#382 Stem Cells and Type 1 Diabetes
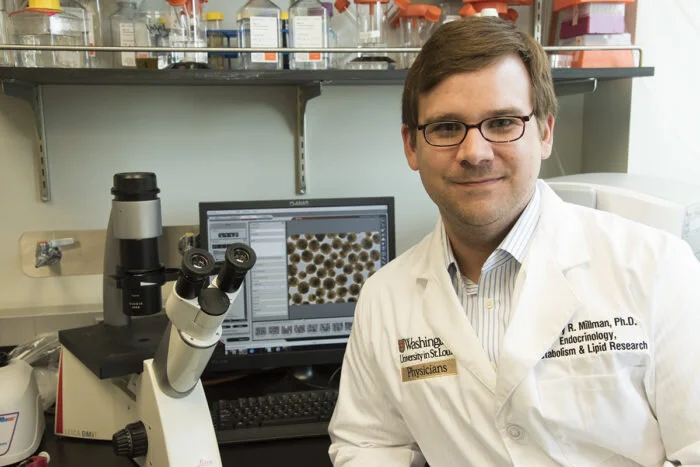
Jeffrey R. Millman, PhD
After reading an article about stem cell research, Scott invites Dr. Jeffrey Millman onto the show to talk about stem cells and Type 1 diabetes. Dr. Millman discusses how he and his colleagues developed a protocol for generating functional pancreatic beta cells in vitro from human pluripotent stem cells. In this episode, Dr. Millman describes the fascinating research currently being developed at the Millman Laboratory at Washington University School of Medicine in St. Louis.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:06
Hello friends and welcome to Episode 382 of the Juicebox Podcast today, my guest is Jeffrey Millman. Jeffrey is a PhD. He's a researcher, and he is working on some very interesting stuff regarding Type One Diabetes that I think you're going to enjoy hearing about. I reached out to Jeffrey, after reading an article online that started off by saying new technique efficiently converts human stem cells into insulin producing cells, I thought, well, that's interesting, and seems like a leap. I reached out to Jeff, and he was kind enough to come on the show. Best thing about him is that as he's explaining all of these, what I'm going to tell you are pretty technical ideas. He does it in a way that you can understand. I mean, I understood it, so I'm assuming that means we all can. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making changes to your health care plan. We're becoming bold with insulin.
Today's episode of The Juicebox Podcast is sponsored by the dexcom g six continuous glucose monitor, and the Omni pod tubeless insulin pump, you can get a free no obligation demo of the Omni pod sent directly to your house by going to my Omni pod.com forward slash juice box and learn more about the dexcom g six continuous glucose monitor@dexcom.com forward slash juice box. When you use the Dexcom g six like my daughter has been using for ever now. You're going to see your blood sugar trends in real time. And what direction are they moving? And how fast are they moving in that direction. There's a huge difference between having a 95 blood sugar that is stable, and a 95 blood sugar that is rising or falling. Rising blood sugars may need insulin. Falling blood sugars may need carbs. Steady blood sugars don't need anything. But with the finger stick, all you see is 95. But with the dexcom you see 95 and all the rest. The best thing is, you can share that information. If you're an adult with Type One Diabetes and you want your wife, your mother, your sister to see that information. They can they can follow it on their iPhone or Android phone. Actually, you could share that information with up to 10 people at a time. Imagine what a great thing that might be for your child away at school or your child up the street, husband, wife, school nurse, anyone you want to see your information can see it and no finger sticks. Come on dexcom.com forward slash juice box, get the game. The Omni pod tubeless insulin pump makes your life easier. You do not need to be injecting insulin all the time with a pen or a syringe. And if you already have a pump, but it's not the only pod. The Omni pod doesn't have tubing, so you don't need to be connected to a controller or have to disconnect to shower, go for a run, play sport or take a swim. You can get that insulin the way you're meant to 24 seven, my daughter has been wearing an omni pod tubeless insulin pump. Since she was four years old, she is 16. Now she's had an omni pod on every day. It has been an absolute friend in this journey as the Dexcom Omni pod would be thrilled to send you a free, no obligation demo, do that at my Omni pod.com forward slash juice box. And of course there are links in the show notes of this podcast player and at Juicebox podcast.com. To all of the sponsors. One last thing, head over to T one d exchange.org. forward slash juicebox to take a very short survey and that information will be collected anonymously, hundred percent HIPAA compliant and it goes to making huge decisions that help people with type one diabetes every day. It is a selfless, easy thing you can do to help people type one. And you can also support the podcast when you do it. Dexcom on the pod T one D exchange. They're great sponsors. So check them out. dexcom.com forward slash juicebox my omnipod.com forward slash juice box T one d exchange.org. forward slash juice box. I put the ads up front today so you can really settle in and focus On what Jeff is saying. It's pretty fascinating. As a matter of fact. It's astonishing. Alright, let's get going.
I have a handful of questions, but mainly, I just like to hear your thoughts.
Jeffrey R. Millman, PhD 5:35
Yeah, I appreciate the invite. And one of the things that we try to do over here is to reach as wide of an audience as possible. And so I view this as a good opportunity to reach further into the Type One Diabetes audience. Hi, my name is Dr. Jeffrey Millman. I'm an associate professor of medicine and Biomedical Engineering at the Washington University School of Medicine. My lab uses sim cells for the study of treatment of diabetes, and I'm very happy to be here today.
Scott Benner 6:05
Thank you so much for doing this. Okay. How do we do this? am I calling you Jeff Jeffrey. Dr. Millman, what do you like?
Unknown Speaker 6:12
Um,
Jeffrey R. Millman, PhD 6:13
I would say,
Scott Benner 6:15
Jeff, would probably be best. Hi, Jeff. Well, I'm Scott. And I saw an article that was floating around in the news. Let me see if I could be more honest than that, Jeff. There's the thing that I think of is cure season, where everyone floats their research out as far as they can, I always assume they're looking for more funding. And it has this sort of unintended consequence of reaching newly diagnosed people who think that they've been diagnosed just five seconds before the cure was going to come. And so I always kind of pick through them to see what's interesting, and what seems more like, you know, what I just described, and your seemed really interesting. And I just thought this, this seems rooted in real science. It seems like science that's available to us now that we understand. And that's why I reached out, I guess, first, let me understand, you know, how did you Why did you go to college for what what were you thinking of doing when you were becoming a student?
Jeffrey R. Millman, PhD 7:18
Right, so I definitely didn't have diabetes research on my mind, when I went into college, even doing biomedical research was not a thought that had crossed my mind. My I went to the college and got a degree in chemical engineering, actually, I had, I came from a very poor and rural area in North Carolina that didn't have a very robust school system. And so I wasn't actually exposed to what, what that what biomedical research was little known what kind of biology was, and so I went into college thinking, I would just go and be an engineer, get a good paying job, you know, raise a family and all that sort of good stuff. And actually, during my time, as a undergraduate doing chemical engineering, I became more and more exposed to the overall biomedical sciences. And I thought, well, that's pretty interesting, you know, maybe going and doing work that is actually helping people's health is more interesting than going and working at a chemical plant to go and make the latest and greatest and shampoos, for example, or at a petroleum plant, which is pretty typical for a chemical engineer, as I went on, after my undergraduate work, to complete a PhD still in chemical engineering, but I sought out a laboratory that did some work with stem cells. And about halfway through my time during my PhD, mostly trying to catch up on the biology, kind of classroom training, but that I hadn't yet received during my undergraduate degree, I received a unique opportunity that my lab received funding from the jdrf, which is one of the largest supporters of diabetes research in the world. And that set me on the course that I've been on ever since. So they they awarded a grant to my lab that covered the last portion of my training during my PhD. And during that I got exposure to diabetes, the the needs that patients diabetes have in house themselves could be helpful for them. And so that prompted me after I got my PhD, that I was looking at all the options that I had after after that, and I was like, well, I really enjoy doing the research. But scientifically that the questions of how do you make a cell from a stem cell that can respond to sugar and secrete insulin? I thought that scientifically was very interesting. And I obviously didn't realize how major of a need that that was for a lot of people. Yeah. And so after that, I switched my trajectory completely to stem cell biology for for the context of coming up with a functional cure for diabetes. And that's led me to where I am today.
Scott Benner 10:34
That's cool. I want to ask you a question. I don't want to get too far off the path, though. But you went to MIT. So I was wondering how frustrating it was in high school, to not be in a terrific school system, is that something you felt as a kid, I
Jeffrey R. Millman, PhD 10:49
didn't really understand my situation until I was much older. If you're kind of born and raised in a certain area, you don't really know what you're missing out on. And I was fortunate in that for the last two years of my high school, I was able to get into this state wide magnet school program. So I was actually able to bless you with your high school, leave my school district and go as far as a high school that's actually part of the UNC system. And so I got to live on campus there for free and get advanced course work that I did not, I was not able to get during my, you know, pre High School and first two years of high school in my school district that I grew up in. And so that's really, you know, began to open my eyes to what the other possibilities were, though I didn't really get my head wrapped around by middle sciences. Until I got into college, I would say going to that Magnet School for high school was very important to be because I don't know if I would have been a fairly
Scott Benner 12:09
receptive to the new knowledge out there about you know, what biomedical research actually was, if I hadn't received a stronger foundation that the the second high school that I went to was able to afford me. So in hindsight is frustrating. But at the time I did it, it really realized what my situation does. It is really interesting, isn't it that you just don't know what you don't know. I'm, by the way, imagining your entire family that they must have Monday through Sunday t shirts that say my son went to MIT, my brother went to MIT, I would be wearing them constantly, I'd said to me, it's a very impressive thing. So you know, it's an it's amazing path to get from where you were to there and now doing this. So I wonder if you could tell me why stem cells are more interesting than other avenues for helping people with who can't make insulin.
Jeffrey R. Millman, PhD 13:04
I guess they were sorry, I'll start off by saying that there is a functional care for diabetes that is already out there. And that is cell replacement therapy, taking introducing cells that can be taking from a deceased donor, and transplanting them into a patient with Type One Diabetes. And it's not a perfect procedure. But in a lot of cases a patient will have can have reduced or eliminated the need for insulin injection, a lot of nuances there, I'm skipping over but that does exist. And this procedure is done probably about 100 times per year, more or less worldwide. And so I think that this is kind of unique in the cell therapy space of their being a kind of putting diabetes aside and thinking about it more generally, when it comes to cell therapy, what you would use themselves for this is pretty unique that there's already you know, very strong proof of concept that this can work. So why aren't Why isn't everybody receiving a cell therapy? Then and the very first challenge which I've dedicated the last 10 years or so, to overcoming is the problem of cell sourcing. I mentioned that the cells currently come from deceased donors and there just aren't that many deceased donors that are rounds and available for providing replacement, introducing cells for patients. It's kind of like if you ever watched these medical dramas like Chicago hope or Grey's Anatomy or you know or whatever, and you're like oh, we need to have a you know, replacement heart or liver or kidney in the next 24 or 48 hours. Are the patients going going to die and there isn't immediate organs available is that sort of thing, they just aren't that many donor organs available overall. Okay. Fortunately, for for diabetes, we have a therapy that is very effective and can, you know, maintain people's health for many decades, and that's insulin. But we still have this problem of self sourcing. And so when I was looking at options out there for what we would use, besides, besides the sea stoners, I felt that humans themselves for the most obvious choice that to make that occur. And the main reason for that is that the stem cells are capable of growing and dividing and making more of themselves virtually indefinitely. In my academic lab here, which we are not a, like a manufacturing facility, we don't make cells for going to people. So we're relatively small scale versus a company that would actually do this. But even in my in a relatively humble laboratory, we easily make several billions of cells every single week for our own studies here. And that would be enough for, you know, multiple people as as well. So having the ability to make a virtually unlimited number of cells as your starting material is a clear advantage. And most cells can't do that you can't just like take interesting cells in the body and grow them up indefinitely, they just like they just don't grow. So you'd have a stem cell to do that. The other advantage of these stem cells is that they essentially represent a cell type that is very early during embryonic development. And what that means is that we can, if we give them the correct signals, basically putting in like proteins, or sugars or chemicals into the, into the flask that we're keeping the cells, then we can direct them to transform from the sim cell into any cell found in the body. So you have a one mixture of proteins and chemicals, you can go and make heart cells, a different mixture will give you liver cells. And of course, the mixture that we care about quite a bit is, is producing cells in that particular cell type that produces insulin in the body is called the beta cell. So this is a unique feature that isn't really replicated by any of the other options there. And we've been quite successful with it, I believe, with our preclinical modeling in diabetic mice. Let me just interject here and make sure that people understand they're listening when you were talking about doing a transplant, that then infers that the patient needs anti rejection meds, is that right? Right. And that's still a pretty major problem. Right?
Scott Benner 18:02
Right. And so now you're basically treat change or excuse me exchanging Type One Diabetes for possibly cancer? Is that the concept of why that's not more widely considered? Do you think
Jeffrey R. Millman, PhD 18:14
so you need that you need a suppressant drugs can have a whole host of side effects. I'm not quite certain of cancer is one of them. Okay? Is there it's possible but the most obvious issues with that is that you're weakening a patient's immune system in order to make them so they don't reject the introducing cells that are be transplanted into them. So they'll be more susceptible to infection or sepsis, for example. Yeah. And that's maybe where it's a decimal as part of the reason as well, why there are only a few procedures done each year, because the people who are receiving these is facing cells from deceased donors, basically, the sickest of the sickest. They have severe hypoglycemic unawareness usually been hospitalized multiple times, because of that other organ failures to
Scott Benner 19:08
sorry, other organ failures as well, that sometimes
Jeffrey R. Millman, PhD 19:12
Yeah, severe complications. In addition to that, though, for though, I think one of the more scary things since what I've spoken to patients in the past, and you probably know better about this than I do is the is the issues of, you know, loss of eyesight, but also hyperglycemic awareness is fear that you might just go to sleep and not wake up. Yeah. And so, you know, these are these are particular, these are the sickest of the sick when it comes to patients type one diabetes. And so in that case, the negative side effects of immunosuppressant drugs outweighs the complications that they have from from their diabetes, right, right. However, that's obviously a calculus that boasts patient with type one diabetes. BDS can't accept, in most cases, the side effects of immunosuppressive drugs is not worth it in order to have better management of their diabetes. So this probably gets to maybe the third advantage of working with stem cells as a cell source here is the fact that we can genetically engineer these cells in order to make them better for transplantation. And kind of one of the newer areas that my lab has gotten into in recent in the recent year is to genetically engineer the cells so that you do not need to give the patient's immunosuppressant drugs anymore. That's basically change what signals the interesting cells are giving to the immune system to trick the immune system into thinking the cells are, should be there and are not from an actual donor.
Scott Benner 20:59
That's that's magic. Jeff, that's, that's absolutely amazing to hear it really, it's, it's astonishing to hear someone say that I tell the cell to give off a signal that makes the immune I mean, that's crazy, man, like, You're brilliant. How did you? Thank God, you're not making shampoo? Although I bet my hair would be amazing.
