. But along the way, we have to take action, in order to get to that point of what we hoped for. You can't just sit back in the launch your chair and be like, well, if it comes to me great, and I really hope that it does. That's
Scott Benner 1:02:31
not really gonna work towards it also work. If you've heard people on this podcast before we have multiple issues. And I'll say to them, If I gave you a magic wand and could make one of these go away, which one would it be? They almost never say diabetes. It's fascinating. Like, I always think like, Hola, definitely gonna say diabetes, and always like, Oh, no, I would rather not have to deal with this or, and I think my point is that even if you have one thing going on in your life, and the guy across the street has one thing, and you think, Oh, his thinks easier than my thing. If you had his thing in five minutes, you'd be like, dammit, my thing, I'll get my thing back, or how do I get rid of this now? Like nothing? I don't know. You know, this sucks. Don't get me wrong. And diabetes is relentless. And it's 24 hours and etc. But there's a way to, there is a way to get through it and not right not have to live with all these feelings. And I think in the beginning, it's hard to imagine that's true. But it really is.
Jennifer Smith, CDE 1:03:24
And I think something around it, too, is actually opening up to the feelings in the beginning and letting yourself feel all those things. You know, the stages of grief, really let yourself work through that. Don't turn it off. Let yourself work through. I feel really horrible. Could I have done something about it? No, I couldn't have changed this. Okay, let's move on. Right? There's there's only so much that you can or you're going to just feel bad forever. I don't want that for anybody was the person
Scott Benner 1:03:58
here that I didn't get through that said every hospital should have a crying room. It's the soundproof room that you can go into the chair in a box of tissues that you just sit there and
Jennifer Smith, CDE 1:04:08
let it out. And garage is a really nice place for
Scott Benner 1:04:12
me. It's like ice cream in the garage in case you're one. Well, thank you very much for doing this course.
Jennifer Smith, CDE 1:04:20
Absolutely. Good. Very good topic. I'll talk to you soon.
Scott Benner 1:04:33
First, I'd like to thank Jenny Smith for coming on the show today and continuing to pour her great knowledge into this podcast. Don't forget you can find Jenny at integrated diabetes.com. And if this is the first bold beginnings episode, you've heard there's a whole series of it, you should go back and find them. Thanks so much to Ian pen from Medtronic. diabetes please go to in pen today.com To get started. And of course the Omni pod five is available at On the pod.com forward slash juice box
I don't want to lie to you. I'm tired. This is my last editing job of the day this episode and so for that reason, I'm not going to say anything else. Just thanks so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. I gotta go to bed
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#755 Bold Beginnings: Exercise
Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 755 of the Juicebox Podcast.
Jenny Smith and I are back today with another episode of the bull beginning series and today Jenny and I are gonna talk about exercise. While you're listening today, don't forget two things. One, Jenny works at integrated diabetes.com. You can check her out and hire if you like, and to nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan. We're becoming bold with insulin. If you're a US resident who has type one diabetes, or is the caregiver of someone with type one, in fewer than 10 minutes, you could go to T one D exchange.org. Forward slash juice box and fill out their survey. When you complete the survey. You've helped the podcast, you've helped people living with type one diabetes, and you may just have helped yourself T one D exchange.org. Forward slash juicebox. Hope you're enjoying the bowl beginning series. It's not done yet, there's more coming. If you've missed the earlier episodes, you don't even have to listen to them in order if you don't want to just go find them.
