#1585 After Dark: Coma
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
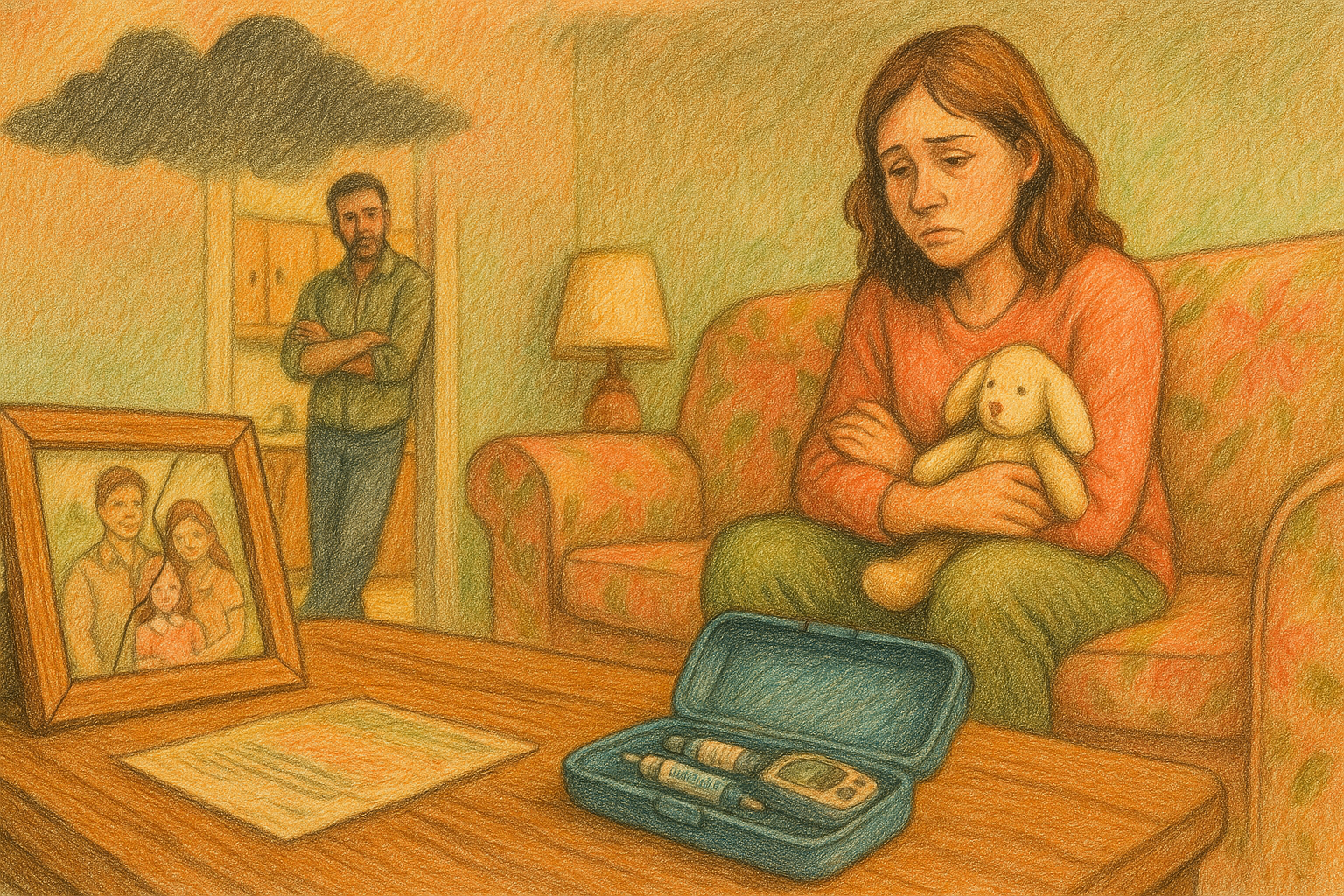
A mother recounts her son’s near-fatal DKA, coma, recovery, and life with type 1 diabetes, blending hope, resilience, and humor. - Book Link
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Welcome back friends to another episode of The Juicebox podcast.
Rosana 0:14
My name is Rosanna. My youngest is 14 and has type one diabetes.
Scott Benner 0:19
If your loved one is newly diagnosed with type one diabetes, and you're seeking a clear, practical perspective, check out the bold beginning series on the Juicebox podcast. It's hosted by myself and Jenny Smith, an experienced diabetes educator with over 35 years of personal insight into type one our series cuts through the medical jargon and delivers straightforward answers to your most pressing questions, you'll gain insight from real patients and caregivers and find practical advice to help you confidently navigate life with type one. You can start your journey informed and empowered with the Juicebox podcast, the bold beginning series and all of the collections in the Juicebox podcast are available in your audio app and at Juicebox podcast.com in the menu. Nothing you hear on the Juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. This episode of The Juicebox podcast is brought to you by my favorite diabetes organization touched by type one, please take a moment to learn more about them. At touched by type one.org, on Facebook and Instagram. Touched by type one.org. Check out their many programs, their annual conference awareness campaign, their D box program, dancing for diabetes. They have a dance program for local kids, a golf night and so much more touched by type one.org. You're looking to help, or you want to see people helping people with type one. You want touched by type one.org. I'm having an on body vibe alert. This episode of The Juicebox podcast is sponsored by ever since 365 the only one year where CGM that's one insertion and one CGM a year, one CGM one year, not every 10 or 14 days ever since cgm.com/juicebox This episode is sponsored by the tandem mobi system, which is powered by tandems, newest algorithm control iq plus technology, tandem Moby has a predictive algorithm that helps prevent highs and lows, and is now available for ages two and up. Learn more and get started today at tandem diabetes.com/juicebox
Rosana 2:37
My name is Rosanna. I'm a 53 year old, mother of four. My youngest is 14 and has type one diabetes. And I have six grandchildren. Oh,
Scott Benner 2:49
Rosanna, an eclectic Little Mix going on over there. Oh, boy, yeah, I do. Were you 12 when you had your first one or no? How old were you when you had your first kid? 22 okay, that's all fair. Well,
Rosana 3:02
they are third, 3129 20 and 14. Second marriage. No same marriage.
Scott Benner 3:09
Wow. What happened?
Rosana 3:11
We thought we were done after the first two. They were girls. We kind of built a business. And then, surprise, I was pregnant at a boy. The last one was kind of so the boy was always like, when he was three or four, was always like, I wish I had a sibling. Why do my sisters have each other and I don't have anyone? So we tried, had a miscarriage, gave up, and then at 39 got pregnant with
Scott Benner 3:34
leaf. You tried to get pregnant because your kid asked you to,
Rosana 3:38
yeah. I mean, I had always wanted like, six kids, but it didn't look like it was going to work out that way. So,
Scott Benner 3:45
oh, you're either brave or stupid. I can't wait to find out which one while we're talking both, for sure, you and I are the same age of a 14 year old. Yes. Oh, that makes me nervous.
Rosana 3:59
Yes. I feel very old some days, oh,
Scott Benner 4:01
I can't imagine, like, Wait till that 14 year old is, like, 18 and you're almost 60. Oh, good luck. It's gonna be awesome. Which one of those four has type one you said the youngest? Oh, look at you. Yep, yep. Couldn't just stop, huh? Is there other autoimmune in your family, none. It was a complete surprise, no thyroid or celiac, even with the grandmother. I
Rosana 4:27
mean, I have a cousin who has celiac. That's it, though, huh? Yeah, my mom has passed away. I think in her past, there may have been a thyroid issue, but it was never discussed.
Scott Benner 4:38
Was she super thin or opposite? No, she was opposite, opposite. Did it hit her like out of nowhere? Was she heavier her whole life? She was heavier most of her life, and she passed away about a year ago, of a year and a half ago, she had CLL, chronic lympho. FONA leukemia, oh my gosh. How was she in her 80s?
Rosana 5:04
She was 72
Scott Benner 5:08
Oh, it's too young, yeah. Oh, I'm sorry. She was, Are you her oldest? Yes, yeah. Look at me doing the math. You figuring things out. Are we going to use the name of your child who has type one leaf, l, e, i, f, okay. Like leaf Garrett, yes. Like Leif Erickson, the Viking. Does anyone remember the leaf Garrett posters on girls rooms, bedroom walls when we were in school? Yeah? I remember, yeah. The boys had Heather Locklear or the girl from the or the girl from the fall guys angels, or the Charlie's Angels, ones and boys had leaf, and girls had leaf. Garrett everybody's bedroom you walked into.
Rosana 5:55
Yeah, I didn't have posters.
Scott Benner 5:58
Where are we getting $1 from you little getting great. Oh my gosh. How old was he when he was diagnosed? Just turned 14 a week after his 14th birthday. Oh, this is very recent. It is about eight months. Oh my gosh. I haven't done a very recent one in a while. Are you okay?
Rosana 6:16
I am getting there. It was a wild ride. We were in the hospital for two months. No,
Scott Benner 6:21
wait, hold on. All right, let's go back to the beginning. What is the first thing you noticed that made you concerned for his health?
Rosana 6:28
Well, nothing. I guess that's the problem. My husband and I, my ex husband and I are divorced. We've been divorced about eight years, and he's the only minor child. He goes back and forth weekly. Every week he's one week. He's with me one week he's with his dad. The day before he was going to his dad's for the week, he had mentioned being thirsty, and I was like, well, you need to drink more water, like, because he'd always been healthy. He was on a competitive soccer team, right? We only saw the doctor when he needed a sports physical, so it didn't connect that anything was wrong?
Scott Benner 7:01
Oh, this one's so dumb. It doesn't know to drink when it's thirsty. Great, well, and he was
Rosana 7:05
drinking too much soda, I'm sure, like drink some water. So he went to his dad's. I went on a work trip. I came home and he was gonna go ahead and stay the next weekend with his dad's, because he was gonna have a slumber party for his birthday. But Saturday afternoon, his dad called me and said, Hey, he's really sick. He's asking for you, will you come and get him? So I went and picked him up, and he was gaunt and white, like he had obviously lost weight. And so I took him. It was like Saturday afternoon. I took him straight to the urgent care near our house, and they ran strep, flu, a, flu B, COVID, mono,
Scott Benner 7:45
and they did a UA, really, yes,
Rosana 7:49
and they said, and by this time, it's after five, and they're like, Well, it all, you know, all these things came up negative. We still think it's strep. They did a long strep test, and they said, We won't know for a couple of days, but we're gonna send you home with an antibiotic. She did mention that the UA showed high sugars and high proteins, but then she said, Well, that's probably because he hasn't been eating. And we found out he'd lost 20 pounds, yeah, and he was only 110
Scott Benner 8:14
I was gonna say 14. How much? How big he was, 90 at that point, 90 pounds. Yeah. Oh my gosh. Now that did that set off an alarm for you?
Rosana 8:25
Well, yeah, at that point, I'm like, Okay, this like,
Scott Benner 8:28
yeah, stop running the urgent care playbook here, and let's think a little closer, right? So well, but
Rosana 8:33
I'm like, okay, they know what they're doing, right? So I go home, I get the antibiotic, and go home, and Sunday, he spends all day, lying on the couch watching the TV, peeing, which, you know, I didn't know anything about type one diabetes, yeah, didn't know what the symptoms were. So he's like all now I look and I see all the symptoms during that day, Sunday night, went to sleep, he peed the bed, which he's not done since he was little, and I couldn't pick him up, and he was non responsive to me. Oh my gosh. So I called his dad, who met me at the apartment, and we rushed him to the Children's Hospital. They immediately took him back and almost immediately told us he was in DKA. His sugars were 649 his ketones were over 80, and his Ph, his blood pH, was 6.70 God, which. I didn't know what any of those numbers meant at the time, but they told us they were not conducive with
Scott Benner 9:35
life. Yeah, that's not a good thing to hear.
Rosana 9:38
So he slipped into a coma, and he was in a coma for about four days. And you know how you watch, like, Grey's Anatomy or shows, and they just like, wake up out of a coma, and they're like, wide awake.
Scott Benner 9:50
Well, they need to, yeah, they need to move this scene along. So they got to talk again. Not like that. Is that what you're telling
Rosana 9:56
me? Yes. Not like that. You know, one day he's like. Responding by squeezing your hand, but he's not awake, and then it's just like he's slowly, like it's, he's fighting through a boggy water or something to come back to consciousness. So it took him a few days.
Scott Benner 10:12
Oh, my God. So go ahead, keep going. I'm sorry. No, don't be. Are you okay? Talking about it? I mean, it's very recent.
Rosana 10:19
Yeah, yeah. I'm trying to get through it, because that was not the
Scott Benner 10:22
end. I almost cried. So, like, I'm like, You must be really upset, like, and I'll tell you, what got me was, is that, you know, I remember being told when we got Arden there, Hey, she's like, 24 hours away from being in a coma. And also thinking about all the stories I've heard of people who have been diagnosed like this and not made it, you know, so
Rosana 10:42
well. And the doctors, like the second night, one of the doctors, and they were all so good and so attentive and doing everything they could, and they just they didn't know what else to do, and they were running all kinds of tests because they couldn't figure out why he wasn't coming back. And I wasn't sure why they were running all the tests. To me that was like, okay, he's in DKA, and this is what happens. But I guess it doesn't always follow that. Usually when they get the sugars down, they rebound pretty
Scott Benner 11:09
quickly, okay? And he didn't, Jeez, what are they telling you? Two days into it, what are they saying?
Rosana 11:16
You know, it was kind of a wait and see. And they kept running tests and trying to figure out, you know, different things. And one night, I'm laying there because I slept in the room, the whole basically, I lived in the hospital for two months, and I'm quietly crying on the bed, you know, the guest bed, and one of the doctors, the female doctor, came over and kind of crouched in front of me and put her head down for a few minutes, and then she looked at me, and she was crying. She's like, I'm so sorry. You're going through this. I'm so sorry. And it's like, you could tell they were really emotional and upset about it.
Scott Benner 11:48
Yeah, lost as well. They weren't exactly sure what was happening, yeah. And so he woke up about
Rosana 11:54
four days later, and they started, you know, the rehab and swallow tests. And because he'd had every thing connected to him imaginable, dialysis, EEG, yeah, the EEG is on the head, intubated pic lines, you name it. So they started, you know, dealing with all of that. He had a swallow test. He had an MRI, which showed a little bit of brain bleed, and then he was awake for about six or seven days as they're trying to get everything back in order. And then one night, something happened, and he started thrashing. They thought he had a stroke. They weren't sure why they were giving him drugs, like one night, they were giving him fentanyl. And I was like, What are you like? Because I deal with fentanyl every day, like, this is not good. And they were like, No, this is medical. That's okay.
Scott Benner 12:49
Can I ask you? I mean, are you on your own at that because you said because the way you described your life, right up until you said you were divorced, I never would have expected you to be divorced, like four kids married that long. I was like, they're gonna be stuck with each other forever. When that got introduced, I was like, oh, gosh, and now you're in there. Like, do you and your ex reconcile enough to be together during this? Like, I mean, maybe you have that agreement already.
Rosana 13:14
He was there the entire time along with his girlfriend, awesome. So that's a total other trauma that we won't discuss.
Scott Benner 13:24
I mean, listen, you don't have to dig deep into it, but four kids a marriage this long, he did something wrong,
Rosana 13:30
right? Yeah. I mean, the easy, the easy answer is, midlife crisis.
Scott Benner 13:34
Gotcha. I mean, like, you smell it a mile away. So it's just you your ex and his girlfriend hanging out in your son's hospital room, who's in a coma, and the three older kids were in there, off and on. Okay? Is there a conversation that's had out loud, like, do you say we don't know if he's gonna live through this or not, or how do you manage that unknown? Time? This episode is sponsored by tandem Diabetes Care, and today I'm going to tell you about tandems, newest pump and algorithm, the tandem mobi system with control iq plus technology features auto Bolus, which can cover missed meal boluses and help prevent hyperglycemia. It has a dedicated sleep activity setting and is controlled from your personal iPhone. Tandem will help you to check your benefits today through my link, tandem diabetes.com/juicebox, this is going to help you to get started with tandem, smallest pump yet that's powered by its best algorithm ever control iq plus technology helps to keep blood sugars in range by predicting glucose levels 30 minutes ahead, and it adjusts insulin accordingly. You can wear the tandem Moby in a number of ways. Wear it on body with a patch like adhesive sleeve that is sold separately. Clip it discreetly to your clothing or slip it into your pocket head. Now to my link, tandem diabetes.com/juicebox to check out your benefits and. Get started today. Today's episode is sponsored by a long term CGM that's going to help you to stay on top of your glucose readings the ever since 365 I'm talking, of course, about the world's first and only CGM that lasts for one year, one year, one CGM. Are you tired of those other CGM the ones that give you all those problems that you didn't expect, knocking them off, false alerts not lasting as long as they're supposed to. If you're tired of those constant frustrations, use my link ever since cgm.com/juicebox to learn more about the ever since 365 some of you may be able to experience the ever since 365 for as low as $199 for a full year. At my link, you'll find those details and can learn about eligibility ever since cgm.com/juicebox check it out. There was a lot of
Rosana 15:57
just kind of discussion on what ifs you know, because it wasn't just that, like when he woke up, it wasn't just is he going to live? It's also they had no idea what kind of neurological deficits he would have. So and then after he went into he had a stroke, which later they determined is something else, but he
Scott Benner 16:15
went back into a coma. So the thrashing led back to the coma. Yeah,
Rosana 16:19
something he had, his blood pressure went too high. Oh, god. Okay, so by this time, he'd been on constant dialysis for two weeks, and that was as long as they could do it for. And so they sent us to another city. They life flighted him, and we drove to another city to have a different kind of dialysis. And once we got there, his doctor there took all of his records home to try to figure out what was going on, and came back and said that she believed he had had press, which is pulmonary rehabilitative encephalopathy, with the syndrome,
Scott Benner 16:57
okay? And this is as a result of the dka, or in addition,
Rosana 17:01
they think so, yes, and then his blood pressure skyrocketing, and he had a hemorrhage in his occipital lobe. We were there for about three weeks. He got out of the PICU, went to a regular ward. We had our diabetes education, he was in therapy, and then we were moved to an inpatient rehab at Bethany in town. Stayed there for three weeks, and just once he woke up from that, he just progressed really quickly, much, much quicker than they thought he would. They really thought there would be more neurological issues.
Scott Benner 17:36
That's what the swallow test is for, right? It's looking for early neurological issues,
Rosana 17:40
yes, and to see if he can swallow anything without aspirating, because he'd had a he'd been intubated and had a feeding tube most of the time.
Scott Benner 17:49
So even though he comes out of this, I mean, and that's obviously good news, you're still unsure of his path to that
Rosana 17:55
right? And in the end, it ended up being they were worried about his peripheral vision, and he has foot drop okay. After we came home, we were still in therapy for those things. He still has about a 20% foot drop, but he's walking and even running. I mean, he's just, he kind of, if he's not thinking about it, he kind of walks on the balls of his feet.
Scott Benner 18:17
So for people who don't know is that where you take a step and your foot kind of doesn't come along with you, no? Or what is
Rosana 18:23
that? I think, if it's more severe, yes, it's just he doesn't walk with a heel toe strike. Okay, his feet are always more pointed than they should be. And
Scott Benner 18:33
is this going to be forever, or is it a thing they can help him with?
Rosana 18:36
Well, rehab finally got to a point where they said that they didn't think it was going to help. Rehab was going to help anymore. So now we're looking at possible neuromuscular doctors or Botox
Scott Benner 18:47
therapy. Okay, with some hindsight, let me take you out of this moment for a second before you die. Yeah? Like she's just gonna explode and start crying, if only that was the end of it. No, no, I know. I want to give you a pause because and I'm a little embarrassed, but as I logged on here, I thought, people listen. You might not listen much like, but for people who listen, they know like, I'm kind of proud that I don't prep for the episodes. Like, I find my way through the conversation with people, and I think that's what makes it interesting. Except when I logged on today, I did think like, how this lady got a hold of a VIP link, and like, I'm like, I'll figure it out. And then, as you're talking, I thought, oh God, you put the post up in the Facebook group, like, right? And then people said you should be on the podcast. You're that person, right?
Rosana 19:33
I don't know about you. Asked you, you asked for some after dark people to sign up, and I sent to send you emails, and I sent you an email.
Scott Benner 19:41
Oh, no, kidding. Okay, yeah, anyway, like, one way or the other, until you really start telling your story, I'm not sitting here thinking, Oh, this is the person who's gonna tell me that their kid was in DK and in the hospital for two months. So like, I'm Yeah, being my dumb self, like in the beginning, trying to loosen you up to get ready for the podcast, and as you're talking, I was like. Oh, geez, that's okay, no. And now I'm hearing you struggling, and I just thought, like, let's break for a second. So with some hindsight, how long were his symptoms active before you ended up in the hospital?
Rosana 20:16
As far as actual symptoms, other than the thirst, I don't really remember anything. Looking back now, I remember throughout the school year, he would call me and say his stomach hurt after lunch, and in my mind, it was because he was bored and didn't want to be at school.
Scott Benner 20:30
He thought he was trying to get out of school. I mean, he's the fourth kid like this time. I've heard it all. He's also like, he's like, I could push this lady around. She's old and she don't got the she ain't got the energy for this anymore, you know. But now I wonder, what was that distance though, that stomach pain to the diagnosis? How long had that happened? You know, it had been months, months, okay, and then the thirst,
Rosana 20:52
the thirst was the first thing that I could look back and say, hey, you know, that's pre and that was only a week and a half
Scott Benner 20:58
before, okay, okay, please don't but I imagine you are, but please don't beat yourself up over it. But are you beating yourself up over this?
Rosana 21:05
No, at first I was beating myself up over believing urgent care and taking him home for 36 hours, but after, like, reading all of the posts and listening to blog, you know your podcast, I mean,
Scott Benner 21:19
it really is just kind of, what happens, yeah, I mean, because it does seem like, from a from an outsider's perspective, who's not been dealing with all this stuff for their whole life, it seems insane that urgent care could miss. Oh, yeah, what you're describing happened 36 hours later. You know what I mean? Like, it does seem insane, but at the same time, like, I don't know, like, they probably, so once I got
Rosana 21:42
to the hospital and we were settled in, you know, I looked at the paperwork that urgent care sent me home with, and it said, Well, I didn't have it with me. That was the deal. I didn't have my paperwork with me. So I called urgent care, and the receptionist was new, and I said, Hey, I don't have my paperwork from Saturday. Can you email it to he said, Well, I don't know when he figured it out, and he sent it to me. And this paperwork, as opposed to the paperwork I got sent home with that, I remember reading that paperwork said blood sugars, high, proteins, high, no numbers. It just said high. Well, the paperwork he emailed me had numbers, okay, and was in bright red. So I'm like, why didn't somebody see this?
Scott Benner 22:28
I mean, even high, like a blood sugar, that's high on a I mean, let's guess it's over 400 maybe over 500 right?
