#706 Bold Beginnings: Adult Diagnosis
Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 706 of the Juicebox Podcast.
Today is going to be the second installment of the bold beginning series. While you're listening to this episode, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin. If you're a US resident who has type one diabetes, or is the caregiver of someone with type one, please consider going to T one D exchange.org. Forward slash juicebox. To take the survey, the T one D exchange survey benefits people living with type one diabetes, it's incredibly easy to do and will take you fewer than 10 minutes, T one D exchange.org forward slash juicebox. Also, today, you're going to hear Jenny Smith, Jenny is a CDE. She has had type one diabetes for over 30 years. And she works at integrated diabetes.com If you're interested in learning more about what she does.
This episode of The Juicebox Podcast is sponsored by Ian pen from Medtronic diabetes in pen is an insulin pen that talks to an application on your smartphone and gives you much of the functionality that you will get from an insulin pump in Penn today.com. Today's show is also being sponsored by touched by type one, I need you to go to touched by type one.org. When you get there, go to the program's tab, click on annual conference and get your free tickets for the 2022 touched by type one Annual Conference, which will be held on August 27. in Orlando, Florida. I think last I heard, I'm going to be speaking, I think in three or four different sessions there. So come on out. Let's talk about some diabetes touched by type $1. Work. So Jenny, here are the questions that adults asked in the Facebook group. And that is, here's a statement. This one says that newly diagnosed those are often treated as type twos for a while, then we get tested and learn why nothing ever quite worked. I think a lot of should be more widely known about. So if you're diagnosed as an adult, I mean, Fair's fair, what I hear from most people is and it's, it's wrong, but doctors look at them. And if they look like they're reasonably in shape and fit, they think they have type one. And if they look like they're not they think they have type two, and it's very common to be to be stuck into a category without anybody.
Jennifer Smith, CDE 3:12
Correct. And that's in a I mean, what you just said is also in an environment with doctors who really are thinking type one thin, normal size looks, you know, like they maybe are an athlete or something like that. I'll actually say I mean, I've got a number of people that I've worked with over the years that are athletes, like I've worked with a couple endurance athletes who were initially misdiagnosed in the emergency department, as type two and sent home with completely a lack of information and a prescription for oral meds that were not going to do anything for them.
Scott Benner 3:54
Yeah. Yeah. You'd be surprised how many people I've spoken to who are dismissed at their diagnosis because the very next statement here on in our questions is, when I was first diagnosed as an adult, I couldn't get in to see an endo for a while because I wasn't quote unquote, critical and I wasn't hospitalized for DKA. And one of their first questions was, how do you even know I'm a type one. And you know, nobody does antibody testing right away for you. And this person says I just wish I would have known to ask for a C peptide test. When this was starting. It is not uncommon at all handful of metformin get home, take these come see us in a month, let us know how you're doing except you don't have type two diabetes. You have type one diabetes, and that's not going to help you. So and then you are in a real you're at a risk then a significant risk. Yeah.
Jennifer Smith, CDE 4:48
Yeah, absolutely. And I think that the issue there too, is adults. We're we're very misinformed when it comes to our education system. All right, we just we really are in terms of many health conditions, but diabetes included, there's still a lot of really good misinformation out there about diabetes. And so as adults, if you have all these symptoms, and you have no knowledge of diabetes, no personal history from family member or friend or anything, you may go to the doctors because you don't feel very good eventually. And then you get diagnosed, we are told your type two diabetes, well, maybe you don't even know there's type one diabetes, or you don't even know that you should ask to say, Well, gosh, this doesn't seem to be what I you know, what, what I would fit into for a diagnosis? I think so I think teaching is important. Yeah, it's
Scott Benner 5:48
important to know that you can be thin and lean and healthy and have type one or type two diabetes. Correct, right? I mean, and there's just so many in here, like I was diagnosed a month ago, at age 55, a week after my birthday. How was that possible? No one in my family has this. I was 50. My first question was, what the this person is obviously shocked. And then the next thing I want to get to, which I think is super important is, and I won't read the whole thing, but diagnosed at 47 years old, full time job, fast paced lifestyle. They can't get started, really, they don't know anybody that has diabetes, they're busy, they get up, they go to work, they're counting. They're I mean, people end up being hopeful, right? Like this person probably lived their whole life, you get sick, someone gives you a medication, you take two a day for seven days, you feel better. That's that, right? What you expect when this happens. And then when that's not the case, they say, look, it's almost five years later, I still struggle with my Basal with my Pre-Bolus times, this person doesn't know what they're doing. And so
Jennifer Smith, CDE 6:47
and I think a big thing of it goes a little further than not necessarily knowing what they're doing. One, I've found, definitely, that adults diagnosed with type one and absolutely with type two, are very poorly educated from the beginning, in terms of what to do, but along with that is they've already had a life and a schedule and a structure to that life, adding in something that they haven't been given the right information many times from the get go. And now they have to disrupt a lot to learn how to fit this in, to what their schedule was. Whereas kids are, they're different. I'm not saying that it's not difficult, but it's different, because who's helping the child
Scott Benner 7:43
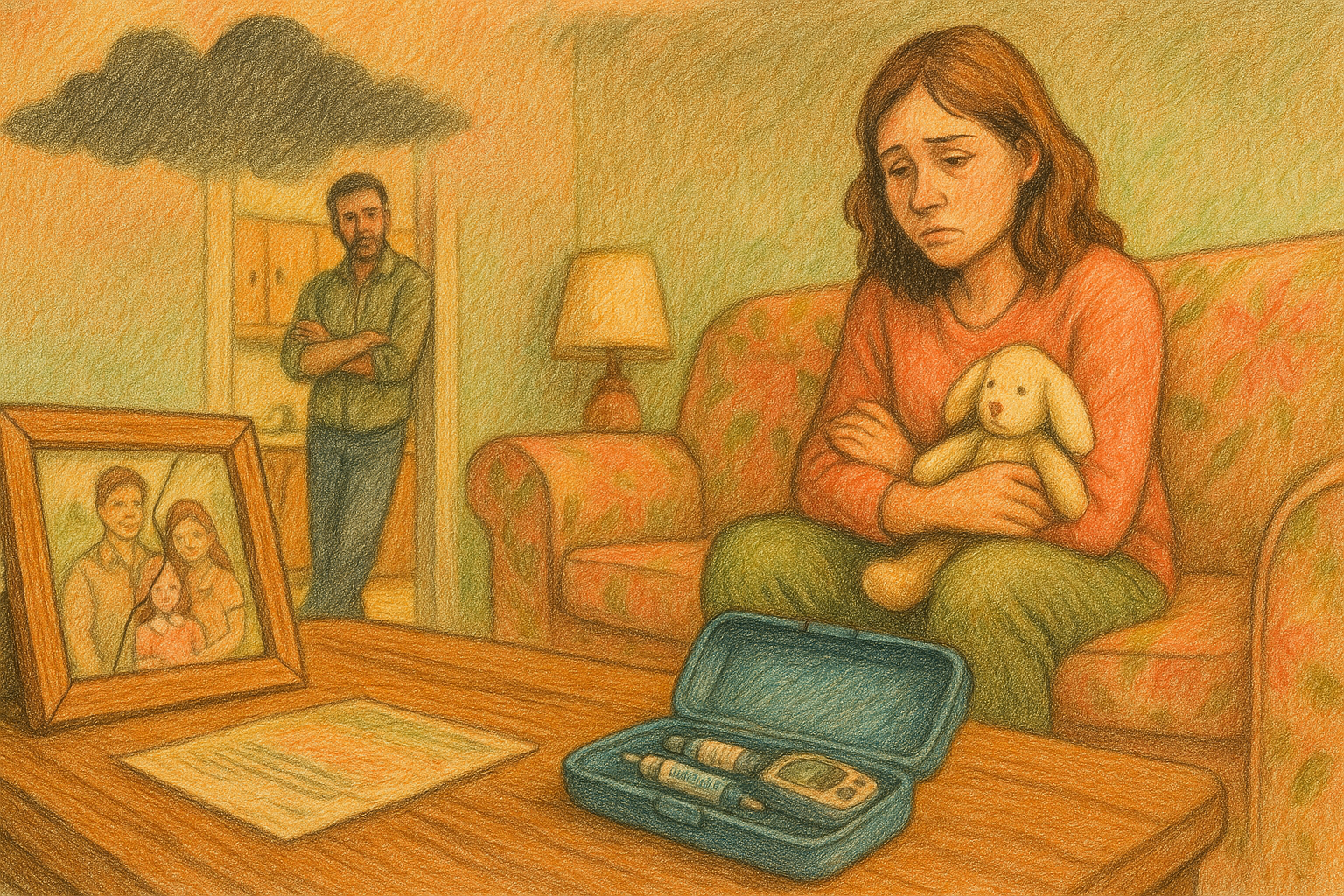
write it because when you're diagnosed as an adult, it's on you, it's on you. And when your diet when a child is diagnosed, some person I mean, hopefully, right? A caregiver basically stops the rest of their life to figure this thing out, because the diabetes is really a newborn baby, all of a sudden, correct can't help itself. If you don't know what you're doing yet. And it's a it's a very slow process and a scary process and, and a process where you feel like you're about to drop the baby every five seconds. And, you know, you just sit on the sofa. But, you know, it's funny to piggyback on what you just said, and the next question, somebody said that they got a ton of code, they got a ton of information in their education at the hospital, but none of it's happening in their real life. So what they, they felt like they left completely prepared,
Jennifer Smith, CDE 8:29
which is great to hear that yay for whoever educated you.
Scott Benner 8:35
And then there you go, you shop at home. And there's nothing there, the person actually said I had to start listening to the podcasts and reading posts in the Facebook group, but that they still feel out of control. You know, please do a show for older diagnosed people, a different issues like work pressure schedules, exercise, cycles, evening events, etc, etc, all these things, and it's very liquid. It's very true. I mean, Jenny, you know, like, if my daughter runs on a schedule, I can run her blood sugar, like it's nothing but if you start throwing in a bunch of different problems, ya know, and variables like this adult issues, it changes and I never go ahead and say that, you know, Sam, so no, I
Jennifer Smith, CDE 9:16
was gonna say you're AB you're absolutely right, adult issues are your own to manage to begin with, and many, thankfully, there are a good number of people who have a very supportive, significant other spouse, or a really good friend that, you know, gives them some support or help. I think one of the, not everybody has this option, but I've had a couple of people who've actually after diagnosis, they actually decided to do the best they could for themselves to really get an idea. They took one or two weeks off of work. And they said I am I'm just gonna I mean if I'm going to really nail understanding this as much as I can, and then I'm going to add this other variable back into the picture. I'm going to add work back. Now I'm going to add exercise back. It's but there are a lot of adults who don't have that option, you don't have the time you can take off. So you have to do diabetes, along with what was already in your life. And it adds a layer. I mean, I can say, as somebody who had had diabetes, long time before I had kids, adding kids into the picture has added a layer to my management that is very different than I did before.
Scott Benner 10:28
Yeah, I saw a woman walk out of an elevator yesterday with a libre on her arm, and she was lugging a baby, and had a four year old behind her. And I thought, oh, that's different than just walking off the elevator. It really is. You know, it's, there's this this next person said it this is very interesting, because I brought it up in the honeymoon episode for newly diagnosed but this person says, I thought I was doomed. I was in denial. And I spent days researching articles about potential cores, cures, excuse me supplements to prevent disease progression and everything. So they fell down a rabbit hole. Then they said they went into a depression, hopelessness. And on top of all that, blood sugar is all over the place. Yeah, yeah, let me keep reading, I kept calling my doctor when numbers didn't make sense. And they repeatedly told me it's okay, if you're 180 to 200 for a few hours after you eat, you're not damaging yourself unless this occurs for long term.