This episode of The Juicebox Podcast is sponsored by touched by type one, please go learn about my favorite diabetes organization at touched by type one.org and find them on Facebook and Instagram while you're at it. Today's episode of The Juicebox Podcast is sponsored by in pen from Medtronic diabetes in pen is an insulin pen that offers some of the functionality that you've come to expect from an insulin pump. I know you're thinking, Oh, Scott, please tell me more. Well, I will. Yes, the pen is a pen. But it also has an application that lives on your smart device. This app shows you your current glucose levels, meal history, dose history and activity log glucose history, active insulin remaining a dosing calculator and reports that you and your physician can use while you're trying to decide what your next step is. Well, well well, it's not just an insulin pen, now is in Penn today.com. That's where you're going to find out more information and get started. If you're ready to try the M pen, just fill out the form at M pen today.com or do some more reading. There's actually some videos you could check out too about the dosing calculator, the dose reminders, carb counting support, and the digital logbook. So if you want to lighten your diabetes management load, but you're not ready for an insulin pump in Penn is probably right for you in Penn today.com. In Penn also offers 24 hour Technical Support hands on product training and online educational resources. And here's something else that you'll find it in Penn today.com It is actually very exciting. Now this offer is for people with commercial insurance in terms and conditions do apply. But you may pay as little as $35 for the pen. And that's because Medtronic diabetes does not want cost to be a roadblock to you getting the therapy you need within pen $35 How crazy is that? In pen today.com in pen requires a prescription and settings from your healthcare provider. You must use proper settings and follow the instructions as directed. Or you can experience high or low glucose levels. For more safety information where to get started today, you can go to in Penn today.com What's next, Jenny? Hey, we're back with the ball beginnings series. And we're going to talk about something today. That's going to happen to everybody I hope exercise, but we're not gonna dig super deep into it. We just want to make sure that newly diagnosed people understand the impacts.
Jennifer Smith, CDE 4:20
Right? Absolutely. They think it's a neglected topic. At that initial like diagnosis and the overwhelmingness of everything that you're trying to learn about. Exercise is like way, way at the bottom and what to expect to try to learn right and also,
Scott Benner 4:40
I also think that when people think of exercise, they think of at 11 o'clock I'm gonna go to the gym and I'm gonna run on the treadmill and I'm gonna lift these things then I'm going to do this I'm gonna go back but exercise could be cleaning the house or cutting your lawn or your kid going to a store. Yeah, walking around it whatever. Do we say Walmart in the variable series? Yeah. So yeah, shopping, anything that takes your, your level of activity from where it kind of normally is to an elevated place because your settings for your insulin are usually set up for when you're sitting in school or at work or sleeping or whatever. And then, let's just explain. I'm going to ask you to do it. What happens when there's two kinds of exercise? Look at me, anaerobic, and your aerobic. What is
Jennifer Smith, CDE 5:39
it and the other one? You're so funny. Oh, my goodness.
Scott Benner 5:42
I made weightlifting like sign like movement.
Jennifer Smith, CDE 5:45
Yeah. Anaerobic. Yes, like resistance and weight training. In which you're not increasing or not for long periods, increasing your heart rate, right. And then there's cardio kind of exercise or aerobic where you're using oxygen at an increased rate, right. And they both do something different to your blood sugar
Scott Benner 6:07
or could Alright, so anaerobic like from my childhood, Lou Ferrigno, lifting weight. There you go, and aerobic. What's her name? married to the guy from CNN. Oh, yeah. Oh, my God, famous actress. Did that thing in Vietnam? People didn't want that. There you go. There you go. I knew how was it possible? I could, I could give you her entire litany of what she did throughout her life couldn't think of her name. That's ridiculous.
Jennifer Smith, CDE 6:38
I actually am very, very proud. Because my husband is like the trivia man. He knows. Like, he knows. He can look at somebody be like, he did this. And he did this. And this is his name. And like the song that I I'm like, I know the song. I tell you all the words and the group is hmm, I don't know who the singer is.
Scott Benner 6:57
I'm worried that I didn't go to Olivia Newton. John. I was just trying to think of like people who used to make VHS tapes of them working out in leotard. So you would work out in your living room. But but so the point is, is that you're there's two different kinds of exercises you might get involved in. And they have two different impacts. Is that correct? Yes. Okay. So aerobic exercise may make my blood sugar drop down. Yes. And weightlifting and resistance stuff could make my blood sugar go up? Correct. Okay.
Jennifer Smith, CDE 7:30
In fact, the anaerobic or the weightlifting resistance. The heavier the load, the more that you're doing in that is more of an adrenaline kind of released, right? It's the more pumping kind of and so that can be the reason it's causing a rise in blood sugar. And the others, typically, aerobic, whether it's running or jumping on the trampoline, and a trampoline and the past couple of years. I've heard more comments about trampoline, blood sugar than any other sport for kids.