Rosana 22:34
The numbers that they sent me said 500 plus, because that's as high as their thing that, you know, test for and proteins were 80 plus. You just
Scott Benner 22:43
have to want, you do have to wonder, I don't want to, like, get into, like, the blame game, but like, you do have to wonder, like, I mean, they don't see any 500 plus blood sugars from people just because they're sick. I can't be right, especially a little 14 year
Rosana 22:56
old kid, and it was an NP, but I think that it was near closing time.
Scott Benner 23:01
Oh, you can eat Buffalo Wild Wings up the street. Maybe we needed to get going.
Rosana 23:04
Yeah, I don't know. Yeah, I don't know. Does Buffalo Wild
Scott Benner 23:08
Wings do all you can eat? I don't know. Oh, my God. So, okay, so you're not alone. Listen, just real quick, the girlfriend's not like way younger than you. Is she? I think she might be about eight to 10 years younger than me. Geez, I'm
Rosana 23:22
sorry. It all sucks. Not as much of an age gap as the girlfriend he had before that. So, oh,
Scott Benner 23:27
okay, least he brought the one he found at the gym, not the one he found at the club. Is that what you're saying? I'm so sorry. They both work for him. So, oh geez, it's a good collection system. Are you still in business with him? No, oh yeah, you made him buy you out, I imagine, yeah, good for you. Okay. Wow, you've had quite a decade. Are you okay to move forward now, like I stopped you so you could collect yourself and say some stupid so you could relax. You want to keep telling the story now? Please do Yeah, sure.
Rosana 23:56
So we've been home since December 6, and he's doing really well. His diabetes is like, probably the least has been up to this point, the least of his problems. I mean, as we're healing from all the other stuff, even now it's still he's within range about 95% of the time. Awesome, yeah, and he just got a tandem Moby Monday. Do you like it? He is, and he's been doing really well, keeping everything in in range.
Scott Benner 24:21
Awesome. That's great. Tandem diabetes.com/juicebox.
Rosana 24:26
We tried to get the Omnipod, and our insurance was like, Yeah, you're gonna have to pay out of pocket to eat. You reach your out of pocket Max every year, okay? And we're like, yeah, we're not gonna do that.
Scott Benner 24:36
Okay? Omnipod.com/juicebox, use the links support the show. Let's move on. Though, if diabetes is the least of his issues, what are his issues?
Rosana 24:46
I mean, he'd still like to play competitive soccer again, so getting his foot issue is probably the biggest thing right now.
Scott Benner 24:54
But that's physically like is he struggling psychologically by being waylaid like this? You
Rosana 25:00
know, he asked a lot of questions. At first, we have a scrapbook because he wanted to know. He wanted to see it all. He also firmly believes that he's a miracle, being alive. Being alive, okay, yes. And there was a whole thing centered around Ezekiel 37 which is a scripture about dry bones coming alive, which is his favorite song. He
Scott Benner 25:23
doesn't feel like this was all purposeless and no,
Rosana 25:26
and he's kind of a typical youngest child where, you know, he's enjoying the attention.
Scott Benner 25:32
It's like, Finally, someone's paying attention. I had to get this foot drop and diabetes and be in a coma, but they really are looking at leaf now, yeah, well, I'm sure he would have taken it a different way. Yes. So neurologically, all okay,
Rosana 25:45
seems to me, he missed a whole quarter of school, and then when he went back, it was for half days, because he was going to therapy in the morning. So they dropped his math, which was his favorite subject, they dropped him from algebra down to pre algebra, which he'd already taken. That was one thing they were worried about. Was his math, whatever part of your brain does math
Scott Benner 26:06
really? Oh, that was a that was a health decision, not a school decision. Well, it was a school
Rosana 26:11
decision, but we're just kind of waiting and seeing how that comes back.
Scott Benner 26:14
Is he having difficulty with mathematics?
Rosana 26:17
He doesn't think so. So we're going to wait and see how next school year goes.
Scott Benner 26:21
Do you notice anything different about him, like intellectually, or how quick he is, the sense of humor, stuff like that? I
Rosana 26:29
think his peripheral vision is still has a deficit, and that kind of makes a difference, kind of in how he does things. Yeah,
Scott Benner 26:37
other than that, not really.
Rosana 26:41
He still has a really close knit group of friends. He still plays video games. He's just not playing soccer right now.
Scott Benner 26:47
Did the doctors give you any indication of why they thought this became so severe? No, they still don't know. And do they have a feeling for how long he was without as much insulin as he needed before. No, no,
Rosana 27:03
we went back to the hospital here in town and took a basket for the nurses, and they were all very happy to see him. And several of the nurses said that he was one of the worst cases that they had had. And they were very, very happy to see
Scott Benner 27:17
him, happy to see him meeting. They're a little stunned he's alive and doing okay,
Rosana 27:21
yeah, walking around and smiling and joking. Does that
Scott Benner 27:25
make you feel like, does that make you feel lucky, or does it make you mad? I don't know how you I'm wondering.
Rosana 27:33
Makes me feel blessed. I think it's just that he's he is still alive. Yeah,
Scott Benner 27:39
it's so random, right? Like, it feels like, like a car accident, almost like in its right. How did the other three kids? I know some of them are much older, but like, how did they, how did they handle, like, going through all this? Did everybody do it differently?
Rosana 27:51
They were all pretty emotional about it. My 20 year old son, Joel, he got a tattoo
Scott Benner 27:57
for his brother, oh, I was gonna say, depicting the event. Where, like, it says Ezekiel 37 that makes more sense than my idea. Yeah,
Rosana 28:06
so and his older sister spent a lot of time with us. Came, came to the city and stayed with me some nights. And the second sister has four children, and was pregnant.
Scott Benner 28:15
Oh gosh, she didn't. She didn't have any space for any of that, huh? Probably
Rosana 28:19
no. So she, she came with when she could, but that is
Scott Benner 28:23
interesting, right? Did I met? Am I remembering right, that she's is she 33
Rosana 28:27
she's 2929 you're 22nd
Scott Benner 28:30
one, you're 29 okay, you're but the old, the oldest 133's right? She's 31 I was gonna give myself credit for remembering that number randomly. But okay, but your 29 year old has four kids. You know, was was pregnant with the fourth. During this happening, she's pregnant with the fifth. The fifth, yeah, are you guys? Like, where are you building an army for the Lord, what's going on over
Rosana 28:51
there? Kinda, I guess her husband is second of seven. Oh, no kidding, yeah. And he was homeschooled, and she was homeschooled. And I'm
Scott Benner 29:00
not talking to you from Utah, right? No,
Rosana 29:03
okay, we're not the denim jumper kind of homeschoolers. I don't
Scott Benner 29:07
know what that means, but I'm sure those people are offended, and everybody else is laughing. Wow, that's that really is life altering, isn't it like that's, I mean, do you feel like life's the same thing as it
Rosana 29:19
used to be? No, but that wasn't the end of the trauma. So
Scott Benner 29:23
wait, all right, I'll write my question down and then keep going. Where's there's give me the rest.
Rosana 29:29
So about a month after we came home, I had just bought a house, in fact, just closed on it on that day, and later that evening, my daughter, who was 39 Weeks Pregnant, she was planning to have a home birth with the midwife, and she had a placental abruption. I
Scott Benner 29:44
don't think I can handle your life anymore.
Rosana 29:49
And they live about 30 miles south of town, so about 45 minutes from the hospital, and they called me. I was just leaving work. It was rush hour traffic, and I said, I'll meet. You there. I'll get the other kids. And so I met them at the hospital. They pulled up right behind me, like he said. He literally put the cruise control on 100 put the blinkers on, and drove on the shoulder. I don't know how he made it without stopping or without getting stopped, but he did. I took the kids and parked and cleaned up the van because it was not good. Kids were pretty traumatized.
Scott Benner 30:25
Were they in the car for the for the 100 mile? Are you just here to say speeding is okay? Is that what you're saying?
Rosana 30:33
No, I was, I was pretty traumatized about that, that she had passed out on the way. He
Scott Benner 30:37
was,
Rosana 30:38
he was pretty shaken. She's, you are
Scott Benner 30:41
gonna make me cry. Rosanna, Jesus, oh, God, this guy who's not 30, probably, maybe all of like, 30 years old, maybe is in a car with his pregnant wife and his four kids, and she loses consciousness. Yes, dear, jeez. Oh, okay, all right, so he what happens? Is she okay? She
Rosana 31:03
had an emergency C section. She's okay. They had to, I think they had to give her turnover. If they had to give her blood transfusion, I think they did, but she was okay. They, you know, kicked her out. 48 hours later,
Scott Benner 31:15
really, they're like, Okay, get out. Typical
Rosana 31:19
baby was born with a hard knot in his umbilical cord. Oh, and they did not know how long he had been without oxygen. How long ago is this now? January? Mid January, and how was the baby? He spent a month in the NICU, the first 72 hours on a cooling pad, which very few hospitals have, but luckily enough, Children's Hospital here had one. They still were, like, we don't know what kind of neurological deficits he's gonna have. Like, basically, I go to the hospital room and it looks almost identical to my sons. It's two floors lower and it's a smaller bed. He's got all the things hooked up to him, EEGs, and he's tiny. He's got a bunch of dark hair, you know, just all over his head. For a while, he had a feeding tube, and they didn't think that he would be able to swallow or eat on his own, but that went away. They didn't think he'd ever be able to breastfeed. He did. He is at home now, progressing. He's still, I think they say neurologically behind, not rolling over yet. He's about four months old. How
Scott Benner 32:26
long does it take to get a real assessment? How old does he have to be before they can start figuring out what has or hasn't happened?
Rosana 32:33
I don't know when with Leif, they told us that brain, any kind of brain bleed or brain tears to take up to a year to heal, and so they told us to wait a year before we really start
Scott Benner 32:46
trying to assess what happened, right? I hope this wasn't too upsetting to your husband. Ex husband's girlfriend, sorry she wasn't there too, right? No,
Rosana 32:55
not this time. Okay,
Scott Benner 32:58
I don't know how you don't know, by the way, not to be there.
Rosana 33:04
Yeah,
Scott Benner 33:06
it was a whole thing. I can't imagine. It wasn't just wait in the waiting room. Like, what are you doing anyway? No, no, oh, my goodness. Well, has any other horrible things happened to any people you love?
Rosana 33:20
No, please. No, no. You're
Scott Benner 33:21
like, I mean, you know, it's funny now, like, I go back to the beginning of our conversation where I just thought you were telling me that your son was diagnosed with type one diabetes eight months ago, and I said, you're okay, but now I'm going to ask you much differently, because I think it's possible the answer is, no, Scott, I'm not but are you okay? I
Rosana 33:37
most days I'm getting there. I probably should see a therapist, but I'm out of money and I have no time, so let's
Scott Benner 33:44
forget everybody else for a second and just think about you for a second. What's the journey you've been on? Like forget the nuts and bolts of it. How have you felt, and how have you gotten through how you felt and what has it led to?
Rosana 33:57
Definitely traumatized. My personality is such that I'm always anxious and always looking for how the next shoe is going to drop, basically what's going to go wrong. Obviously, this is something I'd never imagined. So no matter how much you worry, it always ends up being something you didn't worry about. A lot of, you know, kind of depression, maybe, of just trying to handle little being alone. And his dad stepped up and has really helped, and he still goes, you know, week on, week off, to his dad's house, which gives both of us a break, basically, right? But yeah, just handling it alone, and yeah, financially.
Scott Benner 34:37
How much do? What can you tell me? What was the bill.
Rosana 34:41
Obviously, they have their bill. The insurance has what they're going to pay. And then we had our out of pocket Max, which I have pretty good insurance through my work. So our out of pocket Max was 8700
Scott Benner 34:53
still a lot of money, huh? Yeah. Do you remember the pre insurance bill? The bill the hospital?
Rosana 35:00
It was very close to 2 million. Wow, yeah,
Scott Benner 35:03
jeez. And the insurance company, like, what do they do? They pay half of it.
Rosana 35:08
Oh, I think it was less than half. Yeah, I want to say it was like, 750,000
Scott Benner 35:12
Okay, and then you get to pay, uh, can you imagine? What do they need your eight grand for? Like, if seven you don't even, like, if 750,000 was a good number for them, what do they need? Your eight grand? Eight grand for? What are they doing with that? Buying a cooling pad? I don't think so. There's only one hospital has one. Oh, my God. Okay, so you've you feel like you've been depressed. Definitely struggled with that for a few months. And I've struggled, not clinically, like I've never seen a therapist, and I always kind of have when I start feeling that way, I have steps, I guess, to get myself out of it. If that makes sense. Is it wrapped around your anxiety that something else is going to happen?
Rosana 35:56
Oh, yeah, but I think this definitely, like proved to me that things are going to happen, whether I worry or not
Scott Benner 36:03
prior to your son's illness coming on, had there been a lot of health issues at all to deal with over the previous years?
Rosana 36:12
Nope, none of my kids have been sick or unhealthy. In fact, Leif was really the only he had broken his collarbone before he'd actually broken it twice. They had to break him to get they had to break his collarbone to get him out of me. He was a very big child.
Scott Benner 36:28
Sorry. I mean, honestly, did you say just leave him in it's all right. Like, I was like, I changed my mind he could live in there. I didn't know all this was gonna happen. But point being, is that you've made your fair share of babies your you know, your daughter's making them probably. I mean, it sounds like everybody's pretty fertile, so there's a lot of kids going on and, like, and no one's been sick. And then all of a sudden, you're 53 and your son is, like, being life flighted and is in a coma, yeah. And then before you can look up your daughter's almost losing her life and a baby in a
Rosana 37:03
pregnancy, Yep, yeah. And it feels like, so I live in Oklahoma, in the middle of tornado alley, and it does. It feels like it's just, you know, kind of a normal day, and all of a sudden tornadoes come through, lift your house, drop it back down, and you're just supposed to get up the next morning and go back to
Scott Benner 37:24
work, yeah, and that's what you've been doing, yep. But you think maybe you should talk to somebody I don't know, Rosanna, you probably should let me just listen. There are days you wake up and you like, is it dread, or do you feel like, Oh no, here it comes. And then you something bad is going to happen today, and then you have to you have to talk yourself out of it. No, you
Rosana 37:46
know, the anxiety has pretty much, I mean, I think for now, I've kind of looked at being 53 and looking at the rest of my life as being alone and having to get up every day and go to work and take care of everything by myself.
Scott Benner 38:00
You feel lonely, yeah, yeah. Well, you should start your own business and then start dating the men that work for you. I think that sounds like it works. I hear that works. Do you try to date? Do you try to go meet people I haven't dated in four years? I did before that. In fact, in 2019 I went on 10 first dates. Oh, and then what happened COVID. I
Rosana 38:27
actually got married, and COVID hit. And, well, I got married during COVID, I think because I thought the end of the world was coming or something, I'm not sure. And I needed major surgery, and he was there and being helpful, and then he lost his job, and turned out that he was a ranching alcoholic and decided to start stealing things from me and pawning them.
Scott Benner 38:49
Rosanna, listen, I need you to. I need you just to. I don't know what I need you to do. Hold on a second. You know, it's not often people come on here with so many problems that I'm like, have you tried drinking?
Rosana 39:04
No, not no to look at me. I'm like, very
Scott Benner 39:07
feel together, calm. So you took a shot with some guy and then he wasn't all he purported to be. How long were you with him before you married him? Over six months. Yeah, that's not long enough. Was he your age?
Rosana 39:22
Yes, yeah. And I only knew my first husband six months before. And then, how
Scott Benner 39:28
long were you married to him for? Though, 23 years. So you thought, Oh, this is how it works. Yeah, yeah, it's not how it works. I'm sorry to ask you, like this way, do you feel lonely, like, intellectually, or do you feel lonely, physically, probably both. I mean, the kids just bang, they use the apps, and then they have sex. You could cover half of this that way, if you wanted to right, swipe, swipe, swipe. You show up somewhere. Yeah, I think you do. You're not
Rosana 39:56
up for that. You know, after all this, I'm feeling very. Bold and frumpy, like, I'm in my Nana years, you know, 53
Scott Benner 40:04
I don't think that's true. I don't think you're Nana yet. Like, I mean, just because that kid got out there and started working early doesn't mean that you're like a grandmom. I
Rosana 40:14
mean, I feel like a lot of the guys my age are looking for younger women, and they can get them really, how do they do that? I mean, there's a lot of single women,
Scott Benner 40:23
so they're out there fishing for girls with daddy issues, and you're like, could you go older? Could you get like, could you go to 60? I mean, possibly, you know what? I mean, like, a surprise 60 year old guy. Yeah, right. They got meds now, like, if need be. I mean, listen, you're in a it's a difficult situation. I don't say otherwise. You know what? I mean, like I'm sitting here joking with you, but I don't think I could date like that seems ridiculous.
Rosana 40:49
No, it's not fun. Yeah, I'm not a looker. I'm not someone you would like twice. You have to get to know me before you decide to like me.
Scott Benner 40:59
I'm sure that's not true, but so you're worried that you're not visually, uh, appealing enough to, like do the quick dating thing. Yeah, so you worry guys are going to reach cheat just for
Rosana 41:10
sex. I don't even think they're interested
Scott Benner 41:13
in that. You never been a guy, so,
Rosana 41:17
I mean, after the last two I think they're mostly interested in somebody to take care of them.
Scott Benner 41:21
Oh, you, you end up finding guys who are, like, near to wells and need help.
Rosana 41:26
Yeah? I mean, they need somebody to cook and clean and yeah, pay for, yeah, pay for the second. With the second one, that was pay for things. But yeah,
Scott Benner 41:33
I can't imagine. Was he your age? Yeah, he's looking for you to pay the bills.
Rosana 41:38
Yeah. I mean, he's, he's since married again and living with his parents.
Scott Benner 41:43
Was that his third marriage? Yeah. See, he married you left you married another woman. Is in his 50s, married a third time, living with his parents, yeah. Oh, goodness, is it that bad out there? Yeah, that's upsetting. I mean, he should be embarrassed.
Rosana 42:03
And maybe it's just where I live, I don't know. Well, I
Scott Benner 42:06
was gonna say, Can you move? Well, not now that I have, you know, children and grandchildren. Yeah, you don't want to leave the kids. No, they're all here. Well, you should be depressed. I guess it's, I guess I don't want to argue with you about it, but I think you should talk to somebody about it, though, someday I'm gonna chuck it all and move to London. Really is that? Chuck it all? You're all on your own. Go yourselves. I'm out of here. Send pictures if you want, but don't feel pressured. Is that a dream of yours to live there? Oh
Rosana 42:39
yeah, I got to go for the first time last year, and it was everything I thought it would be.
Scott Benner 42:43
Why don't you and leaf go? Well, it's expensive, is it? I don't know. I've never been there. I think it's fancy that you've got to go at all.
Rosana 42:50
I'm a huge history like, I've read history since I was a kid, and I know I'm an anglophile. I know so much about one you know English history,
Scott Benner 43:00
right? And you just and that'd be a good place for you to eat. What can you guys go explore for a while, or
Rosana 43:06
go live there? Or, I'm hoping some someday when I've recovered from this.
Scott Benner 43:10
What do you think that looks like being recovered from this? I kind
Rosana 43:15
of have a five year plan of just trying to get out of debt and get physically back to where I can, you know, go and do fun stuff, and by then, leaf will graduate high school and
Scott Benner 43:25
I'll have some more freedom, okay, getting out of debt. Is that from the medical
Rosana 43:30
stuff? Oh, I wish I could say it was, but it's not. Is
Scott Benner 43:33
it from your crack Asia? From your crack addiction?
Rosana 43:37
No, it's from going to London last year. Oh, and also, I've written three books and self published and paid for my dream that turns out I'm not very good at marketing. Well,
Scott Benner 43:49
you should have come and found me rose, and I would have told you that that's not going to work. I had a publisher, and it's impossible to move, yeah? Impossible to move books like it just, it's really hard. Yeah, yeah. Also, I'm looking at you here, and you're not giving yourself enough credit for how you look. So I decided to, like, find you on the thing. You're fine. Don't worry about it that I wouldn't. I wouldn't worry about that one time if I was you. How much does it cost to self publish a book? Well, the
Rosana 44:16
last time around, I figured out that I could put it on Amazon and I wouldn't have to pay up front. But the first few times I sent it to a publishing I sent it to someplace where you could pay for copies and then sell them on your own. Okay, so, and then, you know, writing it, I you have a lot of copies of your book. Is that what you're telling me? Yeah, no, I have a couple boxes. Yeah. I also paid for an editor and I paid for an illustrator, because one of the books I wrote was a children's
Scott Benner 44:42
book. Well, let me ask you a question, do you think it's a good book? Yeah, yeah. You just can't, like, there's no way to get people to notice it,
Rosana 44:49
right? Yeah. I mean, you kind of have to be really into social media and have a lot of followers.
Scott Benner 44:54
Yeah, listen, I have a lot of followers, and it's still hard to make people notice stuff. So, yeah, yeah. Yes, you're at the whim of the platforms. Generally speaking,
Rosana 45:02
that's okay. Lesson learned. I went after my dream. I'm proud of myself for doing that. Now I just have to pay for it.
Scott Benner 45:07
I would give that book as gifts at every gift giving occasion for the rest of my life. Anytime somebody has a baby, I'd be like, hey, congratulations, Mazel Tov, here's a book. It's signed, I would tell
Rosana 45:19
them. The funny thing is, it's at the Children's Book is at my local library. I took it there, and it gets checked out all the time. People, like, always checked out. Yeah, yeah. And the library, in fact, said they have two copies now, so they'll check it out. They just
Scott Benner 45:33
won't buy it. Yeah? I mean, it's a tough road. I'll share a story with you that you're gonna say, well, would have been nice, Scott, if you shared this with me before I self published my book, while I was writing my book, which is now over. I mean, a long time ago, 2013 right? I had a daily relationship with my publisher. We talked all the time, and I'd pick around and, like, ask questions. And I one time said, like, Are people always bothering you with their book ideas? And she laughed, and she's like, constantly, like, Do you know what the worst ones are? And I was like, what's that? She goes, the people who think they have a good idea for a children's book. And I was like, Oh, yeah. She goes, everybody, everybody thinks they have a children's book. And I was like, Okay. And she goes, and don't get me wrong, she's like, some of them do, and she's like, but a lot of them don't,
Rosana 46:23
oh, I've read some. I'm like, and that's what kind of made me, pushed me into going ahead and publishing mine, because I was like, if they can get theirs out in the store, surely
Scott Benner 46:32
you could. Yes. Can you do something like, I mean, honestly, could you go to a local bookstore and tell them you'd like to, like, look, I want to put an author event here one evening, and I can bring in a certain amount of people and like, could you do that? Could you invite 2030 people to come? I've done
Rosana 46:50
book signing signings here in town, sold a few books. My biggest problem is I am very much an introvert, and I feel very awkward saying here, please find my book,
Scott Benner 47:02
so you're gonna find this next little thing interesting. Then after I got my book written, and I was out, you know, pushing it, which is the only way to talk about what you're doing, you're just out there, like, just trying to make anybody aware of it, I finished an interview one day, and the publisher called me, and they were like, that was so good. And I said, thank you. I was like, Why do you seem like, surprised that I did a good job with the interview? And she goes, I think it's just because authors are terrible at talking. Usually, that's why we write. Yeah, that's exactly what she said. She said, You're clearly not really an like, I'm not a writer. Like, you know what I mean? Like, I'm not a book author, and she's like, but on this part of it, you're way better at this part of it, she's like, significantly better. They just go out there and they sit and they wait for questions. Nobody asks them a question, and they sit there. Have you ever heard me tell that story about the book fair I went to one time? I think I did. You were talking? Yeah, yeah. I mean, I was stunned. I looked around the room and I was like, do all these people think someone's just gonna walk up to them and magically buy this book? Like I was out in front of the table handful of books. I was like, Hey, check this out. I sold all those books. I was out of there by like, lunch. That's what you I mean, if you're not doing that either, there's no way I'm just always so awkward I don't know you're doing a good job of this. Why do
Rosana 48:22
you think you're leading? You're telling you're asking me questions,
Scott Benner 48:27
and I really am the secret to this whole thing. But that's not the point. The point is that is that people should I never do this, but if you send me the link to your book, I'll put it in the show notes of the podcast.