Today's episode of the podcast is sponsored by Ian pen from Medtronic diabetes. And I would like to tell you a little bit about it. The pen is an insulin pen. But it's not just an insulin pen. Yes, it has a cap. And yes, it has a needle and a cartridge and a little window where you can see how much you're dosing, little knob twist at the end and a button you push. It's an insulin pen, right, just like you expect. But here's the stuff you don't expect. How about an app on your cell phone that shows you reports easily shareable reports with data that is generated for up to 90 days in pen can do that because it's connected to that app by Bluetooth. The impact app is also going to give you an activity log. So you can see a list of recent actions including doses meals and glucose readings. Your active insulin remaining is right there on the screen. With that in pen app, see how much insulin is still working in your body. And in pen has a dosing calculator to help you take the guesswork out of dosing your insulin. The app uses your glucose levels, and a carbohydrate estimate to recommend the dose that's right for you. That sounds like a thing you get with an insulin pump. It even considers the amount of insulin that's still working in your body to help you avoid lows in Penn today.com. Forward slash juice box. One a digital logbook, in pen has that one carb counting support Oh, well, the pen app can help you estimate carbs based on your meal size. There's also a fixed dose option that allows you to choose the same carb amount for a specific meal each day. seems too good to be true. It isn't in pen today.com forward slash juice box, head over there now get started today. There are links in the show notes of your podcast player and links at juicebox podcast.com. To the in pen. And all of the sponsors of the Juicebox Podcast including touched by type one whose annual event is coming up in Orlando on August 27. And the Tickets are free. Did you hear that at the beginning of the show. Don't forget touched by type one dotwork. In Penn requires a prescription and settings from your healthcare provider, you must use proper settings and follow the instructions as directed, where you could experience high or low glucose levels for more safety information visit in Penn today.com.
Jennifer Smith, CDE 14:06
Right, but how do you stop it now? Like if it's occurring, and it's damaging long term? Well, then tell me what I should do. So I can stop it from happening long term. Yeah, excellent. Right. Like it's
Scott Benner 14:17
like, they feel like they're like, you could do a little math, you'll be alright. But that leads to a meth problem. Right, right. And it really is the same thing. Like I didn't I'm sorry, it's such an odd if anybody has a math problem, I'm so sorry. But like, I mean, it's just like, that's how it seems to me. It's just like, Absolutely, Hey, it's okay. Don't worry about it. But it's okay. Don't worry about we have so many episodes where people say, listen, they told me it was okay if I was up to 180. And then one day it was 190. And I thought well, that's only 10 More than one ad and then 200 was only 20 More and then 250 was only 50 More than 200 and I was okay with 200 Before you know it, blah blah, blah, blah, blah. Right and it's not it doesn't help you in this moment when here you On your house hopeless, alone, feeling depressed, unable to manage diabetes? I think the one of the, you know, I'll tell you a genuine I don't know if I would have said this five years ago, but having that Facebook page really teach me like you have to go find other people. Because for a little while, you need to know that other people live with this, and they do a good job.
Jennifer Smith, CDE 15:23
Because I was gonna do the same thing. Yeah, yeah, hope is incredibly
Scott Benner 15:27
important. And I'm not saying you got to go to some like type one retreat with people or something like that if you want to you can but but just knowing it I, I interviewed a girl this morning. I see if I can tell this really quickly. Last year I ever interviewed a girl from Canada who was allergic to insulin. i Yeah, figured it out. A doctor in Texas heard the podcast, she had a patient who was going through something similar. The doctor called me I put the doctor in touch with the person from Canada. conversations went back and forth. Long story short, the girl in Texas started using a Frezza. And she's doing much better now. During the conversation that I just had with her the girl from Texas, which is in the podcast summer, like go find I think it's called allergic dance on Park.
Jennifer Smith, CDE 16:20
All right. That's my alert that I should have turned off for going to pick my child up from the bus stop, which is not my job this afternoon. That
Scott Benner 16:29
kid can wait, Jenny, we're making a podcast. Wait, tell him to stand there a little longer, he'll be fine. But in the course of interviewing this girl from Texas, the mother spoke about how this is such a rare thing. But that she found a Facebook group with seven people in it who are allergic to insulin. And it was everything to her. Yeah, everything to find those other people, right. And I just think that it's not. For some people, it is not going to be intuitive to go look for other strangers and find comfort in them. But I am telling you, I've been doing this a long time. And not nearly as long as Jenny has been. And it's incredibly important.
Jennifer Smith, CDE 17:12
No I and I wouldn't 100% agree with that I would include for adults specifically too, don't be afraid to reach out for some type of mental health support to there's a lot that you have to navigate and it really helps to have somebody to even maybe help you get some structure or an idea of how to restructure things. I asked an adult as you said from a touch point, I I did not have diabetes friends, really, until I was an adult. I didn't. I had the people that I got to work with on a clinical bases. But I really didn't have anybody I connected with until I went to a diabetes like athletic training camp. Right.
Scott Benner 18:09
And you met people there
Jennifer Smith, CDE 18:10
and I met you it was it was like diabetes disney world to me. Everybody was beeping and buzzing and complaining about blood sugar's and how are you going to adjust before the five mile run? We're going to go on? I mean, it was I smiled the whole time that was there. Because it was exciting to connect.
Scott Benner 18:31
As as crazy as this might sound. I know this is a weird statement. But for you personally, if everyone in the world had type one diabetes, that would be better for you. You'd,
Jennifer Smith, CDE 18:43
right? I mean, the whole the whole world would just, it would just understand it wouldn't be a oh, well, you know, I'm gonna bring that special dessert for you because you have diabetes, kind of like the weird comments that you end up getting, right? No, just you don't understand. So sometimes that is even off putting for you as an adult to try to explain to somebody because there's so much missing that you can't explain in just five minutes of why you could actually eat the regular dessert if you wanted to. You just don't bother and you're by yourself. And then you're by yourself. And
Scott Benner 19:23
listen, I only have the context of a parent but I can tell you that when your child is diagnosed, you have no recourse you're not you know, I'm not I'm not I'm not dropping her in a in a basket or a fire station. She's my kid I'm gonna figure this out right
Jennifer Smith, CDE 19:36
she's not Moses you're not gonna let her go down the street
Scott Benner 19:42
I'm not very religious Jenny So I don't know that whole thing but it did pop into my head about should I say I didn't float it out or stream but I couldn't remember the whole parable. Anyway. The it slowly you understand it? And you don't you don't you give yourself over to it. It's a life change. As much as you won't want it to be at first, and you may do a really good job of giving diabetes, a lower impact in your life, but it's going to have one of the only, like, the only thing I can say is, you know, when you get a bad cold, and for three days, you just the world understands, you're going to lay down, you're going to be sick, and nobody's going to hear from you. And you find a way to make that time you do that when you're the parent of a child, you okay? Well, we're, you know, as an example, we were in the we had just renovated a portion of our home when our son was diagnosed, we'd done it, and we had it broken into two phases. For five years, while I learned about diabetes, my children had to jump out the front door, because I didn't have steps. And that is one, that's great. Yes, that is one of the things I put on the back burner, while we were figuring out diabetes, for Arden. And but when you're going to be an adult, and this is going to happen to you, there's no one there. I mean, maybe you have a spouse if you're lucky, right. But you'll be surprised at how many adults I see who try not to share their diabetes with spouses, which is a personal decision, you know, so you're going to have to say to yourself, I got to look at this 24 hour clock at this seven day, calendar this 30 day month, and find some time in here to just learn about this, and find a way to incorporate it because unlike a bad cold, it's not going away, but it will get you know, if I if I had something hopeful to say I would say that diabetes doesn't get easy. But sometimes you get so good at it that it can feel easy, some days. And those days sometimes grow into weeks, where you just go, oh, this was an All right, you know, you're gonna have to make that time in your life, you can't just put your head down and run through it, because it's not going to work that way. And you
Jennifer Smith, CDE 21:45
can start in from an adult perspective of a major change to your structure or your day schedule. Even if you just start with a basic of kids, then given this medicine called insulin, and I was told to take it, here. And here. If that's where you start, then that's That's it? Yes. Just take what you were told to take. And then moving on, you can kind of build on that. Especially if you've got technology, I would say that's another big one that adults should definitely ask about. I know, parents are definitely the ones to beat down knocked down camp outside the doctor's office until they get the products and the technology that they want. Adults do the same thing. Yeah, I asked for a CGM right away on diagnosis, you know, ask for a pump. And or start the discussion sooner than later, depending on you know, what you think you can handle
Scott Benner 22:46
to, to use a phrase from the podcast or something else, you should dictate the pace? Don't Don't let a doctor say, hey, we'll look at it three months back. No, no, let's do it. Now. You know, I want to get an insulin pump. Let's start that right now. I don't want to talk about it three months from now, you know, the other thing is, too, is you know, I tell people all the time, you might get a clunker of a doctor. Don't, don't don't suffer with it if that happens, right. And it's you know, I have a note here to myself, that children get treated better than adults do in medical situations. And it's because in my mind, it's a business. And if and if I see you treating my kid poorly, I don't want to come back here. So everyone's very nice and accommodating. It's how kids get treated adults, do not get treated that way. And by the way, if you are if your husband's a doctor, or your wife's a doctor, or you're a nurse, even if you're like you know, an OB nurse and know nothing about diabetes, your doctor is going to assume you know all about it. Yeah, and not tell you anything, because you're gonna think other nurse they know. And we know that's not true, too. So,
Jennifer Smith, CDE 23:55
in fact, in hiring my own Endo, or endos, you know, in over the past years as an adult on my own. I think since I've been in the profession of diabetes education. I've had more doctors who seem they seem almost standoffish, kind of scared to suggest and or talk about things. I'm usually the one to bring up the questions or hey, look at this. I'm thinking about this. What do you think about this? And I don't, I don't want that I'm paying you to help me. I don't want you just so you can write my prescriptions for
Scott Benner 24:36
me, I still need help with just a guy with a podcast. And every once in a while I get that I get the like, Well, what do you think I'm like, you saw what I think like that's the best I can do. What do you think? I'd love to hear what you think? Let's collaborate a little bit. It's it's not undoable. And I would I'd want to I'd want to finish this up by saying that I've interviewed you Dozens of people diagnosed in their 30s or 40s, their 50s and their 60s. And they're doing well. It's so possible to do. I would. I mean, listen, I'm biased. I'd find Juicebox Podcast type one diabetes, the private Facebook group and just lurk around and watch people talk. You can learn a lot that way. If you have a question great, if not just sit back and watch. And the Pro Tip series from the podcast that begins at Episode 210, with an episode called newly diagnosed or starting over, I think if you listen to the Pro Tip series that Jenny and I put together, it's absolutely free. I think you could get your a onesie into the sixes pretty comfortably. If you need any help find me and ask and I will absolutely ask. And if you're really, really lost, Jenny works at a place called Integrated diabetes, and it's at integrated diabetes.com. So you could
Jennifer Smith, CDE 25:48
thanks yeah, I was actually going to bring in the the fact that you've got a really wonderful list of endocrinologists. And I think there are even some diabetes educators within the list on the website on your website, right?
Scott Benner 26:01
juicebox, Doc's dot com.com Voc acids a list. It's curated by the people who listen to the podcast, who say that my doctor is cool with how I manage. I manage through, you know what I've heard on the podcast and you know, so other people can find them
Jennifer Smith, CDE 26:19
and you have some pretty good connections in a good majority of the states and bigger cities
Scott Benner 26:24
is getting bigger and bigger. It's not. It's not not worth your time to go check it out. You might find something near you for sure. Yeah. Okay. All right, Eddie, thank you so much. Thank you real quick when you get a dog.
Jennifer Smith, CDE 26:35
Oh, we've had a dog a long time.
Scott Benner 26:36
I know. I thought you have cats. Oh,
Jennifer Smith, CDE 26:39
well, we have a zoo. We have two kids. We've got a chocolate lab who's like 85 pounds. We've got two fish. We got two cats.
Scott Benner 26:48
I'm still recording, by the way, but I did not know your dog.
Jennifer Smith, CDE 26:51
Oh, yes. We've got more hair like floating around.
Scott Benner 26:56
That dog bark and I went, What the hell is Jenny dog sitting? I've never heard a dog barking all the time. I've talked to you.
Jennifer Smith, CDE 27:03
I know. Usually. In fact, I've heard your dog's bark before. And I'm I am surprised that in all the years he has not ever bar
Scott Benner 27:13
I swear to you, I thought you were dog sitting with that happen. I was like, although true.