Jeffrey R. Millman, PhD 21:20
Yeah, your hair probably be great. Maybe some stem cells can help you out with that. No, I and the analogy I get here is that, you know, the sentences I just said, you know, a few years ago were like, legitimate science fiction. Being able to do this, in a like a realistic way was simply not possible even a few years ago, it was an idea people had. But the theology wasn't there, both on the stem cell technology side, but also the genetic engineering side, in order to be able to do that at all meaningfully. And only really, in the last, I would say, year or so half both the genetic engineering capabilities and the stem cell technology doesn't the point that we realized that we can do this now it's no longer, you know, five years ago is definitely science fiction of like, oh, that'd be nice to do. But a year ago, we realized that, oh, we can do this now. And you know, overcome one of the major challenges of a cell therapy for patients with diabetes. So this may be one of the fun aspects of my job here, as a faculty member, is that, you know, we get we had the flexibility to, you know, start pushing the envelope and going beyond a transforming things that are science fiction into something that's reality, and hopefully, eventually a therapy that can help the millions of people that could benefit from it.
Scott Benner 22:56
And tell me how you go about testing this? It's, it's on lab mice, is that correct?
Jeffrey R. Millman, PhD 23:02
Right. So the test out how effective ourselves are in terms of as a potential therapy, we take lab mice, we give them a compound that is able to destroy the mouse's own introducing cells, we get the mice diabetes, by you know, basically killing off their their own cells, and then we do a transplantation into these mice at the sea, you know, are we able to first reverse diabetes in these mice? Can we do it rapidly? And the second question is, how long are we able to keep that diabetes care? And number three, are there any ill effects of the transplants? Do they one of the fears is the potential of the cells we're putting into the mice to perhaps become a tumor? And so we go and we look for any signs of tumor formation, or you know, any other sort of, like biochemical changes in the blood chemistry of the balance that would be indicative of major health problems. And it really only this year, with our recent scientific applications, have we been able to answer positively to all those questions, and with heinously, the cells that we have now are able to virtually instantaneously reverse diabetes in these mice. It takes about a week or so because we have blood the blood vessels grow into the cells we're putting into the mice, but after that, the diabetes has been reverse diabetes reversal last for the lifetime of the mice, which is about a year and then there has been no signs of any health problems associated with the transplant the blood chemistry looks Good. And the there's no signs of tumor formation. And we've done this a lot of times. Now I think the total number of mice that we have transplanted with our latest version of the technology is over 100. And so far, we have a 100% success rate when it comes to curing diabetes, and a 100% safety rating when it comes to mice we have transmitted,
Scott Benner 25:28
what's the next step after a mouse? Unless, by the way, Jeff, and I'm just thinking out loud here? What if you found a way to turn a person with diabetes into a mouse and then gave them stem cells, then turn them back into a person? I think really that maybe is what you should be looking into. But just in case, that's not possible, what do you do after you've proven it out over and over again, in a laptop mouse? Do you move on to a larger animal something that's more closely related to people? I don't know, what's the process?
Jeffrey R. Millman, PhD 25:57
Well, I think also, we have to keep in mind how important the diabetic mouse community is to us. And maybe they should be the priority first. I'm just kidding, of course. So, actually, you asked a very hard question. And it's actually been in a lot of discussions, and there have been a lot of people who are, you know, experts in the field that give very different answers to the the question that you just just proposed, there are, there's an argument to be made, that having great success with a mouse model of diabetes is sufficient, and that we shouldn't waste any more time trying to make larger animals work with the technology instead should just go straight into a phase one clinical trial, I think it's a lot of merits to that. There's also an argument to be made, that a large animal like a nonhuman primate or a pig has a physiology that is more similar to a person than what a mouse is. And that showing pre clinical success. And one of those models is a necessary stepping stone, when it comes from going to where we're at right now with great care rates in mice before we put it into a person. And so I I personally am kind of stuck between these two positions. And I think a lot of it depends on sort of your,
on your
what you're trying to get out of this, I think as maybe a if I put on my academic hat, I think it's a lot of value. For going into the larger animal models, we can do a lot more testing and a lot more invasive work. When it comes to large animals. And I apologize for the siren in the background. I'm actually at the medical school that you
Scott Benner 28:19
might get, you might get more work done if you moved out of that firehouse, I think
Jeffrey R. Millman, PhD 28:26
well, the Dalmatians are very nice to keep about lab morale, you can give them
Unknown Speaker 28:31
diabetes and see if you can.
Scott Benner 28:34
Well, you're in between you're not I'm in between what what stops? So is it biases is that people who are just like, Look, I want to move on this, I think it works or is there real, scientific reasoning for both of the ideas? Maybe we should try another animal larger? Maybe we should jump to a person like what are the arguments for each Do You Have you heard them? So the
Jeffrey R. Millman, PhD 28:57
arguments for going into a person is that there is that mice are as good as a large animal in terms of guaranteeing the safety of a person. In fact, there's already when he made that mice are better safety model. For them what a pig or a non human primate is, because of some of the special genetic mice that we have. They allow for health issues to be easier to detect than what you would see inside of a large animal. So the argument for going to people would be that mice are as good if not better than then barge animals to ensure safety of a person. And so if we already have all the data, proving the safety of the product before going into a person, we might as well go into a person to you know number one, help to accelerate transition to translation of this over to a, a care. And number two, the the effectiveness of the treatment in a person is going to be more meaningful than the effectiveness of a treatment in any animal model. Because obviously, we care about how it works in a person a lot more than we care about a monkey or a pig, or a mouse or a Dalmatian. So that's the argument for doing it. The argument for doing it in a large animal is that we can you know, do, we don't have to go through as much regulatory hurdles, basically, to go and get answers in terms of effectiveness inside once transplanted into a large animal model. There isn't a you know, FDA? Well, at the clinical trials when it comes to large animals or regulations for it, we can't go about it, willy nilly. And there's ethics to consider. But those you know, those are similar to what we already do with with the mice. And so we'd be able to, if we decided to do large animal work today, we would probably be able to in Sydney, we didn't have the program going right now, we would be able to realistically do this in probably two or three months, as opposed to if we decided we wanted to go into a person today, assuming the FDA didn't require the large animal intermediate. I don't know the answer to that. Right now. It would probably take two years to go into a person.
Scott Benner 31:38
Well, I have questions around this. Because I'm always fascinated that as people we see things as either or it's always one or the other. Why not? Both? Why not move forward on both of them at the same time? And then abandon the one that that doesn't end up being needed? Like, and and are there any? I don't know what the word I'm looking for is, but does the FDA ever make allowances for people in situations that are dire? And Couldn't you find a person in their 60s has had Type One Diabetes their whole life? Who is really at the end of their health rope and just say this is this is reasonable to try with them? Do you know what I mean? Like, when does common sense? jump into this?
Jeffrey R. Millman, PhD 32:21
Right, and I think the way you phrased the question at the beginning, it kind of matches what I the way that I do this is at the flexibility of being a academic working in the space, that I try to do what I can in order to, you know, in terms of developing new technologies, and giving advice to people to help companies go into clinical trials as fast as possible. But in the meantime, we do our own academic research here. And I'm not doing academic research on people. And so we have already done some large animal transplantations as part of our academic mission here. So essentially, kind of terms of like me personally, when it comes to being in the field. You know, I'm kind of able to play both sides, if you will, without having a academic program that uses large animal models of diabetes, while also trying to help companies that may be wanting to bypass that and go into a clinical trial. However, when it comes to, you know, an individual company's perspective, and I don't want to I'm not speaking for anybody in particular, but just kind of thinking about the types of questions a company would want to ask themselves, they would need to make a decision on you know, if, you know, they want to, you know, spend finite resources on a large animal models or on clinical trials are trying to split it across both and they may face the reality that they don't have the resources to, both and you know, may need to go and choose one over the other. So that that's maybe the argument for not doing everything is if you don't have the finances to do it, or the ability to do it, you got to go down the only option that you have available to you. So you made reference to kind of a an emergency clearance type of decree, I don't know what the exact terminology is for it's from from the FDA. And this is it's been happening a lot when it comes to like COVID-19 testing. I know a lot of these diagnostic kits I've been receiving like emergency clearance from the FDA, since we're in the middle of a global pandemic that is killing hundreds of thousands of people this year alone in diabetes, for the most part doesn't really fit in terms of
terms of that there being a good pill parallel there.
Overall, the FDA again, as I as I understand it, I'm not I don't represent the FDA or anything, but as I understand it, the, you know, FDA is wanting to balance risk here. And if you have a new therapy that you're wanting to do a trial for get a vergence, the approval for what is the alternative there? What's the relative risk and reward there. And since
diabetes is,
you know, that is controlled to at least a certain degree by insulin or insulin sensitizers. The oftentimes there isn't a, I could imagine the FDA looking at that and thinking that's there is not a justification for a kind of an emergency clearance or emergency clinical trials, when it comes to a cell therapy. With that said, there's gonna be maybe some sub populations of patients for which that could be an argument for I could imagine I'm just kind of spitballing here a little bit, but there are kind of going outside of type one diabetes, there are certainly certain rare genetic forms of diabetes, the so called like Modi's or neonatal diabetes, or Wolfram syndrome, or cystic fibrosis and do cbds, that maybe some of those cases could fall into that that'd be one possibility going forward with it. But it just that some,
Scott Benner 36:33
somewhere the imperative lies that it's worth the risk and taking the leap. And by the way, like, I'm obviously not a historian on this, but don't most of our major advancements fit into a mold like that, like just something that had to be done. And we did it and it works. So we kept going.
Jeffrey R. Millman, PhD 36:51
Yeah, I'm no medical historian. Well, I don't know if I can really
Scott Benner 36:55
yeah, think about, it just makes sense. Listen, maybe I'm writing science fiction, too. But it just makes sense that, you know, there's somebody out there who's in a dire enough situation that be like, Hey, give me the mouse thing. And let me see what happens. And if it doesn't go, Well, it doesn't go well. But I didn't have much to lose to begin with. And, you know, he just would think that was I don't know, Jeff, maybe we left prisoners with type one out for doing that, you know, there's got to be a way is what I'm saying. There's got to be somebody who would be willing to like make take the risk, because the risk would be reasonable for them.
Jeffrey R. Millman, PhD 37:27
Oh, you mentioned the prisoner thing. I don't know if you're aware of medical care. And but I do know a little bit when it comes to prisoners, when it comes to what we call human subjects research, there's actually been a bit of an issue in the past in this country, on kind of compelling prisoners to engage in human subjects. Research, I don't know that it's the proper clinical trials. But there's actually a lot of it becomes the issue of like, having the ability to properly consents to things. And if you're a prisoner, and do prayer, given you're kind of maybe can feel compelled to do things that are against your self interest, because of the imbalanced power dynamic. So actually, if you want to do any research with human subjects, and you want to do it with prisoners, there's actually a lot of additional regulations involved in doing that. Because of the inherent, disproportionate power dynamic that occurs when you're dealing with a prisoner, to the point that I don't think there actually is much work at any done with prisoners. Because of what's happened in the past.
Scott Benner 38:49
It's, it's funny, I was just reaching in my mind for someone who would be in a dire enough situation, like I wasn't saying to, like knock three months off of a larceny run, I was talking, you know, I was talking more about like, I'm gonna spend my life in prison, maybe I would take a risk with that life to to get it out. And meanwhile, I completely understand what you just said, and all the other parts of that, that seem untenable. I really, I could have just as easily reached for any other, you know, example out of my head, I wasn't like, you know, we have those prisoners, we should use them. That's not what I was.
Jeffrey R. Millman, PhD 39:23
But I think I'm glad you brought it up, though, because I I spent a lot of time speaking to audiences of patients with that diabetes in their families. And I know that there is a frustration that exists when it comes to the perceived slow pace of scientific discovery. And that actually being translated into a into an actual therapy that been themselves or a loved one, and oftentimes gets very direct questions about like, why is this true? Like you can already do amazing stuff with mice? Like, why aren't we just putting it into people right now as a very reasonable question. And the frustration behind the question, I think is very reasonable. But I think the like the prisoner thing is an example of the types of considerations so we have want to keep in mind that the path from a having very good preclinical animal model evidence of a new treatment, or functional care for for diabetes, is just the beginning. And to go from where we are at right now, academic research into a therapy that can benefit yourself or a loved one, loved one is a long path that has to be treated very, very carefully. You know, the prisoner thing kind of illustrates one of the ethical dilemmas that could occur, you know, issues of, you know, the large animal model that we talked about several minutes ago is another one as well, like, is that required or not, and people who are experts in the field, you know, disagree on that, on that one issue. So I think all the points we've been bringing up here, I think, very clearly illustrates that it's not a straight in easy and direct line going from where we are to where you want to be that there is, you know, a lot of care that needs to be taken in order to do this correctly. Otherwise, we're going to end up, you know, taking even longer to translate this care to help people in the long term, and, you know, could potentially hurt some people along the way, we're not very careful in how we're doing this. And we, we don't want to, we don't want for that to to occur. And to give you maybe an example of that, this is pretty, pretty another again, I'm not a medical historian, but I do know a little bit of things that are becoming more famous kind of a case studies that are out there. So in the 90s, there was a lot of hope and hype for gene therapy to care, a lot of diseases, we were getting better at genetic engineering technologies at the time. Of course, now we're a lot better. But the 90s is really where a lot of the stuff started to happen. Instead, there was a clinical trial started to do gene therapy for children with a severe genetic, immune deficiency that you may have heard, like bubble boy type of terminology, these people have mutations, a mutation that basically gives them little to no immune system. So there's clinical trials that happen in the late 90s, in order to in order to treat these patients, and one of the patients, a young boy actually died from the treatments. And so what happens is a bit that's very unfortunate, very tragic. And what happened to the field is that basically, all work with clinical trials with gene therapy stops, and nobody was willing to pursue gene therapy for people for about two decades, and only now have things kind of warmed up to begin doing this again. And fortunately, it seems to be a lot of people are treading a lot more carefully. And are and are, you know, doing a lot better. Again, the technology is approved a whole lot and gene therapy, the way we do it now is a light year ahead of where things were in the 90s. Right. So and so so i think is a cautionary tale that if we do this wrong, we can end up you know, hurting people and then delaying progress to a cure potentially for decades. Because Because the academia side will run away from it, because it's like, it's scary, and it went wrong. And you don't want to be attached to it at that correct. Yeah,
Scott Benner 44:24
I say so there's that human so it's just a myriad of things to consider. And some of them have the potential to significantly waylay progress. And and so you want to be careful moving forward and do it in a meaningful way. I you know, I don't listen, I'm not a person who thinks that you've got the answer over there on your desk and you're just not giving it to us. I don't have that feeling but a lot of people do get that idea of like, well, there's more money in the treatment that there isn't a you know, in this but this is not a cure either. This would be you know, this would be a treatment that would go on you don't honestly know it. You would need more cells, as a human life move forward at this point. So
Jeffrey R. Millman, PhD 45:05
yeah, the timing issue is one of the big scientific questions right now. And the city where the large animals actually have a benefit here, that we are limited by the lifespan of the mice that we're using currently, in our studies, and that's about a year. And so we know for for a year for the lifetime of the mice, the cells seem to function perfectly fine until the mouse is dies due to old age. And so we don't know if that means that at like, one year, one day in a person, all of a sudden, the, the transplant doesn't work anymore. And then the patient wouldn't need a dosing, or if those are going to last for years and years and years or decades, or for the lifetime of the actual patient. Right. It's but I do think that even kind of in the worst case scenario here, if the cells end up, only working for a year or so, which I just intuitively, I think that's not going to be the case. But as soon as That's true. I suspect that many people would choose a dosage of cells every year or so over what they have to do every single day. Again, I'm not I'm coming from this from an outsider's perspective, I am not diabetic, and I don't have any family members who are diabetic as well. But I spent a lot of time because like, it's very important to, you know, keep the eye on the prize here. So I spend a lot of time speaking with patients understand their stories and their motivations there. So that I had that in mind while I'm conducting my academic research here. And from from like, from, from my discussions with everybody, and to get out of you know, this a lot better than I do. That I think that most people would accept a once a year treatment over what they have to do right now.