Rosana 48:36
It doesn't have anything to do with diabetes, although maybe I need to write a book. I don't know.
Scott Benner 48:41
I don't care. Okay, I don't I don't know what it's about. I don't care what it's about. I don't even care if it's good. What do you think of that? But if you send me a link to where people can buy it, I will put it in the show notes of the podcast player. Because, by the way, let me just say this out loud. No one else try that like, don't I am NOT DO I already turned down 10 emails a day from people like, I just want to come on and talk to come on and talk to people about my app idea or my business idea. Oh, shut up. Leave me alone. Leave me alone. So uh, but for you, Rosanna, because of everything you've been through, that's why poor pitiful, because of the luck you and your family have, we're gonna see if some people might not buy this book. What is the Book about? The children's book. Yeah,
Rosana 49:23
here's the other thing. I'm terrible at describing it, so it is and I wrote it when my oldest daughter was a child, was a baby. Okay?
Scott Benner 49:32
It's about the life of a rock, like a pet rock.
Rosana 49:36
It's called stone story, and it's about a rock that's in a creek, and he gets kicked out of the creek. And over the years, he gets kicked and damaged and thrown through a window, and then at some point, thrown in the trash. And then somebody digs them out of the trash and cleans them up and puts him in a special place in the wall of that's being built. And he's a shiny jewel. Yeah, nice.
Scott Benner 50:00
And what does that mean to you? Is that something you feel like happened to you?
Rosana 50:04
Yeah? I mean, I think it's a kind of a parable, I guess, or an allegory, whatever you call that, but of how people sometimes feel,
Scott Benner 50:11
you know, yeah, well, I think everybody has a good opportunity to be a part of that, of that wall like, you know, just what do you need? You need somebody around you that cares a little bit, a little bit of a little bit of self confidence. Maybe that's where you're, you know, where you could start for yourself, like along the road here, like, you know, people have been through some hard things. You've supported them and done a great job of being somebody's mom a number of times, right? You know, you tried to be a good wife, and just because the person on the other side of that doesn't receive it that way. Doesn't mean you didn't do well at it. You know, even the second guy who took advantage like you were, you were earnest with him, I imagine, oh yeah, yeah, right, I'd get out there and do it again. I'm not kidding. Persona like, what's the alternative for punishment? No, but what's the alternative? Now that you know this is how it could go. Anything better than this is going to be a win. So your bar is super low. So that's awesome. And the other seriously, Hey, you can't get let down, really, if somebody has sold your belongings. I mean, you know what? I mean, like, it's not good. He didn't sell him, he didn't sell him for meth. Did he?
Rosana 51:17
Life does not sound that bad in my head.
Scott Benner 51:21
Well, I'm trying to be fun. But my point here is that, like, you know, I'd say, get out there and try again now, you know, maybe put up a little more of a wall. Let's not marry anybody six months in. But, you know, thought the world was ending. I hear what you're saying in the moment, it felt like, I mean, I felt like it was ending to me too. I'm
Rosana 51:39
not. I rationally knew that. I think it was just, you know, emotionally, because I was also staring down I needed a full hysterectomy surgery, and I had no one to help me.
Scott Benner 51:49
Oh, you, Oh, you, you maybe did a little of, like, if I'm married, this will be easier,
Rosana 51:54
you know, and yeah, and then the whole COVID thing, and I got laid off, and then I was working from home, and it was just he was there, and he was helpful, and he was nice.
Scott Benner 52:06
Well, listen, put that right on your profile. Hysterectomy. Can't get pregnant. You know what I
Rosana 52:09
mean? Well, I'm 53 I don't think I could have anyway at this point, but
Scott Benner 52:13
we're going to be telling them you're 43 in the profile. So you gotta jazz this up a little bit. You know what I mean? Same thing you got to do with the book when you're selling it. Yeah, did you say it was about a rock or a stone? A stone? Yeah, that's good. Don't say rock stones better. Is it shiny the stone? Well, not to begin with, no, but at the end, it's
Rosana 52:31
shiny. It's been through everything it is, yeah, like a tumbler of life,
Scott Benner 52:36
exactly. Do you not see this as your path, too? Why can't you actually be that Shiny Stone. It could be just waiting for somebody to find me. What would have to happen for you to end up in that wall nice and shiny, I guess somebody coming along that actually saw me, for me, yeah, and not for what I could do for them. That'd be a damn good start, wouldn't it? Well, yep, let me say this, Rosanna, you're not going to meet those people in your apartment. They're not. They're not. I mean, look, unless they're at work. Oh yeah, you said, I think before we started recording, you said you work with, how did you put it? Tell me what you said, again, criminals and lawyers. She's like, I work with criminals and lawyers, and often, would you say the lawyers are worse than the criminal? The lawyers are worse than the criminals? Okay, yeah, okay, so yeah, for you specifically, let's not date at work. I think that's, that's an obvious one, especially like, yeah, I probably want to avoid cops to older cops, right? Yeah, yeah, no disrespect to older cops, but you all know what I mean. A little jaded by now, you know I'm saying, yeah, yeah, right. So what do we do? Like, do you I mean, I don't even know how to do this. Like, I'm sitting here thinking, like, if I had to go meet somebody right now, I swear I don't know what to do. But can I say this last summer, my wife went away for business, my kids were they didn't live here, you know? No, I was by myself, is what I'm saying. And I wanted to see that first mission, Impossible movie of the two parter that ends the series. The second part is out. Now. I want to see the first part. Nobody went with me. I went to a theater. I went out one night, made the podcast. I did my business was supposed to do, you know, and I went out to a movie, and I'm sitting there watching a movie. I am by myself. There's probably 10 people in there, not many at all. Movie ends. Lady in front of me turns around, looks. She goes, boy, I really love that. I said I did too. And we started chatting a little bit. She's a lovely woman, probably a little younger than me. She kept chatting with me as we walked out, she stopped me in the parking lot to talk again. And I thought, hmm, I could get this lady, and she was being very friendly, and she was lovely. And of course, me, being married in the that I wasn't there looking for a date, slowed down the whole thing. I said to her, it was really nice to meet her, and I left, and she went on her way. But we could have kept talking like if I would have said to her, if I wasn't, let me just be clear, if I wasn't married, I could have said to her. We should go. You sit down somewhere and get a drink and talk. She we would have gone. Now I don't know how that would have ended, maybe with her selling my belongings. I don't know exactly. I gotta tell you like I didn't expect that. And there it was. So maybe you just gotta keep putting yourself out there till something, something fires off. You know?
Rosana 55:19
Yeah. I mean, this woman obviously had more confidence than I do. I don't
Scott Benner 55:23
know about that. I think we were just caught up in the we enjoyed the movie, and we started talking to each other. Yeah, if she's listening, really pretty Indian lady in her 40s. I wasn't married, I definitely would have asked you out. We were having a good time so and all it was is that we had like, a mutual like interest. At the moment, it was enough to start talking about that. Don't go picking other people have self published their books, because then we're going to find more introverted people, and you guys are just going
Rosana 55:50
to sit still and not talk well. And everything I like is an introverted thing. I mean,
Scott Benner 55:54
well, there's a good point. What are some of the things you enjoy doing? I
Rosana 55:57
love history of museums and antique stores. And I do genealogy, I go to cemeteries.
Scott Benner 56:05
Well, these seem like things other people like to do. Why don't you? Like, that's awesome. Like, I mean, can't you find somebody else who enjoys like, I mean, let's start cheaper. Like, going to cemeteries, do that, and then, and then find somebody that wants to travel and go see other stuff and like, I mean, people love history. There's got to be other it's got to be men who enjoy that too, yeah. And they don't have to be like, it could be friendly at first, because you said you want people to get to know you, right? Yeah. Rosanna, this is done deal. I think this is easy. Let's get this accomplished. Don't do it through Facebook. I feel like I just sat through a therapy session, though. Do you feel good? Good enough to send me a co pay?
Rosana 56:47
Oh, but I'll send you a link to my book.
Scott Benner 56:49
Awesome. Not even offer me a free book. Fine. That's fine. Well, I'm glad that this felt good. Do you feel better now?
Rosana 56:55
Yeah, yeah. I'm obviously going to sit back and be worried about all the stuff I said. But
Scott Benner 57:00
really, do not worry about anything. I don't know anyone in my personal life. Well, that's upsetting to me. I wish everybody listened. No, I tried, I tried. Believe me, you get it out there. Thank you. Yeah, awesome, awesome. That is that. I appreciate that very much. Oh, I didn't even ask you, but does the podcast, is it been valuable for you with your son's
Rosana 57:22
diabetes? Oh, yeah. Like, right away, I found the Facebook page, and then, think her name is Nico. She had I asked a question. She posted a series bold beginnings. I think it was Yep. So I listened to all of those. And then I've been listening to defining,
Scott Benner 57:38
defining diabetes, going through different terms. You can understand what they mean.
Rosana 57:42
And then also, I listen to like, the new ones as they come out.
Scott Benner 57:45
Awesome. Well, I appreciate that very much. I do. And you've probably just made it so that Rob will drop the bull beginnings trailer right after you stop talking.
Rosana 57:53
It was a very good one. Yeah,
Scott Benner 57:55
I appreciate that. See, it's a series, as a lot of people seem to find, that it's helpful getting
Rosana 57:59
going. I mean, I reading Facebook posts on the group, I think we had a special understanding of diabetes because we actually went through diabetes education three times. How so, once at the hospital in the city, and then once at the rehab. And then when we came back, our endocrinologist made us go through education, like a five part education series. Okay, wow, so we got the same thing three times.
Scott Benner 58:28
And Was that helpful, or did you still was the bold beginning still additive for you?
Rosana 58:33
The bold beginnings was definitely helped fill in, like this is what we can really do, you
Scott Benner 58:38
know? Okay, took you from maybe more basic ideas to something a little deeper. Yeah, yeah, awesome. I'm glad, and I'm glad he's doing well, that's awesome. I hope he gets back to playing soccer. That would be I mean, I hate soccer, but I if he likes it, I'm okay with it. By the way, hates a strong word. I just don't understand it. It seems like track and field without purpose. It's a lot of running, a lot of running, not a lot of scoring, that's what I'm saying. Yeah. Nevertheless, those of you love it, I'm not saying you shouldn't love it. Continue on, and please stop sending emails saying, Stop talking badly about soccer, because that happens a lot. I just don't like soccer. It's no shade. It was really nice of you to share this. I know that was a really difficult thing to talk about. And then you talked about some personal stuff, which was, was really kind of you. I'm sure you're not nearly the only person living through, you know, being still young and viable, but feeling older and, you know, I mean, listen, we didn't really say it out loud, but what you're thinking, and that didn't say, is that, like people my age, the good ones are probably taken it's a lot of picking through the others to find the ones that are left, right, right, yeah, well, but if you don't pick, you won't find and I guarantee they're good people out there. Yeah, that's, that's the hope, yeah. And if not, you can always use male escorts. There's nothing wrong with that. Did they exist? And I. I, you know, I don't know. Hey, have you actually, like, lived through a heart like a tornado?
Rosana 1:00:05
I mean, not one that's actually hit me, but gone overhead and I curved it? I mean, I've been here most of my life, so they're always close frightening on a scale of one to 10. I don't get frightened by those kinds of things. Interesting, but definitely, I mean, sounded like a train coming,
Scott Benner 1:00:26
yeah, just cruising down the coming at you from, like, just a direction, yeah? So that doesn't scare you, but you do worry about things that could happen to my kids that don't exist. You always like that. Or was that after you had babies, after I had babies, for sure. Yeah, that's a, it's a God's little joke there. Yeah, yeah, I got you. All right.
Rosana 1:00:47
Well, I mean, yeah, even the ones that are grown up and out of the house,
Scott Benner 1:00:51
oh, good news. You don't stop worrying about them. Never. Jesus. All right. Well, this is good not spend the rest of my life doing that. I guess, Rosanna, you were really nice to do this. I know this was difficult for you, so I appreciate it very much. Thank you. Yep, hold on one second for
me. The podcast episode that you just enjoyed was sponsored by ever since CGM, they make the ever since 365 that thing lasts a whole year. One insertion every year. Come on. You probably feel like I'm messing with you, but I'm not. Ever since cgm.com/juicebox the podcast you just enjoyed, was sponsored by tandem diabetes care. Learn more about tandems, newest automated insulin delivery system, tandem Moby, with control iq plus technology at tandem diabetes.com/juicebox. There are links in the show notes and links at Juicebox podcast.com. Touched by type one, sponsored this episode of The Juicebox podcast. Check them out at touched by type one.org on Instagram and Facebook. Give them a follow. Go check out what they're doing. They are helping people with type one diabetes in ways you just can't imagine.
I can't thank you enough for listening. Please make sure you're subscribed or following in your audio app. I'll be back tomorrow with another episode of The Juicebox podcast. If this is your first time listening to the Juicebox podcast and you'd like to hear more, download Apple podcast or Spotify, really, any audio app at all, look for the Juicebox podcast and follow or subscribe. We put out new content every day that you'll enjoy. Want to learn more about your diabetes management. Go to Juicebox podcast.com up in the menu and look for bold Beginnings The Diabetes Pro Tip series and much more. This podcast is full of collections and series of information that will help you to live better with insulin. The episode you just heard was professionally edited by wrong way recording, wrongwayrecording.com

Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1584 Tiger By the Tail
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
Andrew, living with T1D for 31 years, and his wife Gina share their journey after their 3-year-old daughter’s diagnosis—while raising a toddler and expecting another baby.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Here we are back together again, friends for another episode of The Juicebox podcast.
Andrew 0:15
My name is Andrew gears. I was diagnosed at the age of seven or eight in late April, our three year old daughter, Brooke, unfortunately, got diagnosed as well.
Scott Benner 0:27
If your loved one is newly diagnosed with type one diabetes, and you're seeking a clear, practical perspective, check out the bold beginning series on the Juicebox podcast. It's hosted by myself and Jenny Smith, an experienced diabetes educator with over 35 years of personal insight into type one, our series cuts through the medical jargon and delivers straightforward answers to your most pressing questions. You'll gain insight from real patients and caregivers and find practical advice to help you confidently navigate life with type one. You can start your journey informed and empowered with the Juicebox podcast, the bold beginning series and all of the collections in the Juicebox podcast are available in your audio app and at Juicebox podcast.com in the menu. Please don't forget that nothing you hear on the Juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin.
This episode of The Juicebox podcast is sponsored by Medtronic diabetes and their mini med 780 G system designed to help ease the burden of diabetes management, imagine fewer worries about Miss boluses or miscalculated carbs thanks to meal detection technology and automatic correction doses. Learn more and get started today at Medtronic diabetes.com/juicebox today's episode of The Juicebox podcast is sponsored by the contour next gen blood glucose meter. This is the meter that my daughter has on her person right now. It is incredibly accurate and waiting for you at contour next.com/juicebox this episode of The Juicebox podcast is sponsored by the twist a ID system powered by tide pool that features the twist loop algorithm, which you can target to a glucose level as low as 87 Learn more at twist.com/juicebox. That's twist with two eyes.com/juicebox. Get precision insulin delivery with a target range that you choose at twist.com/juicebox. That's t, w, i, i s t.com/juicebox,
Andrew 2:47
my name is Andrew gears. I was diagnosed at the age of seven or eight, so I've had that type one diabetes for 3132 years now, and about 1212, to 14 months ago, in late April, our three year old daughter, Brooke, she unfortunately got diagnosed as well, which kind of came as a shock to all of us.
Scott Benner 3:08
And Gina's here too, your wife. So Gina is Brooke, your only child.
Speaker 1 3:13
No, Brooke is our oldest. We have another child, Graham, who is two years old, and we have another baby on the way. Do any week now?
Scott Benner 3:23
Oh, I saw you on camera. I just thought you had a big lunch. But does that what's going on?
Speaker 1 3:28
No, no,
Scott Benner 3:30
I wasn't confused. Well, congratulations. Thank you. That's lovely. Do you know what you're having?
Speaker 1 3:36
No, we're going to be surprised with this one. I think it's our final so we have boy girls. So we figured this would be a good last hurrah to be surprised. Did you know
Scott Benner 3:45
The first two when they were coming? Yes, yes. So have you shared at all with Andrew? Like, does it feel similar to one of them or the other one the pregnancy?
Speaker 1 3:54
I'm thinking it's girl. He is thinking, I think more boy. But also he's got such a special relationship with Brooke, which will come out through our conversation, that I think he's afraid for it to be another girl and to split his, you know, and you're you have a daughter. So, I mean, the daddy daughter relationship is, is very strong.
Scott Benner 4:16
It's fun most of the time. Yeah, although I'll tell you Andrew, as they get older, they they push back. So
Andrew 4:22
I both. I have a co worker. She always says, I enjoyed these first 11 years, because then our son's name is Graham. She goes, Graham's gonna become your best friend. So soak up these first 11 years, because that pendulum swings pretty quickly and aggressively.
Scott Benner 4:34
My son and I make the I'm scared face at each other once in a while. But no, no, it's that's lovely. Congratulations. How long you guys been
Speaker 1 4:41
married? We've been married six years. Six years this August. Awesome.
Scott Benner 4:45
That's great. You guys, you got busy and got started making, making a family, huh?
Speaker 1 4:49
Yeah. Well, we got together in our 30s, and we lived, you know, in Chicago. That's where we met. That's where Brooke was born. And then we moved to Louisville, Kentucky. So, yeah, you know, we kind of got all the fun out of the way early on, and we were ready for family.
Scott Benner 5:09
I just want to say now that you've mentioned Kentucky that I saw on the internet, I think it was yesterday, somebody took a replica of the General Lee from the Dukes of Hazzard and jumped it through a square over a fountain in Kentucky. Is there any way you knew that that was happening? I don't know how big
Andrew 5:24
Kentucky is. I did only because, and I'll be shocked you, and if you say that you were aware of this, I got a like, an Instagram reel, or a couple co workers had shared a video, because I do some work in that area. It's in Somerset Kentucky, okay? And I know the exact location where they did that. So I had a good chuckle thinking, God, that would have been fantastic. I was out there watching that live, but that's that's about an hour and a half from us. I have
Scott Benner 5:47
to tell you, prior to me seeing that video yesterday, my only story about Kentucky was at a waffle house, but this was a much better story. Also, did you? Did you see the video the cameraman that just got out of the way at the end of
Andrew 5:57
it? I didn't see that part. I just saw him just completely take off, airborne through that blue fountain. And I thought, okay, that is like the Sunday
Scott Benner 6:05
it comes crashing down on the other side. The guy loses it. It starts heading to the left. And there's a guy on the side of the road with a camera on the street, and he is committed to getting as much of that as he can, because he grabs that camera, jumps out of the way the last second it's I would have been gone much quicker than him, is what I'm saying. But nevertheless, casualties, no, they looked like it went okay. I think one of the doors fell off, but other than that, so I'm gonna just bounce around the way this occurs to me. So, Gina, can you tell me a little bit about what you recall about your daughter's diagnosis?
Speaker 1 6:35
Yeah. So, I mean, I remember it like when she was born. I was traveling for work, going to Chicago, and I was in Chicago prior to Brooke's diagnosis, we had noticed some erratic behaviors from her, and I just kind of chalked it up to toddler threes. You know, they say terrible twos, but really it's like terrible threes, just tantrums, and, you know, they were just becoming really extreme, really aggressive, crying, hitting, just more so than I thought was maybe normal. You know, our nanny, who happened to at the time, be a type one diabetic as well, had asked me, you know, have you ever thought about checking Brooke's blood sugar? Or do you ever think that Brooke could be diagnosed with type one? And this is something Andrew and I honestly never talked about when we were having kids dating, the likelihood of our kids ever getting type one. So I remember telling her No, but I'll, you know, run it across Andrew. And I remember vividly having the conversation with Andrew, do you think that Brooke would ever get type one? And he shot it down immediately. Absolutely not. No. And that was kind of that we never talked about, like checking our blood sugar, nothing.
Scott Benner 8:00
Can I jump in and ask Andrew, did you shoot it down so quickly because you didn't want it to be true, or because you didn't think it was a
Andrew 8:06
possibility? No, I just never thought there was any chance. I and we'll get into this, I'm sure. But I think that's why the day of her diagnosis, I just, I mean, I was stopped and stuck like a deer in headlights, feeling so exposed and ignorant, because it had truly just never crossed my mind, not for a single second. You know, Gina even references that specific conversation in our kitchen where she said, you remember the one time I asked, like, hey, what do you think the odds are that any of our kids would have type one diabetes? And he said very quickly, like, oh, zero, yeah. No chance. You know the way the doctors had kind of explained how my diagnosis had occurred, which I'm sure we'll get into at some point, I just thought it was, you know, no hereditary component, a series of events, a possible sickness followed by some emotional stress. But I never that never crossed my mind when we talked about family, growing family, the last thing that I ever thought about was potential type one diabetes presenting itself in any of our children. Yeah,
Scott Benner 9:07
do either of you have other autoimmune issues in your family line or personally,
Speaker 1 9:11
Andrew's mom, Andrew's family has autoimmune his mom is celiac. She's got shogrims. His sister celiac. They both have hypothyroid. Her brother was celiac.
Scott Benner 9:28
You have type one. Do you have anything else, Andrew, besides type one?
Andrew 9:31
Not right now, but I'll be honest. You know, Brooke's diagnosis has made me think I'm much more adamant about annual blood tests, getting the comprehensive panel taken care of, but right now, just type one, and I'll be honest, I look at what my mom, sister and brother like, what their diets entail, and their strictness around intense celiac as well. And you know, I always look at it and say, like, Hey, I just have to give some insulin. I can still eat whatever I want, but as long as I exercise and. Give insulin. So everyone's got kind of their challenges, and you got to play the cards that you're dealt. But at the end of the day, that's that's something that's definitely top of mind nowadays. So just being aggressive and out in front with that, with Brooke over the years, and making sure I'm getting my annual blood work done, and you know, our son, Graham, and our third child that's to come here in the near future, just making sure that we're doing what we need to do to detect that early and often, I think, is of paramount importance
Scott Benner 10:26
for us now. Gina, there is there any autoimmune on your side of the family? No, nothing. No. IBS, eczema, anything?