Scott Benner 8:07
I think they cuz I think it's the, it's kind of what I was bringing up at the beginning. Like your kid is like eight. And they're like running, you know, sitting down watching TV, and then all of a sudden, they look up like a puppy that saw something, jump on the trampoline now. And then they run outside and do that. And you're like, Wait, stop.
Jennifer Smith, CDE 8:27
We just hit they're all shiny dangly objects. That's what it is. They're they're here, you they look content. And then they're like, Oh, look at all it is. It's like a puppy. It's like it, there's a squirrel over there. So there's
Scott Benner 8:39
these two situations, you might fall in one, you know that soccer practice is at six o'clock. And you can prepare for it in one way and to have your kids start chasing each other around the house and run up and down the stairs 75 times 45 minutes after they ate with a bunch of active insulin inside and your blood sugar tax. Right, right. So no one tells you about that when you're diagnosed with diabetes.
Jennifer Smith, CDE 9:03
No, not at all. And if you are, again, in the kid category, or even the teen category, and teens are very much in that sedentary might move up, somebody comes over. It's the same really. And so you have to consider those really, like quick spurts of activity could be lengthy. They could be 10 minutes and your kid is done. And they're like, I want to sit down and read a book again. Right? So paying attention in those times, can give you like future vision then to what to maybe do. But it's it's all learning. Really. It's it's paying attention. It's not going to be perfect. Don't expect it to be perfect. Know that you have the tools to manage and some idea that if something's planned, you can try to accommodate and see how it works out. If something's unplanned, one of the best things is just making sure you got some carbs to manage. Because that's all you can do to fix it.
Scott Benner 10:07
Yeah, I. So kind of the way I think about it is, you ever see those beach houses up on the stilts? Okay? Those people said, I know that one day water is going to come rushing in here. And I'm gonna put my house up where the water can't get to it. And I think it's water. But I don't understand how to say. So that's fine. It's pre planning, right? Yes, somebody else built their house in the ground, the water comes rushing into the house goes back out into the ocean. They're like, I don't know what happened. What happened? You didn't plan very well. So the way I see all this is not that Arden doesn't have fluctuations around exercise if she's not prepared for it. But rock solid settings, and rock solid understanding of how to Bolus for meals so that you don't end up with a lot of insulin. In the body. It's not accounted for correctly for need. So if if Arden does not prepare to like, go downstairs and get on the treadmill and run she will get low? Absolutely, absolutely. Well to Yeah, but she'll get low like 66. And then she'll need something and it'll bring her blood sugar back up. She doesn't go from like 95 to 20. Like it's not like some crazy drop, because she won't go running when she's got meal insulin active, because she knows better at this point. Right? Right, because that's going to make her blood sugar low. So I think most of activity is not having active insulin, or cutting your Basal, if you're on a pump in a way prior to the activity, where you kind of create one of those black holes so that the drop, can't drop, because there's nothing there to pull it down, because we call it a drop. But it's not really a blood sugar drop in this scenario. It's a poll. But that doesn't make any sense, right? Well, I
Jennifer Smith, CDE 12:01
think what I've seen in a timeframe, which might make sense for again, more newly diagnosed is the common time period when you haven't accommodated before more spontaneous exercise. Whether it's insulin or extra food, or however you're going to do it, if you haven't accommodated 15 to 20 minutes into movement, that aerobic is a drop zone, and again, not dropped, like over a cliff, it's you might have been floating along pretty stable. And it's definitely going to start nudging down, right. Yeah. So that's a timeframe at least that may give a little bit of reference to people who are new to trying to figure out what to watch for,
Scott Benner 12:44
right. And I think if you find yourself in a scenario where blood sugars are dropping and rising, and you don't understand why you're going to be more susceptible to a problem during exercise as well, right? It just really did strike me as I just said that. Calling a blood sugar drop a drop makes it feel surprising, the word usage makes it feel like it's unknowable, it just happened, it just dropped out of nowhere, like those are the phrases people use. But that's not really the case. In most situations, it's you have some active insulin, it's, it's taking sugar out of your blood, your blood sugar number is falling because of that, then suddenly you start exercising. And there it is. I mean, I would think that if you made me just give one piece of advice, I'd say do not exercise, aerobic ly with active insulin on board.