Jennifer Smith, CDE 27:18
We often we most often do these more in the morning. And usually if we're getting deliveries, which I expect, probably something came and somebody knocked on the door, they usually come in the afternoon. So that could be why today
Scott Benner 27:33
you and I almost never do this in the afternoon, actually, that ever is the big deal. Sorry. Well, it's it's a holiday weekend. So I hope you have a great time. Thank you. New episodes of the bulk beginning series will come out every Friday. Thank you so much to Ian Penn from Medtronic diabetes, for sponsoring this episode of The Juicebox Podcast. Please remember to head over to in pen today.com. If you'd like to learn more about that insulin pen that talks to that app through Bluetooth. I'd like to remind you again about touched by type one, it's touched by type one.org. Of course, Jenny Smith works at integrated diabetes.com and bold beginnings episodes. And all of the episodes of The Juicebox Podcast are available at juicebox podcast.com. And in any one of your favorite audio apps, like Apple podcasts, Amazon, Music, Spotify, and stuff like that. If you need a list of apps that are free to use, by the way, I also have those at juicebox podcast.com, where you can head over to the private Facebook page for the Juicebox Podcast. It's called Juicebox Podcast type one diabetes. There are links there to all the series, tons of questions and answers from people living with diabetes, and links to audio players. If you're enjoying the podcast, please hit subscribe or follow in whatever audio player you're using right now. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Test your knowledge of episode 706
1. What is the main topic of Episode 706?
2. What common issue do newly diagnosed adults often face?
3. Why do some adults fail to get immediate testing for type 1 diabetes?
4. What type of test is often missed at diagnosis for adults with type 1 diabetes?
5. What advice is given to adults newly diagnosed with type 1 diabetes?
6. What did Scott and Jenny recommend about diabetes technology for adults?
7. What is a common feeling among newly diagnosed adults?
8. How can newly diagnosed adults find support?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#702 Bold Beginnings: Honeymooning
Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 702 of the Juicebox Podcast.
Today is the first episode in the bold beginnings series. While you're listening to this episode, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin. If you're a US resident who has type one diabetes, or is the caregiver of someone with type one, please consider going to T one D exchange.org. Forward slash juicebox. To take the survey, the T one D exchange survey benefits people living with type one diabetes, it's incredibly easy to do and will take you fewer than 10 minutes T one D exchange.org forward slash juicebox. Also today you're going to hear Jenny Smith. Jenny is a CDE. She has had type one diabetes for over 30 years. And she works at integrated diabetes.com If you're interested in learning more about what she does.
This episode of The Juicebox Podcast is sponsored by Ian pen from Medtronic diabetes in pen is an insulin pen that talks to an application on your smartphone and gives you much of the functionality that you will get from an insulin pump. In Penn today.com. The podcast is also sponsored today by us med. Don't just get your diabetes supplies from anywhere. Get them from us med Call today for your free benefits check 888-721-1514 Or you could just go to us med.com. Forward slash juicebox. Us men always provides 90 days worth of supplies, and they give you fast and free shipping us med.com forward slash juicebox. So we did this little episode recently where we talked about we're going to go through the steps of the questions that people sent in about being newly diagnosed. This is going to be our first episode about it. We have it broken down. It's not really it's still it's gonna be a lot of episodes, but we haven't broken down to honeymoon. What it's like to be diagnosis and adult. different terminology. highs and lows, the 1515 rule long acting insulin, fear of insulin, range and food choices Pre-Bolus ng carb guidelines and impact of food stalking, flexibility school exercise guilt, fear and hope. Podcast the community medical care team journaling, technology and supplies, insurance. And that's it. So that's it. That's it. I have it narrowed down to like I don't know, 15 or 20. Yeah, so we're gonna go through and have these conversations. So you and I put these in order, and we thought honeymooning went first. So we're gonna have to feel our way through this a little bit, because we've never done this before. In the past, I just started the conversation. And then we chatted to where we wanted it to go in the in the in the pro tips. But this one, we have questions from people. So why we thought this was important, is because going into the Facebook group with 25,000 people on it and asking them, What do you wish you would have known or someone would have told you when you were newly diagnosed? So under the heading of honeymoon, the first thing that we have here is a better explanation of the honeymoon phase would have been helpful. Let's talk about what that is.
Jennifer Smith, CDE 4:09
Yeah. Better is is a it's like a rabbit hole of consideration. Right, though, like, better explanation kind of starts with Well, how was it explained to the person or to the majority of people to begin with? Yeah, and I do think it's a concept that's really it's a gray area, have known, honestly. Because it's a time period, essentially, where after diagnosis, you've got some remaining beta cells, at least many people do. Not everybody but many people do. It seems like the sooner you get containment of the blood sugar levels, the more likely you are to have if there are remaining betas, their assistance and they come I'm back to help and that may eventually reduce your overall insulin needs. I mean by how much again, this is a person to person, you may need less overall dosing for mealtimes. Maybe just Basil is holding things really, you know, tight for you in that honeymoon phase. But I think a good word to go along with honeymoon is unpredictable. Honestly.
Scott Benner 5:29
So, the, you know, let me jump to another question, because I think it'll pull the conversation together, right? This person says mi honeymooning, how will I know. And I think that's such a good point. Because you really don't know what diabetes is to begin with. So whatever it is for you on day one is how you imagine it is and a lot of people get caught up in thinking, well, this is it. You know, and someone can tell you in the moment, hey, you might experience a honeymoon, and a honeymoon is going to be, you might have some beta cells that are still helping along with insulin production. That might be great. Because if it's stable, then we'll use you know, less insulin. But it also could wax and wane. It could be one day, you're getting help. And the next day, you're not the next day you are and you know, especially you're probably going to be MDI at that point, right. So you've got to for the most part, right, you've got a fixed amount of insulin in us a basil. And then one day, you're, you know, your pancreas is like, I'll help and no thanks. I already put the insulin in today, and you're feeding insulin all day. So it's a lot.
Jennifer Smith, CDE 6:34
It is a lot. And I think a misconception too, is that it shouldn't really be mistaken. And it could be easy to think, Well, gosh, maybe i i was incorrectly diagnosed. Right? Maybe I am really getting better. Maybe I was just sick or something was going on this downplay in insulin need. Especially being tested. I mean, most people who are who are diagnosed with type one, or assume type one, get the antibody testing and all those things that we've already talked about to to really give a positive diagnosis. But once that's there, even if your insulin needs go down in this expected honeymoon time period, you're not you're not getting better. And that's sad to say it is
Scott Benner 7:27
because it'll hit you that way. Because it happened to me. Yeah, there was a couple of days where art in just out of nowhere did not need insulin. And or at least that's how it felt like, you know, my memory on it could be, you know, right. I'm getting pretty old those long time ago. But right, my recollection is there were two days where Arden didn't need insulin, and I and I've told this story before calling our pediatrician who's a friend. And I preface what I said by going I know I'm wrong. But I have to say this because it feels imperative that I tell you that I don't think Arden has diabetes, somebody made a mistake. Right? And he sat very quiet and sad and said, she asked diabetes, this could happen. You should call the endo and talk to them. And I was like, okay. Yeah, but the problem day to day and why the question gets asked by people who are like, you know, when you ask somebody, what do you wish you knew? I think first of all, you need to know what could happen, you need to know it might not happen. Correct. You know, you might catch diabetes very early. And then your honeymoon might be longer, you might catch it later, it might be shorter, and 1000 other variables that could influence if there's a fluctuation, and if there is how big it is. This person says the lows were horrible. And we had a scary middle of the night, barely conscious, 32 blood sugar, about three weeks after diagnosis. So this is a person who didn't have this information was never told.
Jennifer Smith, CDE 8:51
Right. And that's I guess it also brings in a timeline of when, and that's a that's a major question that's also often asked is, well, how long can I expect this to last for? It could be a week, it could be a couple of days, it could be weeks, it could even be years. And for the most part, the years that length of time in honeymoon. I more often see in adults who are diagnosed who research has has shown as an adult diagnosed you more often have a reserve of betas after diagnosis that's a little bit larger than really young children or even kids or teens really. In fact, there's there are a lot of good studies for kids diagnosed under the age of five. I believe that actually so it's that the onset of type one is much more rapid and much more aggressive. And that there is more likely that there's less or almost no beta cell action left in really little kids were diagnosed very quickly. Yes, yeah.
Scott Benner 10:02
Artem was to and, you know, besides those two days, well, here's the rest of me right. Besides those two days, I'm going to tell you that I didn't notice. But I also was a guy holding the meter and a handful of syringes and a vial of insulin right? There were no CGM, I couldn't see anything happening. And these people who are listening very likely are not being handled a CGM right away either.
Jennifer Smith, CDE 10:26
Many of them are not I've had, in the past couple of months, I've had a handful of people who've actually left the hospital with a CGM on their child. Okay, well, that's fine. But again, that's it's a small percent, but it is encouraging to see how that's progressed in importance for visibility. And or they've left with a prescription to get it within a week or two after leaving the hospital or after diagnosis, which again, is, in my opinion, pretty quick turnaround,
Scott Benner 10:57
the context that the the glucose monitor line gives you, it's just, it's different. Because otherwise, in your mind, it just feels like the blood sugar is coming in and out of hyperspace. Like, it's you know, it's 78. And then the next time you look up, it's 250. And without context for how it got there, your brain struggles to make sense of it, you know, especially when it's very likely that the doctor has given you basic ideas of what to do count these carbs. Use this, you know, use this formula, inject this insulin, if you're lucky, you got that right information. Right. And because we're talking about newly diagnosed and not just children, I've interviewed a number of adults, you know, you know, over and over again, but lately, one that's sticking to my head where they just told her like your take 10 units of this and eat. Yeah, that was it, you know? Right, right, exactly. consideration about carbs or anything. Honestly, it's more
Jennifer Smith, CDE 11:55
than for adults, I've seen many more adults being diagnosed, let's say correctly with type one, but given more of a really old school, way to dose insulin, and prior to giving them any, you know, real information or education, if you will, it's like you said it's eat your meal, take 10 units of insulin, take it three times a day with each meal time and go about your business until you actually see an educator or somebody who can help adjust this for you. Where again, that's it's that's really old way to dose.
Scott Benner 12:34
But you're seeing it more and more you're saying.
US med takes over 800 private insurers and they accept Medicare nationwide. They have an A plus rating with the Better Business Bureau and they always provide 90 days worth of supplies. US med carries everything from insulin pumps and diabetes testing supplies to the latest and CGM like FreeStyle Libre two and Dexcom G six, better service and better cares what you're gonna get from us med head over there now to us med.com forward slash juice box or call 888-721-1514 To get your free benefits check. And to get started, you're gonna get white glove treatment at US med. They are the number one fastest growing tandem distributor nationwide, the number one specialty distributor for Omni pod dash. They're where we get our hands on the pod five suppliers from they also are the number one distributor for FreeStyle Libre systems nationwide, and the number one rated distributor index com customer service satisfaction surveys. Come on us med.com forward slash juicebox. Everybody gets your diabetes supplies from somewhere. And everybody knows how much of a pain it can be. US med says they're gonna give you better service and better care than what you're accustomed to. Today's episode of the podcast is sponsored by Ian pen from Medtronic diabetes. And I would like to tell you a little bit about it. The pen is an insulin pen, but it's not just an insulin pen. Yes, it has a cap. And yes, it has a needle and a cartridge and a little window where you can see how much you're dosing. little knob twist at the end and a button you push. It's an insulin pen, right just like you expect. But here's the stuff you don't expect. How about an app on your cell phone that shows you reports easily shareable reports with data that is generated for up to 90 days in pen can do that because it's connected to that app by Bluetooth. The impact app is also going to give you an activity log so you can see a list of recent actions including doses meals and glucose readings. Your active insulin remaining is right there on the screen. With that in pen app, see how much insulin is still working in your body. And in Penn has a dosing calculator to help you take the guesswork out of dosing your insulin. The app uses your glucose levels and a carbohydrate estimate to recommend the dose that's right for you. That sounds like a thing you get with an insulin pump. It even considers the amount of insulin that's still working in your body to help you avoid lows in pen today.com. Forward slash juicebox. Want a digital logbook, in pen has that one carb counting support Oh, well, the pen app can help you estimate carvers based on your meal size. There's also a fixed dose option that allows you to choose the same carb amount for a specific meal each day seems too good to be true. It isn't in pen today.com forward slash juice box, head over there now get started today. There are links in the show notes of your podcast player, and links at juicebox podcast.com. To the in pen, US Med and all of the sponsors of the Juicebox Podcast when you click the links you're supporting the show. In Penn requires a prescription and settings from your health care provider, you must use proper settings and follow the instructions as directed, where you could experience high or low glucose levels for more safety information visit in Penn today.com. Yeah,
Jennifer Smith, CDE 16:41
I see it, I see it often enough that it sort of frightens me, given all the technology we have today. And the types of insulin we have today and the way that they are meant to work to specifically especially our rapid acting insulins to mimic sort of digestion for the food that it was formulated to cover which is carbohydrate. So why don't we just educate people? Well, give me an idea what your meals look like. I mean, this is pretty easy question to ask people upon diagnosis, okay, your meal seemed to be this. And as an educated clinician, you should really have an idea about how to carb count, especially if you are in the profession of diabetes. And that's you should be able to say okay, let's start easy and just say, for every 15, you take one, right, at least
Scott Benner 17:36
it gives people context,
Jennifer Smith, CDE 17:38
something's starting to work with a starting point, even if it's completely wrong, and they need to be a one to five, at least, then in a couple of days, you can say, well, that's clearly not working, let's adjust it, but they already have the concept of counting and dosage.