Speaker 1 10:34
No. I mean, the kids is babies, like Graham right now has eczema, and Brooke has had some eczema, but like nothing, that's extreme. I mean,
Scott Benner 10:43
I'm interested in my one question before I move forward, is the the friend that was like saying to you, like, do you think there could be type one? Do you think they were trying to hint to you that they thought it was type one? Or do you think it was just like an actual wonderment of theirs? I wonder if that's a thing that could happen. No,
Speaker 1 10:57
our nanny, I think she was expressing her concern that her behavior seemed out of the norm, and she's here today. She's watching the kids right now, and she's honestly a godsend. Her name's Donna, and I think she was brought to us, you know, for honestly, this very reason, if not, and many others, but lucky to meet her, yeah. So I'm in Chicago, and Brooke is with Donna Graham. Is not even a year old. He's 11 months. And something happened in the morning where Brooke just had, like a knockout tantrum that just didn't warrant any kind of reaction that she was giving Donna, sure, and Donna just something in her was like, This doesn't seem right, and she took it upon herself. She knew she was overstepping, but she's like, I just, I can't she finger poked her, because Donna is the type one, and she finger pokes herself all the time, and the meter just registered high. Is
Scott Benner 12:01
it just random that Donna has type one diabetes? Yeah, yeah,
Speaker 1 12:04
yeah, huh? How cool. Yeah,
Scott Benner 12:07
it's crazy, yeah.
Speaker 1 12:08
So you know, her meter ran registered high. So she's like shaking. She calls my mother in law because she was afraid to call Andrew, overstepping. And then the possibility of sharing this news. And my mother in law was like, Did you wash your fingers? Wash your hands, to make sure that you know there's nothing sticky on there. Did it again? And I think it was either high or force something crazy. High. Donna
Scott Benner 12:37
said, this isn't my first day. I know what I'm doing, but I'll do it one more time. Right, right?
Speaker 1 12:40
Yeah. So then, you know, my mother in law was like, call Andrew. He's, you gotta call him. He's got to come home. So she made the call to Andrew, and then I, I get a call from Andrew. I think I've silenced him first, because I was in a meeting, and then he's like, call me back. And I was like, Oh, that's not great. And he's just kind of rambling and crying. And I'm like, what? And he just tells me, Brooke has diabetes. Oh,
Scott Benner 13:09
gosh, how did that, like, hit you? Did you believe it? At first,
Speaker 1 13:13
I was numb. I was really calm. I was really numb. I was shaking because I wanted to get the hell home. You know, I got to the airport right away. I got on a flight right away. I remember calling my mom, and this is what he told me, I get to the hospital. I just see my baby in the hospital bed, Andrew's crying, you know, he's like, uncontrollable. And it didn't really hit me until we were checked in at Children's and, you know, she started to, like, claw at the door, wanting to go home, and she just didn't want anybody touching her anymore. She didn't want any more finger pokes and and then I'm like, thinking to myself, this is our life now,
Scott Benner 14:03
Andrew in that room, what's the crying? Is it just breath that something happened? Are you picturing a life for her? What is it that's got you at that moment? The brand new twist insulin pump offers peace of mind with unmatched personalization and allows you to target a glucose level as low as 87 there are more reasons why you might be interested in checking out twist, but just in case that one got you twist.com/juicebox, that's twist with two eyes.com/juicebox. You can target glucose levels between 87 and 180 it's completely up to you. In addition to precision insulin delivery that's made possible by twist design, twist also offers you the ability to edit your carb entries even after you've bolused. This gives the twist loop algorithm the best information to make its decisions with, and the twist loop algorithm. Rhythm lives on the pump, so you don't have to stay next to your phone for it to do its job. Twist is coming very soon, so if you'd like to learn more or get on the wait list, go to twist.com/juicebox. That's twist with two eyes.com/juicebox. Links in the show notes. Links at Juicebox podcast.com. The contour next gen blood glucose meter is sponsoring this episode of The Juicebox podcast, and it's entirely possible that it is less expensive in cash than you're paying right now for your meter through your insurance company. That's right. If you go to my link, contour next.com/juicebox you're going to find links to Walmart, Amazon, Walgreen, CVS, Rite, aid, Kroger and Meijer. You could be paying more right now through your insurance for your test strips in meter than you would pay through my link for the contour next gen and contour next test strips in cash. What am I saying? My link may be cheaper out of your pocket than you're paying right now, even with your insurance. And I don't know what meter you have right now. I can't say that, but what I can say for sure is that the contour next gen meter is accurate. It is reliable, and it is the meter that we've been using for years. Contour next.com/juicebox dot com, slash Juicebox. And if you already have a contour meter and you're buying test strips, doing so through the Juicebox podcast link will help to support the show.
Andrew 16:30
And I get emotional now sure about it. Think all of the above. And I knew when Donna called us, or called me, I should say about an hour away from home, and, you know, she was getting a little long winded, and I just said, Hey, I, you know, do you mind spit it out? I feel like something's coming. And she said, you know, essentially, hey, when you left, as you could see, she was having terrible, a terrible tantrum. And what Gina had left out was we were on a family vacation in Florida, and the week prior to that, she'd send me videos. I flew back a week early to work, and they stayed down there for an extra week with Gina's parents, and she was sending me videos and said, you know, these are so abnormal. And of course, at this stage, she's eaten, you know, chocolate chip mini muffins for breakfast, you know, Skittles for lunch. You know, just normal stuff. So in that moment, I think there was a lot going on. I think first and foremost, I was thinking like, How in the hell did you miss the exact signs of her diagnosis that you had? Yeah,
Scott Benner 17:27
I wanted to ask you, do you know, I mean, you were young, do you remember anything about your own
Andrew 17:31
I remember two specific events. I remember going to the barman Bay. I think it was Barnum and Bailey, you know, the circus, yeah, when, when it used to be actual animals at them. And I remember drinking. I still have the cup at my parents house, but, you know, one of the extra large cup had a tiger tail, is the cup holder, and still at my parents house. But, you know, those are pretty large, and I was just downing drinks. I mean, Sprite after sprite after Sprite, then water after water. My mom wasn't a registered nurse. She's retired now, but for a few nights leading up to that, that circus, she told my dad, you know, I think he's got diabetes. He's up urinating, he's drinking so much, no bed wetting, nothing like that. But just, you know that the telltale signs that are present, but it's just hard for people to act on right until there's an actual diagnosis. So I remember that, and then I remember one day it's been too weak to go to school, and I remember the finger poke at the doctor's office. It was like five something, getting to the Children's Hospital, and then, you know, I was in there for, I think, about five nights, I want to say, with Brooke. Luckily we caught it early enough, where it was a one night stay at the hospital. It just felt like two weeks as I'm sure any parent who has a child with type one diabetes that that probably resonates with them. But, you know, in that moment, I just remember thinking number one, like, how, how in the world we were just cracking jokes about her bathroom usage. She was potty training. And then every 20 minutes she'd be on her little, you know, little toddler toilet filling the thing up, you know, that was the first thing that just really pissed me off. I was angry at myself. And then number two, when Donna had called No, just thought through all of, you know, the challenges and just yeah, you feel like some of their innocence is just kind of stripped and stolen, you know. And you look at a three year old and how did that happen, and why? And the mind is, you know, it's a powerful thing. You know, luckily, when Gina got there, she's always kind of been the rock, and she jumped to it. I was kind of frozen, stuck, you know, just letting my mind race a little bit. And like Gina had just mentioned, that first night in the hospital bed boy, when Brooke was kind of clawing at the door. And you know how regimented it is during the diagnosis period? Hey, here's her food. She has 30 minutes to eat. In 30 minutes, we're going to come back, take the food and give her a shot. And it was, you know, just the reality, like, wow, in the moments notice, like, things have changed very drastically, and this isn't temporary.
Scott Benner 19:57
So how was your experience growing up with. Have fun. I give my parents
Andrew 20:01
all the credit in the world. It wasn't a factor. I mean, I had the lows. I had the highs very early on. I remember in second grade, in order to do sleepovers and overnight camps for soccer and basketball, it taught me the importance of being able to kind of control your sugar, check your sugars, give insulin, give your shots. It was insulin and mph at the time. So, you know, my mom would roll it up in an aluminum foil label, everything, the notes on when to take it so it was present, that's for sure. But, you know, I didn't have an understanding around it. I still remember coming back from the hospital and going back to school. Yeah, you know, no one could eat or drink during class, but the teacher had juice boxes and peanut butter crackers in her drawer. And I remember that first day walking up there saying, I need another Juicebox and another pack of peanut butter crackers. And the teacher said, Hey, you're you're all out. I don't know. I don't know if that's the way it's supposed to be, but I just remember thinking like, how great is this? I can eat and drink in class, and no, no one else can, you know? So I'd say the first few months was learning, and then my mom saying, hey, probably breaking it down in more of layman's terms, so that an eight year old can understand right when that is designed. And the question I always ask myself is, could I feel a low blood sugar at that age? Because what I always tell Gina is our lives, and any, anyone who has a toddler or a baby, I just remember life becoming so much more independent when I could feel low coming on or a high that was hitting me. You know, your body just kind of tells you what's going on. And, you know, I always look at it during the rough patches, like in the middle of the night, when we can't sleep because all the sirens and the alarms are shooting off from her phone, Brooke phone, my phone, you know, you feel like you're in the middle of a war. Yeah, I just keep on saying like, we're we're getting there. You know, you see a three year old become a four year old, and the growth that takes place. And, you know, in my mind, I'm just thinking, we're in the thick of it right now. As anyone with a like, I said, a baby, a toddler, an infant, probably is, but once that individual's body can say, hey, I'm low, I'm high, your body wakes you up naturally. When you do go low in the middle of the night, that happens for you? Oh, gosh, yeah. I mean, I didn't use a CGM in a weird way. I remember listening to the podcast with, I think it was Noah Gray, the chiefs tight end, but where he talked about the blessing that he's been given with diabetes. And, you know, I chuckled at that at first, and I was thinking, like, boy, this guy is he's got more faith than I do. Let's put it that way. I looked at it like the one positive that has come from Brooks diagnosis is it has forced me to use updated technology. I always despise the CGM because the readings wouldn't be accurate with a finger poke. I'd go into exercise, the CGM would say I was 140 within 10 minutes, I was taking like a glucagon pack to get my sugar up to where I need it, and there's a 60 point differential. But you know, through Brooks diagnosis, I didn't want her to start wearing a CGM with a no on a three year old that patch takes up looks bigger, yeah, takes up an entire butt cheek or the back part of her arm. So, you know, in solidarity more than anything. But then through her getting it, it has been a blessing with, you know, control when my a 1c is finally where it should be, and as hers comes down, my comes down. So,
Scott Benner 23:06
yeah, let me ask you that, like, so I get that while you're growing up, your mom says, you know, hey, you can do anything. We're going to play sports. We're going to do a list. You just need to do these shots. When I tell you to you do that. But outcomes wise, what was your a 1c like, as a child and through, like, high school, into college. Oh, I'd have to
Andrew 23:23
take a look at that. I mean, even recently, I look at the last trend chart, because I took a screenshot to compare my chart with my results to Brooks. You know, I was consistently, I'd say the last few years, eight, one to eight, five, okay. I'd always tell myself, that's not bad, because the endocrines would say, oh, you know, pretty good. You should use advanced technology, closed loop systems. And I'd say, Yeah, thanks, but no thanks. And that was the end of it. So
Scott Benner 23:47
even to up to recently, you were an MDI, were using a pump. I've always
Andrew 23:51
used a pump, okay? And my interference said, Hey, man, you got a Ferrari, but you got cloth interior, roll up windows and no radio you gotta use,
Scott Benner 23:59
right? Let me ask Gina. Now he's sitting here telling this story about growing up and all this. Do you know any of that before Brooks diagnosed? Is that a thing that you guys actually spoke because it occurs to me that if you got married a little later in life, that might be a thing you don't talk about.
Speaker 1 24:15
So I remember his mom telling me the story of him getting diagnosed and just this little tough guy walking around the hospital with his, you know, his IV card, and just, you know, determined as hell, which is Andro, it always sounded like from the stories. I mean, yes, he had diabetes, but he was never deprived of anything. So in terms of food, like,
Scott Benner 24:43
yeah, and that was more, how you how she told the story, yeah, now that your kids had diabetes for how long? Just 18 months, yeah, since April. Yeah. Do you look back and wonder, where were all those other stories were? How come they didn't those stories didn't get
Speaker 1 24:57
told, you know, I mean, now. We share now we swap more stories, for sure. And you know, I give Anne so much credit because she didn't have the technology that we have. The fact that you wouldn't even know what your child's blood sugar was, and you were just always going in and finger poking. Imagine that, right? You know, is kind of crazy.
Scott Benner 25:21
Yeah, it's interesting how the technology changed everything. Yeah, prior to diagnosis of Brooke, if Andrew had a story about, like, a kid in school that said something about him, about diabetes, or a time he got really low, or, like, did you hear about any of that as a thing you knew and it just seemed like this anomalous thing, or is it something you didn't speak about. Today's episode is sponsored by Medtronic diabetes, who is making life with diabetes easier with the mini med 780 G system. The mini med 780 G automated insulin delivery system anticipates, adjusts and corrects every five minutes. Real world results show people achieving up to 80% time and range with recommended settings, without increasing lows. But of course, Individual results may vary. The 780 G works around the clock, so you can focus on what matters. Have you heard about Medtronic extended infusion set? It's the first and only infusion set labeled for up to a seven day wear. This feature is repeatedly asked for, and Medtronic has delivered. 97% of people using the 780 G reported that they could manage their diabetes without major disruptions of sleep. They felt more free to eat what they wanted, and they felt less stress with fewer alarms and alerts you can't beat that learn more about how you can spend less time and effort managing your diabetes by visiting Medtronic diabetes.com/juicebox
Speaker 1 26:48
No, so, I mean, while we were dating and everything, I remember, like, you know, we would have like, a night out of drinking. I would always get like, low blood sugar in the morning, and he would finger poke me in the morning just to see what it was, and he's like, Yeah, you're not low.
Scott Benner 27:05
You're fine. You're just hungry and hung over, right, yeah, right. I do
Speaker 1 27:09
remember vividly, though, a story he told me of when he was traveling and we were dating, where this was probably one of his worst lows and the scariest low he had. He was dreaming, and it was me in the dream telling him he has to wake up. You got to wake up, go to your backpack. And he was so low, he like, was able to manage to get to so when I hear that, I'm like, oh gosh. Like, yeah, you know, because he's never made it a big deal,
Scott Benner 27:39
and I'm sorry. I feel like this is important, this first marriage for both you, yes, yeah, yeah. So this was like, you guys were busy building careers and doing stuff like that, yeah, yeah. Okay. And when you're dating Gina, does it ever occur to you, like, if I'm marrying somebody with red hair, my kids might have red hair. If I'm marrying somebody with diabetes, they might have diabetes.
Speaker 1 28:00
I mean, I thought about it more, but to myself, like I never brought it up to him, because it was something he never, he never talked about. He never talked about his diabetes as like a deficiency. You know, it was never, it never held him back in any way. I mean, he's physically fit. He's an athlete. He played d1 soccer, yeah, it was never an issue, okay? I mean, he would have cocktails on our honeymoon. We went to Italy. He ate pasta, you know? I mean, so it never limited our experience. So
Scott Benner 28:36
looking back now with your your new life experiences, do you think he should have told you more? Is your level of understanding of diabetes prior to Brooke and after? What's the swing? Do you know what I mean? Like, oh,
Speaker 1 28:49
it's extreme. I mean, so when we were in the hospital, I had told the nurses and the educator, I'm like, talk to me like I don't know anything because I don't know anything. Like, I never understood carb counting. I mean, I still was like, not even understanding like, and I feel silly saying this now, but like, when you give insulin, it's because you're, you know, you're too high, not because you're low. And you eat because you're low. You know, I never even understood what he was doing.
Scott Benner 29:22
So Andrew, my two part question is, is, did you not tell her that stuff on purpose? Or were you not really that keyed in? Like, is this a situation that, like, after Brooks diagnosed, you learn so much that you look back at yourself and think, God, what was I doing before this? Or did you know and it just wasn't a thing you shared?
Andrew 29:38
No, I never concealed anything. I've shared this with Gina. I have learned more in the last 1415, months from her diagnosis than I have in the combined 3031, 32 years that I have had it because you're worried about her now, yeah, that's an understatement. Yeah, that's a given. So when I was growing up, I mean, it was different. And this is funny, because, like, my mom brought my diagnosis pamphlets from like 1992 thinking that they could be beneficial for Brooke. And you've talked about this on previous podcasts where, hey, if they're low, give them 15 grams, and wait 15 minutes if they're still low, give give them 15 with, you know, suggestions on insulin shots, because this was before technology was available, but the game has changed so much in terms of just resources and educational content that are out there. Finally, I always tell Gina this, I said I've learned more from the Juicebox podcast, and I sincerely mean this, than the 20 plus endocrine centers that I've gone to with all the different areas I've lived. And that's not a knock on any of them, but sure, I think traditionally, people just want to avoid hypoglycemia as much as possible, and that's it. And I think that was evident when you when we went in for Brooks first, you know, I don't know if it was three months or six months, but her follow up and her a 1c was like in the high eights. And they said, Oh, this is great, and she's in range 55 or 60% of the time. And I said, I know it can be better, like I'm seeing people on the Facebook group and on these podcasts that are achieving, you know, unbelievable numbers in the mid fives and low sixes with toddlers like this can be done. So I think it really just lit a fire under my rear end to making sure that, hey, I'm going to do everything in my power to make sure that she gets a head start with this where her a 1c is in great control. We develop those habits early on. We're definitely getting better. We haven't arrived, and I don't know if anyone ever truly does, because the disease state changes
Scott Benner 31:34
and flows too. Man, like sometimes you got it, and then the next month you're like, what happened? Do you know what your a 1c was before her diagnosis. Her a 1c or mine, yours before her diagnosis. Where were you settled in at 8.1 and what are you now? Five, seven? Wow, wow. That's crazy. Good for you. You
Andrew 31:51
know, I got an insulin pump, metronics. First one, it was like this intense indigo blue. My thought it was cool as a 13 year old and big old block. But, you know, that didn't, that didn't, that didn't have a closed loop system or anything, no really intelligent about it. It was just one large, massive insulin shock, for lack of better words, with a basal. But you know, ever since switching over, really understanding how a CGM works, again, I do ask myself, like, if I understood that it's not reading the blood, but it's reading the tissue. And if I understand that, there's usually a 10 to 15 minute delay, 15 minute delay, what I've stuck with that 10 years ago, when an endocrine was successful with getting me to initially trial it, you know, these are the things I'm glad I slowed down, and it was nice, you know, Gina is much more patient than I am. So really saying, hey, if this could benefit long term, we need to, you know, give it a try. And
Scott Benner 32:40
it would be nice if they would realize, like, Look, someone had to go first, right? Somebody had to make a CGM, and it was going to be what it was going to be, right? But there should have been some sort of plan in place to say, we're going to slap this thing on some people, and it's not going to be the magic that they expected to be. Like, I guess they didn't know. But like, now, in hindsight, there's so many stories, like, a bad CGM experience puts people off for like, a decade before they try it again. That's not uncommon, right? That story of yours if, like, Okay, I tried it, I didn't like it, or it was super inaccurate, or woke me up in the middle of the night and wanted me to calibrate. All that, whatever this story ends up being, there's a giant like, some people called that first Medtronic CGM they would like, playfully call it like a, you know, a harpoon. And then, yeah, that's not a playful thing to call something. Now, their new one, there's Templar one, which is, I think, just about out now, like looks like the rest of them, looks like a Dexcom, looks like a libre like little, tiny thing, you know, but, yeah, put you off for such a long time. So are you telling me that, like, when she's diagnosed? Do you think, Oh, my God, my a one season the eights. This is how I know how to take care of diabetes. This is what's going to happen to Brooke. Or were you still like, this is good. Like, they told me, I'm doing okay. No,
Andrew 33:50
I knew an eight was high average at best. Yeah, exactly, yeah. Air quotes over here, as I say, average. But you know, in hindsight, my overnight high, so the amount of time I'd wake up at 181 90. Now that I'm on a closed loop pump, you know, I wake up like 110 without doing anything, and I just think, like seven to nine hours, six to eight hours, however many hours that is. But that's at least 25% of the day where you can be in the low hundreds. That's a lot of time. You know what I
Scott Benner 34:17
mean? You're saying, even if you reach that 180 overnight, you don't wake up at it because it's pushing it down the whole time.
Andrew 34:23
No, I will. I've become a little obsessive with this now. Like, it's become a game where, like, okay, you know, where can I keep my three day average on my g7 or, like, on the tandem app, like, can I get it to 100% in range? So, like, if I start flirting with my high limit on my CGM, which, you know, again, even the simple trick on that episode, I think it was you and Jenny who did it, but where you talk about changing the preset high number, where, why 180 or 200 whatever it is, if you set it at 140 and you're heading in that direction, you know, you can kind of bump and nudge it in the right direction. So, you know, implementing stuff like that has worked. And then if I notice a trend, because a lack of extra. Size, or maybe more of like a starchy carby meal before bed, I'll set an alarm like, you know, if I'm, let's say 160 I give whatever the tandem suggests, maybe a few extra tenths of a unit. And then I'll set an alarm for two hours just to make sure that it's heading down. And if not, I'll kind of, you know, bridge Bolus a bit more to get it where it needs to be. But it's, you know, it's become almost like a competition, which, you know, that's why it's down to a five seven at this point.
Scott Benner 35:25
And Gina, does that surprise you about his personality? No, here's my question. Why do you think he didn't do it previously?