Scott Benner 47:05
Well, yeah, I think for my daughter, I would definitely want that. And I believe she would do as I'm speaking for, but and what are we talking about? Do you do know how we're talking about the implantation? Is it just a large needle? Like thing? How do you How would you get the cells where they need to go?
Jeffrey R. Millman, PhD 47:22
I, I guess how?
Unknown Speaker 47:24
Much another question. Yeah,
Jeffrey R. Millman, PhD 47:27
yeah. So the way we currently do it in mice is not the way that we would do it in people. One of the problems with with my side, everything is anybody. And we don't necessarily have like cutting edge. microsurgery equipment in my lab literally is like me sitting there with a mice. So to do surgeries for my lab, like the only real thing that I'd be as the director of the lab, I feel to actually do in the lab. But you know, it's literally me over a mouse, putting themselves into the mouse. And so we actually currently in the mice, transplant them into the kidney. Because for practical reasons, not for translation reason, okay. But for for people, we would need to figure out the best location to do this. And the complication there is, is basically the amount of blood that is available. One of the great things about producing cells is that they don't actually need to be in the pancreas or native Oregon, in order to do their job. If they have enough blood flow, they're able to sense the sugar levels and the blood and deliver insulin into the bloodstream. So that's the only real requirement there. But not every area in your body has the same amount of blood available for the institute's themselves do their job. And so a lot of people are hoping just to be able to put the cells just underneath the skin, or maybe into a muscle so they could have a needle injection type of thing. And that's looking promising. Now, it's kind of hard to do that, just with like naked cells into the into the spaces because of the relatively low density of blood vessels there. But if a lot of work done with various types of biomaterials that can help to promote an increase in blood vessel formation there in order to enable so you basically kind of created like a little pockets underneath your skin or in your muscle that is supportive of the introducing cells to do their job by providing them with enough enough insulin. Alternatively, you could put them into a different organ. People don't want to do it in the kidney because of a lot of people with diabetes, having kidney issues. So what's actually done clinically right now is to inject them into the liver. So that is highly vaster alized as an Oregon, and also most of the work that insulin does, and your body actually occurs in the liver, and so having the instantly delivered directly into the liver is good. From a physiology perspective.
Scott Benner 50:24
That's really incredibly interesting. I'm having a lot of fun talking to you about stuff that I thought I wasn't gonna understand. But I am understanding I, I, I want you to know that over the years, I have many opportunities to talk to people who are in similar positions to yours, but I never felt like what they were doing had a real chance. And and you talked earlier about how things have sped up so much recently, I just wondered if we could detour for a half a second. What made that leap? Is it? Is it like the advent of supercomputers? Are there like how did you how did we speed up like this,
Jeffrey R. Millman, PhD 50:58
I wish we could figure this out with supercomputers, because that'd probably be a lot less work and less pipetting on my teams. And in order to do this. So really, the watershed moment here, occur occurred, actually, before I became a faculty member here at washu. So after I got my PhD from MIT, I, and I decided I wanted to do diabetes research, I actually did a what's called a postdoctoral fellowship, which is basically your time between getting your PhD and becoming a faculty member. So I did that down the streets, from MIT at Harvard University, in a famous diabetes lab over over there. And so the test that I had during that period of time was to figure out how to make these cells basically, when I started doing my fellowship, I, the field didn't actually know how to produce these cells at all, we knew how to make progenitor cells. So these are cells that were kind of halfway between a stem cell and a introducing cell. But we didn't know actually the correct proteins and chemicals to, to put into our flask in order to make them go all the way into a insulin producing cells if people had tried to do what you just suggested with supercomputers or that kind of kind of computational methods in order to do that. And the truth of the matter is, we don't understand biology enough, in order for these, what we call in silico methods to be able to be very productive predictive of approaches to making it so I was tasked with basically trying to figure out how to get over this problem that have existed for the 20 years that themselves had been since since those had been invented 20 years prior to this. And we hadn't been able to figure out how to make these cells during that time period. So essentially, the trick was to read a lot of papers that were describing how this occurs, naturally in embryos. So this is mostly like, how do you get cells and fruit flies or fish or mice. And so those are the, what we call model organisms that we use to try to understand how a embryo develops, develops naturally, to go and look at what lessons people had learned from studying these animals, and then trying to translate them over to our humans stemcell bioreactor context. And so I literally went through I did, I did a estimation after the fact there was about a 180 papers, and found that only about two or three of the
papers actually
provided chemicals and proteins that we could put onto ourselves cells in order to actually make them basically it was a matter of going through the literature, finding papers that were irrelevant to actually making the cells in our artificial lab ground context, and find the few that were actually relevant and to kind of make these what to call first generation cells. So we're able to take these few papers, figure out the compounds from it, and be the first to make introducing cells that were capable of controlling diabetes in mice. And once we were able to do that with them, first of all possible with existing technology, and do some of the Pacific compounds for how to do that. It became a question of being the first To do it to taking these cells that were very immature still, but were definitely the correct cell types that we wanted to make there and optimize. And so that's optimization is taking something and making it better, is infinitely easier than going from nothing to being the first to create something. Yeah. So it's really the watershed moment that we went from not being able to do this for 20 years, to then, over the course of then figuring out how to do the first iteration of this, and then go for the next five years after that into a improved sell product that is now able to reverse diabetes and be safe. And all these great things that we talked about earlier. I want to understand the
Scott Benner 55:47
timeline, you reading that literature and coming to that, that idea. How long ago was that?
Jeffrey R. Millman, PhD 55:54
So I started in 2011, doing this, and we pretty much had figured it out by 2013. And we published the scientific reports on that in 2014.
Scott Benner 56:11
And one day, well, this becomes a thing we're gonna call it the milman method, is that correct? We're gonna get your name, right.
Jeffrey R. Millman, PhD 56:16
Well, there's a reason I keep on using the word we and that seems to Team science, right? It's like, nowadays, science is so big and so hard that it is really difficult for a individual to be the one to to come up with something that's truly transformative, that moves the field forward and not impossible. But more often than not, you are better off working with, with grapes. And now of course, I lead a team of 10 scientists here at Wash U. And so everything that I'm involved in, but obviously involves other people on my team, and oftentimes other people at other institutions as well. And so I really think that team science is the way to go forward here, because it's not going to be one person. If this is a problem, that is too important to expect a individual person to solve, we all need to be working together. In order to do this. And everybody that I work with on this all shared the same vision that we're all in this together for the greater good of coming up with a therapy.
Scott Benner 57:30
And we're seeing this with COVID. Right now, too, right? Aren't labs sharing information at a, just an unprecedented rate now around COVID?
Jeffrey R. Millman, PhD 57:40
Yeah, it's something that I have never seen, to that extent before in my professional career, that, you know, we have these groups that, you know, we're never working together, all of a sudden started to work together to solve this very important problem of how to deal with COVID-19. And it's complications. And I think part of this as well is kind of where we're at now, in terms of the ease of communication and the ease of disseminating information. There's a lot of me, this has been a lot because of how much the Internet has advanced even in the last 10 years. But in particular, it's become kind of a trend in the last maybe three years or so it's on my radar. I know it existed before. This is what we call preprint servers. So normally, when you publish a scientific article, you write it up, you have to be submitted to a journal. And then there's an editor assigned to it editor goes through it to kind of make sure it's not completely wacko. And then it goes through a process called peer review, where sent out to usually three other scientists in your field, your peers, and they go and they critique it. And they recommend that it's either published as this has to be revised or is rejected. And this is a process that maybe on average, can take between six months and eight months. But it's not uncommon for it to take over a year before it's actually published and out there for the scientific field to go and benefit from. However, there have been what are called preprint servers that have been developed where before you submit it to peer review, like a discus, you'll do an additional step before that you submit the article to a preprint server, it still gets a quick look over from an editor to make sure that it's not something you know, crazy or inappropriate. But then within 24 hours of being submitted, it is online and available for everybody to look at again, it's not peer reviewed yet as this disclaimer forth, but these preprint servers have been amazing. In order to not have this six month, eight month, one year lag, and information being disseminated, and the information is out in 24 hours after being submitted, and obviously, that's very important when you're facing a immediate healthcare crisis of a, a pandemic.
Scott Benner 1:00:20
Do you think that generationally that that researchers have moved along with society thinking, bigger picture? Do you see that as well? Because I mean, listen, if I was going to cure something, I can see, I'm 50 years old, I can see me thinking, I want my name on this, I want people to know, I cured this, I can also see how when we get to COVID, everyone in the lab all over the country in the world are starting to think well, Hell, I could get this too. So I guess maybe we ought to get to work on this. And, you know, like, I could see that kind of breaking the levee have been maybe not caring so much about who gets the credit, but more caring that there's a way to treat. And, and I do but I do wonder like, I look at the like my son's 20, he doesn't have type one. But you know, I look at his generation. And I listen to hear him speak with friends. And it all just feels a little more inclusive when they're talking. And I do wonder, too, if that isn't a little bit of maybe credits, not the most important thing, although, you know, I mean, you know what I'm saying? Like, I'm wondering if things aren't just shifting in general, but what you said about the internet and communication improving is huge. I don't think people think of the internet as, as all that it really is, you know, I think they think of it as making the Xbox work or, you know, being able to send an email. But but it's really fascinating. Jeff, I'm thrilled you came on. Can Oh, let me ask you the question. First, do you think that there's a the community, the scientific communities moving along with maybe the social world,
Jeffrey R. Millman, PhD 1:01:49
I think there's definitely parallels there. And I definitely would say overall, younger and newer faculty tend to use the, like the preprint servers and the early rapid dissemination of information more than senior investigators, I'm not certain how much of that is kind of a different inherent kind of technological aptitudes of younger people and older people overall. Or, you know, if there's the the mentality when it comes to the credits, but but I guess that is an important thing to acknowledge that one of the things that scientists like myself have to balance is that, you know, we all come into it with kind of ultra altruistic views of wanting to benefit. No people, in this case, you know, people with with diabetes is something very, very important to me. So we come up with all sorts of views. But there is a kind of a reality that a scientist needs the face of, you know, being able to have a career and maintain a laboratory, we, you know, we all have to compete, because it all comes down to money, essentially, but not like not like money that we're taking home, to an editor in our bank accounts, but like money in order to actually do the work all scientists, diabetes researchers and all the researchers, we're all competing for a finite amount of research funding that is out there. And thankfully, we have foundation support from you know, jdrf, and American Diabetes Association to allow for them to be more money, focus on diabetes, then there would be otherwise we're just relying on federal money like the, from the National Institutes of Health, but then it is all still finite. And in the end, you still have to as a scientist, you know, compete for these grants and publish papers of sufficient renown. In order to motivate a foundation or government agency to give you the funding, there is a balance that we have to strike, because we want to do good. But we also need to ensure that we are competitive for the money in order in order for us to do the good that we are, you know, striving to accomplish. So when I talk to my trainees in my laboratory about this, I oftentimes will purposely point out that I am thinking about the discussion one way or another, I'm like, okay, we're thinking about we're talking about this right now, in terms of what is the best stuff we can be doing in order to lessen human suffering or improve patient health? And then or switch be like, Okay, well, this is the stuff we need to do in order to ensure that we have funding for the next five years, and the way we approach questions or the steps we might take can be different depending on what is kind of the immediate concern there. If only and we as scientists have to balance all of this, and it's a juggling act, that different scientists perhaps have different durations will come to different answers to? Well,
Scott Benner 1:05:16
I'll tell you what you just said, it's not lost on me at all. Because this podcast, I know, you don't know it, but this podcast helps people. A lot of people understand how to manage their insulin, which brings their time and range, tighter brings their agencies down and gives them better health outcomes. And it's a full time job making this podcast so I take ads on the podcast, and there are some people who think you shouldn't take ads, but to them, I would say, if I didn't have an ad, then I'd have a different job and you wouldn't have this podcast. So you know, at some point, you have to, you know, you have to you got to you got to eat right, you're not you're not rolling around St. Louis in a Lambo. I don't imagine Jeff, right. When you say, when you say you need that money, you need it for equipment, lab space, materials and quality people, right? Like I imagined someone who knows what they're doing cost more than someone who doesn't know what they're doing.
Jeffrey R. Millman, PhD 1:06:08
Right. And it doesn't get good, good, maybe a good distinction to make fair like when like when by my lab gets a research grant from jdrf, or ADA or NIH or whatever, I personally don't get like a raise or anything like I don't take home, I have a salary, I have a set salary. And that set salary is there, no matter if I am doing a good job in terms of curing diabetes, or doing a bad job when it comes to curing diabetes. Or if I bring in big grants or I'm not begging and break the big grants, the amount of money I take home is the same. So I actually don't receive any of the money personally, but you're right, the money, the money all goes to supplies and equipment and the salaries in order to hire people or to train people in my lab in my laboratory. And that's very important as well, that part of my mission here is not just to be you know, coming up with a functional cure for diabetes, but also to be training the next generation of scientists and so I have undergraduate researchers come to my lab and some of them need have financial aid requirements in order to be attending watched in the first place and so I have to pay a portion of that in order to have them have the privilege of being able to do Diabetes Research. Same thing with a PhD students, I have to pay their siphon and their tuition, and also postdoctoral fellows as well. And these are all people that I'm training that are doing the work but I'm hoping are going to be trained to then you know, go on and either companies or in their own academic labs to continue the fight for a cure for diabetes and they but they but they need to if they don't get a salary to be able to do it then they're going to go and do other things like not a big purchase or go work on a different disease area and I'm rather than work on diabetes with me then go and you know, make shampoo at Johnson and Johnson but like I was thinking about doing for a while or you know, go and work on a different disease area, no offense to that disease areas, but my focus is diabetes and so I'm going to compete in order to do the best I can in terms of research and in terms of training in order to advance that as much as possible.