Scott Benner 17:52
Your, your your story makes me think that maybe at diagnosis, people are like, well, they're gonna get great technology. And then now this is going to matter. So I'll just say something that won't kill them today, then they can go to the next person, and the next person will do a better job of this. But your point is, I mean, listen, it's not a brag, but I think you could bring me up to any person using insulin. And I think I could probably ask them four or five questions and make a pretty educated guess about how to cover their meal. Yes. So absolutely. Yes, it just doesn't it's not I hate to say it's not that hard. But you know, it shouldn't be if you're a clinician, I guess. Just this next thing here says, What do I need to know, during the honeymoon stage, you really have to put yourself in the position of a person who's just been whacked over the head with a shovel while someone's yelling, you have diabetes. And they're like, wait, what she's she said before they teach carb counting. Like when do I know if it's a true DKA? Or hold on a second? These are broken up questions. So let's skip the car panic and go. When do I know if it's a true DKA situation are just part of the honeymoon stage? What do you think they mean by that?
Jennifer Smith, CDE 19:01
Well, high blood? It's a good question. Because if high blood sugars are just sustained high,
Scott Benner 19:07
and then they again, do ketones because somebody told them if you're over this for a certain amount of time test your ketones, right. And they're fresh from a traumatic moment in their life where these kids had or they had a high blood pressure and they were in the hospital for it. Right. Oh, I see. Okay.
Jennifer Smith, CDE 19:22
I mean, that's what I that's what I would certainly expect but it is it's a it's a good question. But I think it's a pretty complex question. Because if you're in this window where honeymoon could be the case, and all of a sudden you're running high blood sugars, okay, great. Go ahead, do the steps. You know, test for ketones. dose, call your call your doctor and say, Hey, we've been running higher all of a sudden, it seems like without visible illness or stress or anything in the picture. Seems like you're likely at that point then coming out of honeymoon and you actually need To increase your doses, potentially basil to start, maybe the doses that are covering mealtimes, especially if they've been very, very, very conservative. But I mean with high blood sugars, regardless of what point of diabetes diagnosis you're in, if it's a stain high test for ketones, right, good first step.
Scott Benner 20:20
You know, it's funny, I always think about these things, all these topics about I think of them as like, if we were in an elevator for three minutes, and you said to me, Scott, honeymooning, what do I do? I think, and I don't want to give away that I've watched more than one season of Big Brother, which I'm embarrassed by, but I think you have to expect the unexpected. Like, if Thank you, if you just need to live in the in the reality for a little while, that things are going to change more frequently. Or they could change more frequently, I should say. Then you hope and right. And that's where you hear people online, say stuff that I don't like that they say, but I understand where it comes from, like, you know, carbs, times this plus this equals elephant, you know, or when they say like, nothing makes any sense, right. But if you expect it to be varied, then it does make sense, but it's varied. Right, you know, if you if you put yourself in a position where you say, This is what should be happening, I did what the doctor told me, I measured it correctly. This is wrong. None of this makes sense. I give up. You're gonna, you're gonna make yourself crazy. Right? Yeah, you just have to stay very flexible in the beginning.
Jennifer Smith, CDE 21:29
And I think that the flexibility and especially in terms of what people should know, after diagnosis around honeymooning is that expect that it may be in the picture for you at some point, sooner than later after diagnosis. And that once you're exiting the honeymoon, it doesn't necessarily mean that you're doing anything wrong. Right? This isn't it's not really, it's not your fault, that you're coming out of the honeymoon time period that you need more insulin. It is what it is. Yeah. So I mean, there's a lot of, I mean, in the grand scheme of diabetes management, there's like, a lot of psychological stuff anyway. But I think this is a, this is a period where you may feel really, really confident. And honestly, during a honeymoon time period, it may seem a lot easier for some people because they have these really tiny insulin doses is they're only on basil. They feel like oh my gosh, I'm an eating and checking my blood sugar looks like it's in this target range. And they may not even be dosing mealtime insulin, maybe Basil is just cutting it for them, right? And then it starts to inch and creep and change. And that's where again, like that psychological piece of management kind of comes in, because a lot of people think, well, well, maybe I need to cut back. Maybe I'm doing too much, maybe I'm eating too much. So I'll just eat iceberg lettuce. And that means it's okay.
Scott Benner 23:04
It's such a good point that in the beginning, you're very likely using such a small amount of insulin and it can make you feel like I've got this it's so easy. But if your Basal is point one an hour, and you know your whole meal, insulin is like a unit for a meal or something like that, like, I'm not belittling, it's hard, and it's scary and everything else. But you're basically playing wiffle ball in the backyard with your dad, you're not hitting up a Clayton Kershaw right now, yeah, go crazy. When you put the ball over the hedge line, you know, they may just say, okay, and to me, it's all experiences. I mean, I don't know how many times I could talk about it, but you have to do a thing. You have to see how the thing works out. And then you decide, do I need a little more, a little less, a little sooner? A little later? How does this insulin work? And you do it again, and again and again, until one day, it just makes sense every time you do it? And? And the truth is, is that, you know, in the beginning, you do have more going against us than just understanding that you have the other parts, the psychological aspects of it, and what could really be, you could be suffering with depression at that point, or, you know, there's a lot happening. I interviewed an adult recently, she's in her mid 30s. And she said they were explaining to her about her diabetes, and she just sat there thinking I don't have diabetes. Like she wasn't listening to anybody. You know, she's like, a young fit person. And she's like, I don't this is wrong. Like she couldn't get past the I think they're wrong about this. You don't know how many important things were said to you. While you were staring at the wall thinking, hey, what was wrong? Yeah, what the hell just happened to us? Yeah. Okay. Yeah. Is there anything here we're missing? I do want to go to one more question here. But I want to make sure you have everything out that you want to say.
Jennifer Smith, CDE 24:49
Um, I don't. I don't think so. I mean, outside of just one other question that I think has come up in conversation in discussing with some newly diagnosed people that I've worked with, a lot of people end up asking, is there anything that can sustain this honeymoon? Right? And there's, there's only one study that I know of, and it was done in adult men. So not even a broad spectrum of, you know, gender or anything. But it showed that exercise in newly diagnosed men proved that the honeymoon lasted a fair amount of time longer than those who didn't include exercise in that time period post diagnosis.
Scott Benner 25:40
I wonder why that is. So
Jennifer Smith, CDE 25:43
again, I mean, something like that, certainly, you need to study it in more people more, you know, kids, teens, women, but at least it was a good visual that there is that one thing that was shown that could potentially prolong it, and I would, I would expect, it's just from a sensitization standpoint, right building muscle making the muscles work, which makes your insulin work better. And if your body is more sensitive, your pancreas also doesn't have to work as long so maybe it preserves the beta cells longer, right would be my expectation
Scott Benner 26:17
what let's put this part in here to like, so we know about like Tomislav, for example. Right. There's that drug trial. Yeah, about a long gating people's honeymoons? What's the real benefit of that? For the patient? Beyond that you don't need to use insulin, and you don't have to have diabetes, as soon like, I mean, the lesson to think of put off three, four years, then hey, you know, I'm saying, that's amazing. But if I'm just doing something that's going to extend my honeymoon by a week, or a month or two, like, what's the real benefit of that? Is there one?
Jennifer Smith, CDE 26:50
I guess the benefit to me especially would be for if it's even keeping people from some type of diagnosis, you know, in those who are tested with antibodies and are given the drug in order to extend the time without diabetes, any years without diabetes are definitely a benefit.
Scott Benner 27:10
I get that one I'm talking about, like, if running around like a lunatic makes it take three less. Like, if it gives you three weeks back, you know what I mean? Like, like, you've had diabetes for over 30 years? Yes. Would it be any different if you had it for three weeks less? No, no, right. But I would not, but three, three years less, God bless we would like that. Right.
Jennifer Smith, CDE 27:33
Absolutely. Three years less. Absolutely. And, you know, from the standpoint of ease to the body and whatnot, I think more information needs to be gathered as to people who were diagnosed without use of something like this. What type of outcome with control, like healthy management long term? What was their end outcome compared to people who got the use of this drug and had an extended let's call it honeymoon time, where their body was allowed to help them a little bit more. They had to use less injection, less pumped insulin less, right? What did that bring in down the road? Did it improve anything down the road? And that's going to take years to look at differences
Scott Benner 28:26
from I think, from my perspective, from a person who talks to a lot of people. When I hear about people wringing their hands about honeymooning what I really hear from them, mostly, they just wanted to stop. They just they just like, can we just get to the part where this is reasonably predictable? Please? Like, like, what what is happening, Jenny?
Jennifer Smith, CDE 28:46
I don't know. That's not me. It sounds like you're getting a weather. Emergency weather alert.
Scott Benner 28:51
Maybe a tornado here. Oh, great. Now live, you're gonna ever hear this episode? Scott, he's on his way up.
Jennifer Smith, CDE 29:01
I was gonna say do you need to go to the basement? I don't live
Scott Benner 29:03
in that kind of an area. This is the kind of an area where people go like, why don't we get these tornado alerts. But But, but to go back to my thought that was very odd. They just, I mean, listen, if it's a situation where one day your kid can go to baseball practice and the next day, they can't because one day the pancreas isn't doing anything and the next day it is. It's it's it makes you nuts. Like it just does. And I you mostly hear people say I just want to get to the next part at this point. All right. And I don't you know, I don't not understand that. I think but but this person asked this last question that says they're talking about a two year old who overnight is experiencing lows with no insulin at all. And they say he can hover at 90 for hours and then slowly creep down to 70. But here's the thing. Isn't this interesting? If Jenny's blood sugar would hover it 90 For hours overnight, and then slowly creep down to 70. She would text me in the morning, a picture of her CGM ago, look how good I am at this. And that's the thing you don't have context for when you're looking at your two year old baby who's had diabetes for two months. Right? That, you know,
Jennifer Smith, CDE 30:19
there's not enough history to it for it, this example, this family, this person, there's not enough. I, I have a sense of, of what that means to me. I also have a sense, if I got an alert overnight, and I saw what was happening. Even without using the system that I'm using previous to this, I would have a strategy that I 99% of the time would have worked, right to say, Okay, it's drifting, this is happening, this is what I need to do, or I can go back to bed, because I know that it's all gonna be totally fine. Right? So knew there are, there are a lot of kids, especially kids that I work with, who are still using multiple daily injections or MDI. Because once that Basal injection is there, you can't take it away.