Jennifer Smith, CDE 13:37
And if you do know how much carb you may need to cover, the active insulin that's there with, again, spontaneous activity and whatnot in kids is pretty much the whole day, I would say to what you can play on in schools and that kind of thing. But if it's spontaneous, and you've got active insulin, because you didn't plan to go out and jump on the trampoline with four friends after lunch, you got this insulin, it's going to need some additional food beyond what it was given to cover. Yeah, because the exercise is mobilizing that insulin faster
Scott Benner 14:09
and not just in a situation where you unexpectedly find yourself doing something but what happens when you eat dinner and then go to baseball practice. Right, right. Like that's what here's a plan. Yeah, there you go. You can also you have to sort of understand Jenny mentioned adrenaline a little while ago. Baseball is a good example. Because it's not a ton of running around for the most part, right? But people will say how come my kids blood sugar gets high in a baseball game, but not at a baseball practice. And it could just be because there's no competition at the practice. They don't feel a sense of competition. So there's no adrenaline rise. These things take time to figure out honestly do but I and I'm not just self promoting here. But if you listen to the Pro Tip series, that should teach you how to keep things more stable. And then you should have an easier time being able to see what's going on in these situations so that you can adapt to them. Absolutely. Some stuff from people here, how do I adapt existing routines and lifestyles for diabetes, like swimming, summer camping, hiking, that's what we're talking about. It might be what you're eating, you might eat something with more protein in it more fat in it to hold your blood sugar up longer. You may do Temp Basal decreases before activity to help that, again, all that's in those episodes. But I just think it's important for people who are newly diagnosed to understand that it's going to happen because people don't tell you that and no, then there you go. Right. So
Jennifer Smith, CDE 15:48
and then it's scary. It becomes scary, because nobody told you to expect that this activity that your kid loves to do, but it's sporadic is going to do this versus this.
Scott Benner 15:59
And you see this this feedback from the person said, My son was in baseball and swimming, when he was first diagnosed, the doctor flat out told me he would have to rethink the sports he was playing. And that crazy for things that would work around his diabetes. While we were learning how to manage the disease. I was led to believe he could not live a normal life with sports. Oh, but of course, he
Jennifer Smith, CDE 16:23
could oh my gosh, I'm, I feel so bad that they were told that Yeah, that's really
Scott Benner 16:29
terrible. It really is. Meanwhile, the tight end for the Ravens has type one diabetes, and you have type one diabetes, and you run for some reason I don't understand why. And it's so to a lot of other people right there professional has been professional baseball players on this podcast, who have type one, it is very doable. But you need to, you need to do the things you need to do that you you have to have your basil, right, you have to understand how to Bolus from meals, you have to understand the impacts of different foods. And now you have to add understanding how to keep active insulin away from certain activities. Or you if you become a bodybuilder, you might find yourself bolusing before you workout,
Jennifer Smith, CDE 17:15
correct, absolutely anaerobic exercise, can for many people, not always, but it can depending on the length and the weight. And you know, all of that it can drive blood sugar's up again, when it's going to be based on on your response, it could be that you start out in a really great place. And by the end of your lifting session, you're riding high or you're kind of nudging up, essentially. But overall, you have to just pay attention to you. Some of the lifters that I've worked with have taken a Bolus at the beginning of lifting session to accommodate and avoid and avoid arise. Some of them have set a temporary basil to accommodate for that. Some of them end up doing a little bit of both anaerobic and aerobic exercise, knowing that their blood sugar is going to get driven up by weights, they end up allowing that drift to happen to a certain point, and then following it with aerobic exercise, which they know is going to navigate it down and tends to kind of smooth things a little bit more on the back end rather than a dramatic drop, like we often see with cardio. Yeah. So
Scott Benner 18:24
you also have to, you know, when we talk about mixed meals, right, like it's easy to pick one food and Bolus four. But what do you do when you're having meatloaf and mashed potatoes and applesauce and these all have different impacts. Also, you could head out into the backyard to move a pile of rocks, which you would think well that's lifting except what if the pile of rocks is 45 feet from so now you're lifting and then you're walking, right and then you're lifting and you're walking, you're you're having two different impacts, you could end up doing something like that in the backyard for example, and it not looking on your blood sugar like anything happen, because you could be getting a pull down from the aerobic and a push up from the anaerobic and this all you know what I always say the podcast makes things seem simple, but Jesus. But it's very doable. And I think that's the important thing. But everything starts, in my opinion with understanding how insulin works, like with Absolutely. Well thank you very much. I appreciate course, always I'll talk to you soon.