Scott Benner 1:08:36
That really speaks to me what you said honestly, you need quality people who who want to do it and I loved your answer because I want people to hear that I honestly want people to know that you're listening in my estimation, you're a brilliant guy who could be doing other things you could be rolling around a lab working on conditioner, wearing $200 shoes and driving a you know a fat car and and living a completely different life but you're putting your ability to think through these ideas into something as important as diabetes and and I appreciate that I hope other people do as well. I have a couple of quick questions. And I'll let you out here. I know we're over time a little bit different does this have any application what you're working on to type to
Jeffrey R. Millman, PhD 1:09:18
get at the type two situation is a little bit more complicated than type one. But the short answer is yes. The type two type population is more heterogeneous and there are definitely many people maybe even most people with type two diabetes that probably wouldn't benefit from from this because their diabetes is already managed sufficiently with diet and exercise and or with these other you know, drugs like the instances of Tyson drugs. However, I think that in my discussion with endocrinologist backs us up as Well, that's the more severe type two diabetic patients, the ones who are taking insulin like patients Type One Diabetes do as well, they would be able to benefit from it, since you could think about these cells as essentially a insulin production source. And the patients need insulin, then it could become from the cells and set up in the insulin injection, the complication there, which makes it a little bit maybe a little bit more challenging than in the Type One Diabetes case is that most patients with type two diabetes have what's called insulin resistance. And so they per kilogram of or pound the body weights, they require a larger dose of insulin in order to maintain normal blood sugar levels. And so what that would translate over to is that you would be the transplant even more cells into a typical patient with type two diabetes than the typical patient with Type One Diabetes. But that is a hurdle that could be overcome, again, because of the positive features of stem cells in terms of being a self renewing cell source that, you know, we can go and make a few billion cells for them, as opposed to baby 1 billion cells that a patient with Type One Diabetes would need.
Scott Benner 1:11:25
Okay, I see. All right. My last two questions are this one seems kind of outlandish, but are there like you taught a cell how to sense glucose and make insulin? What else could you teach it to do? can it make me taller? Or like what else? Like, you know, I'm saying like, Where's this headed?
Jeffrey R. Millman, PhD 1:11:44
So I guess the way to think about it is that we are only teaching the cells, what evolution already taught the cells, basically, we're not telling them to do anything that is artificial. All we're doing is trying to give them the signals, they would normally get in the developing embryo that would tell them to become a beta cell or is producing cell, all we're doing is trying to copy that inside of the laboratory. So evolution already figured all this stuff out for us. And all we're doing is trying to copy evolutions work in the laboratory. So that means that we have so we do some sort of exotic genetic engineering tricks just possible, I guess, but at least with how we're making the interesting cells, that means that we can't tell the cells instruct the cells to do anything that they wouldn't naturally be able to do in the body. But with that said, I mean, maybe he gives them a growth hormone artificially to go and make you grow taller, and produce insulin, but you're probably better off not doing that. Yeah, I was hoping you could
Scott Benner 1:13:05
fix my plantar fasciitis actually, or, or I could dunk one or the other. I wasn't sure what I was going for exactly there. But I just wanted to understand, you know it. And that's a really great explanation of it, that you can just do what what nature knows how to do, that's, that's really is probably comforting, to be perfectly honest.
Jeffrey R. Millman, PhD 1:13:26
My, my professional advice for you would be to just get the shoes with like platform shoes, or like, get a springboard in order to go and probably to be much more economical for you, then try to use a cell therapy for it. Well,
Scott Benner 1:13:40
Jeff, I was gonna tell you, you could come back on the show whenever you want it if I could jump higher, but now you're making me rethink my offer. Well, so two things. And so I don't forget to say it whenever you were terrific. And I really enjoyed this. So if you ever have anything else you want to say, carpenter, you just let me know. And I guess my last question is then timelines like, what are your What are your hopes for this?
Unknown Speaker 1:14:07
Yeah, I
Jeffrey R. Millman, PhD 1:14:10
you can imagine I dislike the timeline question because, of course, should I be held anything but also because it's very difficult to predict timelines when it comes to any clinical work little than kind of a major novel clinical treatments, like a cell replacement therapy for for diabetes. I am hopeful that in the next few years, we there would be clinical trials that are like could be initiated, and we have been in discussions with a lot of partners in order to make that happen. And that does seem to be very realistic. So I feel pretty good about in the next few years clinical trials could begin. However, I think the bigger question which is a lot harder to answer is, when is this going to be a widespread treatment that the average person with diabetes could have made available for them? And that's simply impossible to know the answer to I've been doing this a long time, I'm not naive enough to ask you that question.
Scott Benner 1:15:31
I was just wondering what you were hoping your next steps were? So what what gets you to those clinical trials? Is it money?
Jeffrey R. Millman, PhD 1:15:37
Money? Yeah, it comes down to money. And that's both in terms of, you know, advancing our technology, but also just doing the necessary steps to translate our kind of, we want to call it a research grade process into an actual clinical grade process, it all comes down to dollars and cents, is it
better? It's,
Scott Benner 1:15:58
I'm sorry, Is this better off in academia? Or would it be better off privatized? What if somebody came along and bought it with this fear be then that they might not follow through the same way, and they'd want to bastardize it for something else? Or, like what gets it done more quickly?
Jeffrey R. Millman, PhD 1:16:13
I think that there are viable paths with either direction. And kind of the fear that you mentioned, when it came to kind of a company involvement, that there are protections that can be put into place to make sure that a company doesn't like swoop up the patents, and then sits on them to prevent a care from actually helping people, Jeff,
Scott Benner 1:16:39
is that I don't mean to cut you off. But is that light bulb story true? You ever heard that, that 100 years ago, a guy designed a light bulb that would never burn out and a light bulb company called him in, bought his patent from him burned everything he brought and broke all the light bulbs right in front of him? Have you ever heard that?
Jeffrey R. Millman, PhD 1:16:56
I have heard that I have no idea if this actually true or not. But I think we I think the the people who manage, like technology portfolios are a lot more savvy than they are 100 years ago. And I guess one of the aspects that we haven't talked about when it comes to to my research here is that in addition to the the core technical team that we have here, Washington University, also has an extensive technology management office here. And their job is to worry about these sorts of things to make sure because obviously, I'm not a patent attorney or lawyer to give me the file past inventions or to figure out licensing deals with, with companies or other entities, I don't know how to do that stuff. It's so washu. And it's pretty true for other major research universities as well have a office that is dedicated to that, in order to protect the interest of the university, but also the interest of the technology. And so this kind of relates to the protections that are put into place to make sure that somebody doesn't go and buy the patent for your light bulb and then destroy everything and make it so it's not available for people you can write, you write in into these contracts, essentially, that the person who license or buys the path that has to proceed with commercialization. And there are very strict deliverables that a licensee has to do in order to continue having the rights the patent, if they do what you said, which is the sit on the patents, then they're in violation of the agreement, and the path that reverts back to Wash U. And in this case, to or the university, whoever holds that the patent rights are originally and then we're able to go and you know, find a partner who was not going to play these, these silly games. Yeah, I guess it's possible, but there are ways of protecting yourself and also protecting the interests of patients. And so this idea that that companies are out there and would never allow for never allow for a cure for diabetes to come. Because they make so much money off of insulin just isn't true there. There isn't any real basis in reality for it. And in fact, I would say that, overall, the companies that that I'm aware of in the space, all view this as being the future and all have at least a small internal program and not a large program to make sure they end up not following The the lesson of like a Kodak, for example, who were the ones who discovered digital photography, and they just decided not to pursue it because their film industry, business was making so much money. But then other people develop digital photography, and Kodak get left in the dust because there's a Kodak and Polaroid Sorry, I forget which one, right, but the film one. So I think that's actually probably the the more relevant analogy here than the than the lightbulb analogy that these companies make money from from insulin and that's true, and you're gonna get arguments that they make too much money from from insulin, as well. But they all believe that the future is cell therapy, and they don't want to be like, Polaroid or Kodak, which whichever company was to, you know, be out of the diabetes business because they didn't adjust your business model with the time
Scott Benner 1:21:00
Well, people are still going to be diagnosed, and they're still going to need this treatment. And they'll just find a way to build this treatment to cover the cost they lost on something else. So it's it. I believe that totally. And I think that, like you said that people are smart enough to see that there are other applications and you want to be involved. So what are we looking for here? Do we need, like Beyonce type money to start getting interested in diabetes? Or do we need Elon Musk? Or what level of wealth? Do we need to get interested in type one for this to move forward? You know, I'm saying like, it's not just like, you know, not like a B level actor, we need something else, right? Who do you think Who's your Who's your dream guy who like wakes up one day, it's like, I care about type one diabetes, all of a sudden,
Jeffrey R. Millman, PhD 1:21:45
I, I don't know that I have a good answer to that. I think that'd be a little bit beyond beyond my paygrade. But Elan Musk, you know, going and, you know, sending being the first private company to send astronauts into space. And yesterday, that rocket with his car to Mars, I'm sure that I'm going to guess the amount of money that went into that would be a good amount of money. That's one day that that would definitely help out quite a bit, though, of course, what he's doing with this company is very, very valuable as well. So I don't have a good number for you. But I can tell you that the number number one limiting factor towards progression, for here, it all comes down to money and the limited amount of money that's there. And especially in the world of COVID-19, for which where, you know, there's a lot less money to go around, both because a lot of money thing rejected COVID-19, again, which is a very important thing, but but also, like foundations overall are raising less money in the economy has slowed down a whole lot. There's less money available overall. And a lot of the traditional diabetes foundations that have been very supportive. In the past, I've had to really clamp down in terms of the amount of money they're giving out right now, because their fundraising has been so small this year, versus that years past. And so it's unfortunate that it does seem that COVID-19 is making it so that we were already in a bad situation where there wasn't enough money for diabetes research. And now there is even less money for diabetes research.
Scott Benner 1:23:28
Alright, so I think you know, what we need to do is whatever that powder is, you give the mice that makes their pancreas stop working, we got to slip some of that into like Joe Rogan's coffee or something like that. I think this is the way to get. I'm obviously
Jeffrey R. Millman, PhD 1:23:40
I don't think I would support that.
Scott Benner 1:23:41
No, I don't either. I'm just being Jeff, I genuinely cannot thank you enough for doing this. And I just want to let you go, because I've kept you much longer than I said I was going to, and thank you. And honestly, if there's any thing you ever want to add, and you found this valuable, please come back on. Yeah, this
Jeffrey R. Millman, PhD 1:24:01
is really my pleasure. I really enjoyed our conversation. And I'm hoping that your audience gets, you know, a little more information about what's going on when it comes to diabetes futures, because it really is exciting. And I think there's a lot of reasons for hope. And I hope that message came across in our discussion. So thank you very much for having me on.
Scott Benner 1:24:17
It's my pleasure. Is there any way they can track your progress online?
Jeffrey R. Millman, PhD 1:24:21
Yeah, so I'm very active on Twitter, at Jeffrey r Millman. So that's usually the first place that any announcements about progress come from from from my lab. And we also have a website that is fairly up to date as well. That is kind of a complicated address. But if you just look up milman lab Wash U it should be the very first result in Google.
Scott Benner 1:24:48
Thanks so much to Dexcom and Omni pod for sponsoring this episode of the Juicebox Podcast. Get your free no obligation demo of the Omni pod tubeless insulin pump at my Omni pod COMM forward slash juice box and learn all you need to know about the dexcom g six continuous glucose monitor@dexcom.com forward slash juice box, lend your support to the T one D exchange at T one d exchange.org forward slash juice box, make an addition to that research and help people with type one diabetes to live better. Don't forget to follow Jeff on Twitter, Jeffrey r Millman I don't normally. What I mean to say, I've seen a lot of people cure a lot of mice of Type One Diabetes over the years. This just felt new, a little different to me. And I thought it was well worth understanding the process that got Jeff and his group to where they are right now. I hope you found it interesting as well. I also really thought it was interesting to hear more about, you know, some of the financial support that research needs and, and how difficult it is to get and the you know, considerations behind Do you want to get a regular company involved in this? Or do you want to keep it academic. I like finding out more about you know, the corners of those stories. I really appreciate what Jeff did today, I thought he was a great Shepherd of information did a really good job of explaining it without over promising or you know, hyping it beyond what it was. I hope you enjoyed it as well. Thanks so much for listening to the Juicebox Podcast for sharing the show. There's a couple of great new reviews up on Apple podcasts in the US and Canada and a couple of other places. I appreciate all you guys taking the time. And thanks again, for sharing the show. Just the other day, the show had its most popular downloaded slash stream day in the history of the show. And it was 25% greater than the last most popular day. And as a matter of fact, over the last four months, the show has bested its downloads every month. It's really growing. That is definitely because of you guys. And I really appreciate it. Last thing, if you're interested in a private Facebook group, for the listeners of the show, one of those exists, just head over to Facebook and search for Juicebox Podcast, it'll pop up Juicebox Podcast colon type one diabetes, that's a private Facebook group, you'll have to answer a couple of easy questions to you know, prove your human being. And then once you're in, you're going to see what is now 5500 users 4000 of them are active every day. It's an amazing Facebook group, maybe one of the biggest anomalies in the world might be more of a crazy thing, this Facebook group then telling a cell to make insulin. And by that I mean people are actually nice on Facebook and helpful and thoughtful and not awfully ego and not always trying to prove people wrong. It's a it's an uncommon Facebook group that I think you might like and if you think you can make an addition to it, please jump in. If you're not looking for that much activity, but you want to keep up with the podcast on Facebook. There's also a bold with insulin public group. And if you're more of an Instagram person you're looking for at Juicebox Podcast. Also, if you're looking for the diabetes pro tip episodes to listen to again or share with a friend and you're finding it difficult to dig them out of you know the many many episodes that are there in your podcast app. I've put them all at diabetes pro tip.com. And of course if you have a great diabetes practitioner or you're looking for one, check out juicebox docs.com. Give a penny take a penny kind of an idea you can leave your great endo for someone else or take someone else's and give them a try.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#381 Brent has a Story
Husband and father of three
Brent shares his 20-year journey as a person with Type 1 diabetes, a husband and father to three young children. After 15 years of manual daily injections and multiple daily finger sticks, Brent switched to a T1D physician in 2015 which has made all the difference in his daily management and overall health. He now uses a continuous glucose monitor and insulin pump and talks about the success he's had using technology for the past five years. Brent offers a laid-back personal perspective on why it's so important to take care of yourself and practice patience when living with T1D.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:09
Hello, everyone, welcome to Episode 381 of the Juicebox Podcast. On today's show, we're gonna be speaking with Brent. Brent has had Type One Diabetes for 20 years. He's been married for a long time and he's got three kids. Brent's progression with Type One Diabetes has been steady but slow. And it's really coming together for him. So he's here to tell you his story. In fact, this is brandstory.
Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making changes to your health care plan. We're becoming bold with insulin. If you're looking for a terrific endocrinologist, or have one that you'd like to share with people, please go to juicebox docs.com. And if you're enjoying the pro tip series of the podcast and like to share that with someone, or if you're looking to see the episodes all in one place, without using your podcast app, you're looking for diabetes pro tip.com.
This episode of The Juicebox Podcast is sponsored by the Contour Next One blood glucose meter, please visit Contour Next one.com Ford slash juice box to learn more about the Contour Next One. There's so much information at this link. I don't even know where you'll begin. But where I'm going to start by telling you about Arden's blood glucose meter, the Contour Next One blood glucose meter is incredibly accurate and cheaply priced. It's actually possible that the test trips purchased directly with cash could be cheaper than what you're paying through your copay with your insurance company, when that'd be interesting. Check it out. While you're there, you're gonna see all of the contour products listed right at the top. There's resources, such as downloadable log books, and the contour diabetes app that works in conjunction with the meter that's available for Apple or Android, it's even possible that you could be eligible for a free Contour Next One meter seriously, you got to go click around on those links. There's a test trip savings card there, it's worth picking around and learning about everything, not just about ardens meter. But if you're in the market for a new meter, I can't say enough good things about the Contour. Next One. It's absolutely been the most accurate meter My daughter has ever used. I'd also like to direct your attention to touched by type one.org. It's a great diabetes organization doing wonderful things with people living with type one diabetes, and they'd love it if you check them out on Facebook, Instagram. We're at touched by type one.org.