Speaker 1 35:31
I think, I mean, he's also very stubborn, and I think he had one bad experience or then, you know, he just gets turned off, and it's kind of very hard for him to revert, you know, to change his mind about something, you know, this kind of competition side that you're hearing of him. And this, you know, obsessive compulsive. He also has it with Brooke and her diabetes, yeah, which is a little hard for me, you know, as the mom again, I don't know what they go through, I don't feel what they go through. And this is where my experience, you know, is is different than his. You know, Andrew has played such a big part in caregiver of her diabetes that it's been a big adjustment for me, especially as a mom. You know who you know knows their children's cries, knows what they need. It's like mother's intuition. That is not at all the case right now. Why
Scott Benner 36:31
is it hard for you? Is it hard to see someone besides you know what to do for her? Yes, yeah, okay, absolutely. You liked it better when he was just a dummy over in the corner and you were, like, handling everything, yeah,
Speaker 1 36:42
you know, like, you know, I nursed her, you know. I mean, I did everything, and he, you know. I mean, he always had a special relationship with her, but now it's on a whole nother level, and I love that for them, you know, everyone tells him when we tell people, yeah, we have a daughter with type one. Oh, my husband's actually type one too. Oh, wow, that's so great. You know, that's great for her. He's like, Yeah, but no, I think yes, because he has already so much knowledge, and he's gained so much from your podcast, more than I have, because this is his language. This is what he knows. And he's also in the medical field, so he just gets the stuff little easier, a lot, yeah, a lot easier than I
Scott Benner 37:29
do. Okay, did you try bold beginnings? Yes,
Speaker 1 37:33
yes. And I do. I listen to it when I'm on the treadmill or taking the kids for a walk, and I love all of that, and that's been so helpful for me and understanding. But like, he knows how to go into the Omnipod and set the settings and change this and change that. Whereas I'm a little bit more like the doctor's telling us we need to kind of do this way, oh, he is very much more like, no, no, I'm pushing back. I don't like this. I know it can be better where I'm very thankful for him, because if he didn't have diabetes, I don't know if we would be like this.
Scott Benner 38:09
Yeah. How it would be for you? Have you ever had to help him out of a low Has he ever had a seizure or been unable to help himself?
Speaker 1 38:15
No, okay. He's never had to use a glucagon pen, but you have them? Andrew, yes, yeah.
Andrew 38:21
Since Brooks diagnosis, I started, I was gonna say you didn't have one before, right? There was a gap from 1996 to 2024 let's, let's call a spade a spade. But I, you know again, that I always wondered, like, why do people need this? When I get a low in the night, like, I'll wake up everybody and everybody is different. So like, I'm fortunate, my body was very in tune, especially with lows. I mean highs. Like, I used to be able to sit around probably mid twos, low twos all day long and not realize it. But the lows, my body was always very attentive and responsive. Only twice did I have episodes where and both happened after flights, which I'm still trying to crack the code on something happens on flights where, like, even if you're high and you give insulin, it doesn't want to come down on the flight, but when you land, like, 45 minutes later, it's like it hits with a double whammy. And those are the two times I had scary lows. I'd say those were dangerous lows. But luckily, no seizure, no medical attention needed. It was just putting as many Skittles and a Swedish Fish in my in my mouth as I could. And just, you know, chew, swallow, and just know that in the next 10 to 15 minutes, the sweating will stop, I'll be able to feel the fingertips all that sort of stuff. But wow. I mean, those were road the two incidents, both after airplanes, which now I'll put my my pump into activity mode. I tend to go in a little bit higher. I don't let it give auto corrections, so I'm starting to figure that out. But something with gravity or flights or the pressure in the cabin, yeah, I
Scott Benner 39:50
think the pressure, we have an episode somewhere, but the pressure can push the insulin through the tubing, and so you end up getting some insulin that's in the tube. So if you're on a tube pump, you could end up getting more insulin that way. That's
Andrew 40:03
probably exactly what it is, because I've always been on one,
Scott Benner 40:06
yeah, that could be that, for sure. There's a thing they don't tell you. One thing
Andrew 40:10
that Gina had said, I'll never forget this. She made a comment, she's been fantastic, like I I sympathize with anyone who walks into this situation without any kind of previous experience, because it's a lot and, you know, to your question earlier, I think you had said, like, hey, what you know, did you think about telling her? The reality is, like, no one really understands diabetes unless you you have it or you're intimately involved, whether it's your child or spouse or someone living with you, like, there's, there's so many ebbs and flows to your point that a lot of times, I just there wasn't a point in chatting about it, because the person typically confused type one to type two, or the conversation would turn to like, Well, do you eat a lot of candy?
Scott Benner 40:51
Yeah, yeah. So you didn't mind her knowing. You just thought, like, maybe there's not going to come a lot of it, of that conversation,
Andrew 40:58
yeah, that and it was never real. It's not like I hit it, like she saw my pump on, you know, our first date, hey, I'm gonna give insulin real quick, which, you know, it's, it was just part of me, and that's how I look at it. With Brooke is like her baseline will be having type one diabetes. She won't look back and say, like, I have a co worker who got diagnosed after he was in the Navy and got it while he was in the Navy. Yeah, that'll get you out of the Navy. So, you know, understanding what life was like before that or after it. Like, the good news is this will be her baseline. So I look at that as a positive
Scott Benner 41:29
tell me the difference between before you started listening to the podcast and now? Like, what do you do now that you didn't do before? Like, this is a big change. You moved your A, 1c almost three full points. So what would you tell people was the difference?
Speaker 1 41:45
Well, and I'll just chime in too, yeah, please. Brooks a 1c is 5.7 Okay, and she was like, probably, I think she was nine when she got diagnosed. So I mean, all of the things that Andrew has learned through your podcast. I mean, yes, our endo team has been lovely. I think we've now found a doctor that we will see consistently, but the tips and tricks have not been from them, okay, it's been from your podcast.
Scott Benner 42:16
Okay, yeah, yeah. And, but you know what I mean, Andrew, like data specifically? Yeah, here's my first question. Is, what you're doing now, more or less effort than before, less is the short answer. Okay? And is it because you're putting the effort into more valuable places?
Andrew 42:33
Yeah, I care. Finally, you know, I was never one of those who hit a rebellious day saying, Woe is me. I'm not going to live my life and not going to live my life and not care about this. I'd still give insulin, but I wasn't given insulin 10 to 15 minutes before a meal, right? If I was going high, I'd give a unit. I'm trying to think what I used to do with the Medtronic pump I had when I didn't use the smart feature, but I'd give it. I checked my blood profiles, 214 it would have insulin on board, but didn't make any auto correction. I just give, you know, to me, that's another two units, and if I started to go low, then I'd pop a yogurt pouch or some Swedish Fish, life saver, whatever it was in my bag. But I was Yo yo, and a lot more. So for me, I'd say, becoming a little more consistent with what I'm actually eating now too. And thanks to the CGM, you know, I realized the effect that certain foods have on me now. So like pasta. I'll eat pasta if I go to a restaurant and the pasta looks good, but for the most part, I steer clear of it, just because I can control the sugar the first maybe hour to maybe even three hours after I eat it. But middle of the night, I look at and I'm like, How did I go up to 275, yeah, you know, the closed loop still got me back down to like 121, 10, with due time. But I'm just starting to realize certain foods hit me a little bit differently. We talk about the complexities of the disease state. The hard part is, I was at dinner with my coworker. He had tuna sashimi and, like, some kind of steak. So to me, I wouldn't give anything. He gave two and a half units, and I said, for protein only. Said, Oh yeah, this will spike me throughout the night. So, you know, next thing I know, I'm experimenting with seafood and steak like, will this drive my sugar up? And it really didn't. But, you know, I share that story just because it's just different one person to the next. So, so for me, the pre bolusing was huge.
Scott Benner 44:16
Okay, not a thing somebody ever told you to do, or a thing you knew to do that you didn't do.
Andrew 44:20
I believe when I was younger, my mom, which would have come from the endocrine and said, like, let's try and do this 30 minutes before you eat. But I was eight, you know, 1012, I said, Okay, I'm just going to start eating because I'm hungry. And, you know, I think that was the end of it. I think as a parent, you don't want to restrict your kid too much. I totally get that, yeah, and that never changed. You know, through my teens, through the college years, through the post college years, still going out eating whatever that was, one small thing that the trend with the arrows, like understanding what an arrow straight up, an arrow to the right, like I'm more comfortable and very confident in bumping and nudging that down now and catching it with a gummy or two. Or a little bit of yogurt when I see it start to take off, maybe a little bit more aggressively than what I had hoped, and to what Gina had had said earlier, like, we do the same philosophy with Brooke now, like even today, she has a granola bar every day for breakfast, like some banana chocolate. Try and keep it as unprocessed as possible. We have it down to a near science, I'd say. But today, for some reason, she went up to 240 So Gina had text me and said, Hey, did you give her a different bar this morning? No, it's her usual one. And I look at the follow app and she's 252 60. So I said, Hey, do me a favor. Rage bolster with one unit. We'll catch it when it's on its way down. But you know, the same things that I've learned just from listening to the podcast we're putting into the actual play with Brooke now and again, she went from a 9192 I forget what it was, where they were saying, like, Oh, this is good to you know, hey, let's really be adamant. Let's figure out what's working what's not. Let's start trialing some things. Like, I know there's room for improvement, yeah, for a four year old like their their diets not as regimented as an adult. So trying as best as we can to apply what we can without we want her to be a normal toddler. There's no doubt we're never going to be the parents, and I applaud those that can do this, but she's not going to have, you know, greens and protein, like she's going to eat what her little brother's eating, or she's going to have cake at the birthday party, and we look at each thing now, as you know, not really a failure, but a lesson learned. So like now, we know when we do cake, maybe we need an extended Bolus, or maybe more more insulin upfront or with more lead time, but that was a painful lesson to learn. I'd get so frustrated and irritated at the erratic blood sugars early on. And you know, to Gina's point, she's trying to figure things out, right? She has no idea what this disease is, because she's never needed to know it.
Scott Benner 46:47
Can I ask you, Gina Andrew leaves for a week, goes away from work, how much of this can you accomplish? Or do you just go into like, does it become him helping remotely? Or do you just accept different outcomes?
Speaker 1 47:00
Oh, it's a little bit of both. So it's like, if I'm, you know, if Andrew's traveling for work, I mean, even, like, so now I'm fully staying at home with the kids, which has been great. But I tell them, like, you know, let me drive. Like, I know I'm not going to be yes, chime in. But like, let me do it a little bit. And if I make a mistake, I learn from it. We'll fix it. We definitely communicate together. He gets a little bit more upset. He would like me to or he would like her to stay pretty strict with what we know works, and we know not every day is going to be the same, even if she eats the same foods, okay, but at the end of the day, she's also four years old, and the granola bar she liked today, she's maybe gonna like tomorrow, right? So I just sometimes, I also have another kid here, a two year old, and I just sometimes I just don't have the fight in me. So
Scott Benner 47:58
Andrew, Does that scare you? Or are you up tight and you can't be flexible?
Andrew 48:02
Depends on the day you catch me, I guess. But I think I was out for a full week in January, and she ran it perfectly. Yeah, she does a fantastic job. Now, honestly, I'm more of a passenger. I mean, I still have the follow app up quite a bit, just kind of, kind of looking at it, because she Brooks doing summer camp. Now that was a little bit of a concern, because, you know, the swimming in the water phone doesn't project the sugars, and she still can't. I always ask her when she's low, hey, how do you feel? And she can't really articulate that yet. I think once she said, I feel fuzzy. So I was like, Okay, we're getting somewhere.
Speaker 1 48:38
She felt wiggly, wiggly.
Scott Benner 48:41
Yeah, I think I've heard wiggly before, good. I mean, she's so little, right? Like, yeah, the word she has her are pretty limited. What's her understanding of her situation?
Speaker 1 48:51
Oh my gosh, she is so aware. And it's almost like, and I hope this never changes, but it's, she's, you know, she'll tell people I I'm a diabetic, and this is my Omnipod, and this my Dexcom, and now I have one, and we just recently changed to one phone, so we are just, you know, graduated to the one phone. Oh, yeah, sure. Not using the controller anymore. Was a bit of a nightmare, because re learning the algorithm, and she was yo yoing, and we didn't have the auto correction turned off.
Scott Benner 49:26
Oh, she's on the pod five then, yeah, correct. Okay, and Andrew, you're using Moby. No, I use tandem tea slim too. Okay. Did you upgrade the new control IQ, the the new algorithm? Has that been different for you. I was
Andrew 49:41
Medtronic all my life. I was laughing when he said, the harpoon like first thing, when I saw the auto inserter similar to the Dexcom g7 where, like, it's, it's standardized. It's a uniform application each time. You know, I was used to for 34 years. Using that Harpoon, you got to angle it right with that long needle, where, if it hit, like. Man, if it hit the wrong spot, that thing would hurt. I switch over the tandem T slim too, because again, I was in that mindset of like, hey, if Brooke is using all this closed loop technology and our devices communicate, I I need to be able to understand that and experience it myself. So I did tan MT slim two. And then for the CGM, we both use the Dexcom g7 Yeah, because the g6 when we started that was, that was a bear. I remember you had to use the gun to insert it and then attach the adapter as well. Kind of pop
Scott Benner 50:30
it in, yeah? You pop the transmitter into the sensor bed. Yes,
Andrew 50:33
yes, but that the pop would freak her out. So we did okay, two or three tries with that, and then I had messaged the Facebook group out of curiosity, like, how are people doing this with toddlers? Our three or three and a half year old just freaks out, and it's, you know, the tears I have flashbacks to when we got back from the hospital and Gina had said, I don't know how we're going to do this. I literally just had to pin her down in the pantry to give her an insulin shot. Lo and behold, like the g7 something had changed with the software, where you could use it now with the PDM, but also have an iPhone for I forget what it was, but we switched the g7 early on, just because that one step application process was a game changer, and that pop that the device makes it was just so much more subtle and gentler. I think mentally for her to overcome that was significantly easier. Okay,
Scott Benner 51:23
it makes sense to me. Gino, yeah. Gene, what's your level of comfort? Like, seriously, like, Andrew just disappears. He poof, he's gone. You're good. You think you could do this forever?
Speaker 1 51:34
Yes, I just don't have, like, I mean, I know I would get it, but like, the the pushing back of like to the doctors, and I know this can be better. I mean, I know I would be able to take that on. That's my only thing, is just really understanding the technology of it, like the Omnipod, like nobody ever satis, like when we got her on the Omnipod, this was so frustrating. We got the transmitter phone, and then we find out you don't need that because you want to do the follow app like nothing was or maybe it was communicated to us, and we were just in such a fog of like, follow it. Well, yeah, but I'm like, What in the hell? Like, nobody is making this easy.
Scott Benner 52:22
You know, it definitely isn't easy. None of it's easy,
Speaker 1 52:26
you know. And like, we're buying these devices, and, I mean, you know, we're fortunate where we can but like, if somebody wasted their money on that, and that's like, a $200 expense like that was just so frustrating to me, or the Pre-Bolus seen and, you know, setting the target range, you know, your target range shouldn't be 300 like, that's absurd. It should be, you know, realistically, 160 nobody's ever talked to us
Scott Benner 52:53
about that. That's crazy. You're at a pretty made a reasonable size, like Children's Hospital and everything when you were diagnosed and all, and your endos seems to know what they're doing.
Andrew 53:03
Well, we never deal with we, I don't mean to interrupt, but we didn't really, we didn't really deal with endos, to be honest. We had a variety of care team personnel, but we had brought that up as a concern in our last appointment, so we have one now, but
Scott Benner 53:16
nurse practitioners, people, yeah, and
Speaker 1 53:18
your messaging through my chart, and they won't, you know, get on a call it, yeah, it just didn't. We didn't feel like we had individualized care for her, where we just had a doctor that was getting to know us and getting to know Brooke, yeah, and we expressed that. I mean, it got to the point where I had called Andrews endo from when he was diagnosed, is still practicing up in Cincinnati Children's, and I reached out to them, and I'm like, I'm going to make a damn appointment with him, like, if we need to go to Cincinnati every three months, that's whatever. Yeah, but I think we're on a better track now, okay, but I mean to answer your question, could I do this if Andrew wasn't in the picture? Absolutely do I think I would do I think I benefit having Andrew as my partner in doing this without a doubt.
Scott Benner 54:12
Yeah, no, obviously I just wanted to, yeah, kind of understand where you were, where you're at in the whole thing. Yeah, yeah, Andrew. So can I ask you, do you think you were motivated like to do better for yourself so that you knew what to do for Brooke. What's the thing that pushes you deeper than just, oh, my daughter got diagnosed, so I paid attention to like, what do you think the psychological component is of you saying I've been 8.1 my whole life? But that's not okay, and I can fix it like that.
Andrew 54:39
I think priorities change, obviously, especially as you know your family grows so, you know, trying to be as healthy as possible, just so there's no long term medical issues. And again, we're not talking about an A, 1c that was 12 or anything, but you know, with due time, like in a one season, the eights and nines, you're probably at higher risk. Less than someone who's running typically in the mid
Scott Benner 55:01
fives. Let's put it that way. So yeah, I'm gonna say definitely. So
Andrew 55:05
you know that was in my mind of like, okay, like, start embracing the technology and give it another shot. Why not? There's nothing to lose. And then I also look at it just solidarity is not the right word, but being able to show like, my daughter as she gets older, like you can have outstanding care and still do what you want to do, eat, what you want to eat, exercise as much as you want to exercise. You know, almost the role model thing comes into play. And just, you know, I want her to to see that it doesn't need to be restrictive in any way whatsoever. Yes, you're going to have the highs and you're going to be moody, you're going to have lows and feel very off and tired afterwards. But you know, outside of that, like it shouldn't restrict you in any way whatsoever. And I don't want her to grow up thinking that, you know, for some reason she can't do something because of fear that her sugar might be going high or low. So yeah, I'd say two things, really just the long term vision of making sure that I'm around as long as I possibly can be with no complications from it so I can, you know, continue to have fun with my kids. And,
Scott Benner 56:11
yeah, you know, your average a, 1c slightly over an eighth. Your average blood sugar is like 185 your average blood sugar now is probably more like 9092, something like there, like that, which is crazy. You cut in half. Yeah,
Andrew 56:24
yeah, absolutely crazy. And, you know, full transparency didn't really make too many changes to the diet. I mean,
Scott Benner 56:30
pre bolusing, stopping highs, if they happen, looking, looking, basically, I'm going to adopt you, Andrew. I'm pretty sure I'll send Arden to Gina. You mean, you're pre Boston your meals, and you're looking in again after you eat to make sure nothing's going crazy and and adjusting it if you do bingo, yeah, you got good settings, that's
Andrew 56:49
it, yeah? And then I changed my high alert. Personally, it's, it's 140 now, yeah,
Scott Benner 56:53
you said it was more like 200 before, right?
Andrew 56:56
Yeah, it's like 180 or 200 but still, like on the episode I listen to, you know, if it's if it's 180 I think it was you who said this, if it's 180 and you get those alerts like, why not at 140 when you can detect that it's starting to trend a little bit higher, you know, catching it 40 points lower than what it normally would trigger an alert for. I don't see there being much downside. So I did that. And then, you know, hopefully, at some point maybe, you know, we make that 131 20, the more episodes I listen to, and the more people I chat with that I've met. I don't know if that's the right word, but communicated with through the Facebook group like it is crazy how good some of these parents are with backtracking. I was sending Brooks auto logs when we couldn't figure out her Omnipod and she was running high. I was sending someone auto logs. She's not a medical professional. Never, never claimed to be, but her daughter's name was Kate, so hopefully, if she's listening, she understands the impact she had with us, finally understanding the Omnipod, but she could back math the auto events to figure out, you know, if her insulin sensitivity ratio needed to be tweaked, if her food to car or carb to insulin ratio at a specific time needed to be massaged a little bit. But it's fascinating like this, the group and the educational resources that are available through that
Scott Benner 58:11
so those beautiful diabetes dorks out there. Good job, Kate, that's awesome. Yeah,
Andrew 58:16
exactly. So it allows people like me to nerd out and, you know, try and try and get our daughter scare one step
Scott Benner 58:23
further. Yeah, I'm gonna say honestly, if Kate's listening, she should contact me. I'd have a conversation with her about that. That'd be awesome. I
Speaker 1 58:29
mean, it was amazing. I will tell you what he was showing me, and I was and then it was also kind of annoying, because nobody had ever told us to change her auto correct amounts, like it was set at point 05 and it's like, well, she's constantly getting these little bits of insulin. Why not just take her to point five?
Scott Benner 58:52
Yeah? Plus she's gaining weight and getting bigger, she goes right, like, that's probably happening all the time, changing her knees, yeah.
Andrew 58:58
Let me real quick. You know, I don't mean to interrupt you, but I just remember
Scott Benner 59:04
figure out if that's because you got married late and you're an adult when you got married, or if genius told you to apologize when she when you cut her off. But that's awesome when you do that every time. Yeah, yeah, also, and in fairness, Gina, you're like, nine months pregnant, so, yeah, you know what I mean? Like, I might pay for this in 30 minutes if I don't. No, no, no, you could get hit with a rolling pin or something. I don't know how it goes exactly in 2025 sorry,
Andrew 59:28
but when she because everyone raved about the Omnipod and when she got diagnosed, I wasn't even on board with the CGM because I wasn't wearing one yet. And again, the optics of that on a little three year old body, I'm like, I had a really hard time during diagnosis. I remember, I'm not a very anxious person. I have never had a panic attack, but that first night, when you know she's she's fighting us tooth and nail at 2am to check her blood sugar and crying, and you're their parent, like you should be a safety net, not this. Is this source of fear of what's going to happen. And I remember we checked Brooke's blood sugar, and it was like 92 and for the first time in days, I was like, hell yeah, she's finally in a normal range. And Gina said, that's fantastic. So we both kind of put our heads down and go to sleep, and I'm like, Wait, is that fantastic? She's had diabetes for three days. I have no idea how sensitive her body is to insulin, how much insulin is on board. Is she actually trending down rapidly? Because she'd be 50 in the next 30 minutes, and we're going to sleep through, you know, the mind starts racing. So in that moment, I realized we have no choice. We're going to have to get her on a CGM. And I said, but absolutely no to an insulin pump. The visual of that would just be a reminder, and I'm sure you're thinking a reminder of what I think it's really just just guilt of the hereditary.
Scott Benner 1:00:48
This is the part where I kind of want to finish up because, like, I've been waiting to ask you for a while, or do you feel are you? Do you feel shame? Do you feel guilty? Like, what's the feeling that comes with all this?
Andrew 1:00:59
I think ignorant would be the first word that, like, I just remember being stopped out of my my tracks and thinking that there was never really any kind of hereditary component. I thought when I got diagnosed it was a fluke, I swear, I think the doctor had said, like, it's probably from the combination of, yeah, I had, like, bronchitis, which turned into pneumonia, I want to say, but it was right after my grandpa had died, who I was close with, so they'd kind of served up like, you know, extreme sadness followed by an intense sickness might have attacked the beta cells and the pancreas, something that didn't make too much sense at the time. I still never heard that philosophy to this day, so who knows. But
Scott Benner 1:01:38
let me tell you this. I've heard people tell stories about having traumatic events and then having a diagnosis after but it's my expectation full well, like whether it's an illness or a traumatic event, that you did have markers for type one diabetes. It's not like somebody ran around the corner yelled boo and you got diabetes, right? Like you? Yeah, right. You may have had one to, you know, however many number of markers I'm going to tell you right now, with all that autoimmune on your side of the family, nothing about your diabetes or your daughter's diabetes surprises me, not at all. I talk to a lot of people like I could have bet 50 bucks on this one. You know what? I mean, it's not crazy at all, but, you know, fair enough. You get sick, you have a sadness, like, you know, like, that kind of stuff happens. You've got the markers already. Here you go. You have type one telling people that that doesn't mean that anybody else isn't going to get it. It's fair. Like, there's, it's still a relatively low, you know, percentage. Like, please don't hold me to this. I think, like, there's a one in, like, maybe, like, a certain percent chance for the regular population, and that chance goes up, but not even that significantly, if you have type, if your parent has type one. But I'm telling you, like, what are you Irish? German? Irish? Sure. Yeah, yeah, I could tell by all the celiac in your family there was Irish in you. Like, I mean, that's how many people I've spoken to like that doesn't surprise me at all.