Scott Benner 31:09
Yeah, this is an example from someone who obviously pumps because they were able to turn their basil off off, right? If they were MDI, they would continue to get low. It's funny, yes, I just was explained to somebody the other day, a person who just doesn't know anything about diabetes, and we're talking about low blood sugars. And they said, Why does it keep getting low? And I said, well, the insulin is dumb, it doesn't know. I think that the insulin is pulling glucose out of your blood, pulling it out, pulling it out, pulling it out, it doesn't get to a number and say, Oh, good, we're done. It just, it will continue to take glucose out of your blood until the power of the insulin is gone. And it doesn't care that you are where you want to be too low, having a seizure doesn't matter, it's going to does taking
Jennifer Smith, CDE 31:52
correct. And that's, you know, on pumpers if it was happening enough, again, in this particular example, you could say okay, well, this has happened night after night, I've had to turn the basil off. But if you've got a pump, you can program it just program is zero basil from this point of drop to this point of leveling out and and take care of it. You know, but on again, injections, it's it's really difficult. And so often, what we end up having to do is really make sure that the morning is when the Basal is adjusted, assuming that the overnight lows in this case, and assuming it's honeymoon in this case, is the pancreas is just kicking out at this point. Yeah, this is where it's taking most of its action. And so you don't need any injected or pumped insulin here, because your body is helping.
Scott Benner 32:39
And then the last question that people constantly ask is, How do I know when it's over? And yeah, that one's easy, because you need a lot more insulin,
Jennifer Smith, CDE 32:48
your insulin needs go up. And it's again, this is a visible Okay, was it today because it was a birthday party or a cookout or something? And so we just had a lot more that was different, or is it ongoing in the next? Okay, this was today, tomorrow looks similar. The next day, it looks similar By day three of needing more insulin and nothing else has really shifted or changed. You're probably getting to that point of honeymoon is ending
Scott Benner 33:15
experience after experience day after day showing the same thing. Yeah, you're probably not being helped by your pancreas anymore. The other thing too, is I don't want to be like ham fisted about it. But you know, when you have type one diabetes, and you're not getting any help from your, uh, you know, the way I used to explain it to one of my daughter's teachers when they wouldn't understand I said, Look, here's Arden right now, her blood sugar is perfect. If I take this pump for her, take it from her, just she got no more insulin, and we give her a half a bite of this cookie. She's going to be dead in four days. And you're like, I'm laying there like what? And I'm like, Yeah, her blood sugar is going to continue to rise and there is nothing her body can do about it. I said it will put it into decay, it will end her life a bite of this cookie without insulin. And so you can see it. When you don't have insulin, your blood sugar wants to go up. And if you you know if you can, you know, if you have some stability, say you are using a CGM and you have some stability at 120 and then you eat something and you know, you Bolus for it and three hours later, you're 120 Still but then it keeps rising and keeps rising and keeps rising. Your Basil is probably not strong enough. And then you need to probably go over and listen to the pro tip episodes about how to get going and taking care of your blood sugar. So alright, did we do it? Is this good?
Jennifer Smith, CDE 34:29
I think this is pretty good. Yeah,
Scott Benner 34:31
I you know, every time we do this, I wait for you to look at me and go, Dude, you're so wrong. Stop talking.
Jennifer Smith, CDE 34:38
I don't think I've ever said that to you.
Scott Benner 34:40
You just keep there's that little kid inside of me. It's like I'm gonna mess up eventually. And Jenny's gonna be like shaking her head at me and be like, What are you talking about? Stop but I think
Jennifer Smith, CDE 34:48
the only one time that I did correct you is when you told me that I wasn't nurse and I'm like, Yeah, I'm not a nurse, dietitian.
Scott Benner 34:55
I misspoke and there's the truth right now. We're still recording she would stop me if you I misspoke one time in how many years have we been doing this together? Oh my god, you're like, I'm not a nurse. Oh my god, I felt like I was married to you for a second. I was like, Oh, she finally got me he's so excited
new episodes of the bold beginning series will come out every Friday. Thank you so much to Ian pen from Medtronic diabetes, for sponsoring this episode of The Juicebox Podcast. Please remember to head over to Ian pen today.com. If you'd like to learn more about that insulin pen that talks to that app, through Bluetooth, I also want to thank you s Med, and remind you that you can get a free benefits check right now at us med.com forward slash juice box or by dialing 888-721-1514.
It would be a great companion to these episodes to become a member of the private Facebook group. For the Juicebox Podcast. It's absolutely free. But it's a private group so that you can feel comfortable speaking openly with other people who are living in a similar situation as you it's called Juicebox Podcast type one diabetes, you'll just have to answer a couple of questions to prove to that Facebook algorithm that you're a real person, and then you'll go right in to a space with over 25,000 members. There's so much activity on that Facebook page every day, there's bound to be a conversation. That's about something you've wondered about something you're experiencing, or something that you know enough about to help someone else with Juicebox Podcast, type one diabetes on Facebook, in that same group, at the feature tab at the top, you'll see lists of other series of the Juicebox Podcast, like the diabetes pro tip episodes that have been mentioned, or the defining diabetes series, which will also be mentioned here. If we haven't already, everything you need to know is it juicebox podcast.com are right there in that private Facebook group Juicebox Podcast type on diabetes. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. Let me just remind you again, before we go that Jenny works at integrated diabetes.com If you're interested in hiring her, she's interested in helping you. Also, for US residents, T one D exchange.org Ford slash juice box, it really is a valuable thing for you to do to complete that survey. And it genuinely helps people with type one diabetes, and it supports the Juicebox Podcast. So if you can spend just 10 minutes today taking that survey, I would just greatly appreciate it t one D exchange.org. Forward slash juicebox. I've seen listeners of the podcast be involved in a number of different trials around diabetes, they got the opportunity from the T one D exchange. The one that comes to mind right now is that there was one person involved in a new adhesive study for the Dexcom G six. But there are many other opportunities. So beyond answering the questions in the survey and helping people with type one by lending your your data to the T one D exchange and I don't mean like super personal stuff. I mean simple questions about type one diabetes, which by the way, are HIPAA compliant and anonymous. Anyway, by by answering those questions in the survey, you will also give yourself the opportunity to hear about trials and studies. T one D exchange.org forward slash juicebox
Test your knowledge of episode 702
1. What is the main topic discussed in Episode 702?
2. What is the purpose of the Bold Beginnings series?
3. How many topics are covered in the Bold Beginnings series?
4. Who is Jenny Smith?
5. What is the honeymoon phase in type 1 diabetes?
6. What can influence the duration of the honeymoon phase?
7. What is a common misconception about the honeymoon phase?
8. How should you manage insulin during the honeymoon phase?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#698 Defining Bold Beginnings
Jenny and Scott lay out the newest series on the podcast. Bold Beginnings will answer the questions that most people have after a type 1 diabetes diagnosis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 698 of the Juicebox Podcast.
Today's show is going to be slightly different. Jenny and I are discussing the next series that's coming up on the podcast the series is going to be called Bold beginnings. And it's based on listener feedback. In this episode, you're going to hear me tell Jenny the idea that I had explained to her about the feedback that I got from the audience. And then we take the big ideas from the feedback, almost like bullet points, we go over them, put them in an order we want to record in and talk about them as we go. So basically, you're going to listen to a meeting that Jenny and I had about the next series of the podcasts, but think of it more like a trailer, and extended trailer for a new series. While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin.
This episode of The Juicebox Podcast is sponsored by Ian pen from Medtronic diabetes, find out more and get started today with the M pen at in pen today.com. The podcast is also sponsored by us med us med is a place where you can get your diabetes supplies, and US med wants you to have better service and better care than you're accustomed to get yourself a free benefits check right now at us med.com forward slash juice box or by calling 888-721-1514. If you're a US resident who has type one diabetes, or is the caregiver of someone with type one, please go to T one D exchange.org. Forward slash juicebox. Join the registry, take the survey, it will take you fewer than 10 minutes. When you do this. When you complete the survey, you'll be helping people with type one diabetes and supporting the Juicebox Podcast. The survey is fast. It's easy. There's nothing on there. You don't know the answer to it's HIPAA compliant. And absolutely anonymous, T one D exchange.org. Ford slash juicebox. I have an idea for today. So, in you'll so we're recording already. So if you say no, it's fine. We'll just not do it. But okay, I don't think you're gonna say no,
Unknown Speaker 2:58
I usually don't. Well, you're
Scott Benner 2:59
Yes, you don't usually. So far, you haven't said no. I've said some weird things. But once or twice, you've been okay with it. So I had this idea a couple of months ago. And I kept thinking, again, the private Facebook group is just a font of information, because you can see what people are thinking. Right? Sure. And then eventually, if you see people think the same thing over and over and over again, you think to yourself, Well, this must be a question a lot of people have. So I, I put this question out. And I said, What do you wish you would have known at diagnosis. And what I got back, turned out to be an 80 page Word document full of information. Now, Isabel has gone through and she's taken out, like duplicate questions and things. I was gonna ask how much was duplicate? Not as much as you would think when you hear AVP. But but a fair amount was was duplicate stuff. And she broke and she broke it down into into sections, like put people's questions into, you know, under headers. And I was thinking that we should do individual episodes based on those headers. Sure, and then combine the episodes together in a series. You know, I don't know what I'll call it yet. But it'll be something about questions that newly diagnosed people have, like frequently asked questions of newly diagnosed type ones or something like that.
Jennifer Smith, CDE 4:27
Yeah, I'm curious how did since you've read through all 80 pages, or you're like, Oh, this is 80 pages. That's a lot.
Scott Benner 4:37
I've been making my way through section by section.
Jennifer Smith, CDE 4:41
And because I'm curious if some of the questions are. Gosh, I really would have liked to know this because definitely right up front. This would have been super, super duper beneficial. Whereas some questions may be, well, gosh, this would have been Nice to know upfront, but it's a little bit more. I know you say like ninja level, right? It's a little bit more down the road, definitely you would use this, but you're not going to use this two days from diagnosis
Scott Benner 5:13
and see the way you're thinking about it is the way I was thinking about it. And so what I what I thought was, if we take each header and almost handle it, like it's an ask Scott and Jenny episode. Sure, right. And then and then go through them have conversations, why does my voice break only with you? You don't might be because we're on Mondays.
Jennifer Smith, CDE 5:35
That could be I was actually gonna say if my voice today is very scratchy. I actually canceled clients like two days last week, because I had laryngitis
Scott Benner 5:44
No kidding. Oh, why don't want to talk?
Jennifer Smith, CDE 5:49
No, no, no, no, I think I'm definitely better. My voice is not like, weird, not there for five minutes. So yeah,
Scott Benner 5:56
so what I thought was, and this is good for your situation, is I just want to talk through the document with you. But we're gonna, we're gonna record it. So I sent you an email, which will open up into your apple notes.
Unknown Speaker 6:12
Okay. Let's see, we'll go to my email and see where your email is.
Scott Benner 6:21
I just think that conversationally is the only way to work through all this. Because otherwise, you know, what most people would do, who are creating content for diabetes, they read these, they choose a handful of questions. And they turn it into some bulleted point less than they put a, you know, two sentences after each one. But I think that, when we're talking about it, the length of time that we decide to talk about a question, usually is pretty accurate to answering the question. So some of the most part, I mean, I think we do a good, I think we do a good job of seeing the big picture when we hear people's questions, I guess, is what I'm saying. So do you have my email? I don't really know. Second,
Jennifer Smith, CDE 7:10
do you not talk a lot on weekends? Is that why you are saying that? Maybe it's because it's Mondays that your voice cracks a
Scott Benner 7:16
lot? I don't talk as much over the weekend. My wife would disagree with that, I imagine. But I don't think I do not nearly as much as I mean, I record this show. I mean, the last couple of months have been crazy. I've been recording like five times a week. So I talk a lot a lot. Yeah. And then I put ads on things. I probably I probably sit and talk directly for 10 hours a week. Just like constantly talking. There are times when my throat feels sore. It's not It's unpleasant. Okay, did the tag
Jennifer Smith, CDE 7:47
I'm right there with you. I talk all week as well. Sometimes at the end of my like, really long days, which are Mondays and Fridays. I get done. I have to like, take a couple breaths before I like walk out of my office space because two children like they just they want you know, they want like, Oh, now can I talk to you and you know, kids my age have no inner monologue whatsoever. And it just all comes out. And I'm like, Oh my gosh, Mommy needs quiet tie with a bubble bath.