Brent 3:30
My name is Brent. I live in Payson, Utah. It's a town about an hour south of Salt Lake. I have had Type One Diabetes for just a tad over 20 years. I've been married for a little over 10 years. As three kids, two boys and a girl. My oldest son is eight. My daughter is four and my youngest son is one almost too
Scott Benner 3:59
bright. Do me a favor that cord with the with the microphone. I try not to brush spider, let it touch your clothes. Okay. Okay, that's all otherwise sounds terrific. And I appreciate you telling us about yourself. How old were you when you were diagnosed?
Brent 4:15
So I was 17 happened over Christmas break of all times. And I believe that was the Christmas break of 1999 to 2000. So I always just go off of 2000 since that's kind of an easy time to remember how long I've had it.
Scott Benner 4:39
Brent, you know what? It's funny. We all put so much effort into being worried about y2k and what would happen to computers and we should have been worried about what was going to happen to your pancreas.
Brent 4:49
Yeah, I had no worries about y2k either, didn't bother me at all.
Scott Benner 4:55
I do remember being in a number of meetings at my job and I just kept thinking I feel like we're making a big deal out of this. And the computers just gonna say it's January 1 2000. Here we go. But such an odd thing. Anyway, tell me about your diagnosis a little bit.
Brent 5:12
Yeah. So, um, you know, my memory is kind of fade a little bit, you know, the other. Yeah. I remember it being a Sunday morning. pretty typical Sunday morning, I'm a, I'm a member of the Church of Jesus Christ of Latter Day Saints growing up here in Utah. But anyways, you know, did my regular thing and getting ready for church and going to church, and I was over there at church, I remember a couple people saying, it looks like you a little thin, and I, I just brushed that comment kind of off, I didn't really think anything of it. And after coming home from church that day, I was not feeling good at all, I just want to lay down and do nothing. Yeah. I was the kind of kid that, you know, wanted to be playing video games all the time, or watching TV or something. But for some reason, I just wanted to lay down and do nothing. I was using the bathroom a ton during the night, I think I got up at least once an hour. But anyways, after church, my parents had noticed that I was just doing nothing. And we had a friend that lived pretty close by who was a doctor. So he came over and kind of checked me out. And he had told my parents that I need go to the hospital. So we went to the hospital. I don't remember other much than checking into the hospital. And, you know, they ran some more tests. And, you know, told me I had diabetes, I had really no idea what that meant. I think I spent the course of the next couple days or three days in the hospital, learning about all I could and how to kind of manage it from there.
Scott Benner 7:20
They won't ever tell you what your blood sugar was, at your time of diagnosis.
Brent 7:24
I don't remember the exact number. But I remember it was over 600. So it was pretty high.
Scott Benner 7:30
That's why you weren't playing video games. Whenever.
Brent 7:33
Yeah, take it right out. I was
Scott Benner 7:36
our bread. Listen, we got it. We've got to dig down on something for a second here. Because since you listened through the entire show, you said in like a month and a half. So you're aware. And I've never been able to put my finger on this yet. But I asked every time to try to get closer to the answer. Why is the show so popular with Mormons? And why do they come on all the time? And like you have to be the sixth? or seventh perhaps? Like you do? Have you heard them as they're as they're talking? Sometimes people don't identify themselves right away. Sometimes I out them for having like, 43 kids or something like that. And I'm like, hey, so, but um, is there anything about the community? That's is diabetes? more prevalent? That doesn't make any sense? But is that possible?
Brent 8:27
I don't think it's any more prevalent around here anyways, I mean, I just I found the podcast, and it seemed really interesting, you know, listening to you and how you talked about your daughter, you know, finding out she had diabetes, and it was just really interesting in it. It hit me because you know, I've had it for at the time, it was only 19 and a half years when I had started listening, but you know, I've had it for 20 years ago. I've really not connected with a lot of other type one diabetics,
Scott Benner 9:01
so maybe it's the opposite maybe. Maybe there's just nobody in Utah. So everybody there needs to find Am I might be the Mitt Romney of type one. Diabetes, podcasting. It's possible. Is this not true? If you were to say that maybe.
Brent 9:14
And I really haven't listened to any other.
Scott Benner 9:19
Just found this one.
Brent 9:20
Yeah, I found this one. And you know, it just
clicked right off and I listened. I really liked it.
Scott Benner 9:26
I would like people of all religions to listen, I'm just telling you that, you know, it just comes up. So frequently. I'm not wondering how many people I've interviewed. Who, who did not tell me? It's possible. I've interviewed 306 people from the church. I don't know. Anyway,
Brent 9:45
I suppose.
Scott Benner 9:47
So how did you find how did you find growing up? And 20 years ago, what kind of technology they started with?
Brent 9:55
Um, so I remember, just syringes and vials. Well, what it was. I've used human log for most of my diabetes life. That's what I used. And I think it was humulin was what the other was called the long acting one.
Scott Benner 10:19
Yeah. What's your most dear? I'm sorry to cut you off? Did your parents jump in and help? Because that's a weird age, it's 17? Or did they do the like, he's a man, he'll handle it. Like, where? Where did that fall? And how did that impact you how, however it went.
Brent 10:34
So I do remember me handling most of it. I mean, my parents, you know, were they were there in the hospital learning about it just as much as I was. But, you know, I'm, I was practically an adult. So, you know, I just pretty much handled everything on my own, you know, short of, you know, setting up doctor's appointments and insurance and that kind of thing. But, you know, managing the diabetes, I pretty much handled it on my own, from what I remember,
Scott Benner 11:07
where you're out where your outcomes, what you were looking for, like, I'm interested how a 17 year old, you know, 20 years ago with some syringes, and some, you know, insulin we don't use anymore. Like, was your health where you wanted it to be? Or was that constant struggle? Or did was it not thought of that way at the time?
Brent 11:27
I honestly don't remember too much about how I did. Way back then I will tell you this. So later that summer later
2000
I got an early graduation gift and my sister also, there's this, I think it's kind of a high school program national throughout the country. It's called people to people, student ambassadors. Have you heard of that?
Scott Benner 11:56
I have not. No. But it was, um, so what it is.
Brent 12:01
Yeah. So what that is, it's a program that's available to youth, basically. And they go on a big trip somewhere around the world and experience
other cultures, okay.
And anyways, so that summer, my parents had bought my sister and I, well, we actually, you know, helped pay for it ourselves to we went into this program, I think our particular group, there was about 30 or 40 youth and, you know, five or six adult leaders. And we went to Scandinavia for three weeks. So here I am, I'm only six months newly diagnosed, I don't remember having any, or not very many worries about my diabetes and taking, you know, all the supplies that needed to go with me. Yeah. They had us keep a journal as part of the kind of the program. And I don't remember writing anything about my diabetes, rather than just everything I was experiencing. Right?
Scott Benner 13:19
Well, is that because the insulin back back then what you were doing is you were shooting insulin a couple times a day at certain times, then making sure to eat at certain times. Is that about it?
Brent 13:29
Yeah. So you know, I was doing my normal meal time. boluses, if you will, you know, take the insulin for meals. And then I was doing the human, I believe, a shot in the morning and then shot at night.
Scott Benner 13:42
And how do you find, like, how you manage now, compared to that. So how do you manage now?
Brent 13:49
I have been using a pub since 2015, a tandem pump. And I'm actually just got started on my second tandem pump. Just this past November,
Scott Benner 14:01
so you were 1616 years on in on MDI.
Brent 14:05
Yes, yes, that is. That is correct. I did. Okay. I won't say I did gray. And this might have been around maybe 2005. My blood sugar's were or my Avon See, I would say was probably between 10 and 13. So I mean, it wasn't the greatest right. And I wonder, I mean, I was also the doctor I was seeing was just a family physician. So it wasn't anybody specialized in diabetes. But it eventually turned to a point where he recommended me to diabetes doctor and I was able to reduce my agency a bit with I think I got it down between nine and 10%. So I mean, that was a pretty significant increase.
Scott Benner 15:00
Yeah, I mean, you moved it from what? Like more like, and was it swinging around like 10 1112? Like, or did you not? Check? How often were you checking it? I guess it's my question.
Brent 15:12
I was probably the only checking three times a day, I would guess
Scott Benner 15:15
your blood sugar three times a day. And did you go to an endo appointment quarterly? Or was it not that frequent?
Unknown Speaker 15:21
Um,
Brent 15:23
I mean, with the family physician, I think it might have been
maybe every three to six months. So maybe quarterly
Scott Benner 15:31
sees now you've listened to the podcast straight through, as you're listening. Do you think wow, the way people are doing it now is no, it's just not close to what I was doing growing up. Did you have that thought ever while you were listening?
Brent 15:43
I've had it a few times. I mean, it's understandable to me. No, that was 20 years ago. So I mean, things were a lot different back 20 years ago.
Scott Benner 15:54
Yeah. million percent.
Brent 15:56
Definitely blood sugar machines. I, when I was first started, I used a lot of one touch machines. And the first one I had thing was huge. And test trip was huge. And it required tons of blood compared to blood sugar machines today.
Scott Benner 16:17
Do you think that was that part of the impediment around testing more? Or was there just not an onus on testing more? Nobody was like you were testing enough for your doctor?
Brent 16:26
I think I was testing enough for my doctor.
Scott Benner 16:28
Friend. What about for you though? Like, were you? Like, how did you feel with a onesies that were that high? Was it an impediment? Did your body adjust to it? Is it something you look back on now and worry about?
Brent 16:43
I mean, yeah, I do worry about it. I mean, obviously, that's not a great a one C and, and whatnot. But I mean,
I'm still alive today,
Scott Benner 16:54
I really appreciate you being on because I mean, the podcast is five years old. So you're talking to people who are mostly brought up around faster acting insulin, you know, their carb counting, covering meals, you know, testing more frequently, we're in glucose monitors. That's the kind of stuff. And I think that people sometimes make the mistake of believing that that's just how it's how it is how it's always been. And, you know, like, that's it. And even today, there are more people in the world with diabetes, who have a story, it's like yours, then a story like theirs. But then those people who are listening going, Oh my gosh, like, you know, my one sees in the sevens and I'm always wanting to get it down. And, you know, like, I know what my blood sugar is all the time, etc. I think we all need to really remember that most people don't have access to good information, tools, and sometimes, you know, even, you know, the meters and the glucose monitors and the pumps and etc. Even smartphones, you know, it's easy to like, get caught in a bubble and think that this is how it is. But I think it's more the way you're describing honestly.
Brent 18:05
Yeah, most certainly as I mean.
Yeah, sorry. I lost my train of thought.
Scott Benner 18:15
up early in the morning. What time is it there?
Brent 18:17
It's a
it's just after seven. I get up at 530 here because I actually start work normally at
Scott Benner 18:25
seven o'clock. Oh, no kidding. You work from home or you.
Brent 18:28
I actually work I commute. I've got about a half an hour
Scott Benner 18:32
ish commute. I appreciate you making time for this. I really do.
Brent 18:36
Yeah. I felt this was pretty important. So I
Scott Benner 18:40
Well, what did you ask? You asked you asked for time off for this.
Brent 18:45
I just told him I was gonna come in later. Oh,
Unknown Speaker 18:47
thank you very much.
Brent 18:48
Look at this, this and I still work my normal time is the level of
Scott Benner 18:52
dedication. Brian, I expect from everyone listening to the show, just you know, Brent, listen to all of the episodes. He didn't say, Oh, I didn't think that one would be interesting. I don't want to hear that from you. People listen all the way through. And if I need you to get up early to be on the podcast, that's just what you have to do. Just kidding, from what what made it feel important to be on the podcast.
Brent 19:13
I just, you know, I just wanted to share my story, you know, hear, you know, let the listeners hear kind of another. Another story. I mean, that's what got me into this podcast, was hearing your daughter's story. And you know, to change in yours, your life, her life, your whole family's life. Just you know, having another point of view, basically. Yeah.
Scott Benner 19:40
So did it help you more like spiritually, like psychologically or was it helpful management wise or what did you what what's happened after hearing all those experiences,
Brent 19:51
I would say all the above. I mean, it's, you know, I think I've tried to get myself more involved with Other type one diabetics, and it's kind of even listening to this podcast. And you know, it's just kind of helped me even reflect on myself and how I manage my own diabetes.
Scott Benner 20:14
Were you meeting people? Is it online? or in person?
Brent 20:18
Yeah, it's mainly through Facebook groups and stuff.
Yeah, that's kind of the the main part.
I have some family that's got type one diabetes, and some pretty close friends that has it. But you know, aside from that, it's mainly been just online.
Scott Benner 20:40
Yeah. Do you find yourself talking about it more since you've listened? Or have you always been kind of open and conversational about it?
Brent 20:49
I've been pretty open about talking about it. But I think I, I do feel like I have been more open to talking about my diabetes to people since I have been listening to the podcast.
Scott Benner 21:01
Okay. That's excellent. Well, one second, Arden is asking me a question.
Unknown Speaker 21:08
Let's see,
Scott Benner 21:10
the blood sugar got a little low. And she's in class. She's trying to treat it already. But her blood sugar hasn't popped back up yet. And she's just like, my phone won't shut up. So she's had this very interesting, this is ridiculous. Solar people, you know, what, most likely? And then all the everything I gave her as you know, hey, try this or this. She is not right now. So why are you telling me about the phone? If you're not willing to Alright, listen, let's not try to make sense of children, I guess. So, her blood sugars have just required less insulin for the last over a week now. And at first, I know everybody's gonna laugh at me. But our What is this? What is this?
Unknown Speaker 22:05
What? Oh,
Scott Benner 22:08
I don't have a January electric statement. That's not why they're calling they're lying to me. Sorry about that. So her blood sugar's have been lower. And everyone's gonna laugh, because, you know, I always say like, don't just say they're sick. I think they're getting a cold. But when Arden has certain kinds of illnesses, her blood sugar just is easier to control. She needs less insulin. It's always been that way. So when this happened, we just assumed that's what was happening. We started cutting insulin back, you know, the way we normally do, but it still wasn't helping. And she was, you know, still just lower, lower, lower, lower, but she'd also kind of lost her appetite. So we thought, all right, we've made it even worse, you know, you couldn't, you know, she doesn't want to eat a whole lot. You know, you're trying to Bolus you don't really know how much to do. So her blood sugar's been a little up and down for the last few days. And finally, last night, I thought, what if so Arden just recently got an infusion of iron. And her her ferritin level was very low, which happens to me too, and it happened to her. So she'd been tired and rundown and is going on for a long time. And through the process of trying to diagnose this. We went through a lot of different things, one of them being thinking it was her hypothyroid medication, because the symptoms of low iron and hypothyroidism, so perfectly match each other that that made sense. So, yes, you know what I mean? So we lost a lot of time and art and spent a lot of time feeling rundown. And now she's had the iron for a month or so. And you can see her changing, like, she's got more energy, she's not as tired, she looks better, you know, like all the stuffs happening. Right? But she doesn't feel perfect yet, which we didn't expect and even the doctor that she saw, who was the hematologist told her Listen, it's going to take two to three months for you to feel the complete effects of this iron transfusion. Or infusion, excuse me. And you know, so in you know, he told her like two more months from now, however good you feel, then that's how good you're gonna feel from this. But I started wondering out loud yesterday with Kelly. Is it possible that as her cells are dying off and regenerating, but regenerating now being built from building blocks that have the correct amount of iron and ferritin in them? That's how she's feeling better, but could that be why her insulin needs have been higher? Because Arden's bazel rate is significantly higher than I would expect it to be. And it's not just like around food, like you're a grown man. What's your base rate?