A huge thank you to Jenny Smith for being here with me again today. And I'd like to remind you that you can hire Jenny integrated diabetes.com. I'd also like to thank Ian pen from Medtronic diabetes. If you're looking for an insulin pen that does more, you're looking for the in pen in pen today.com In a few moments, I'll tell you a lot about the show, but one of the things I'll tell you is how to find the series. So if you've just stumbled upon this one, and you'd like to find the rest, there's a way to do that. And I'll be telling you about it in just a second.
If you're into helping people, especially people with type one diabetes, I'd like to ask you to go to T one D exchange.org. Forward slash juicebox. When you get there, fill out the survey completely. And you've helped somebody, all you need to be is a US resident who has type one diabetes, or is the caregiver of someone with type one, t one D exchange.org. Ford slash juicebox. Join the registry, complete the survey, help someone with type one diabetes, help yourself perhaps, and support the Juicebox Podcast, you will do all of this in the fewer than 10 minutes that it will take to go to that link and complete the survey. The survey is very simple, you will know all the answers to all the questions. It is also HIPAA compliant, and completely anonymous, T one D exchange.org. Forward slash juicebox. There are links in the show notes of your podcast player and links at juicebox podcast.com. To all of the sponsors. And to T one day exchange, when you take the time to click on my links or to type them in a browser. You're telling the sponsors that you came from the Juicebox Podcast, and that is a wonderful way to support the show. Are you looking for a vibrant and intelligent community around diabetes? look no farther than the Facebook page, the private Facebook page for the Juicebox Podcast. It's called Juicebox Podcast type one diabetes. The group has over 28,000 members. And those members are responsible for between 70 and 110 new posts every day, on the Facebook page. Every conceivable conversation around diabetes is happening at Juicebox Podcast, type one diabetes on Facebook, you're gonna see great questions, thoughtful answers, and supportive people. No matter if you're an adult living with type one diabetes, or the caregiver of someone with type one, this group is for you. Doesn't matter if you eat low carb, or high carb or somewhere in between your questions and thoughts are welcome on our Facebook page. I hope you check it out. Last little bit if you're looking for the diabetes Pro Tip series, or the defining diabetes series or any of the other multitude of series that exists within the podcast, you can find them in a number of ways. They are at juicebox podcast.com. They are at diabetes pro tip.com. And if you belong to the private Facebook group, you can find them listed in the featured tab. Now if you're enjoying the podcast, please consider sharing it with someone else that helps the podcast grow more than anything word of mouth is definitely how the show has become what it is. If you have already shared it with everybody you can think of and you've bought it on the pod or index comm or supported one of the other sponsors. You've done the T one D exchange survey. And now you're looking for another way to give back to the podcast. Super simple. A five star rating and a thoughtful review in whichever audio app you listen in would be amazing. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Test your knowledge of episode 755
1. How does physical activity impact blood sugar levels?
2. How should insulin doses be adjusted based on physical activity?
3. Which types of exercises are beneficial for diabetes management?
4. How should one prepare for exercise to avoid blood sugar fluctuations?
5. What is the role of consistent physical activity in long-term diabetes management?
6. How should blood sugar levels be monitored in relation to exercise?
7. How should low blood sugar episodes during exercise be handled?
8. What are the benefits of incorporating different types of physical activities, such as aerobic and anaerobic exercises?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!