Andrew 1:03:03
Yeah, that's crazy that there's, you know, you can tie it down at the Gina's
Scott Benner 1:03:07
Got nice dark hair. She might be the only thing holding this off. You know what? I mean, Gina, what are you Italian? Greek and Italian? Yeah, like, she might be helping a little bit. Who knows? But, you know, I mean, that's not a hard and fast rule or anything like that, obviously. But I speak to a ton of people and that part of the world, you see a little more autoimmune issues. And then, you know, come over here, and you know, that gets mixed your mom, your dad mix up there, and you know, there's a lot of autoimmune like, all that thyroid, all that celiac. I mean, it's coming Gina, what's what's the bathroom line look like after Thanksgiving dinner? Is it crazy?
Speaker 1 1:03:45
Well, you know, yeah, I mean, it's all gluten free at their house. So you
Scott Benner 1:03:49
ever said this out loud? Andrew, I've never heard more people talk about anything than your family. Have you ever heard that
Speaker 1 1:03:57
one? No, that's really funny.
Scott Benner 1:03:59
Andrew, you're not in therapy, right? No, I can tell, because you're telling, yeah, yeah, oh, don't worry, she's gonna keep encouraging you. Because when I asked if you were ashamed, you used a different word, but you are describing shame,
Andrew 1:04:11
yeah, I think I used guild that was going to be my, my second, you know, descriptor, yeah, you know, like, it's hard to not look at it that way, where, you know, and not just for Brooke's purpose, like I look at again, I keep coming back to the complexities of it, and just knowing the load that Gina was going to have to it landed on her plate, did nothing to deserve that. And I just thought through, you know, in that moment, I also think, like I realized, through the last 30 plus years of having it, like some of the struggles, the mood swings, just different events that had come up to realize, like, you know what? There have been some, some moments of heavy lifting with this, that that
Scott Benner 1:04:49
have sucked, yeah, oh, there's no doubt. Can I tell you something? My daughter's gonna be 21 in a couple of weeks. She's had diabetes and she was two. We're pretty good at this, right? Like, we're in a train. Transition period right now, Arden is getting older. She's doing things for herself. There's, you know, she's having her moments where she's figuring things out, and blood sugars are higher than they would be if, you know, if it was me doing it, but it's a transition period, and she still has an Arden still going to keep an A, 1c, in the sixes as a college student, taking care of herself like everybody's happy, don't get me, but there's still moments, you know what I mean, where, like, you say something, and she's, you know, being her own person, and not maybe being as, you know, quick to move on something, or taking something quite as seriously, or whatever it ends up being. And, you know, once in a while it comes up and you start talking about it. Well, my wife and I spent the day together yesterday. We were all over the place, going to different stores. We were just in the car a lot, and we were talking about it, I mean, and we've been at this now for, I mean, she's two, she's 21 minutes for 19 solid years, and we were both crying in the car by the time we got home, like, just trying to talk through how hard this is, you know, like I said to my wife last night. I'm like, I am so sorry. I was like, I would have never asked you out if I knew all this was gonna happen, but I felt like I did it to her just by asking her out. Like, you know what I mean? So I know how you feel. But also, if you ask my wife, she'd say there's a lot of autoimmune on her side of the family, so she feels guilty being dude, it's not your fault. Like you didn't you had no idea. And it's not like, you like, we're like, oh, Gina, let's have a baby. I'm going to try to make one with type one. Let me really concentrate here. Yeah, if it wasn't this, it would be something else, man. Like, everybody gets something, is the thing. I think I've, I think I've come to believe,
Speaker 1 1:06:33
I mean, with Andrew, like, there's never been one moment where I've been like, You caused this, yeah,
Scott Benner 1:06:39
but you feel like that though, Andrew, right?
Andrew 1:06:41
I do. And then, you know, also in conversation, when people make that comment, like, Oh, so you have it. And I'm thinking, correct, but we're talking about two different events here, right, right, exactly. And so,
Speaker 1 1:06:52
yeah, it's like, you always want to chime in and say, well, there. It doesn't mean that he has it, she was going to get it, or that Graham is going to get it. I mean, I will be very honest with you, though, I am terrified to figure out if Graham will have it or if our third will have it. And we did go down the path of T cell and doing the blood test. You know, in talking further with the endo team, Graham is two, so he can start the testing, but if he tests for two antibodies, there's nothing I can do for him, because he's not eligible for teas all yet. Not old enough. Yeah, I'd rather have ignorance right now. You know what I mean, like, just don't let me know anything yet. Yeah, that that thought is
Andrew 1:07:36
always lurking like Graham, I'll never forget this, like three weeks ago, started to have some pretty crazy outbursts. More More so than your, you know, traditional two year old boy, and he came up to me with three consecutive, like, yogurt, yogurts, whatever it is. And I'm thinking that's a lot of yogurt for a little body to be putting down. And he was still, he came with a fourth and was still freaking out, and, like, had a tantrum. And I'm thinking, oh no, you know there's, there's no way, and Gina wasn't home, and I thought, Hey buddy, I apologize in advance, but let me see your finger. And I finger poked him. And in that moment, like, again, I was like, everything from Brooks diagnosis came back to me, and I'm thinking, I, I don't know if we can go down this path again.
Scott Benner 1:08:19
Hey, listen, brush up on thyroid symptoms too, because, I mean, it's a fair bet with your family too. You know what I
Speaker 1 1:08:26
mean? Well, she did test for a marker for thyroid, but dead. Keep in
Scott Benner 1:08:31
mind, yep, going forward, that thyroid symptoms can come and your test results can still look quote, unquote, in range. So if you have thyroid symptoms and a TSH over 2.1 then it's time to start finding a forward thinking endocrinologist to manage your
Andrew 1:08:51
thyroid. Say that one more time. Those parameters thyroid
Scott Benner 1:08:55
symptoms, like, like, I don't know, Andrew, there's a ton of them, but off top my head like no matter how much you sleep, you can't get rested. Your hair is falling out. You're gaining weight for no reason. Your fingernails are brittle. You're having trouble regulating hot and cold. You're having mood swings that you can't explain, like those things and a TSH result over 2.1 if your TSH is like 3.5 and you go to the doctor and say, Hey, I'm having some thyroid symptoms, they see a 3.5 most doctors are going to say that's in range. It's not that, but interesting. I'm going to tell you right now. Go listen episode 413 and let that lady explain it to you. So, yeah, so keep an eye on that, especially with kids, it's hard to tell. I mean, I'm sure they're going to test her every time they do a blood test for thyroid. Moving forward, if they don't, they should be, yeah, they said that they are going to do it yearly, yeah. Well, every time they check her blood, I'd have her, have them do a thyroid also, just figure out where it is now, so that you can next time it goes, like, Did it go up? Did it go down? Like, is it swinging around? Crazy, anything. Mean that maybe draws your attention to it and for yourself too, Andrew, I mean, a lot of people on your side of the family also. I hate to say this, but because of the construction I told you about, we're gonna have to be done. I'm sorry, normally I'd go a little longer with you, but we, we stretched out a little bit, and I'm having a little bit of work done in my house. So it's about, it's about to get real Bangy in here. So I'll just let Rob leave the banging in. But let me let you finish. Is there anything that we didn't talk about that we should have, anything you feel like you left out?
Speaker 1 1:10:28
Not from, I mean, not from my perspective. No. I mean, I know that Andrew probably has a ton of questions about more diabetes and managing and things like that, so he'd probably love to email you.
Scott Benner 1:10:40
Don't email me. Andrew, no, I'm just kidding. You could come back on, or you can send me an email if you want, you know, like if you want to come back on sometime and talk, like, management stuff, we can absolutely do that
Andrew 1:10:49
too. Yeah, I look forward to that. I appreciate the time. And more than anything, we just appreciate the community and the people that have kind of become part of it, because that's that's helped us out, me too, in more ways than words can say. So we appreciate you. Man, no,
Scott Benner 1:11:01
I appreciate that you said that I spent the last week on a cruise ship with a bunch of listeners. Really, that's pretty cool. Yeah, we did a cruise. We just got back, about 100 of us on the cruise ship. It was awesome. Awesome enough we're gonna do it again next year. But,
Speaker 1 1:11:16
yeah, you've built a pretty incredible community. I will tell you that. Thank
Scott Benner 1:11:20
you. I appreciate it. But sitting there really getting to know people like that in person, over meals, over days, and then kind of coming together on Friday with Erica. Came on, Erica from, like, all my mental health stuff, and she came on the on the ship, virtually, and we almost ended up being like a group therapy session, and people were just baring their souls, sure, yeah. I'm telling you from like, parents of kids, parents of young kids, parents of teens, parents of adults, were there and up to I want to say that the oldest type one on the ship was 75 with us. Like, we had such an eclectic group of people, and they just went around the room and started talking, and every story was somehow really different and really same at the same at the same time, yeah, and I just watched one mother, and I'm gonna try to get her to come on. I won't say her details, but the entire week, I thought she was mad at me every time I because I did a lot of speaking, I get, like, three hours here, two hours there. Like, I was always looking out into the crowd. When you do public speaking, if you've never done it before, like, usually, like, if you're up on a stage, I just pick a friendly face on the left and a friendly face on the right, and I talk to those two people, and everyone in the crowd thinks you're looking at them. So you don't lose you know what I mean? You just find two people who think you're funny or engaging, and you just keep going back and forth. But when you're that close to each other, like in a more of a conference room setting, or, like, you know, sometimes it was like a little ballroom. One time we did it in this, like, little restaurant with, like, all this neat seating and everything. And you kind of can't do that because people are a little up on you more. So I kept avoiding this one woman because she looked mad at me. And it wasn't until the very last part of the very last thing that we did when she got the microphone to speak, and I realized she was just holding in a ton of sadness, oh yeah. And then she just let it out, and I watched her feel better for saying it. And then people gave her great advice. People hugged her. They came up to her, they supported her. It was awesome. Oh, I couldn't believe. Like, there are times like I'm going to take a minute after we're done here, and I'm going to think about what you guys said, and I'm going to feel overwhelmed and lucky that I pulled this whole thing together. Then that happens to me a lot, making the podcast and seeing people online, but being in the room, yeah, oh my god. Like I was, everyone was crying. It was, you know, just cathartic and lovely. So anyway, it was, it was awesome.
Speaker 1 1:13:47
Well, you've been tremendously helpful to us. So I mean, there's hundreds of 1000s of people out there that you don't even get to talk to every day, that are communicating back and forth with each other via your
Scott Benner 1:13:59
platform. I have a hard time wrapping my head around it most days, but, yeah, it's pretty amazing. This helped. Like, standing in front of people, I not that I haven't done it at like, I'll go do talks, but they, they last a few hours. So not that they're not people when you get there, but you're so rushed that everybody's just, like, an what are the kids call that the characters that walk through your video game? Like, you know what I mean? Like, you know, I mean, like, there's just a bunch of people there, but you can't really focus on many of them. Get to talk to some of them. But this i i made very certain I ate dinner with every person over the six days where we were there. Very awesome everyone. And it was, it was just a really wonderful experience. So I appreciate all the people that came and all your kind words. Thank you very much.
Speaker 1 1:14:42
Well, we've really been looking forward to this. This is a big fan girl moment for us. So Thanks, Scott. I didn't
Scott Benner 1:14:48
know Andrew was fan growing, but that's awesome.
Andrew 1:14:50
Oh yeah, oh yeah. He's like,
Speaker 1 1:14:53
your number one fan girl. He's like, so Scott said this, and bold beginnings, and Gina, watch this. And yeah, it's
Andrew 1:14:59
like, when. You and Jenny on an episode once. I'll let you go after this. But she had said, You're joking around like your husband probably is wondering who Scott is, and I'm sitting there at dinner that night, like, and then Scott said this. Scott said that I'm like, I bet Gina is sitting here wondering, like, who's Scott again, and why are you spending so much time with us?
Scott Benner 1:15:13
Six more weeks, Gina is going to be like, if Scott can't breastfeed this baby, I don't want to hear about it. Yeah, we appreciate it. Of course. I wish you a ton of success with the upcoming birth and congratulations again. It's really exciting. I don't imagine you're gonna name the baby, Scott, but if you do, please let me know. Never, never. Say Never. Thanks, Scott. Hold on one second for me. Guys, you're very welcome. Hold on one second.
Having an easy to use, an accurate blood glucose meter is just one click away. Contour, next.com/juicebox That's right. Today's episode is sponsored by the contour next gen blood glucose meter. The episode you just enjoyed was sponsored by the twist a ID system powered by tide pool. If you want a commercially available insulin pump with twist loop that offers unmatched personalization and precision for peace of mind, you want twist, twist.com/juicebox, thanks for tuning in today, and thanks to Medtronic diabetes for sponsoring this episode, we've been talking about Medtronic mini med 780 G system today, an automated insulin delivery system that helps make diabetes management easier day and night, whether it's their meal detection technology or the Medtronic extended infusion set, it all comes together to simplify life with diabetes. Go find out more at my link, Medtronic diabetes.com/juicebox you thank you so much for listening. I'll be back very soon with another episode of The Juicebox podcast. If you're not already subscribed or following the podcast in your favorite audio app, like Spotify or Apple podcasts, please do that now. Seriously, just to hit follow or subscribe will really help the show. If you go a little further in Apple podcasts and set it up so that it downloads all new episodes, I'll be your best friend, and if you leave a five star review, ooh, I'll probably send you a Christmas card. Would you like a Christmas card if you're looking for community around type one diabetes, check out the Juicebox podcast. Private, Facebook group, Juicebox podcast, type one diabetes. But everybody is welcome type one type two gestational loved ones. It doesn't matter to me, if you're impacted by diabetes and you're looking for support, comfort or community, check out Juicebox podcast type one diabetes on Facebook. Hey, what's up everybody? If you've noticed that the podcast sounds better and you're thinking like, how does that happen? What you're hearing is Rob at wrong way. Recording, doing his magic to these files. So if you want him to do his magic to you, wrong way. Recording.com, you got a podcast. You want somebody to edit it. You want rob you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1583 Kaiser Rolled
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
‘Clara,’ a 45-year-old nurse with LADA, shares her fight for a proper diagnosis after bad info from Kaiser—and how growing up with a T1D sister shaped her journey.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Welcome back, friends. You are listening to the Juicebox podcast.
Speaker 1 0:13
Hi, I'd like to remain anonymous, but we can pick a name, Sue Clara.
Scott Benner 0:21
My grand rounds series was designed by listeners to tell doctors what they need, and it also helps you to understand what to ask for. There's a mental wellness series that addresses the emotional side of diabetes and practical ways to stay balanced. And when we talk about GLP medications, well we'll break down what they are, how they may help you, and if they fit into your diabetes management plan. What do these three things have in common? They're all available at Juicebox podcast.com, up in the menu. I know it can be hard to find these things in a podcast app, so we've collected them all for you at Juicebox podcast.com. Nothing you hear on the Juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. When you place your first order for ag one, next gen, with my link, you'll also get a free bottle of Ag, d3, k2, a welcome kit and five of the upgraded travel packs. And right now, with every new subscription, you'll get a freaks of nature Sun stick. That's an SPF, 50 Sun stick. With your order, use my link. Drink, AG, one.com/juicebox, summertime is right around the corner, and Omnipod five is the only tube free automated insulin delivery system in the United States, because it's tube free, it's also waterproof, and it goes wherever you go. Learn more at my link, omnipod.com/juicebox That's right. Omnipod is sponsoring this episode of the podcast, and at my link, you can get a free starter kit. Terms and Conditions apply. Eligibility may vary. Full terms and conditions can be found at omnipod.com/juicebox
Unknown Speaker 2:01
you this episode
Scott Benner 2:03
of The Juicebox podcast is sponsored by us. Med, us. Med.com/juice, box, or call 888-721-1514, get your supplies the same way we do from us. Med, Hi, I'd like to remain anonymous, but we can pick a name to Clara. Clara, hey, Clara, how are you I'm good. Scott, how are you doing good? Do you think you'll remember to like respond to that if I call you Clara, hopefully we're gonna find out. It says, By the way, it's whimsical and sweet with an old soul charm. Does that fit you at all? Absolutely awesome. Like, you're like, I'm not gonna say, if it doesn't, that's not really me. I'm kind of a horror. Claire, what do you do for a living? I'm a nurse, okay? And you have type one diabetes yourself. I do. I have Lada about how long ago were you diagnosed?
Speaker 1 2:59
In 2022 is when my first a 1c, was high.
Scott Benner 3:03
Okay, how old are you now? 45 Okay, tell me why we're not using your real name,
Speaker 1 3:09
because I'm a nurse at a hospital, and some of the things I'm going to talk about are kind of closely related to that hospital, and I don't want to get in trouble at work. Okay,
Scott Benner 3:19
did I bring you on to do like a cold drink? No, you just, this is just the vibe of your story. You know it?
Speaker 1 3:26
Yeah, there's just a few things that I just don't want to be traceable to me. I
Scott Benner 3:32
understand, at least where you can go. No, that I I'm listening to it too, but it doesn't sound like me, sorry.
Speaker 1 3:37
Sounds like Clara. She works in a different unit. I'm
Scott Benner 3:41
hearing Clara, and my name is different than that, so that's definitely not me. I got you Okay, well, we will do that for sure. How long have you been a nurse? About 13 years. 13 years. So is it fair to say that you saw your diabetes coming?
Speaker 1 3:56
Kind of, yeah, it was. So the first time it kind of showed up was in 2015 when I was pregnant, and they screened me for gestational diabetes, and I failed that one hour glucose challenge horribly. And I remember the doctor telling me, You're going to have gestational diabetes, and I was so mad at her. I was like, How dare you say this? Like you don't know, but at the same time, I knew, so we didn't talk about yet. But my sister has type one diabetes since she was four. She's two years older than me, so I grew up with type one being everywhere in my life. But that was a long time ago, and in listening to podcasts, you know, you talk about how the management was different in the 80s and 90s. It was a little bit less your face, you know, like there wasn't CGM, sir. It was like, give a shot, check a blood sugar. Give a shot, check a blood sugar. So
Scott Benner 4:55
yeah, and not think about it really, in between, unless you got dizzy or sweaty, right?
Speaker 1 4:59
Yeah. Like it definitely it's like, a weird presence in my life, but at the same time, like, I don't feel like it impacted our lives that much. I like, I look back on it and think, Gosh, my mom really, I have a lot of respect for my mom. Handled
Scott Benner 5:15
it. Do you think she handled it well, or do you think she just didn't know the depth of the issue because of the
Speaker 1 5:21
time, you know, I don't, you know, I don't know. And I my sister and I have talked a lot recently about it, and I know my sister has some gripes about my mom's kind of lack of involvement, like later in her teen years, and, like, her early 20s, I think she did the best with what she could. She definitely wasn't negligent. But, you know, the tools were just kind of what they were it was definitely something we thought about. I remember, you know, we had very healthy dinner, very well rounded, always a protein, a vegetable, you know, like she took care of all that we didn't, you know, my sister ate really well. I mean, a lot of it was kind of diet, like, focused in terms of that. Like, I jokingly tell people a lot, like, when I was a teenager, one of my big rebellions was I ordered a regular soda at a restaurant, and I remember you people, yeah, yeah. And my mom looked at me, and I was like, Yeah, that's right, Pepsi. And she was like, it's happening, yeah, yeah. And she didn't say anything. I also remember as a child knowing that my sister was diagnosed by it, she had to pee and drank a lot, and one day, I decided to see if my mom would notice if I drank a lot and peed a lot, and she didn't notice at all. But I think she probably knew what I was doing. So really, I don't know,
Scott Benner 6:33
without speaking for her broadly, what is your sister's gripe with your mom?
Speaker 1 6:37
She sort of, I have sort of the same gripe with my mom that, like, as we got a little older, she really kind of checked out a
Scott Benner 6:43
little bit, like, don't get pregnant, see ya. Yeah. I mean, she was a really
Speaker 1 6:47
great mom. Like, I That is my feeling. My mom was a great mom, but, like, we got to be later, teenagers and 18, and she was like, I'm done. I did my job. Oh and shit. It's not like she it's not like she wouldn't be there for us, but she was not, like, let me keep day to day. Yeah. I mean, it's also, I have an interesting perspective too, because I grew up with type one so close around me, but I know how, like, it doesn't affect you, unless it affects you, because, like, I was around it, but like, even with it being in my house, around me, I knew very little about what was going on and was sort of not affected. So, like, now, as an adult, having it happen to me, I'm like, I know that people just don't really care, like, what's happening to me, because
Scott Benner 7:31
in my experience, that this does not put up a lot of red flags for people. Did you not feel ignored because your sister got more attention or anything?
Speaker 1 7:39
No, I didn't. Okay. My sister had this challenge and that I didn't like, there was definitely like it was kind of swirling in the background that,
Scott Benner 7:48
like, did you feel like your mom favored one of you over the other? No,
Speaker 1 7:52
she didn't. I do feel like it was even I knew that she put a lot of effort into that with my sister, yeah, but I didn't feel neglected. No, it never occurred to me that I could get type one like. It just kind of never, no
Scott Benner 8:09
one ever looked at you funny or tested your blood sugar once when you were younger, or anything like that.
Speaker 1 8:14
Well, I mean, I guess when I was younger, I think I felt like I made it, you know, like I got like, I didn't get it like, so also, one of the other things my parents did offer to, like, do some kind of screening. I don't remember what, back when I was, like, 18, and I said, No, I don't want to be screened. If it happens, it happens, and I don't want to know, but I think at that time, there was nothing they would have been able to do, like, there was no treatment. It would have just been like, yeah, I guess at 18, you know, I'm also 18, and maybe not making the best decisions. So, like a lot of times, I hope nobody takes this wrong way. When I see people, you know, saying they ask their kids if they want to be screened, I think, oh, gosh, I don't know that they can really make that decision. Yeah? Because even at 18, I was like, No, I don't want to know. Yeah, I die this way. Fine. I want to eat. So I want to eat, what I want to eat, you know, like, which I don't feel like now, you know, like,
Scott Benner 9:04
let me say this to you. I used to say on the podcast a lot. I must have said it so many times. I just, I consciously don't say it anymore. But I don't know, a lot of decisions I would let a 10 year old, a 12 year old, an 18 year old, make that was around health, yeah. Like, what a weird thing. Like, you know, what do you think? Well, Mom, I'm 11, but let me tell you what I think. Like, yeah, you know, like, there's a big push at one point in the diabetes community that I don't see as much anymore, which is, like, you know, it's body autonomy. Like, well, they don't want to wear a CGM. They don't have to because their body and I'm like, okay, except she's six, and, like, you know what I mean? Like, yeah, she doesn't know. The other side of all this, like, a six year old is not making a full decision when you ask them if they want to wear a CGM. Like, of course, they don't. They don't want to do that. Like, yeah, you know, an 18 year old, do you want to be screened for type one diabetes? No, no, thanks. I'm good,
Speaker 1 9:54
yeah. I'm invincible, you know. Like, I don't want to know. Like, it's not going to happen to me, Mom,
Scott Benner 9:58
listen, I don't know if you. Otherwise, just not. But a speed ball didn't kill me last weekend, so I don't think diabetes is going to Okay. You even know what that is. Of course, I know what that is, all right, just checking you, if you're just agreeing to something, you're like, Oh, that sounded fun.