Brent 24:46
Um, varies.
I mean, I have a schedule but I think it's anywhere between point nine an hour to 1.3 an hour
Scott Benner 24:57
right? So my hundred and 40 pounds daughter who's 15 her basal rate during the day has been 2.6. Wow. Right. And so that's just a lot.
Unknown Speaker 25:09
And now that is Yeah.
Scott Benner 25:10
So all of a sudden, yesterday, I was like, Oh my gosh, this isn't a thing, maybe that's going to go away. Like, we're gonna have to adjust to this. Maybe forever. And let's try. So I paired all of her settings down pretty significantly, had a lot of success overnight. But of course, this was my first day time with it. And she got the school and it's just, you know, it was doing great, doing great. And then all of a sudden, it dropped down. And now it just does not seem to want to move again. So that is, yeah, that's
Brent 25:44
interesting. Hold on a second.
Scott Benner 25:55
So I'm gonna get her to test and we're gonna check it out. not know, who knows, I could end up being wrong about this. And three days from now, her blood sugar's might go right back to the way they were, I don't know. But it's a significant difference in the amount of insulin she needs, like significant.
Brent 26:14
Yeah, well, hopefully she gets her numbers back to where they should be. And hopefully to get that figured out.
Scott Benner 26:20
Yeah, I appreciate that. I do. So first, so how do you find pumping versus how you were doing it for so long, because I'm it's very, it's very much interesting to talk to somebody who basically lived a lifetime not using an insulin pump, and now uses one.
Brent 26:36
I love it. I will say that right off, it's great. I don't know how I lived without it.
Unknown Speaker 26:42
Um,
Brent 26:43
so back in 2015, that's when my daughter was born. Okay. And she had some complications with being born that year, and she ended up being in the Nikki for 18 or 19 days, which, you know, that's traumatic in itself. But, you know, towards the end of the year, I had started researching pumps, what pumps I want to use, which one I think is going to be the best for me. I should say, a few years before that. I ended up switching doctors to a another one up in Salt Lake who has type one diabetes himself. And I actually still see him to this day. He's the best. I think it's, you know, if you can find a doctor that has type one diabetes themselves, I don't know if you're gonna get any better than that. Because they have. They understand everything. They have a different perspective than somebody who doesn't, if that makes sense. Oh, of course.
But anyways, so 2015.
I had researched a few different pumps, I didn't even considered Omni pod. And I think I was considering another Medtronic one. But I finally emailed my doctor and saying, here's what I'm looking at. I'm looking at this Medtronic pump. I think I will really like it because it talked with my glucose meter. I think it was the Contour. Next One link or something. had talked Bluetooth with it anyways, anyways, I emailed him, he actually recommended that I also look into CGM. And I actually hadn't even heard of it, which was
quite interesting, I guess.
Scott Benner 28:49
Well, you had no contact with people with diabetes. Right. So yeah, I wouldn't have heard.
Brent 28:54
I mean, I didn't really know anything. I mean, I knew what an insulin pump was. But he recommended two pumps for me. He had first mentioned the Animas five, which I don't think is even available anymore. Because it integrated with dexcom CGM. Oh, and the first thing he had told me is, he wouldn't recommend me doing the Medtronic team because they're CGM, he says wasn't very good. He outright said the dexcom is the best. And, you know, his opinion kind of kind of changed my mind pretty quickly, just because I trusted him and I knew him pretty well. Um, the other pump he recommended was the tandem t slim g4 at the time is what it was, and it was going to be integrating with Dexcom soon and that's the font that I chose. ended up using So I've been with Dexcom since g4.
Scott Benner 30:03
Yeah, cuz that animus vibe, how did that work with the g4 back then? Did they act? They didn't actually speak to each other? Did they? Or they did it. Oh, you know what it was, you could see your CGM data on your pump. Is that right? Yes.
Brent 30:15
But it was
Scott Benner 30:16
That's correct. It wasn't telling it what to do like a closed loop or like, no algorithm or anything like that right now.
Brent 30:21
Nothing like that. Um, I believe you were required to calibrate every
Scott Benner 30:28
12 hours, I believe how I remember it. So.
Brent 30:31
Um, yeah, the pump didn't do anything based off any other readings other than just showing you constantly what your blood sugar was, which was huge. I mean, poking my fingers for 15 years, 16 years, or whatever it was got a little. Yeah, I mean, my fingers. Were pretty callous. So you were
Scott Benner 30:56
you're like, you probably had those fingers, like you saw like people see sometimes online, which, you know, more newly diagnosed, people don't know from but those hard bumps all like everywhere, because you're constantly looking for space on your fingers. And eventually, after years, years, years, they just don't heal as quickly. And it's, it's Stark, right, like you can see it when you're looking.
Brent 31:17
Yeah.
Scott Benner 31:18
Can I ask how that? How did that affect tactilely? like touching things and lifting things? Did it have an
Brent 31:23
impact on that? I didn't seem to notice too much.
I don't know if this was the right thing to do. But I would sometimes take fingernail clippers and try and kind of cut away the callus a little bit. Take
Scott Benner 31:40
them away. You're doing your own landscaping there on your on your
Brent 31:45
Yeah, I did that every once in a while? I don't know.
Scott Benner 31:48
Don't worry, Brent, we will cover that with nothing on the Juicebox Podcast is considered advice. So that's funny, it worked, right? Hey, I guess whatever works, right? diabetes is a lot about, you know, making adjustments on the go and sort of, you know, being your own MacGyver and figuring things out, you know, for you. Yeah.
Unknown Speaker 32:08
Yeah, and
Scott Benner 32:09
I mean, two more things that you made up during this episode, you're gonna be the Mormon MacGyver Just so you know, on the
Unknown Speaker 32:15
on the episode.
Scott Benner 32:18
So, hey, listen, tell me a little bit about having kids when you have type one,
Brent 32:21
it didn't really bother me at all. I mean, I didn't really think of it much. I mean, I know the symptoms, I know what to do with, you know, we we find out things. Luckily, all three of my kids are, are not type one diabetics. But you know, what, if they were, I'm not going to love them any less, and I'm going to know how to help them. And you know, I'm going to be able to basically coach them through it. That kind of thing. If they were,
Scott Benner 32:56
you'd have a leg up, you're kind of if your children ended up with diabetes, it would sort of be like what you were saying about seeing a doctor who has type one, it's just an extra level of understanding.
Brent 33:06
Yeah, it's an extra level of care.
Scott Benner 33:09
Yeah. That's excellent. That's wonderful. Well, what are your goals? Now that you're pumping? And you have a glucose monitor? What do you like? Do you have goals with your agency? Or how do you think of it? Because you are coming from an old school idea of this? So I'm interested in, in what you're doing now?
Brent 33:26
Absolutely. I mean, I see my endocrinologist every quarter, still every three months. And we have a goal of keeping it well below 7%. I usually do that pretty good. My last day when see. I was 6.7. I have been as low as 6.3. before. But you know, just basically under 7% is kind of the the goal with that.
Scott Benner 34:03
Does it fluctuate greatly? quarter to quarter?
Brent 34:07
Ah, not usually. It's usually pretty close between I'd say it's usually between six five and six, eight. Okay. You know, that's that's pretty good. And definitely a huge improvement over when I first started,
Scott Benner 34:23
right? Oh, no.
Brent 34:26
Yeah, I stay pretty consistently. Pretty close to that. The only exception was last year when I was in between jobs. I didn't have a month of Dexcom Okay. And it was just interesting to see how much it affected my pay one see and bloods here without having that for a month. I think my name once he got to 7.5 not horrible. But I mean, I haven't hadn't been over seven for
years.
Scott Benner 34:59
So you You moved anywhere from a half to a full point just from losing your glucose monitor for one month. Yeah, the CGM, the Dexcom. What did that change for you not having it? Like, do you remember that feeling of like, what what's gonna happen to me? I'm losing my CGM. How do I go back to what I was doing before?
Brent 35:19
Yeah, I was part of some groups on Facebook and an app called help around which, you know, it's type one diabetics, you know, trying to help each other giving them supplies and that kind of thing. I was almost in a panic to try and find some supplies that somebody can give me. Yeah, just because, you know, I hadn't been without a CGM for years. Right. And, you know, I didn't end up finding anything, unfortunately. I mean, I got some supplies, but they didn't end up working. I even went back as far as trying to find some GE for supplies, just so I could see my graph you were just gonna see right, it's going on.
Scott Benner 36:04
Listen, your your, your unemployment story is much better than most people's, you're only out of work for a month.
Brent 36:11
Um, so I wasn't out of work. So what happened was, I had switched jobs. February last year, and insurance would kick in until I had been there 90 days, I think. And I had enough of my leftover CGM supply to last for for two months. But then I had that third month where I wasn't gonna go pay out of pocket for the supplies, either. I had plenty of pump supplies. So I didn't have to get off of that. Luckily,
Scott Benner 36:44
can I ask you a question now that you've been through it and not asking, you know, for your your financial situation, but now having done it? Do you wish you would have paid cash for the month?
Brent 36:59
I wish I would have had the cash to pay for
Scott Benner 37:01
it. Right. Right.
Brent 37:04
But I mean, you know, what? Living a month without it. I, you know, came down to I lived 15 years without it. What's a bond can make it 30 days, right?
Scott Benner 37:17
So, can you tell me a little bit about like your health and your your how you physically feel? Do you? Do you have a comparison how you are living now versus how you were living then? And the impact that has on you? Um,
Brent 37:34
I'm not sure that I really notice a whole lot of difference. I mean, I'm not very active than the first
place, which, you know, it's
just something I never get around to running a
Scott Benner 37:48
marathon. But no, so you so it's likely that you began at a higher a one C and kept it steady. So you then your body adapts, and you don't feel the higher blood sugar. Did you feel it when it was coming down when you made the changes?
Brent 38:04
Yeah, I mean, I've I definitely feel my highs and I mean, I, I think I started feeling groggy, you know, 200 and above. And I can tell when I'm high without even having to look at my CGM. I do because that's what I do. Because I look at it pretty often. And I can, yeah, there's a big difference between high and low. I can definitely feel feel that.
Scott Benner 38:38
You just said something I want to ask you about you said you look at your CGM. Often, I was just speaking somewhere this weekend. And someone said to me, how do I stop myself from looking at this data? And I said, I said lower your high alarm? Because then you won't have to wonder if your blood sugar is getting high. It will tell you and then when you're not getting high, you won't think the look. So it made me wonder what your high alarm setup.
Brent 39:05
I have my high alarm set at 180. So anything above 180
Unknown Speaker 39:11
you get a good alarm.
Scott Benner 39:12
But prior to the alarms you find yourself checking.
Brent 39:15
I mean, I look at it fairly often. So I looked at it a few different ways. I have it I have the app on my phone. I have an iPhone. I also use sugar mate. I don't know if you've heard of that. I know
Scott Benner 39:28
sugar mate.
Brent 39:30
I use a Mac app on my work computer computers at home so I can up in the top I can see what my blood sugar is what it's doing
Scott Benner 39:41
Luca gram Is that what it's called? Yeah,
Brent 39:43
yep. I think it's a
sugar may glance or something.
Scott Benner 39:49
Okay. Okay. Oh, I know that one too. All right.
Brent 39:53
But I mean, I just have it everywhere. I have it on my palms. I just see Ever I mean, I'm not sitting there staring at it.
Scott Benner 40:04
No, I understand you're not No, I get that. But what do you see my point, though, that if you, if you know, the alarms going to sound prior to it becoming a problem than it, then you just realize I'll hear the alarm, I don't need to look at it, it'll tell me when it gets there. And that, I think that takes away a level of involvement. And there's also terrific research that says that the lower you bring down your high Dexcom alarm, the lower your a one C will go, because I'm gonna say it here just so other people can hear. But I know you've listened to the podcast already. But the sooner you react to a high or an impending high, the less insulin you need to stop it, most of the time, when you use less insulin, you're less likely to have a low later, and you can bring a 120 for instance, back to a 90 quicker with less insulin, then you can affect the 180. And so it's sort of like a little effort up front to lose all that other stuff. And it just it's a it's a matter of putting your effort in what I think of is a better place, but I'm not telling you how to live your life. But just that's how I do it. I don't know if you see any sense in that or not?
Brent 41:18
Yeah, no, no, I definitely do. It does make sense and whatnot. I know, one eight is just kind of weird. My doctor and I have figured is a good spot to know to have the alerts or not. I keep my phone on silent at work. So it's not
Unknown Speaker 41:39
blaring off vibrates for you.
Brent 41:41
And that kind of thing. And even at home sometimes. But I with my pump, I also get vibrates on my bump when it you know, tire blow as well. So I mean, I have another alert for you? Well,
Scott Benner 41:57
well, let me add one more thought to it is that if you if you as you bring the alert down, you sort of will start using insulin differently in a way that you don't recognize. Exactly. Right. And so eventually you don't find one at anymore, I would tell you for certain that what most people consider a 302 B. That's what I consider 180. Like that feeling you have when you see 300 is what I see. That's how I feel at one ad because we so infrequently see one ad? Oh, yeah, like a high blood sugar here would be like 160. And it's not because we're more involved. I actually think in a weird way, it's because we're less involved. But when we're involved, we're using more of the what you might consider to be the correct amount of insulin for the situation. And you only learn that through experience after experience. So I'm just here's what I'm telling you. Right. I think if you move your low alarm to 150 for a month, and then move it to 130. After that the next time you get your a one c check, there'll be a point lower. Right, I would definitely think that and I would think you wouldn't look at your CGM as much a month or two after that. But that's just that. That's my guess out loud.
Brent 43:14
Yeah, so. So I got my new tendon pump this last November. Okay. And it had it came with the bass like you I'm sure you hadn't
Scott Benner 43:26
heard that shut the bezel off yet. Well,
Brent 43:29
yep. And so actually, I just upgraded or updated my software to control IQ just last week, actually,
Scott Benner 43:38
five days ago. And this is a closed loop system. Not Not really. It doesn't have glucagon in it, but it's it's an algorithm.
Brent 43:45
Yes, yeah. So you know, if my blood sugar gets too high, it increases basal and can even deliver an automatic correction automatic correction bolus.
Scott Benner 43:55
Yeah. How are you finding? Um,
Brent 43:58
it's going pretty well. I mean, is it perfect? Of course not. Nothing's perfect. I mean, my blood sugar still gets high a little bit sometimes. And I'm still still learning it. You know, I'm only five days into it
Scott Benner 44:12
is a big adjustment. So yeah, yeah, you're not gonna have it in five days? That's for certain.