Scott Benner 8:19
I'm in a mood right now. If you want to know how to Pre-Bolus a bagel, that's all I can tell you at this moment. Does your head does your head gets swimming. afterwards. Mine does. Yeah, the if I sit down and do a talk, like for hours, or even when I'm the one of the reasons I don't like people to look at me when I'm recording with them is because I stare at a spot on the desk bond accessing what I understand about diabetes like and I just I talk like
Jennifer Smith, CDE 8:43
plugging yourself into a file, right? Yeah, here's my file. I'm gonna connect to it. I download everything I needed for this circumstance. And then you unplug. Yeah, I do
Scott Benner 8:53
wonder if people don't understand, like people who don't do this would understand that. It's just, there's a there's a, uh, I don't know, a lake, a damned off lake full of information in my head. And if you get me to open it up, I can just let it out. But if you but if you ask me right off the cuff, I'd be like, Oh, hold on a second. So you're saying this happened. But once I started talking about it, it just if it just comes out smoothly, so know why that is?
Jennifer Smith, CDE 9:21
And that's kind of sometimes the reason that I get a little bit thrown off when people who are not in my diabetes world, whether it's friends with diabetes, or people I'm working with or colleagues like you or whatever, the general public without diabetes, when they ask you these very random questions. I have to be very careful about how I start talking about something because like you said, I will go off and then you get the glassy I look like deer in the headlights like this really, I didn't want and all this information. shin and I feel like you're speaking like alien language to me.
Scott Benner 10:05
I find in that scenario, my explanations are are so childish and simple, that if the next thing I said to them was, I have a very popular podcast about diabetes, they think I wonder why? Because I just I'm like, oh, yeah, she's fine. Right. Hasn't outgrown it yet. Right. Yeah. You know, that's not, hey, you know, what, forget it. Like, you know, so it's just, I don't know, I don't get too deep in it. Otherwise, and just like you're saying, I'll just start to talk. Right? And then
Jennifer Smith, CDE 10:40
I don't when I get going, yeah. It's, it's, it's hard to like find the end point, right?
Scott Benner 10:46
No, because there's because the explanation. And I think I mean, to bring it back around to this is the explanation is always conversational, I'm starting to believe that that's sort of why it's harder for doctors, because, because they're in that they fall in that same category as a person writing a blog about it, which is, I have about 350 words here. Before I lose people, and I run out of time, and or whatever the reason, I gotta get it out, I gotta get out succinctly. And this stuff's not generally speaking, not cut and dry. You know? No, you need the big conversation.
Jennifer Smith, CDE 11:24
So well. And I think that's why the conversational learning, as you do is very helpful to many people, because they're already in the realm of something that they are trying to understand, or they understand because they're living it, when you're trying to have a conversation with somebody who doesn't live in the diabetes world, and or has no connection from family or a friend or whatever. The conversation becomes very one sided, you become whether you wanted to or not, you become the educator, right? And then it's less of a conversation and more of a tutorial. And it's not a fun conversation.
Scott Benner 12:04
Right? No, no. and the Self Editing that happens, whether it's by the doctor, or someone writing a blog, is you know that you get to a point you Oh, I don't want to tell them that because they might misunderstand. Or, you know, I wouldn't want anybody's blood sugar to get to like, you know, to think I don't want anybody's blood sugar to get too low. The way I think of that specific thing is people's blood sugar's get too low, all over the world using insulin, but most of them don't know who I am, and will never hear this podcast, right. But if we give them enough information, they maybe could stop it from happening. And I would prefer for them to have a chance than then to not have a chance it it almost feels like a I don't know, it feels like an action movie to me. Like, you know, we've got to jump over this lava. If right, if we don't, the monsters gonna eat us, right? Well, we might as well jump and see what happens, right? Maybe we'll make it over the lava. And that's sort of how I think about this, like you should have the opportunity to succeed. It's not going to work out right for everyone. Or it might take longer or shorter for some people, but not telling everybody so that some people don't fall into the lava. Does that make sense to me because everyone's gonna get eaten by the monster. Correct. That's just
Jennifer Smith, CDE 13:23
and at some point, somebody's going to be ready enough to jump. Maybe they weren't when you first gave them the information. But if you gave it to them, at some point, they're likely going to try to use some tidbit that you provide it right. They'll
Scott Benner 13:38
have this recollection, they'll think oh, you know, I listened to that. Like, again, I I swear I didn't bring this up on purpose. But this idea of talking about these people's questions after being diagnosed, you can listen to these, and maybe maybe three months from now, you'll say to yourself, Oh, I remember someone said that in this thing. I could go back and look again, I could maybe just go with my recollection. But isn't that better than them being blindsided by it? Another great example, I think, is that this morning, in the Facebook page, someone someone's kid had a seizure, their their Dexcom was I don't know if it was in. If it was starting up, they didn't have access to their Dexcom data for a little while. kid had a seizure. She grabbed the G voc hypo pen, she stopped the seizure. She took the kid to the hospital. He's recuperating. Now, my point is, is that she did it like, like you should see her recollection of it. She had the information about what to do. It's not it's not this harried like, oh, it's not the Scarlett O'Hara post where she's like it. The world's happening to me again, you know, come pray. She's not asking for prayers. She's like saying, Look, this thing happened. It sucked. And we took care of it. And here he is. He's fine. And right and i thought i I was proud of that, like, I wish it wouldn't happen to the kid. But I mean, as a person whose child's had a seizure, it can happen, you know what can
Jennifer Smith, CDE 15:08
happen, right? And I think another another thing that you bring in there without really saying it is that, in this circumstance, the parent didn't get emotional, the parent was rational. They said, This is what's happening. This is what I have to do about it. And this is the next step. And that's what you have to do. I mean, if I had a t shirt that says, said, anything, it would be be calm and think like Spock, it would like seriously, if you just all of these things that you learn along the way, many of them are very just rational, do it decision, right? Don't emotion, don't put emotion into it. Because despite there being feelings about diabetes, and how cruddy it can be to manage things at times, and whatever. A lot of its decision that is, right now, this is what I have to do.
Scott Benner 16:02
And someone brought it up to me recently, and I'm gonna have to look into it more because it keeps popping back into my head. They talked about thinking like an astronaut, because everything that an astronaut comes up through is trying to kill them. Right? So when everything that you say you put it in order, like this one's gonna get me first we'll take care of this, then that one, then that one is the seventh thing, the 70 a thing on that list gonna kill me. It might.
Jennifer Smith, CDE 16:29
But but if I clear up one through 69, it might not it
Scott Benner 16:33
might not. And maybe it will something will change or whatever. And I just, I don't know. I think about life that way. Honestly, not just diabetes. So you know, whatever's our most emergent problem. It took me years to explain to my wife that my to do list was fluid. Like she would write it for she'd write it to do list she'd like you didn't do number one yet. I'd be like, well, number six is on fire. So I can't get one through five doc before six burns the house down. I'm gonna have to move the list around a little bit. It's, it's one of the reasons I enjoy making the podcast by myself. And not because people are like you, you could get an assistant or you should do this or what about an editor? And I was like, huh, I don't know. I like, I like the way I think about it. You know? So anyway, did you get my text? 20?
Jennifer Smith, CDE 17:21
Yes, that's right here. I thought I said yes, it came through perfectly fine, and was enjoying our conversation. It's, it's probably the longest text message that I have in. But I should say it's the longest texted note. As I have. No,
Scott Benner 17:38
did it open in your notes? Yes. Okay.
Unknown Speaker 17:40
It opened in my notes now.
Scott Benner 17:41
Yes. It's all good. Well, trust me, it's the longest one I've ever seen either. So scrolling through it, she's got it broken down to carb guidelines and impact of food. This is Isabel who took care of this she's, which is a pretty long list. It is then there's stalking, range, food choices Pre-Bolus Sing the 1515 rule. Fear of insulin highs and lows. Isabel, you did such a nice job of this honeymoon, terminology, flexibility, guilt, fears and hope expectations. And I'm still scrolling. Wow, that's that's a long one. About the podcast and the community around the podcast, medical team. Holy Hannah, technology and diabetes supplies Jenny, I'm gonna need you to quit your job. So we can do this. And insurance and insurance, long acting insulin exercise, journaling. That's interesting school being diagnosed as an adult, family, extra topics and then stuff that she's
Unknown Speaker 18:57
wasn't relevant to that that
Scott Benner 18:58
she didn't find would be relevant to this idea.
Jennifer Smith, CDE 19:02
Or maybe they didn't fit into a category. So I mean, they might be things that we can look through and see if there
Scott Benner 19:07
Yeah, and the rest will call that at some point if we get to it.
Jennifer Smith, CDE 19:12
So now my brain like I did when we first did the pro tips, like we need to rearrange this listing, right? I would probably go through this and list them out according to what I think would be really important first newly diagnosed really go here first and then next year and next year kinds of thing.
Scott Benner 19:36
I was hoping you would think about it. Honestly.
Jennifer Smith, CDE 19:39
I mean things like a medical team, and
Scott Benner 19:52
you ordered diabetes supplies. And if you're like me, you may have been using a place that made you want to reach up with your hands and Grab your hair and urine couldn't read out of your head because it was very frustrating. Or they say things like, well contact your doctor, you don't have to worry about it, then you had to worry about it because they never contacted your doctor. If this sounds familiar, and you're tired of that, I was almost like crap. But now I said it anyway. So if you're tired of that, I suggest you check out us med. US med accepts Medicare nationwide in over 800 private insurers. They carry everything from your insulin pumps to diabetes testing supplies, and the latest CGM. They always provide you with 90 days worth of supplies, and they have fast and free shipping. US med likes to say that they want you to have better service and better care than you're accustomed to today. Why not give us metta shot, they have an A plus rating with the Better Business Bureau. And they've served over 1 million diabetes customers since 1996. Us mad.com forward slash juicebox. That's the place you get your free benefits check. You could also do it at 888-721-1514. Get yourself some white glove treatment. Instead of that treatment that you're accustomed to. Oh, we'll call your doctor for you take care of the whole thing. There's nothing for you to think about bowls. You know what I mean? Us med.com forward slash Juicebox. Podcast is also sponsored today by Ian Penn from Medtronic diabetes, you might want to know more about it. And if you do want to know more, you're in luck, because Google's God is here to tell you about it. The in pen is a is a pen. It's a it's an insulin pen. I thought that was you know, it's an insulin pen. It's an insulin pen, but it's so much more because it connects to an app on your phone. This app gives you access to a dosing calculator, dosing reminders, card counting support a digital logbook, many of the features that people with insulin pumps get. So if you're looking for some of the features that you can get with an insulin pump, like you know how much insulin is active in your system. If that's something you want, you should look into the NPN. There's also an offer on the internet. Now you have to have, let me just say you have to here's I'll read it to you, instead of me just fumbling through the words, this offer is available to people with commercial insurance and Terms and Conditions apply, right? But you may be able to pay as little as $35 for an in pen, which is crazy. Medtronic diabetes does not want costs to be a roadblock to you getting access to the therapy you need. So go check out in pen today.com a great device, I think you're gonna really enjoy it. There's not much to lose here. So go ahead and check it out. There are links in the show notes of your podcast player, and links at juicebox podcast.com. To end Penn, US Med and all of the sponsors, including a link to where you can take the survey for the T 1d Exchange. Check it out, please support the sponsors. When you do you're supporting the show. I really appreciate it. I'm gonna get you back now to my conversation with Jenny, as we talked about bold beginnings. In Penn requires a prescription and settings from your health care provider, you must use proper settings and follow the instructions as directed. But you could experience high or low glucose levels for more safety information visit in Penn today.com.
Jennifer Smith, CDE 23:49
Maybe even food choices before like the carbs and the carb effect kind of thing. I think that the 1515 rule could definitely go along with the lows and the highs, I think can be kind of included together. Gosh, there's so much in here honeymoon definitely up at the top. I think that honeymoon is really poorly explained from the get go. And it's almost like a skirted over sort of comment. That's not explained very well. And so people get lost in whether it's going to happen or it's happening or how to know what's happening or what to do about it. You know what I mean?
Scott Benner 24:34
Yeah, okay, well, let's, let's do this together now. Okay. Okay. So I'm, you tell me and I'll put them up at the top.
Jennifer Smith, CDE 24:44
Well, I would definitely say honeymooning would be a good first, because that's going to mean for the most part. Within a very quick time post diagnosis. If honeymoon is going to happen, that's where it's going to end. happen. So that would be probably first. And then I'm kind of curious, you know, terminology is almost like the defining, yeah, diabetes. Right. So terminology, these are really good. Maybe just the ones pacifically post diagnosis that would be very important to have information about. So I would say, right along with honeymooning the terminology,
Scott Benner 25:30
okay. I have it there. I am putting him in your order.