Speaker 1 10:13
I have not, but I do know what that is, yeah, but yeah. But when that's your
Scott Benner 10:17
feeling like, oh, this won't hurt me. Like, I don't have to use a condom, I don't need to do this. I don't need to do like, what do like, What do you mean? Like, don't talk to the guy who's driving the motorcycle. I can talk to him like, you know, you don't. None of that, you know, they
Speaker 1 10:29
didn't. There wasn't to put us a mat back then. Like, there wasn't any treatment. I don't think so. Like, in that space, like, I would have just known, but still, I think there would have been merit to, like, knowing
Scott Benner 10:42
somebody would have checked your blood sugar once in a while. Probably, yeah,
Speaker 1 10:46
and that leads me kind of interestingly to what I wrote you about, like, was, you know, kind of my struggle with my healthcare team that I had last year was with Kaiser, but I don't think it's like, exclusive to Kaiser. So she tested me for my a 1c she just threw an A 1c and I was doing other labs. She's just like, she said, I'm gonna throw an A 1c in. I get the results back at 6.2 and I was like, Oh my God. Like, I'm freaking out. Yeah. And then I wait a couple days, she never says anything to me. I email her back and say, hey, you know what about this a 1c and she emails me back, an A, 1c is a measure of blood glucose over a three month period. I'm like, Yeah, thanks, but I know that. Like, what about it? Like, what? She was like, Yeah, well, you know
Scott Benner 11:33
you should, don't know, were you just trying to make money running my a, 1c what's going on right now? Yeah. And
Speaker 1 11:38
I was like, it pissed me off so much because I was, like, you threw this lab in, and now it's abnormal, and now you're not responding for like, a week about it. And like, I guess to them, it's like, you know, it's not urgent, but like, you know, to me, it is right. And so I'm like, so you know, what's the plan like? I know there's not, like, going to be a huge plan, but I just, I don't know. I'm a nurse. Like, tell me what the plan is like. And she's like, I don't know. Here's a link to some how to eat healthy and how to exercise. And I'm like, okay, like, How often would you check your a 1c she's like, well, we can't do it any more often than three months. I'm like, I'm not asking, like, how the lab works. I'm saying, What is your plan as a doctor? And they're just like, I don't she was just literally like, I don't know, I guess we would check it in a year. And I'm like, I don't know. There was just something in me that knew that that was not a good plan.
Scott Benner 12:28
Is this person still your doctor? No, no, okay, yeah, no. It's awesome. Like, oh, I ran this test and I got back, I got back something actionable, but we're not going to do anything with
Speaker 1 12:38
it. Yeah, it really made me mad. And so I said, you know, I think I'd like to see Endo, because, you know, my sister's type one and I have a history of gestational diabetes, and I'm real. I'd really like to, like, be proactive about this.
Scott Benner 12:51
So worried about what you're gonna say right now, I just have this. I just have to be honest with you, like, once you tell me I'm 6.2 and my my sister has type one diabetes, this should shift this doctor. But what happened? I used to hate ordering my daughter's diabetes supplies. I never had a good experience, and it was frustrating. But it hasn't been that way for a while, actually, for about three years now, because that's how long we've been using us Med, us, med.com/juicebox, or call 888-721-1514, US med is the number one distributor for FreeStyle Libre systems nationwide. They are the number one specialty distributor for Omnipod dash, the number one fastest growing tandem distributor nationwide, the number one rated distributor in Dexcom customer satisfaction surveys. They have served over 1 million people with diabetes since 1996 and they always provide 90 days worth of supplies and fast and free shipping us med carries everything from insulin pumps and diabetes testing supplies to the latest CGM like the libre three and Dexcom g7 they accept Medicare nationwide and over 800 private insurers find out why us med has an A plus rating with a better business bureau at us med.com/juicebox, or just call them at 888-721-1514, you get started right now, and you'll be getting your supplies the same way we do. Today's episode is brought to you by Omnipod. It might sound crazy to say, but Summertime is right around the corner. That means more swimming, sports activities, vacations, and you know what's a great feeling, being able to stay connected to automated insulin delivery while doing it all. Omnipod five is the only tube free automated insulin delivery system in the US, and because it's tube free and waterproof, it goes everywhere you do, in the pool, in the ocean or on the soccer field, unlike traditional insulin pumps. You never have to disconnect from Omnipod five for daily activities, which means you never have to take a break from automated insulin delivery ready to go tube free. Request your free Omnipod five Starter Kit today at omnipod.com/juicebox Terms and Conditions apply. Eligibility may vary. Full terms and conditions can be found at omnipod.com/juicebox type that link into your browser, or go to Juicebox podcast.com and click on the image of Omnipod right at the bottom. There's also a link right in the show notes of your podcast player. This
Speaker 1 15:33
doctor did not care at all. This doctor was like, Endo. She said, No, this is actually what she did, which really pissed me off. She said, Well, what would you like to talk to endo about so that I can prepare them for your questions? And I was kind of like, that's weird, but I sent an email, just a brief email, like, I have this question, I have this question, I have this question. And what she did was she just forwarded them that email, and they forwarded her response back, so I never got to talk to Endo. They just talk to each other.
Scott Benner 16:01
You know, it's not even the Endo, you know, it's somebody just answering the email. Okay,
Speaker 1 16:05
fast forward, I did end up meeting this Endo, like two years later, and even if I had gotten to this Endo, it wouldn't have helped me. So, oh, anyway, but so
Scott Benner 16:16
say birds the feather flock together. Situation,
Speaker 1 16:19
I they just for anyway, I don't know, they
Scott Benner 16:23
look at you. You won't say anything mean, because you work in the industry. But these are two people that don't, they don't do a good job. Is that, right? Yeah.
Speaker 1 16:30
They were just very, like, lazy about it, and just, like, minimum, just bare minimum. They were like, oh yeah. Just it was, it felt very much like, oh, just another pre diabetic person, which I guess, like, that's how they felt, for all their laziness, they would kind of do what I say, like, as a nurse, I am like, used to being like, not that they listen to me, but I'm used to being like, this is, this is what I want like, okay? And they're like, they either say yes or no. So she said, Well, I'll put a standing order in for an A, 1c every three months, because that was the most you could do it, you know. So I ended up doing a one sees every three months, and they just started. So the first time, it was 6.2 the first time, then I, like, had, like, an extreme diet, like, I was, like, in my mind, I was like, I'm gonna reverse this thing. This is when I didn't have any idea about type, but it could be type one or stages of type one. So I thought, you know, people reverse this. So I, like, was super, super dedicated to this. And then my a 1c after three months was 6.0 and I knew that that was not good. I was like,
Scott Benner 17:30
Oh, but I only ate one piece of chicken for the last three months. Yeah, yeah.
Speaker 1 17:34
I was like, that's, that's a bad sign. Like, if it had gone to like, 5.2 I probably would have been like, I get it, yeah? Like, I reversed this, and I put, you know, whatever. But I was like, oh, man, that barely moved. Not good, yeah. I talked to so I started talking to my sister a lot. She's been so supportive, and she's so patient with me. She just very gently prompted me to ask for the antibody labs, you know, like, yeah, it's hard to tell someone what to do with their health and their doctors, you know. And she never felt like she was forcing me or telling me what to do. She just kind of prompted me along. So I asked for antibody test. She asked the Endo. The endo told her how to do that. I could tell via like, their email messages. And the email message from the endo was like, you can do a gad antibody test, and if it's negative, then she's not Lada. Like, basically just like, you can do that. So she's not, like, you can
Scott Benner 18:31
tell her. Everybody thinks you're not gonna have Lada. That's what they're Yeah,
Speaker 1 18:35
yeah. And this was, like, the first of a long list of, like, came back positive. And I was like, Yeah, told you. But then it's like, Damn, that's actually not good. Like, I won, but like, I really,
Scott Benner 18:48
yeah, I told you guys you weren't paying enough. Oh, I have diabetes,
Speaker 1 18:52
yeah. But then the really screwed up thing is that even once they got that result, they didn't care about it at all. And they were just like, okay, yes, you're Latta anyway. So continue on with monitoring your diet and exercise. And I was like, okay, and I would I was trying, like, this is the other part I feel strongly about. It's like I was trying my hardest to advocate for myself. I was doing all this research. I'm reading, I'm looking things up. I'm like, trying to educate myself, and I'm, like, getting nowhere with them, and I'm getting nowhere with anything. I'm a nurse, my sister's type one, she's helping me. I asked for this test. I got it, like, and still it was just kind of nothing, which, at that point, I guess, like, it's hard, because with Lada, it's it is this, like, weird waiting game where you're like, kind of in between, can I tell you how
Scott Benner 19:43
insulting I find the idea of advocating for yourself? Yeah, listen, I think you should. And I would tell anybody listening, you have to, and I would explain why, but you should not have to go to a doctor and beg them to do their job, because that's. What advocating means. It means keep talking till someone breaks down and does the thing you need.
Speaker 1 20:07
Yeah, I think the other part is like, I was so used to having nothing wrong, which part of me feels extremely like privileged to, like, say, like, Sure, this hit me really hard because I hadn't really dealt with anything. So I recognize that, and that feels like my sister and I have talked about this a lot too, like I just can't even imagine as a kid, like when she went through and I and like I was there and I didn't understand it. You know what I
Scott Benner 20:31
mean? You carrying guilt on that? Have you heard the news? AG, ones next gen is now one of the most clinically backed greens powders. They went above and beyond industry standards and testing, and have made a great product even better. Plus, right now, with your first subscription, you can get this awesome sunscreen stick for free, co founded by pro surfer Kelly Slater, the freaks of nature. Sun stick is exactly what you're looking for. It's extremely water and sweat resistant, and it doesn't leave white streaks everywhere or get in your eyes like those other sunscreen brands take care of your body on the inside and out with ag one plus the sun stick bundle, only available for a limited time. Head to my link. Ag one.com/juicebox, to get $100 of free gifts, including five free travel packs, a free shaker bottle, the freaks of nature Sun stick and more with your first subscription. And that shaker bottle is perfect for the summertime. It's a great size. You can pack it in your bag. You don't want things spilling everywhere, right? And it's TSA approved. So this is perfect for your summer vacation. I just received my freaks of nature Sun stick. It's SPF 50, and it arrived just in time for a little trip that I'm taking with my family. Yeah,
Speaker 1 21:43
and, like, we actually had a really nice conversation a lot of times about like that, I said that to her, and she said, I feel so bad. I wish this had never happened to you. Like, I always wish this never happened to you. And and I feel bad that it has, and I don't even know how she could feel bad about it, you know,
Scott Benner 21:58
yeah, because she had it first, and it feels like it's her thing, and so now you have her thing, and she doesn't want you to feel the way she want to share it with me, yeah, yeah, even though that's unreasonable, big picture. But I understand, yeah, yeah.
Speaker 1 22:10
And I think she wouldn't, you know, obviously she doesn't think she's responsible for it. It's just I felt guilty that I I hadn't, like, checked in on her and, like, it was a weird feeling of like, wow, I really never, like, asked you about this, like, I always just thought you had this under control, and that was a thing that you had under control. And, like, I never checked in on you, and I never was like, how is this going? And in a way, I like that, like, that's not how I think of her, even though I know she has diabetes. Like, it's not like my sister with diabetes. Like, number one thing, you know what I mean, it's not the number one thing that I think about with her. I see
Scott Benner 22:46
both sides of it. Like, on one hand, you're happy not to look at her and just think diabetes, and on the other hand, you're like, God, I didn't realize this is what you were going through. Or I yeah, I would have said something or, you know, because obviously this is a thing that needs support. Yeah,
Speaker 1 23:01
it's interesting. Like, this is like, a weird little segue, like, I work at a children's hospital, and there is a lot of thought about kids who are chronically ill or severely ill, especially in the hospital, and their siblings, and what does that do for their siblings? You know, you asked me early on about, like, did I feel ignored or something? I think it's interesting, like, kids are so adaptable. And I just want to say, like, to parents of kids with type one, I think you're raising kids that are, like, really empathic. My sister was so empathic and so helpful to me, and I think her having that growing up really does affect kids, and I don't think it always affects kids in a bad way. I think it can really make them thoughtful. And, yeah, I mean, it can have different effects. But, you know, like, I just now I'm even so, like, thankful, and I'm impressed of how my sister really helped me through this, and she's been really, you know, even as adults. But like, I think that that's something she's acutely aware of, like, growing up with a chronic disease like that, I feel like I wasn't and, like, was kind of blind about,
Scott Benner 24:07
have you tried going back and explaining this to your parents or no, or is it too late? Are they older?
Speaker 1 24:14
I mean, they are older. I've talked to them. We've talked about it a lot, and I know even, like, before this was happening to me, I talked to my mom about when I when I had a four year old, when I had my four year old, I thought, the thought occurred to me a few times of I have no idea how my mom, I can't even get my kid to sit down in a chair. And how was she giving my sister shots like and checking her blood sugar like, as a parent, seems really hard. I
Scott Benner 24:41
got a regular kid over here with no stuff, and I'm banging my head against the wall here, and your mom had going on what she had going on with your sister. How does that happen? And then how do you regulate that later as an adult, when you think like, oh, I don't think my mom did enough. It's a weird little conundrum. To work your way through.
Speaker 1 25:00
Yeah, yeah. It's hard being a parent's hard. And anyway, go ahead,
Scott Benner 25:05
yeah. I was gonna say, what's the answer? Is the answer, your mom could have done more and she should have, or is the answer that those were the times, and that's all it was. Is that an excuse for not looking harder into it like and if you answer that way, are you telling me that you don't try hard enough with your kid, and that's why nobody answers that way. It's all very weird, you
Speaker 1 25:23
know what? I mean? Yeah, yeah. I think my sister's main complaint was, like, later as a teenager, and I do remember, like, her coming back from college and being like, I haven't checked my blood sugar in months, you know? And like, she definitely had some kind of of that typical late teen, early adult kind of burnout,
Scott Benner 25:41
like, I don't want to, I'll just leave that behind. Thing, do you know, if she was taking her insulin? Yeah, she was
Speaker 1 25:47
taking insulin. But I think she just was like, I feel this, you know, I feel high. I feel think she was going by, feels which, you know, yeah, wasn't, wasn't the best way. But I, you know, and she recognizes that now, and she's doing, been doing really great for a long time.
Scott Benner 26:05
That's awesome. Did she have trouble at that point? Like, is, is the question, like, How did my a 1c go up and nobody said anything to me?
Speaker 1 26:11
I don't think so. I think, I think she knew. And, you know, we've never really talked about specific a 1c is, I haven't, like, asked her, like, we talk currently about agencies, but I don't want to be like, what was your highest a, 1c Tell me about that dark place in your life. Like I was just
Scott Benner 26:27
wondering if maybe there was, like, something visible that your mom saw that she just, like, kind of turned a blind eye to. That's what I was wondering.
Speaker 1 26:35
My sister says, like she stopped making endo appointments for her and that she hadn't been to the endo in a really long time, and at some point, as a teenager, realized she had to make an endo visit for herself. And
Scott Benner 26:45
interesting, your mom get a little drinky when she got over, what happened?
Speaker 1 26:48
Like, I said, she kind of was like, I'm I'm done with you guys. Like, cancer done. And for me, I've had the same feeling about, like, some different stuff. I remember, like, similarly, like, being like, I haven't been to the dentist in a while. Like, I guess I should make my own dentist appointment. I was in high school, you know, and thinking, is this, is this normal? Like, should I, I mean, maybe I should I guess I can. Like, oh, it's like, I guess I will. And then for me, for most of my life, I've kind of looked back on that and reflected that, like, I don't know that it was intentional, but it did make me very independent. It was okay for me, but I wasn't managing a chronic disease, so it's different a
Scott Benner 27:25
little bit. I have a family that pops into my mind now, and they're lovely people, and I actually absolutely adore them. However, if you ask them about their responsibility for their children, it is place to live, healthcare, food till you're 18, and then good luck. Yeah, that's what they think. And I don't know if that's generational or, like, familial, like, maybe that's just how your mom was raised, and she's just gonna raise you the way she she was raised. Like, who knows. But it is weird, once the medical thing gets involved, that to just drop the ball, like, so, so much like, like, you're not dropping a ball. You're dropping like a lead weight. You're like, oh, you know, how did your mom never once think, Oh, my God, my daughter hasn't been to the end, though, right? That's a strange one to me. I'm so sorry. Do you think she had some sort of a little breakdown, or anything like that happen? No, no, wow. You think she's like, Ed, what are you trying to tell
Speaker 1 28:19
No, I don't, I don't, I really don't I my mom did a lot for us. We had a really nice childhood. So it's not that she was, like neglectful in general. I think she's human. She just saw this at the end of her responsibility was here. And maybe she doesn't necessarily do those things for herself either. You know what I mean, like, oh, like, I think it's just kind
Scott Benner 28:43
of, oh yeah. The state says I gotta take care of this kid, but now it's older, so like, No,
Speaker 1 28:48
I just think maybe she's not as on top of dentist appointments as, like, she should be, or, you know, or doctor's appointments. Like, I just think maybe that's not
Scott Benner 28:56
her focus. Is it like, possible that your mom didn't see the diabetes as all that intricate and important, because it was so there were no CGM that she was made. Your sister was probably just doing, like, regular name page at some point, right?
Speaker 1 29:11
Yeah, she was doing regular and mph. But, you know, I will say to get my mom critics. I'm really not trying to No, yeah, when my sister was diagnosed, at that time, they were doing pork, beef or pork insulin in our area, and she took my sister to the big city, hours away, found pediatric endocrinologist, demanded to use human insulin like she really advocated for my sister, and she also really advocated for my sister in school.
Scott Benner 29:37
I take your point. No, I don't think she was like, negligent or anything like that. It's how the whole thing occurred to her so
Speaker 1 29:44
but I do think it back then there was this sort of like I hear on the podcast, at least watch, and it kind of resonates with my experience as a kid that there was like, this is your disease, and you take responsibility. Like there was this handing off of versus. Responsibility that was sort of considered the what was supposed to be done, I think, yeah, in the 80s and 90s.
Scott Benner 30:05
Yeah, that was the end of it. Like we did our part. Now you do your part. You need to learn to manage. Yeah, this is your thing, and you're gonna have to do this your whole life. Isn't it funny that there's no like extension to that? So let me help you get set up, or give any questions or anything like that. It's just very, I mean, of that time, I guess, yeah, yeah, oh, geez. So, okay, so you're sorry, you're diagnosed. Yeah, let's get back to you. Yeah, vaccinated. God, you're diagnosed. It's lot of so is the onset very slow for you? How long does it take for you to get to the point where you are now? Or maybe you're not even there yet?
Speaker 1 30:40
Yeah, it was pretty slow until so like, the turning point for me, although I still, like, I still am not, like, fully insulin dependent. I use insulin to, like, optimize my a, 1c and like, optimize my blood sugar. But, like, my blood sugar grows up really high, but then it does come back down eventually, but it started to change. Was like, I think in beginning of 2024 I think it went over seven and even, and this is another point, like, I really, or I think when I was 6.5 maybe towards the end of 2023 the doctor was like, Well, you could start Metformin, but you don't have to. It's up to you. And I was like, Well, what, what should I do? Like, I was like, What should I do at this point, I was really not as engaged, like, it's hard for me to even think back on like, how I was thinking about it back then, like, I was just not as engaged with it, like I knew it was happening. I was aware it wasn't but it wasn't like, on my mind so daily. And she was like, Well, you know, Metformin has its side effects too, so, you know. And I was like, okay, I can, I think I can do this, like I haven't been perfect, like I haven't been absolutely perfect. I can be more perfect. So this was sort of my struggle, from, like my initial diagnosis in 2022 till, like, last fall, 2024 was I just, even though I knew it was autoimmune, even though I knew it was like, not my fault, I still was, like, struggling so hard to be perfect and like, going on Metformin, really felt like a failure. The whole thing felt like a failure, even when I had just facial diabetes. Gestational diabetes, I felt like a failure, yeah, and I thought I could be perfect. And when I was pregnant, I was not starving myself, but I was so intent on not going on insulin. I was like, I will not go on insulin. I only gained like, 12 pounds my pregnancy, and they were like, You need to gain weight. And I was like, you put me on a diet. Well, what? What do you mean? Like,
Scott Benner 32:47
why am I supposed? Why do you think? Like, why do you think that that's the response? Because you're, I mean, listen, just tell me a few years ago, you're, you're a full grown lady with, like, you know, kids of your own, everything like that. Like, what is that like, psychological pushback that you're having.
Speaker 1 33:03
I think, like, I feel it's strongly that, like, my my emotional response to it is like more than it should be like when it was first, when I was first got this diagnosis, I was like, and I still get really emotional talking about it. And like, as I get so emotional talking about it, I think, God, God. Like, why are you so emotional talking about this? Or think, you know, like, why does this? Like, other people have things happen and they just deal with it, like, what is your I think part of it must be, like, some kind of childhood psychology situation of like that. I didn't have anything wrong with me and like, Now something's wrong, I don't want there to be anything wrong. Yeah. Like, and I had this super strong desire to, like, fix it, stop it, you know, like, yeah, which I think most people obviously do. Like, you know, when something's wrong, you want to fix it, sure. I know because, like, my how emotional it's made me that, like, there's something under there. That's,
Scott Benner 34:00
can you not find it? Can you describe the emotion
Speaker 1 34:05
like it for a long time, I just couldn't even talk about it without crying, like I was just crying for because you were angry or hopeless or like it was just grief, like I felt a lot of grief around it. That's fair, you know. But yeah, and I and it kind of like was, like, that's okay. You can feel grief, but it like went on and on. And so even with Kaiser, I think, in 2024 so in 2024 my blood sugar started to go up. And when they gave me Metformin, and I didn't end up going on it, they the instructions were to check my blood sugar twice a week and make sure at the end of the day and make sure my blood sugar was going down below certain parameters, and it was and I wasn't checking my blood sugar more often. I know I definitely, like, I knew what the a one sees meant, but like, I I don't know. I didn't want to check my blood sugar and see it be high. So I was just doing what they told me, taking my meds, checking my a, 1c every three months. But then at some point in the late summer, I noticed my. Sugars were higher. Like, I would check it at the end of the day and it would be like, over 200
Scott Benner 35:03
and I'd be like, Oh, that's, yeah, that's higher. And
Speaker 1 35:08
then there's this one time when I had stopped eating a lot of things, but for one, for whatever reason, we my kids and I used to go get acai bowls. I hadn't had those because I was like, I can't have that anymore. But for some reason I had one. I was like, Oh, I can have this every once in a while. So I had one, and then I went home, and it had been like hours, and I checked my blood sugar, I it occurred to me, like, I should see how bad that is for me. My blood sugar was like 350 and I was like 350 I was really like, what is that? Yeah, well, I mean, I knew how it happened, but I it, and it was also hours later, and I was like, whoa. And so I called my sister, and was like, I looked this up on the internet. It says I should go the emergency room. And I don't think I should, right, or should I? I'm like, Am I like, what's happening? And she was like, Oh no, you don't need to go to the
Scott Benner 35:59
emergency room. No, sweetie, that's gonna happen now, yeah, yeah.