Brent 44:16
Yeah, you know, I, I would say, you know, give it at least a month to Ghana. Start, you know, to learn
Scott Benner 44:23
on Friday this, it's funny, because you and I are recording this and what February. And in all honesty, this might be out in August. But tomorrow, I'm interviewing somebody who's going to talk about control IQ to, and he's actually been using it longer. I think she was part of a study. So she might have a little more insight about it. But I think that, you know, I can tell you that from the algorithm stuff that we've done is that it's you know, so much about the settings being correct, so that the algorithm can can make good decisions, right? Yeah, I'm sure you'll find your way with it. Do you Do you have an expectation that it will bring your a one seat down? Is that your hope? Or are you just looking to be less involved?
Brent 45:06
Um, I'm hoping that's going to help with my agency. I'm kind of hoping that down, I mean, not that I've been in a horrible a one seat position. But you know, I've also looked forward to not having to manage it as well. And it's kind of nice that it's got a little bit of automatic
kind of control with it.
I believe it states on their website, you know, that control IQ is helping to lessen the burden on man engine diabetes. Yeah, but it does not replace an active role in taking care of it.
Scott Benner 45:52
It's 100% true, but it's my experience. And from everyone I've spoken to so far. If you're, if anyone is expecting an algorithm pump to just make diabetes disappear out of your life, I'm afraid that's not what's gonna happen. But it should, for people with higher like, imagine, you know, past, you know, Brent, from five years ago, having this thing slapped on him with a 12, a one C. And all the sudden, without really understanding anything else about diabetes, or a one c dropping, you know, five points into the sevens, that would be a absolute, you know, miracle for you. And yeah, and so it's going to be for so many of those people that we talked about, you know, at the beginning, people who just not as involved with management, and understanding, you know, the kind of the tools that that help your blood sugar be lower and stable. And the other thing is, and I'm wondering, even in five days, if you've seen this, is it helping your variability? Are you staying more stable?
Brent 46:45
I yes, I have been seeing more stability and less spiking and that kind of stuff. The last 24 hours within the exception of the last tool, any 30 minutes.
My blood sugar
has been pretty flat.
Scott Benner 47:08
Lovely, flat, where where's it flat? At? What number?
Brent 47:11
Um, so just in range, basically. So I have two ranges during the day. I'm 70 to 180. And then at night, I'm 80 to 150.
Scott Benner 47:24
Okay. Yeah. overnights. easier because you're not eating I guess. Yeah.
Brent 47:30
You mean, boosted shouldn't be
Scott Benner 47:33
erratically, right?
Brent 47:35
Yes, theoretically. But yeah, it. I mean, the last 24 hours on my pump here looks really good. I mean, there was only one time where it went high for about 10 minutes, and then it came right back down.
Scott Benner 47:54
So went over went over 184 unit got it back under again.
Brent 47:58
Yeah, yeah. And I think that was also some help with Bolus to that I did on my part, to say
Scott Benner 48:04
this thing's only manipulating your basal insulin right? It's not sending boluses through.
Brent 48:09
It can send an automatic correction bolus
of what it calculates it only I think it can remember from the training video, I think it says it does up to a 60% of the calculated needed bolus. Okay, but it can only do that once every hour.
Scott Benner 48:28
Okay, that doesn't sound bad at all to me.
Brent 48:32
No, no, it's actually really great. But it does mainly adjust the basal rate. Yeah, increase it or decrease it or completely stop it. Have you
Scott Benner 48:43
had any lows in the last five days?
Brent 48:46
I have had some lows. They haven't been horrible.
I think I've only gotten down to
55 the lowest right?
Scott Benner 48:58
So did you in the beginning think oh control? Like he was never gonna let me get low. I'll let me see what it does. And then you got low. Are you gonna intervene in the future, I guess is what I'm asking.
Brent 49:09
I mean, I know it won't prevent everything. And you know, he can only do so much. For instance, if I take way too much of a bolus of my blood sugar is dropping fast. It can only prevent so much. I mean, if there's way too much insulin on board, it's not going to be able to stop it all the way. The hard thing for me and this has actually been true with basal IQ two is not eating well. It's not true. Just basal IQ it's just been most of my life actually not eating one too many glucose tablets or, or that kind of thing to, you know, shoot you up higher than what you were hoping for. Yeah, kind of thing. But I mean the biggest adjustment with control IQ and basal IQ as well is you know that it It's also working to bring to help your blood sugar get up to that to the area that you need to be, and it's hard to not want to just chomp chomp chomp down on stuff, or,
you know, juice box or whatever.
So you don't go get too low.
Scott Benner 50:23
Is that feeling? Or is that a physical feeling when you when you can't stop?
Brent 50:29
It's been both. I mean, you know, when you start getting below 50, you start kind of getting that panic almost that it's like, I just need to eat sugar and sugar and sugar and sugar. And so I can get that right up in that pan thing. And then you know, it goes the other way. And then you kind of start taking more insulin to bring it back down into range.
Scott Benner 50:52
Yeah, but you feel like a physical need to eat. Is that correct?
Brent 50:57
Yes. I mean,
when I go low, you know, I feel First of all, I feel just different. I don't know how to explain it to somebody that's not a diabetic. Um,
Scott Benner 51:15
I had, let me ask you a question I had, I put up an episode just today with a girl named Aggie, and she's from hungry. And she said, she said that, when she gets low, her thoughts make sense in her head. But when she speaks them, they don't make sense to other people. It's like she like she's not saying what she thinks she's saying. But, but in her mind. She's right. So she can't get her thoughts that come out of her mouth. Has that ever happened to you?
Brent 51:44
Um, I don't think it's ever happened to me. I mean, I'm not saying that it won't ever happen.
But I mean, it's just I kind of
I know and I, I keep glucose tablets on me in my pocket all the time. So I always just
had popcorn out, put some in my mouth. And
it's, it's hard waiting for your blood sugar to go up to and not to continue just chomping down on the glucose tablets or whatever.
Scott Benner 52:16
Yeah, it's hard to wait. It's hard to wait I, I actually said in a in my talk this weekend. I was like, sometimes you just have to have the balls to wait. Like, you just have to be able to just wait a little bit. Because if you do, and you're you know, working off of you're like, don't get me wrong, not the first time you're, you're low. But once you've got a historical knowledge of how this works, and you've done the right things, and you're looking at your data, and your data is suggesting to you that this is going the way you expect it to that's the moment when you have to be able to say okay, let me just stop for a second. Let this Let this be and see what happens for a moment. Yeah, you know, it's a tough it's a tough decision to make, but it keeps you off the roller coaster. And there's nothing more true than you know, the thing that causes lows more than anything are highs. So if you you know, if you don't get high, it's sometimes it's it keeps you from getting low later. I don't think people think of it that way. Sometimes. I hear your kids are milling around. Are they all up? Or just yeah,
Brent 53:17
I'm
on my boys. My eight year olds come down a couple of times.
Scott Benner 53:22
He wasn't gonna make it much longer.
Brent 53:26
Yeah, he's got schooling a little while too. So I hope he's got enough.
Scott Benner 53:31
Listen, it's not your fault. You're busy. Hey, listen, any more plans for more kids?
Unknown Speaker 53:37
Um,
Brent 53:39
I think we're kind of hoping to still have one more. One more. Sure.
Unknown Speaker 53:41
Yeah.
Scott Benner 53:44
Four Sounds Sounds like a lot of work.
Brent 53:47
threes a lot of work.
Scott Benner 53:50
would better be worth it? Cuz if it's not worth it? What are you gonna Imagine if you said to me, Scott, I have three. It's a lot of work. And to be honest with you. I don't think it's worth it. I mean, that would be sad. Now, I think
Brent 54:03
yes, it would be sad. Yeah. No,
Scott Benner 54:05
I I agree with you. I there are definitely days where I wish I had more kids. Last night, I went into Arden's room where she was collecting her clothing she's grown out of and she's got a plan to sell it online. Mostly because I don't think she worked very often. And you know, she's she's telling me about her plan to make money. I said, so you're gonna take the clothes I bought and sell them for less money than I paid for him. I said, Why don't you just not buy clothes and steal out of my wallet? Wouldn't that go quicker? But But uh, but but she's I was looking at her and I thought that is, Oh, that's a woman standing in front of me a young woman, right, like, and I said, Come here, give me a hug. And I hugged her and she's like, why are you hugging me? I said, you look older. And I just want to hug you for a second before you look older again. So you're in a really sweet spot with your kids. eight, four and one. I hope you I hope you enjoy all that because There's no no no bullshit, man, it goes fast.
Brent 55:04
I tried to enjoy it. I'm not, you know,
I have ups and downs.
Scott Benner 55:09
Yeah, please. I had little kids, I know the downs. That's amazing. I They're so adorable in the background, you're gonna make people get pregnant. Right? If you if you keep hearing that they can't see what a pain your kids are they just think they're adorable because they're listening. Well, did we not? Did we? Is there anything we didn't say that you were hoping we were talking about?
Brent 55:31
Um, it's funny, I actually, like wrote out my whole story and tried to kind of figure out what I should talk about. Um,
let me just look over some things real quick.
Scott Benner 55:46
I can't wait to hear what you wrote down that we missed. Um, but Brent, honestly, I'm not bad at this, we probably got the most of it. Right.
Brent 55:55
Yeah, no, we definitely have.
I do want to say, you know,
taking care of yourself is very important. You know, especially if you have a family and kids, you know, you want to be around as long as possible. It's important to kind of, you know, take care of yourself, you know, do your best don't beat yourself up for not being perfect, because nobody's perfect. Even with the technology that's out there. Yeah, that's a
Scott Benner 56:29
damn good life lesson. And then it's, I think, 100% true. I mean, I can't speak to it from personal experience, obviously. But from talking to so many people, it feels like that. It wouldn't be difficult for diabetes to overwhelm you, and get the better of you and start feeling like, this is just my life. I can't do any better than this. And it's what's going to be is going to be but I, I really do think you can affect it. So and being positive about it is a is a good first step.
Brent 56:59
Yes, definitely. And and another thing is Be patient. things take time to learn. And that kind of thing I see on Facebook groups all the time, people complaining about everything that goes wrong and whatnot. Both with you know, Dexcom and tandem stuff. Things happen. But a lot of the time they don't happen as much as
Scott Benner 57:23
it looks like it does on Facebook. Yeah, no, Facebook is not to complain. It's not. People don't pop on to go, Oh, my God, everything's going so great. Let me tell you about it.
Brent 57:31
Yeah, yeah, I can tell you was quite an interesting time on Facebook. When Dexcom had their outage a month or two ago, whenever
Scott Benner 57:40
I spoke about it, too. It was interesting.
Brent 57:42
It was just so sad to see all the negativity
out there.
Scott Benner 57:50
Right away, you're thinking, yeah, this thing that's doing this amazing thing for me, you know, and not that you don't want it to do better, and not that the company doesn't want to, you know, fill in gaps when it has them. But yeah, it's it's interesting to see how quickly someone can turn on you. Yes. It really does give you that feeling like, wow, you know, watch my back. Because five seconds ago, I saw this little avatar with this name next to it saying, Next comes the greatest thing that ever happened to me. And three hours into the share not working correctly, which by the way, didn't mean the Dexcom wasn't working. The Dexcom was working fine. It was just, it was the sheer function. And you might have thought that Well, you know what, I heard less people upset when Australia was on fire. So seriously, you would think that would make people upset? No.
Unknown Speaker 58:36
Yeah.
Scott Benner 58:38
Now that's this is where this is where everybody gets upset. But now I hear you. So to just really do your best. Now you're not gonna think about having four kids. And so, but yeah, do your best, right. And it takes time yet sometimes you have to experience things going wrong. So you know what it looks like when they go right. You know how to make them go that way? It just takes time. Like it really does. Yes, it does. Yeah. Not being dramatic and getting frustrated. If you can help. It is a big hump. All right. Listen, you go make those kids smarter by sending them to school. I will you be very happy. I didn't have time to ask you about your magic underwear because I still want to understand it better than I do. And is that an insulting phrase magic underwear. I'm assuming you call it something different.
Brent 59:25
Yes, we do tell something different, but I'm not insulted.
Scott Benner 59:30
Listen, apparently it's not insulting because Mormons continue to come on this podcast. So I feel like I'm doing the right thing here. I really appreciate you doing this. Brent. Thank you.
Brent 59:41
Yeah, no, I really appreciate you taking the time to let me talk to you and share my story.
Scott Benner 59:47
Hundred percent is my pleasure. I hope you have a great day and I'll let you know as soon as this is going to come out. All right
Brent 59:54
now I hope you have a good day as well and I will look forward to when this comes out. I appreciate that.
Scott Benner 59:59
Thank you. family for me, thank you very much.
Unknown Speaker 1:00:01
I will.
Scott Benner 1:00:03
Huge thanks to Brent for coming on and sharing his story. And of course the the Contour Next One blood glucose meter and touched by type one.org. for their support of the Juicebox Podcast, there's a list of all of the advertisers in the show notes of your podcast app, and at Juicebox podcast.com. But you can go to Contour Next one.com Ford slash juice box to find out more about this meter or touched by type one.org. To learn about that great organization. Last thing, if you go to T one d exchange.org. forward slash juice box, you can add your voice to some wonderful Type One Diabetes Research and it's super simple to do. Right there on your phone, your tablet, your PC from your home, you never have to visit a doctor. You never have to visit a site. It's completely HIPAA compliant. You can back out at any time if you change your mind and it is 1,000,000% anonymous. The answers you provide help people make good decisions about how to help people with type one diabetes. That's what your answers can do. Super simple. The ADA has made adjustments to their a one c recommendations for children because of T one D exchange. Test trips are covered by more insurance companies because of D one D exchange. The list goes on and on. This research does great stuff. You can support T one D exchange support people with type one diabetes and support the podcast T one d exchange.org. forward slash juicebox. The survey didn't take me more than 10 minutes to complete. Thanks to everyone for listening to the podcast and for sharing it with someone else. Two days ago, the show had its most popular day in the history of the show. It was it was a day that I will not soon forget the downloads were astonishing. And I very much thank you all for being ardent listeners and for sharing the show so freely means a lot and you're helping the show to grow. So thank you very much. I'll see you soon with another episode of the Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#380 Defining Diabetes: Feet on the Floor
Scott and Jenny Smith define diabetes terms
The third in a three-part series describing what naturally occurs to blood sugars when we first wake up and prepare to start the day. Scott and Jenny tackle basic T1D terminology in this easy guide for newly diagnosed T1D and/or caregivers of someone with T1D.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
This episode of defining diabetes is sponsored by Dexcom Omni pod, the Contour Next One blood glucose meter touched by type one, and the T one D exchange.
I almost made this one larger episode with three topics in it. And then I decided if I didn't break them apart, future listeners wouldn't be able to find them. So this is a defining diabetes episode about feet on the floor. But there are two others that go with it. The other one's called defining diabetes, smokey effect. And the third one defining diabetes dawn phenomenon.
Anyway, the three of them are oddly similar, but completely different. And every one of these ideas needs to be understood. I'm not going to be explaining them by myself. I'm gonna have Jenny Smith with me. I'll tell you a little bit more about Jenny in a second. But first, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. Please always consult a physician before making any changes to your health care plan, or becoming bold with insulin.