Jennifer Smith, CDE 25:35
And then I don't know, I'm kind of like the medical team, I think could maybe be laughed before we move into like a little bit deeper. But I'm wondering like the highs and lows, especially, because there's a fair amount in the fears around highs and lows. And then specifically the 1515 rule. I don't know how many people post diagnosis I get to talk to who specifically asked about that. So clearly, this rule is still being taught. Yeah,
Scott Benner 26:09
exactly. And it's, and it's, and it becomes obvious to people pretty quickly that it doesn't make sense. And then they get stuck. Frustrated. Yeah.
Jennifer Smith, CDE 26:19
Yes. So I would definitely say that. Mmm hmm. I think right along with is there's one about insulin in here. And I think it might even be able to be included around fear of insulin is the Pre-Bolus thing. And I the reason I put it in there is I, I think because from the get go if people aren't taught about timing, you do start to fear insulin. Yeah. Because it seems because it's erratic. Exactly. So I would say, you know, within that 1515 rule, the fear of insulin lows and highs explanation of insulin, and then moving into Pre-Bolus Singh. And I think Pre-Bolus Singh could then move more so into wondering like curb impact, because they kind of go hand in hand.
Unknown Speaker 27:23
There are so many categories here.
Unknown Speaker 27:28
What about what about stalking?
Scott Benner 27:32
Well, stalking is going to be
Jennifer Smith, CDE 27:38
I mean, that kind of goes along with fear of insulin. It goes
Scott Benner 27:41
along with everything. It goes along with, right 1515 It goes along with fear of insulin Pre-Bolus thing you ever have somebody ever have somebody asked you. I had dinner, and I Pre-Bolus. And then I had seconds, what should I do? And it's fascinating. They don't, they're stuck. They're like, I've never had a meal inside of a meal before. What goes on? I can't just Bolus again. And it's funny, because in my mind, I'm like, well, you're taking in more carbs. Why not? You know, and then the I think that what they think is, well, that's so much insulin. And I just put in someone they might be thinking about stalking without ever having been told the word because because it seems like too much to them.
Jennifer Smith, CDE 28:27
And I think the real definition of stalking too in there, or a better definition of stalking, because what you're talking about, in a way it's stacking, but it's not stacking without purpose, right. You know, everything that you eat is going to require insulin, right. And it goes back to the timing of the insulin. And also now that we have wonderful technology, like a CGM. What's your CGM telling you? Yeah. Are you stable? Are you already rising? Are you falling? Are you low falling? Right.
Scott Benner 29:03
So this this lady posted a graph the other day, and it was a 12 hour graph was beautiful. And there was like, I don't know, she took the kid out for waffles and ice cream or something like that in there. And she said something like that her her child had like 250 carbs in this giant like, you know, food. Right?
Unknown Speaker 29:27
That's a lot of food. Holy cow, right?
Scott Benner 29:29
I was like, Wow, no kidding. But she you should have saw the line. And and it was it was so it was so flat. And then everybody comes in and their first thought is that's so many carbs. That's so much insulin. How much insulin was was a smaller kid right. And and she says it was like it was over time I think 17 units she used over out the kid didn't like horsepower. Yeah, this this happen, like stages over a couple of hours. hours. And I kind of chuckled to myself when I read it. Because if Arden has a carb heavy meal, she could use 17 units for a meal. And sure, it's a lot like, you know, I'm not saying it's not, but it's not a lot for that food. It's just it was interesting that people's, that their first thing isn't, Wow, you did that? How can I do that? It was, it was back to their preconceived notions about things. That seems like a lot of carbs, that seems like a lot of insulin. It seems like you know, and, and that's all relative to begin with 17 units. I mean, listen, if you if you had, you know, if you had type one, and you weighed 350 pounds, you might be used in 17 units to move a number, you know, like, like, there's all different reasons why the numbers should be. The numbers are what they are. You know, if Arden goes out has nachos with cheese steak on it, and french fries, you know, we're somewhere near 17 to 20 units. It's you know, because for the fat and everything, there's a lot you know,
Jennifer Smith, CDE 31:04
I don't think I've ever taken a 17 unit bowl. Oh, my
Scott Benner 31:08
like, yeah, well. You eat like a healthy bird.
Jennifer Smith, CDE 31:16
I don't know. I you know, even growing up though, I had definite high insulin needs as a teen. I all teens do. But yeah, I don't know, maybe it was more just from the standpoint that I also started in a very different school of thought and education than we have today. Yeah. I mean, I actually I went to my mom's on Saturday with my boys just for an early Mother's Day. And she's been trying to like do some cleaning and whatnot. And so you know, for my brother and I, she kept really organized files, like every report card we ever had. All of these things. Well, I found in there a scrapbook that I had, at some point put together after my diagnosis with all of my cards, all of my mylar balloons taped into this scrapbook and everything. And I found three of my hospital menus with my choices during that week. You kept all of
Unknown Speaker 32:14
that. I didn't my mother. This is my mom. Yes, this is what she does. But it was snowing.
Jennifer Smith, CDE 32:23
Yes. But it was amazing to me. And in terms of this, that I had a very structured plan that was based on portions and the insulin that went along with it. There wasn't as much variety or variability. And that's just not how my mom did it either. I'm sure other people probably at that time may have. It's just everything was very structured.
Scott Benner 32:50
It makes clear what the technology wasn't there to track anything you did. I mean, if you started if you try to eat 250 carbs back then you would have I mean, you would have been high. I don't see another way. Oh, yeah, your blood sugar would have been high forever. I think that's why some of the the old time he type ones in those group, see, see that? And it fries their mind? Yeah, you know, like you can't do that is always there. I wish the internet was audio. So that because I think you can't do that. In typing, you know, typed out doesn't mean the same thing is how it would sound like, you know, it sounds. It sounds like a direction typed out. You can't do that you're not allowed to do that. What I think they really mean is holy hell, you can't do that. Right. Yes, that's not gonna work. But, but I mean, it does it just, I mean, it does, you know, and again,
Jennifer Smith, CDE 33:44
it goes along with timing of insulin and when to put it in and what you're seeing again, our technology today allows you to do some of these types of things. As long as you're paying attention.
Scott Benner 33:57
Yeah, right. Right. So all right. So we got some stacking fits in there. So right now have honeymooning terminology highs lows 1515 Rule fear of insulin lows and highs Pre-Bolus thing carbon pack stacking
Unknown Speaker 34:14
and then I think I would put do we put food choices somewhere in there? Not yet.
Unknown Speaker 34:24
Um,
Scott Benner 34:26
sort of has to go before Pre-Bolus and doesn't Pre-Bolus
Jennifer Smith, CDE 34:29
thing? Yeah, I would put it in definitely before Pre-Bolus. And then I'm wondering if I was just reading range. I'm assuming we're talking about glucose ranges here.
Scott Benner 34:48
Let me look. Next, make sure I see it the way you said. What range to be out or shoot for. How being 200 for weeks is okay as the body adjusts. But to taper down to More realistic unhealthy range, that it may take a while to normalize blood sugars that have been happening. So it's kind of a broad it is. Yeah,
Jennifer Smith, CDE 35:10
I would probably break it down to range based on what's considered healthy range, what's considered a normal range outside of having diabetes, what is the human body typically aim for. And then I would move into range that might even include things like safe ranges for activity and safe ranges for illness and range that you might hear from your medical providers versus what you're really trying to aim for. Along with, where should your glucose be? What should your target be? Fasting first thing in the morning? What should it be? Or what should you expect after meals? All those things, I think, fit within range.
Scott Benner 36:01
Well, we could do it as as one episode, and just break it up within the episode, right?
Jennifer Smith, CDE 36:10
Yes. And I think I'd I'd move into then definitely, maybe even terminology. And there's one in here that's about I think, the medical care team, right? Because I think they they all in a way go together and medical care team in terms of ranges alone, or they're going to have a very similar range for everybody. They're just going to give you your their blanket statement. You should be here. That your alarms here. Yeah,
Scott Benner 36:44
they're gonna say whatever the ADA said last right. For the most part, 70 to 180 right now is that the numbers,
Jennifer Smith, CDE 36:51
that's the numbers right now, I mean, even even most of the CGM does have that set as their default in terms of data collection 70 to 180, unless you go into your own settings, and actually physically adjust them to see your cumulative information that's scaled to your target range. And again, a lot of people don't even realize that they can do that within their, you know, software, data analysis, like clarity or whatnot. But then even discussing within the medical kind of piece, how to pick a medical team how to ask questions within the medical team, I mean, I'm assuming some of these are the questions within that medical.
Scott Benner 37:32
So what if we didn't worry? What if we put these in order, which we're doing now? Then after we have it in order, then I will apply a topic to every one of our recording dates coming up? Perfect. And then we can be read ahead? And then just sit down when it's time to record and, and have the conversation? Were actually well planned? Jenny, what do you think of that?
Unknown Speaker 38:01
That's a great idea.
Scott Benner 38:04
Listen, I'm gonna tell you, we don't
Jennifer Smith, CDE 38:06
usually ever in fact, we never do. I never know what we're talking about until we click in together and I like gardening. And you're like, let's talk about this today.
Scott Benner 38:14
I'm gonna tell you right now that one of the things about the Pro Tip series that I'm most proud of is just that, that it really is. I mean, we made a bullet pointed list. And then we said the topic out loud and then did what we did. And it's been so valuable for people. I think this is going to do something similar. Now, here's a question for you. This is more of a pocket podcast question. But I'm interested in your opinion. Do we just make this part of the Pro Tip series? Like remember, I said, I wanted to go back and revisit the pro tip episodes. Right? Maybe this is going to do that?
Jennifer Smith, CDE 38:52
It may, it may do enough of that. I think the pro tips are I don't know what the longest pro tip episode was maybe an hour.
Scott Benner 39:01
Yeah, there might be one that's more like our 15 or something like that. But pretty, pretty close to that.
Jennifer Smith, CDE 39:06
Because I think those were very, very specific. And while we talk and veer off and whatever within our conversations, I think if I were to do it, I might actually put this as a pro tip, category, pro tips for newly diagnosed and then put these all up definitely as pro tips, but these are the things within here. If you are newly diagnosed, go here and if there are additional questions based on one specific topic, maybe go to the regular pro tips and look up that you know what I mean?
Scott Benner 39:51
Yeah, no, I do. That's a good idea. All right. So I'm still I'm still pulling topics and bringing I'm up top so that I can see them. So you know, there a lot of Yeah, hold on a second so Okay, so we have still flexibility, medical care team guilt, fears, and hope X and hope expectations, podcast community family journey school journaling, exercise, long acting insulin. I know that when, after the after the topics came back, so I eventually close the thread and I was like, Okay, this is enough. I'm good thanks. And it was very generous of people to come in and spend time but giving real clear explanations of the things that were confusing to them or that they found helpful, etc, right. And then I put it all into this Word document. And I was like, I don't know what to do with this, you know, so I didn't have time. And I thought this is such an asset. I don't want to lose it. But I was like, I don't know what to do with this. And Isabelle said, I'll go through it. And I said, thank you very much. And weeks, took her weeks to like, you know,
Unknown Speaker 41:15
I'm sure. A lot of information 80 pages is no joke.
Scott Benner 41:19
No. And so she went all through it. And I thought, it's a lot. And most people wouldn't put this effort into their content. And I think that's why it's gonna be good. You know? Yeah. So it's even why I'm not scared to discuss it here with you. I mean, honestly, this episode is going to serve as sort of like a primer to let people know what's coming. They probably, they probably won't hear this, too. We have a number of these recorded already, I'll probably put out first get them ready to that it's coming. But there was a there's a voice in my head that says, Don't let people hear you and Jenny talk about this, because they're gonna rip you off. Because that does happen. Jenny, I put up content. And then a week later, everybody's, somebody else has to talk about the same thing like, oh, wow, what a surprise. And but I don't care. Because I think, I think first of all, I think the effort we'll put into, it won't be matched by anyone else. And the information, you know, I would hold up against what anybody else could come up with. And, and the other thing is, I just don't think that this is how, I don't think people put this kind of effort into stuff. I just don't, you know, even going all the way back to the Pro Tip series, like the amount of hours that we spent recording that stuff. You know, a lot. Yeah, and you you know, we say this all the time, but you don't work for me, like you're not getting paid to do that, like, you know, where are you gonna get somebody with your knowledge, and your understanding of how to explain things, and an ability to talk to me because you and I, like, we get along really well. And we vibe off of each other, but we're not similar. Like, you know, it just it just works, you know? And you're not gonna get that so I think we can do this. I think this will be terrific. No, this is really great. Yeah. Okay. So does it repopulate when I move words, do you see it happen right away?