If the mood should strike you, and you'd like to find out more about the dexcom g six continuous glucose monitor, please go to dexcom.com Ford slash juice box. If you're looking for a free no obligation demo of the Omni pod tubeless insulin pump my Omni pod.com forward slash juice box. Want to add your voice to some terrific Type One Diabetes Research without ever leaving your home can do it right there from your phone in just a couple of minutes. T one d exchange.org. forward slash juice box. To check out the blood glucose meter that Arden uses the Contour Next One you go to Contour Next one.com forward slash juice box and of course touched by type one.org. To see Type One Diabetes advocacy done correctly. My friend Jenny Smith has that type one diabetes for over 30 years. Jennifer holds a bachelor's degree in human nutrition and biology from the University of Wisconsin. She is a registered and licensed dietitian, a certified diabetes educator and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. She is also a frequent contributor to the Juicebox Podcast. And I find Jenny's input about type one diabetes and the management of insulin and things around type one to be completely invaluable. She's my favorite person. feet on the floor is something that I didn't know people called a thing until I heard somebody say, Oh, that's that's feet on the floor. And I've always thought yeah, I didn't know that. I just found it. I figured it out. And then I attacked it, then I stopped thinking about it again. You know, so I've in in Arden's life, I've attacked feet on the floor a couple of different ways. So but first, like, I guess we'll, we'll define it. I think of it as if anyone's ever played on a football team. There's this thing you do right before the game, they get everybody together and whip them into a murderous frenzy, and then they send you out on the field. They're literally like saying just shy of go rip everyone's head off. Go do it now. And I feel like that's what your body does. When you stand up. It's like, we got to go, this is it. We're gonna go take a shower. We're gonna make lunch. I got to be on time I got to get to school, and it just Jacks you up so that you can accomplish those things. I know that's not technical. That's how I think of it. Is that about what's happening? Like, what is your body doing when you wake up? I'm assuming cortisol and
Jennifer Smith, CDE 4:14
Yeah, well, bunches of different hormones that are supposed to be there. And again, they're, I mean, if you think of them in terms of the flight or fight hormones, right. They're kind of the same thing. It's not like you're trying to run away from a saber toothed Tiger first thing in the morning, but at least not in today's world. But there are all the things as you just mentioned, in today's world, especially as an adult, there are a lot of things that are on your plate. As soon as you get out of bed in the morning. Yes, I have to get myself ready. If you have children or a spouse or anybody that you're a caretaker for that. You have to get ready. You might have breakfasts that you have to make things that you have to pack calls that you have to make, I mean the list just it goes on and on with the chores in the morning time and even kids Think well, why does it happen with my 12 year old child then? Well, kids have a lot of things that they're not really verbalizing. But their brains are thinking through, especially once they get out of bed. And in a life with diabetes, there are things that they're thinking about, again, they might not be talking about them right away. But, you know, what am I gonna have for breakfast this morning is mom and our mom and dad going to be really worried because my blood sugar is gonna go high. If I choose to eat pancakes today. I mean, there are lots and lots of things that are reasons for the rise. But the base reasons really are those like the cortisol kind of the get go, your body wants to ramp you up, and kind of move you give you energy.
Scott Benner 5:40
So what people call feet on the floor, I think of his bolusing for life. I don't know another way to put it really. So you know, if Arden were to wake up at a, an 85 blood sugar, and lay in bed for two hours looking at Tick Tock and Instagram, her blood sugar would not go up. It's got nothing to do with the timing. It's it's quite honestly, she gets out of bed. And then 1520 minutes later, her blood sugar can go from 85 to 120 and catch a diagonal up arrow and keep going if you don't stop it, right, so I always just have her wake up and bolus. And I don't know how much you know me. I don't know, let's throw some insulin in there. Get on the right side of this game, you know, unit today. One little eye care insulin, get it going. And, and that works terrifically. It really does. But I mean, honestly, this is gonna seem like a strange story to put in here, I guess. But when I was 16, for about three or four years, while I was 16. In my hometown, I volunteered as a fireman was a common thing for people to do. And I trained, you know, I got trained, I think we had to do like 100 hours of training, and then you know, you become a fireman. And when there was a fire at night, like in the middle of the night when you were sleeping. We used to have this old technology was so bad back then it was just this box that sat in your house. And they would send out this radio frequency and the box would pick it up, and then make this horrible, harsh, shrill scream that would wake you up, right? I want to say the company was realistic that made it I'm not gonna remember. But this thing I can't even like, I wouldn't even want to tell you that you'd have to cover your ears, it just would go. But so high pitched and loud. And you'd be standing up, I'd be standing on the floor in my underwear. unaware of how I stood up, it was so loud, right. And a few moments later, you're at the Firehouse, you're getting dressed, you're now in a truck, and you are flying down the road as wide awake in this alert as you have ever been in your entire life. I am crystal clear at that moment. Like that's when I should be taking my SAP. You know what I mean? And that has got to be this. Like just your body just going like holy Hannah. We got to go, you know, and this happening. And now I guess in a modern world. People talk all the time about like, Oh, I don't like to get upset because my cortisol levels go up and I get fluttery or nervous or, you know, anxiety hits me for some people. I think it's it like I think a feet on the floor is his life and you have to give yourself insulin for it because it doesn't go away once it's not like adrenaline. Right? adrenaline pushes you up. And then when the adrenaline's gone, your blood sugar drops back down again.
Jennifer Smith, CDE 8:39
Mm hmm. It's definitely different thing first thing in the morning. And I think that's it's a compounding factor when people are trying to figure out that morning breakfast, right? Because if you haven't realized that the rise is already starting, before you go ahead and even if your Pre-Bolus thing for breakfast, and you're thinking, well, gosh, I've waited 15 minutes. Let's try 20 minutes. Let's try 30 minutes. Let's try 45 minutes. And like finally you're at the hour point and your budget or you're still rising and you're like, Yeah, but I Bolus for my food. You're missing possibly a quarter a half maybe a whole unit and a half of insulin for this feed on the floor. impact. Yeah. And so that's it kind of like I said, it sort of covers up what might be going on behind a breakfast and the food kind of Bolus. Yeah. And so it's making you feel like well, gosh, I just I obviously need more insulin. So I'm going to dump more insulin in then and then you end up like you said, it sticks around for a long time if you don't get ahead of it and by getting ahead of it. I think most people that I talked to in teaching about it, it's you wake up, look at your CGM or do your finger stick and give your give your Bolus for that feet on the floor in me Utley. And sometimes it takes like I said before, a little bit of analysis, let's say, your feet on the floor doesn't really start, maybe it's an hour between waking up. And then it actually starts to rise with again, no food or anything else in the picture. But maybe you're the person who sees it within 20 minutes. That's me. I can wait at a blood sugar of 68. And I can have it start within 15 to 20 minutes,
Scott Benner 10:25
but you also don't strike me
Jennifer Smith, CDE 10:26
Oh, that I don't need to treat that low. Yeah, because
Scott Benner 10:30
it's gonna go up. You also strike me as a person who is active in your mind as well as your like your body. Like you're not you don't get up in the morning and think like, well hang around for a couple of hours. And then like you're moving right? Yeah,
Jennifer Smith, CDE 10:44
I don't have hang around. Yeah. And
Scott Benner 10:46
what's that? I said something that is literally say to you on an episode recently, and you're like, you have all kinds of free time. And I was like, I don't what do you Oh, when I said I fixed my carpet. When I got to pull it out. You're like, Where do you get time for that? I was like, Well, wait, lady, there's a big hole in my car. But I can't just leave it there. You know, Jenny couldn't even imagine. She's like, cut the carpet off. start over again. It's, it's done.
Jennifer Smith, CDE 11:09
Go Why just put like, you know, like, I don't know, I'll play it over it and be like, don't stop here. Mom will take care of it later. And then like three months later, I'd be like, my set plates. Do I
Scott Benner 11:20
really like that? But No, but seriously, like, you have that, like, you have that attitude. And I have to tell you, that I'm not good. I'm a busybody, I'm not good with free time either. As soon as I have too much free time, like I could make another podcast episode. Like I think that right away. I'm like, maybe we could move people along a little sooner I could be working is what I feel like. I this weekend, I talked my wife into relaxing, which she's terrible at. And so everyone's sort of outside, we have a little little patio out back. Everybody's sitting around. We drugged like a television outside. People are watching sports and just hanging around. And I realized the other day, I don't think I ever sat on that patio. And I was mad at myself when by the time it was over, you know, but I just couldn't. I kept thinking of things I had to do, which I know is bad. Don't write me. I know, it's bad. I know it's killing me. But um, but your feet on the floor is what I think of his life like bolusing for life. And really, when you stop and think about these three little episodes, which I'm gonna put up all at the same time, so people can find them all at the same time. You're thinking about, you don't realize you're thinking about what if? What if smokey happens, right? What if you What if you that happens? What if while that's happening, you start experiencing dawn phenomenon. And then you jump up and you're a more high strung person. And you've got this going and you're back here trying to Bolus for toasts with two years. Right, you're a lot already
Jennifer Smith, CDE 12:45
out of three things that you didn't realize could be impacting and the toast had nothing to do with the 290 blood sugar. Yeah.
Scott Benner 12:53
And it makes me think about how many people like to say, Oh, my, my blood sugar goes up every time I take a shower in the morning. But what if it's got nothing to do with the shower and everything to do with the feet on the floor? Correct. We've done it Jenny, this is that if people just listen these podcasts there, he wants to be in the fives. Some of them will make themselves crazy, but I mean, a lot of them will end up in the
Jennifer Smith, CDE 13:19
hopefully you don't need extra meds along the way.
Scott Benner 13:23
Just find yourself in the corner mumbling about oh gee and feet on the floor, and I gotta move my basal insulin so that it combats the dawn phenomenon. And then I'll just go to work and take these four kids.
Jennifer Smith, CDE 13:39
makes me kind of think of what's his name Gollum from Yeah,
Scott Benner 13:42
yeah, just shrink up and start talking to precious and rubbing your head. Yeah, yeah. So anyway, that's why honestly, is we kind of finished this one up. Without joking about it. That's why my theory is always just like, more get ahead. Don't let this stuff like make all of this stuff. Absolutely not even something you think about by being just being first by acting first. I am such a big fan of punching first with diabetes, so that you can at least say I did this and what happened next, I had some impact on instead of covering up defensively and waiting for all this stuff that happened to you and then trying to react on the go You just can't react the diabetes you have to be you know, you have to be first you have to be active I think
Jennifer Smith, CDE 14:31
and in some of that, too, like you said, you know, needing more is the idea of more is important knowing Okay, clearly I didn't do this well, so I just needed more. But I think also looking at, as I said before, you know a couple of trends in the morning time to be able to define Why do you need more? Is it just today or huh? Look at this. I see the trend of lows overnight and now then when I'm high in the morning, then I need more or Every morning I get out of bed at this time, and I've made a note of it. And no matter what I do, I don't even eat for three hours and my blood sugar's already going up before I eat well, clearly, this is the problem. So then it gives you more definition to maybe even quantity of the more, you know, how much more could I possibly need? You know, more three units versus more half unit to two different ideas.
Scott Benner 15:24
I don't know more, just more, did you get higher than more than that? Did it happen the next day, then more than that? What if it's too much, it hasn't been too much. So far, you know, if it gets to be too much, not for nothing, then do less. Every month, just I don't know another way to think about it. Because when I see people try to think about it logically, like like, I guess logically is the wrong word. But mathematically, maybe I see people making themselves crazy, because there are so many of these variables that you can't quantify. And even if you could, you can't quantify them in real time, while living a life, you know. So I just like putting a nice layer of insulin on everything and trying to keep the blood sugar down. And that way, if you don't get high, you don't get high. And that's it. I'd rather stop a lower falling blood sugar, and fight with a high one high. That's all it's so simple. All right. This is this was it feet on the floor, which, again, I would like to call bolusing for life, but then no one's gonna know what I'm talking about. If you'd like to hire Jenny to help you with your type one diabetes, check her out at integrated diabetes.com Thanks so much to the Omni pod tubeless insulin pump. If you'd like to get a free, no obligation demo of the Omni pod, do it now at my Omni pod.com forward slash juice box. Learn more about the dexcom g six continuous glucose monitor, see those trends, see your direction, see your speed dexcom.com forward slash juice box, get the best blood glucose meter on the market, in my opinion, at Contour Next one.com forward slash juicebox. You want to see people doing good things. For other people with type one diabetes, you need to go to touched by type one.org. And of course, to get involved simply in some type one research that helps everyone with Type One Diabetes. And to do that right there from your cell phone or from your sofa without ever leaving your house and just a few minutes, T one d exchange.org forward slash juicebox. You go to those links, you are doing something good for yourself good for somebody else and supporting the podcast. All of those links are available right here in the show notes of your podcast player. And they're also at Juicebox podcast.com. Click the links support the show. You all should know by the way, when I say click the links support the show. The pentameter of that reminds me of save the cheerleader save the world. From heroes, you remember that TV show on NBC. Anyway, here's a little look into my head. There are countless other episodes of the finding diabetes available for you right now. And that's probably a lie because they are accountable. There's not so many of them that I can't count them. But I'm not going to count them a couple of ways to get them going to your podcast, app search defining diabetes, they'll all pop up. Go into the stream in your podcast app, all episodes, scroll down, you'll see them you can go to Juicebox podcast.com. and scroll down a little bit. Right. And you'll see all kinds of stuff. Let me tell you some of the stuff you'll see on the main page all the after dark episodes. Right now we have after dark divorced, and co parenting after dark sex with type one from a male perspective sex with type one from a female perspective, depression and self harm, trauma and addiction, weed smoking, drinking with Type One Diabetes, there's also all kinds of episodes that are focused on algorithm pumping. And then you know what you get actually click books you look up, Oh, hold on. Excuse me. Also, I have all the pro tip episodes right there on the front page, and recent episodes. Now if you go to, then you click on a link up top right, it says Juicebox Podcast, you click on that. Now all of a sudden, you're looking at the defining diabetes episodes. There's fat and protein rise compression low and interstitial fluid rage, bolus bumping nudge feeding insulin, these little diabetes terms that maybe you're just like, I don't know what they mean when they say insulin resistance. But I have an episode Virginia and I explained that to you ketones stop the arrows brittle diabetes low before high Pre-Bolus trust what you know will happen will happen glycemic index and glycemic load as a defining diabetes but you know what we have coming up a pro tip about it. There's non compliance and algorithm and on and on. On and on and on. If there's a diabetes term that's been set out loud, Jenny and I have defined it on defining diabetes.
Two new ones that are out right now around this, like I mentioned the beginning, I think go together with this one. The other two are feet on the floor. And this Moji effect, the sum Mogi effect, I don't know how to say that word, but you'll see it. It'll be the only word that sounds like some Oh, gee, when you read it, looking for a great doctor, or other type of diabetes practitioner, check out check out Whoo, there goes my voice. Check out juicebox Doc's calm and ever growing list of podcast listeners favorite practitioners? absolutely free go in there, find one or send me one to add. Diabetes pro tip episodes can actually be found in all the places I just described in your podcast that ended diabetes pro tip.com. If you're enjoying the podcast, please consider sharing it with someone else.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!