Unknown Speaker 43:08
I see it happen on my screen. Okay. Okay,
Scott Benner 43:11
so you saw me misspell a word. That's embarrassing. Nevermind.
Jennifer Smith, CDE 43:15
Actually, I was gonna ask you what? You had the word long after exercise. And I was like, what else goes along with that? I don't know what long means long time without insulin long time
Scott Benner 43:27
to scroll to make sure we have them all. So I mean, there it is. Right? It's, it's, I think that's everything. I'm gonna go back down and go through it when we're actually you stay up there where the list is. And I'll scroll through and tell you what's here. You can tell me if we have it up top or not. Extra topics. I'm not worried about that right now. Family is family up there. Family is up there. Yep. Being diagnosed as an adult. I don't remember typing
Unknown Speaker 43:57
that is not up there. No,
Scott Benner 43:59
can you add it and we can rename these topics because you know, Isabel's first language isn't English. Oh really? She's French.
Unknown Speaker 44:13
Oh, that's you did tell me Yeah.
Scott Benner 44:14
And I only said that so when she hears this she'll she'll be mad at me for saying that. school.
Unknown Speaker 44:23
School is in there
Scott Benner 44:24
journaling yep exercise. Yes long acting insulin. Yes. Technology and diabetes supplies that's out there. I can add that okay. And then insurance which I know I didn't put up there either. Insurance and the medical team Yes. Yes. Did someone add did I add podcast and community? Yes. While this topic so long I can't get the The header what is it going to be? I'm still scrolling.
Unknown Speaker 45:05
I think the long one.
Scott Benner 45:06
It's guilt fears, hope and expectations is incredibly long. That's here. Okay, there's probably the reason for that is likely going to be that there are a lot of personal anecdotes in here, which took people log in to type out. I'm gonna,
Jennifer Smith, CDE 45:19
I wouldn't expect so to and some of that, you know, we'll go through these obviously ahead of time, but I would expect some of the things within that, especially the fears may be addressed within the other topics,
Scott Benner 45:33
right? Yeah. Yeah, I don't think we're gonna I don't believe that we're gonna have to go through these, these and read everyone's thoughts and answer them. I think I think the way I see this happening is that we prepare by reading them make our own couple of notes, and then we can have a bigger conversation around that and interject people's thoughts when they when they build on everything. Flexibility is up there terminology is up there honeymoon is fear events on lows and highs 1515 Pre-Bolus. thing I'm getting close to the top. Food Choices, range stalking. Carb guidelines and impact of food. Carbon pack gifts,
Jennifer Smith, CDE 46:23
is current guidelines and actual
Scott Benner 46:27
I think that's a topic Yeah. All carbs isn't a topic, better education on how insulin works with specific food groups would have been beneficial.
Unknown Speaker 46:35
The hospitals there's there's curb impact is that the headaches?
Scott Benner 46:41
But hold on a second, you typed it in
Unknown Speaker 46:42
here already?
Scott Benner 46:45
I see what you're saying. You're saying it's possible that I, I shortened it. And I should have wrote that. So I'm gonna put that in there. And I'll change that. Yeah, because this is really interesting. The hospital made it seem very black and white. You eat X carbs, you take this much insulin and go on with your life. Another person said the impact of food nutrition component on blood sugars. Why isn't her blood sugar tracking the same for breakfast day after day, even with meticulous carb counting? You're right, a lot of these are going to be able to like we're going to be able to give an explanation and then point somebody to a different episode to wait where they'll be able to be helped counting carbs as a huge stressor for us easy ways to count carbs and how different things hit you differently would have been great. Yeah, so basically, these last three statements sort of say the same sort of say the same thing. So okay, great. But my point is, is that the luck of having such a large group of people, one of the things that's great about it, is that this is, um, this isn't just a random person saying something now, like we have consensus,
Jennifer Smith, CDE 47:56
this is a pool. This is a pool of you know, I mean, if you were doing like a research project, you would have a lot of participants. Yeah, right. Our research wouldn't be n of 10, which then the general information about like a study like that is like 10 people great, but the world has how many billion people in it right? And now many of them have diabetes. So how relevant is this, but this is a very good yeah, amount of people comments
Scott Benner 48:22
right now, I think this is so be good. And then some people go into more detail, my biggest frustration is that at first they send you home and tell you that your child can only eat carbs during the three main meals. They talk about free snacks outside of it. So you spend hours researching free snacks and loads of money buying them. And then two weeks later in class, they say oh, by the way, she can have carbs whenever she wants just those for it. Here's your new chart, even if they just said we want you to wait a couple of weeks, but at this point will teach tricks and I say okay, yeah, this is this is gonna be good. All right. I'm excited. This is cool. This is what I was hoping would happen. You're up for it. So yay. Do we want to try this last couple of minutes we have do you want to try to put the rest of them in order or?
Jennifer Smith, CDE 49:10
Sure let's see so we have order already for Honeywell and terminology highs lows kind of all the insolence sort of together. I think maybe within the insulin we should also put probably
Unknown Speaker 49:32
let's see highs and lows
Jennifer Smith, CDE 49:33
I think should also maybe be Where's range because the highs and lows kind of go along with range. Okay, so right. So maybe highs and lows and then range. Alright, that's all together.
Scott Benner 49:51
Got it. I feel like guilt fear, hope expectations, podcasts and community Isn't last, like, towards the end may be correct those things so I'm gonna chop those out and put them down lower. Make some space here. I think flexibility is a huge part of it. To be honest. I honestly think your medical team is towards the end newly diagnosed people are not going to break away from a from a new medical team. If it's a bad one, they're not going to even know. Right away. Right? So Correct. Maybe put that more towards the end as well. Oh, great. All right. And long acting insulin could just
Jennifer Smith, CDE 50:40
think long acting needs to be around the well EV around that fears of insulin lows and highs. Because you can also define rapid acting insulin within that even though it wasn't a question asked. I think it's going to be a piece of that fear of insulin.
Scott Benner 50:58
I put it before because I can see myself talking a lot about basil in there. And correct. I just think that basil gets ignored by everybody does. Yeah.
Jennifer Smith, CDE 51:08
It gets ignored by everybody. Except it's the first place that most clinical people adjust first. Yeah, they just don't. Some are Basal here. Yeah. Hi, here. Let's just put some more Basal insulin here. Yeah, probably not. But
Scott Benner 51:23
I put I'm starting to work backwards. I put journaling and family towards the end. Correct? Sure. And so I'm going to put towards the end, we can rejigger these as we need to technology and supplies. That one,
Unknown Speaker 51:38
I might put that with maybe before after insurance before or after insurance. Okay.
Scott Benner 51:43
Being diagnosed as an adult.
Jennifer Smith, CDE 51:50
Um, that might actually, I'm wondering if that wouldn't be too bad to put after honeymoon.
Scott Benner 51:56
Yeah, so that everybody can feel like they're a part of the of the series as it comes out. Right.
Jennifer Smith, CDE 52:02
Right. And because being diagnosed as an adult, you may actually have a more pronounced honeymoon, you may have more of a real honeymoon, depending on how you learn to manage things from the get go. So I think that's good there.
Scott Benner 52:19
And then we left flexibility school and exercising. So I, I would think, I'd like to put flexibility, at least in front of I think flexibility and stalking, right? Yeah, right before guilt and fears might be valuable. Correct. School and exercise. So now schools interesting, because I haven't read them yet. But I'm gonna guess that a lot of these questions were about, hey, how do I just send my kid to school five minutes after they have diabetes. So I don't know about that. And exercise is kind of the same thing. You see people get sedentary after they're diagnosed, because they don't know what to do.
Jennifer Smith, CDE 53:06
Well, I think school and exercise there's something some of these are as well, but they're more visible variables. School is a variable exercising is a variable. So
Unknown Speaker 53:25
choices, maybe,
Jennifer Smith, CDE 53:27
maybe right after school and exercise, or right after flexibility, put school and exercising. Because those both really do require some flexibility in what your typical management style would look like. So
Scott Benner 53:48
you see what I'm doing now? Um, yes, I'm gonna put them in an easier to look at. format. All right, well, this should keep us busy.
Jennifer Smith, CDE 54:03
Along with all the other things that you had us, like scheduled out for the rest of the year, right?
Scott Benner 54:09
I'm gonna, I'm going to, I'm going to put an end to ask Scott and Jenny because the thing about those are, that are great as they can just go somewhere. They're really valuable. They don't need to be attached to anything else. They're great standalone episodes. Right? So I'm going to so basically, at the moment I have I have about three ask Scott and Jenny episodes, a couple more defining episodes, so I'll put up the defining things till they're done. Then I'll put up I'll put up the ask Scott and Jenny's while we're recording these, and then when they ask Scott and Jenny's run out, we should have enough of these to get going. Okay, that makes sense. Fabulous. Right? Neither of us can get sick or get a life.
Jennifer Smith, CDE 54:56
I will promise to try not to get laryngitis again. Yes.
Scott Benner 55:00
Sometimes I look at I was, I was getting ready to go under for my, for my surgery. And I said to my wife, if something should happen, hire an editor. I have like 70 episodes of the podcast that need to go up. I was actually, like, concerned or worried no one would ever hear them, you know. So. Anyway, all right. Well, thank you. This was true. Yeah. I enjoyed listening to this kind of talk through the idea. We'll find I'll find out if I get notes like, could you guys not not record your meetings, please?
Jennifer Smith, CDE 55:37
Well, you know, but I think it's even if you put it up as a as the preliminary pro tip for honeymooning. This is what's coming. If you are newly diagnosed, we promise we are we are getting to some of these big questions that you really want to know sooner than later.
Scott Benner 55:59
910 I'm counting 1112 1314 2020. Okay, so yeah, even the way the podcast runs, usually your episodes go up like once a week on Friday. Okay, you're you're like you're the Friday girl. And but maybe I don't put episodes up on Thursdays maybe so that I can get them out more timely. Maybe I'll put them up Thursday, Friday for 10 weeks, and then we can get them up more quickly. Okay. Thank you so much.
Unknown Speaker 56:27
Yeah, absolutely.
Scott Benner 56:35
A huge thanks to Ian pen from Medtronic diabetes for sponsoring this episode of the podcast learn more about the impended in pen today.com forward slash juice box. Also like to thank us Med and remind you to go to us med.com forward slash juicebox. Or call 888-721-1514. To get your free benefits check. Take the T one D exchange survey AT T one D exchange.org. Forward slash juicebox. The very first episode of bold beginnings will begin in just one week on Friday. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
If you'd like to be part of the Facebook group, where we got all the information for the bulb beginnings series, it's Juicebox Podcast type one diabetes on Facebook. It's a private group. So you'll need to fill out a little bit of information, just answer some questions to prove to the algorithm you're a real person. And just like that, you'll be in and talking with 25,000 people who use insulin Juicebox Podcast, type one diabetes on Facebook. And if you're enjoying the show, please leave a rating and review in the podcast app that you're listening in now. And if you're not listening in a podcast app, please think about doing that. Following the show in a podcast app or subscribing to a show and a podcast that really does help. It helps very much you have no idea it raises the ranking of the show and makes it more visible to other people. So you can tell somebody about it. subscribe or follow on a podcast app. And don't forget to follow the Facebook page. And that's pretty much it. I'll see you soon
Test your knowledge of episode 698
1. What is the main topic discussed in Episode 698?
2. What method did Scott use to gather information for the Bold Beginnings series?
3. How many pages of feedback did Scott receive from the community?
4. Who helped Scott organize the feedback document?
5. What format will the Bold Beginnings series take?
6. What is the goal of the Bold Beginnings series?
7. What did Jenny suggest about the structure of the series?
8. What did Scott compare the information provided in the feedback to?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!