Speaker 1 36:03
She was like, yeah, that's okay. She's like, you could maybe go for a walk or something, drink a lot of water. And I was like, Okay. And so I did all those things. My blood sugar came back down, like, you know, in a couple hours to like, 100 but that was kind of the beginning of, like, get I really was changing. And then also, during that time, last summer, in like, summer of 2024 I started losing a lot of weight, which, again, was kind of confusing to me, because, like, they're telling you to go on a diet, watch what you eat, and you lose weight, and you kind of think, Oh, I'm doing it. It's happening. I'm doing what they told me to do. But to be, to be, like, specific, I know in the podcast, usually like ask specific. So I'm five eight in 2022 I weighed 140 pounds. The next year, I weighed 120 pounds, wow. And then this last fall, in 2024 I weighed 110
Scott Benner 36:58
pounds. I'm sorry, did you go from like, reasonably, like, curvy to thin?
Speaker 1 37:03
140 is like healthy? BMI, yeah, totally. Like healthy, normal weight to like thin people. And my co workers were saying, Hey, you look really great, which was annoying to me, because I was like, Yeah, I have a chronic illness now. It's great, sweet. And then the next year, it went from, Hey, you look good to Are you okay? Like, and my manager even pulled me to the side and said, you've lost a lot of weight. Is something going on with you, which honestly made me really angry at the time. There are bones sticking out of my body that I've never seen before. There's like, all my muscle I lost so much muscle mass. I lost, like, there's like, concave parts of my body that shouldn't be like, it hurts to sit down skeletal.
Scott Benner 37:45
It's not I hear. And I just had a walked into the post office, and the person that runs my post office horrified when they looked at me, and she goes, Hi, are you all right? And I went, Whoa, like, what? And then it took me a minute, because I've now I'm a couple years into having lost weight, yeah, and I just hadn't seen her in a long time, so my brain doesn't catch up right away. And then I go, Oh, you think I have cancer? And she goes, Do you? And I said, No. And she goes, Oh, thank God, because her husband had just recently gone through it. So she, I think she had, like, a real visceral reaction to it. You know what? I mean? Yeah, yeah, it's and by the way, my butt hurts too, if I sit down too much now too, I hear what you're saying,
Speaker 1 38:26
but Yeah, and like that really made me angry a lot, because it just felt like, very, it just felt, I think I felt really like, exposed, like people just kept saying things to me, like, and then I felt like this, need to explain, like, Why, which I didn't necessarily like, want to get into all the time. And so it was this, like, kind of frustrating. Like, spiral. It's a little bit better now, because people are just sort of used to the way I look now, like there's like, everyone has seen me, and there's no more like, Whoa, don't let me put
Scott Benner 38:53
words in your mouth, but, but I'm assuming that when you're when you get diabetes, you feel like you're not in control your body anymore, right? And now you lose the body that you thought you had, and then your weight changes like that. And I imagine now you're like, well, it didn't work the same way anymore. Now doesn't even look the same way. Does it feel like two different losses?
Speaker 1 39:11
I don't know if it feels like that, but it just it feels like I see myself and I I like it. Don't look well, I think I'm starting to look better, but like, I just, I don't, like, I don't recognize myself, yeah, sometimes.
Scott Benner 39:25
And do you think you've just needed insulin this entire time? Yeah?
Speaker 1 39:29
Yeah. I mean, it's interesting, because, like, lat is so interesting, or whatever you want to call it, like, the more I look into it, I've done like, a ridiculous and insane amount of research about it like the doctors can't even agree what they really think it is. I think there's also a lot of like variance in the diagnosis. And I think there's so much for the medical communities to learn about diabetes in general, like all like, all types, so I think they really don't know. Lot about it, like, there's lots of different ways to think about it that are not just type one, type two. There you did, I think you did a podcast with that doctor who talked about the five phenotypes that
Scott Benner 40:10
Dr Hamdy. I was just thinking that, like he was so insistent that there will be more distinctions between types of diabetes in the near future, right? So it's maybe a thing that they're working on behind the scenes,
Speaker 1 40:23
yeah? So it's interesting, because it's like, being Lada, you feel kind of like you don't fit in. Like, sometimes I don't feel like diabetic enough. Like, I don't have like, full, like, diabetes card,
Scott Benner 40:36
like, like, you're like, I like, they're like, you're not type one. You're a lot of that. Yeah, you don't know what it's like, you know, because you're still getting help, I don't get any help, like that vibe, like, yeah, and then, or just it because you have again, just another way to be different, though.
Speaker 1 40:52
Yeah. Anyway, the story with, like, the Endo, the old Endo, is crazy because I finally got referred to Endo. I went to my doctor, the primary I might I weigh 110 pounds. I'm like, something's wrong. Like, I feel like something's wrong. I don't feel well, like something is I've lost all this weight. And like, she was just my blood sugar is, like, going really high. And she's like, how high? She's like, it's fine if it goes over 200 sometimes. And I'm like, but it's not sometimes. It's all the time. Every time I eat, it goes over 200 and she's like, that's fine. Just just really, you need to stop worrying about it.
Scott Benner 41:25
Clara, I have to stop you for a second, because at this point, I'm going to ask you the question that everybody listening is asking. But you're a nurse, how do you not know if you were looking at another person having your experience? What would you have done? Well,
Speaker 1 41:41
I did what I did, what I did. I went in and I said, this is what's happening. Yeah. And she just kind of kept telling me it was fine. And I said, Well, it's not fine with me, right? I said, I'd like to get a CGM. My sister suggested that I got a CGM. And she said, Well, you can, but we're not paying for it. And I said, Okay, well, you're right for it, and I'll pay for it. And she did. And so then, like, with the CGM data, I had a follow up visit with her. My a 1c was eight that time, which, you know, to me, I hate that. That's, you know, feels awful, but like, I know it's not like as world, yeah, it's not like 12 or 16 or, you know, it's like, they still, they still just don't really care. They're like, yeah, that's bad, I guess. Well, they were like, so she basically told me that if I want a better blood sugars than, you know, 200 that I could keep watching my diet and restricting my food. I said, I feel like I'm restricting my food because I don't want my blood sugar to go so high. But I weigh 110 pounds, and so I feel really trapped, like I don't know what to do. And she was like, well, you can either not worry about it, or you can
Scott Benner 42:47
restrict your diet. Wait, and what kind of doctor, this is
Speaker 1 42:51
my primary. Okay. So then she said, I'm referring you to Endo. So then she refers me to Endo, and I have a video visit with her, and she starts a visit. Was like, hi, I heard you wanted to see me, which I feel like she would have been told that, like, you're a problem. There was this crazy lady who was so worried about her blood sugars being high, and, oh, my god, what is her problem? So she's like, so I heard you want to see me. She's like, you are a type two diabetic until you need insulin. My brain was like, I don't think that's right, like, and at that point, like, I had already had my lot of tests, you know, like, I've tested positive for Gad, and she was just, and I was like, okay, so she's like, here's your new prescription for this other DP, DPP, four, and this is our protocol. And I was just like, but, you know, my blood sugar is going up this high. Like, I'm I'm I'm eating, like, nothing, like, like, Right yeah. I'm like, well, like, right now, I had plain Greek yogurt has five grams of carbs. My blood sugar is 190 and she was like, This was after talking for like, a half an hour. And she was like, your blood sugar is what? And I was like, 190 she's like, and you had how many carbs? And I said, Five. And she was like,
Scott Benner 43:57
Oh, well, you need insulin. I was like, Awesome. Awesome. I'm gonna jump out a window now. Thanks, everybody. Yeah, yeah, great.
Speaker 1 44:07
Office visit. I started type two now I'm type one, I guess okay, because according to her, that's what the difference in type one and type two,
Scott Benner 44:13
which five carbs? Yeah, the difference is five carbs. Had you told me that you had 20 carbs, I would have said, that's okay. You have type two diabetes. But if you only had five, then you have type one. This is my medical My God. And by the way, we don't want to say where you're at, but metropolitan area, right? A place where you might expect that there's, like, modern
Speaker 1 44:32
medicine Gotcha. Yes, yeah. Anyway, so then, like, the other struggle I had with this endo was to veer off topic slightly to pediatrics. So my sister also said, you might want to have your kids screen for the antibodies. And so I asked the pediatrician about this the same year, a few months before this was happening, and I said, Hey, you know, I just got diagnosed with Lada, and I'm wondering if I can get my kids screen for the type one antibodies. And she was like, Well, why would we. Do that. I was like, Well, I think the idea is, because my sister talked to me like that, it would help, like, look out for the signs of DKA, so that they wouldn't crash into DKA, or, you know, prevent, like, a more serious illness. And she was like, that's just, she's like, I don't know why we would do that. It's such a simple diagnosis. You should
Scott Benner 45:18
have said, maybe want to come back and live through the last months and months of my life, because apparently nothing about it's simple,
Speaker 1 45:23
right? And I was like, I mean, the way, I'm not very confrontational. No, I
Scott Benner 45:28
can tell, because they're not here, and you're still being polite about it. So go ahead, yeah, I
Speaker 1 45:33
don't like confront them right then, but I like, left the office, Googled it, Googled it. And was like, That was obviously wrong. And luckily for her, luckily for me too, she emailed me right away and said I checked in with pediatric endocrinology, and they said, Yes, we should screen because there's this medication T sealed.
Scott Benner 45:52
Dear Claire, do you remember that definitive thing I said to you 45 minutes ago? I was wrong about that. At least she did that. Yeah, I know. I just said there was no reason to do this, but I did check and they're like, yes, is that what pisses you off? Because it's what pisses me off. I'm getting angry for you. Oh yeah, I was very angry that she would so definitively say something that she did not know the answer to. She
Speaker 1 46:12
also really made me feel like an idiot, yeah, like she really made me feel stupid, like she went out of her way to really make me Phil,
Scott Benner 46:20
why would we do that? There's not no reason to do that. Oh, you're a nurse. Geez, you don't know anything. Like, yeah. Like, I got you
Speaker 1 46:28
Yeah. So I was, like, pissed. So then I got my kids screened, and then getting them screened, I kind of started to look into Teasel a little bit more, because I was, you know, wondering why I'm screening my kids, right? Like, I want to make, kind of make sure, like, I know what I'm doing. Why I'm doing it? What would happen? I start reading about T cell, and I'm like, wait, like, Could I get T sealed? Like, I started thinking about it, and then I asked my atendo about it. I said, hey, I'm interested in this medication, T sealed. What do? What do you know about it? And she responded, Well, you don't qualify for it because you only have one antibody. So then I have to email her back. Well, can you test for the other antibodies?
Scott Benner 47:01
Yes, we only looked for one. So yeah, we found that one. What if we looked for more? So
Speaker 1 47:05
then she said, T cell is a medication for children, and if you had more antibodies, you would have already been diabetic by now, like when you were a teenager. And I said, Great, so can you just test for those, please? But that's not right at all. No, it's not right again, this is then. I had another time where I got asked for those tests. She She said, Fine, I'll test for them. She did. They all came back positive, positive for all of them, except for insulin antibody, which she couldn't test me for, because at that time, they had just put me on insulin. It's like a Pokemon. You collected them all. Yeah, I know. So like, again, I got that test result back, and I was had this like crazy feeling when I when I came back positive, of, like, I knew it, I win. And then again, I was, like, again, not really a win at
Scott Benner 47:53
all. Do you go back to her and say, hey, if I have all five of these, how come I haven't had diabetes for 30 years?
Speaker 1 47:59
No, I, like it was in our messages. So, like, I just really hoped that, like, she had to look at her last message a little bit before she and I said to my friend, I said, I hope she chokes on her coffee this morning when she sees this. And she's my friend, so mean, says to me, she probably doesn't care at all. And I'm like, You're right, she probably doesn't care at all.
Scott Benner 48:18
What do you think? But how long have you been a nurse, 13 years. Why do you think this happens?
Speaker 1 48:24
I think that she really didn't know anything about type one or adult onset type one, and she really was just only dealing with type two and like, I don't know. I just
Scott Benner 48:34
think that's the functional reason. Why do you think a person who is holding your health in their hands, right? You're the one. You're coming to them and saying, I don't know what to do. You help me. And they answer definitively over and over again with the wrong answers,
Speaker 1 48:51
yeah, yeah. And like, I don't know. I don't know the answer for that. I know that healthcare is not perfect, and I see a lot of things happen that aren't perfect all the time. That's just the way it is. And I guess I'm sort of accepting of that, because I've seen things happen, yeah, all the time in a completely different setting, that in the hospital, that is, we do a great job, but I things aren't perfect, and you really do have to watch for watch out for yourself. And like that leads into, like, something else I emailed you about, of just medical distrust, which is, it is funny coming from somebody in the medical world, but like, I mean, I watch doctors looking up things on YouTube, like they don't, they don't know everything. Yeah, they really don't.
Scott Benner 49:33
Sure. I'm freezing up because I don't know if I said this on the podcast recently or not, but if I did whatever, you just live through it. Arden had to go to the emergency room this weekend. She's got tonsillitis. She gets it a lot. We're probably gonna have her tonsils taken out. She starts on a Monday on an antibiotic that she runs for three days, no change. They change her to another antibiotic four days. No change. By then it's Sunday night, two. We really are, like, something's like, she's in trouble. You know what I mean? Like, her tonsils are crossing each other. I'm talking to the doctor on the phone, and the doctor's like, Hey, I think he, you know, I'd like to move her to and she gave me the name of the of the antibiotic. She's like, a much more broad spectrum, but she's like, I can't get it to you now. Like, I think maybe she's at the point where you need to go to the ER and get this through an IV. And I was like, All right, fine. So, like, It's nine o'clock at night on a Sunday, and, by the way, fine, I'm old, like, at this point, like it was the end of a weekend, and I did things that weekend. Like, the last thing I should have been doing was driving to the hospital. Like, all right, right, on, let's go, you know. But while Arden was getting her stuff together, I walked chat GPT through the last week and a half, or the last week of her life with this, and asked what I should expect to happen at the hospital. And then I read through it real quickly. And then I went to the hospital. I did not, I did not look at it while we were at the hospital. And we got a very proficient doctor, okay, and I felt very comfortable the whole way that she was going through things, the way I would expect, and everything. But I stopped maybe three hours into our time at the ER and I went back to chatgpt, and it was like she was reading from chatgpt, which made me realize that this is a thing she probably deals with all the time. So she knows the words to say, because she's probably said them 1000 times, and that this is a very clinical thing. There's not a ton of different answers to these questions. But I was stunned at how perfectly the AI mimicked what she said, which, instead of making me think like, oh, wow, AI is awesome, it made me think she doesn't really know that, much like this is not a special magic person standing in front of me. She just knows the things that this thing just knows how to get to as well. And then we got to the point in the night, Arden had had IV steroids, by the way, I asked the nurse administering the IV steroids, I said, about how long until I see this impacting her blood sugar. And you know what she said? Three days? Oh, three days. Three days. I said, Not 30 minutes. No, about three days. I said, Okay. I texted my wife, I can't listen to the nurse anymore. Now I know she's willing to say she doesn't. Doesn't matter if she knows what she's talking about or not, she's willing to say whatever pops into her head. The doctor says, Look, we're going to image to make sure Arden doesn't have an abscess. I said, that's fine. And if she doesn't, she goes on. If she doesn't, you know, you head home, blah, blah, blah, like all this stuff. If she does, we have to keep her overnight, because she's gonna need another round of IV antibiotics, and, you know, otherwise, like she's going I said, Okay, well, why don't we wait to see what happens when the scan comes back? So now it's 230 in the morning, and the scan comes back, and she says, Great news, no abscess. I'd like to admit Arden. I said, why? She goes well so she can get another round of IV antibiotics tomorrow. And I said, Can't you just give her oral antibiotics, the same one that she could, like, I could pick it up tomorrow morning, and she could keep going with it. It shouldn't be any problem, right? No, yeah, you can do that. And I said, Well, I said, then I'm gonna do that, because three o'clock in the morning, I just want to be candid. I've been through this before. I don't want Arden diabetes being managed in a hospital if they it doesn't need to be, because, no no offense, you don't know the first thing about it, and either does anybody upstairs, and there's gonna be steroids on top of everything else, you're gonna be waking her up all night long to check her blood sugar when she doesn't need it because she's wearing a CGM. I want her to go home and rest and let these antibiotics work. And she goes, Well, airway. And I said, her airways look like this for seven days. You think she's gonna die tonight? And she goes, No. And I went, Okay. And she was, well, I could get a form for you to sign, and you could relinquish the diabetes from us to you and we won't touch it. I said, So your answer is that you're not going to help her at all while she's asleep in the hospital. I'm like, wait a minute. She might need some help. Like, I'm not saying, like, let's forget about it. I'm saying, Don't tinker with her diabetes. And they went back again, and I was like, so why do you want her to stay? And she goes, Well, I'm worried about her airway. And I said, Do you think it's going to be a problem? And she goes, No. And I'm like, I don't know what we're doing right now. And I was like, I'm going to just, can I just get a prescription for the antibiotic? I'm going to pick it up in the morning and I'm going to take her to an ENT tomorrow. And she goes, Oh, you'll see an ENT tomorrow. And I said, Yes, I promise. And she goes, Oh yeah, sure, you can leave that. And meanwhile, my wife's texted me, well, if they want to keep her, let them keep her. And Arden's, like, we got to get the hell out of here. Also, Arden's still dealing with a needle phobia. There's an IV in her arm that's been in there for six hours that she's been staring at it for six hours. Like, I can't believe there's a tube in my arm, which is, I know, ridiculous, but it's a thing she's going through. Anyway, I get done, and we get out in the car, and Arden goes, Why did she want me to stay so badly? And then give up on it so fast, yeah? And I was like, yes, Arden, that's the right question. Yeah. Is it a problem, or is it not right? Like, you don't have an opinion, yeah, yeah. And so, like, your. Opinion was my opinion after she knew that my opinion wasn't her opinion,
Speaker 1 55:05
which is good when you feel like, okay, I got them to do what I want, but then you're like, but wait a minute, like, why is it so easy
Scott Benner 55:10
to right? Because now I'm in the car at three o'clock in the morning thinking like, am I taking her home for her to like, aspirate? Am I wrong? Like, because I don't like, I don't want to be wrong. Then I went back through my common sense again, and I was like, No, I'm like, This doesn't look any worse than it's looked for days. She hasn't died so far, and now we've hit her with such a broad spectrum antibiotic that the truth is that if this doesn't start working, she's in some serious trouble that does not appear to be going that way at all. But all that aside, tell that whole story like, so I can tell you, like, what I know for sure is that that lady didn't know anything for sure, but she kept telling me she did. And then I pushed back, and then she went, No, it's fine. And I wasn't like, I know what now I'm I'm a little heated while I'm talking about it, but I was not argumentative or allowed like I was talking to her very normally. I'm like, you know, just asking questions, letting her answer the questions. And anyway, my The last thing I did was I went back and I asked chat GPT the rest of the conversation. And chat GPT was like, Yeah, I don't think that she needs to be admitted to the hospital. I was like, I keep saying this, but like, How closer do we to medical people just being the facilitator of what the machine tells them to do.
Speaker 1 56:21
Yeah? I mean, I think we're I think we're there. I think a lot of what I've because I've been so crazy in the last little bit, like, I've been listening to a lot of, like, medical, like, really, in the weeds medical podcasts. AI is definitely coming for their jobs. Yeah, sure. No kidding, right? Especially radiology. Radiologists are they're done.
Scott Benner 56:44
They're scrambling. Also they're done. I know a guy who's got a friend who makes a small fortune living at home, oh, at home, reading scans.
Speaker 1 56:52
I think you better invest well, because they're time is ending, but partially to you, I think I've been using chat GPT for a lot. I find it really helpful for communicating with doctors, because I'll ask it something, and then I'll say, please use medical journals citation. So then it will give me this. So I'll ask it a question, and I just copy and paste it to like my doctor in response for something. Because they'll be like, No, we don't want to do that. And I'm like, well, the evidence and the research says this blah, blah, blah, and it's very like, you know, chat GPT is very unemotional, like, and I don't have to get all worked up writing it. I can just be like, okay, yeah.
Scott Benner 57:33
A year ago or so, I had a guy on who was talking about this AI thing that they guy was developing for diabetes. And the truth is, is, I don't even know if he's still working on it or not, but I do know that he pivoted a little bit and came up with another product. And I don't think he would mind me saying it was an idea I had that I shared with him. It's going to be for endos and for diabetes educators, right? But you're going to sit down and do your, you know, do your visit with a doctor, but the the AI is going to listen and record the whole thing, and then it's going to do the transcription notes for the physician, and it's going to pull out like, like. So my idea was and remains, that if you spoke into an AI that that had memory and continued to tell it, you know, visit after visit, year after year, all of your concerns that eventually it might be able to piece something together and go, Oh, you know what? Three months ago, she said her hands were cold, and two months ago she said that, you know, her digestion was off, and that could this person have low iron? Like, you know what I mean, like, that kind of thing that a doctor's not going to put together. Because I know people love to go to the doctor and think, Oh, they're so nice. They, you know, they always remember this or that. I'm like, I tell people all the time, like the last thing the doctor does is stand outside the door and look at your chart so it appears like they remember you when they come back in the room. And I was like, I know you remember them because, you know, it's a much more. It's a different relationship you have with them than that they have with you. But you can't expect those people to remember that six months ago you thought, you know, you got dizzy when you stood up real quick, like or something like that. But if you continue to have that conversation and that AI remembers you and everything you've ever said, I think people are gonna come to like, diagnoses of like, you know, from as simple as my settings aren't right and need to be adjusted to this person might have Hashimotos or like, like, that kind of thing much more quickly. Yeah, yeah.
Speaker 1 59:32
The most recent thing I used chat GPT for that saved my life was, I guess, a little segue into, so I ended up changing insurance from Kaiser to a PPO, we have either option, so I started using the providers at the hot the university hospital that I work at with the hope that they would have some better perspective about this. Also, when I was screening my kids, I asked the. Research assistant who was asking me about my diagnosis, and you know why I'm having my kids scream, blah, blah, blah. And she said, Oh, the adult endos at our hospital are so great. And I was like, Can you give me their name, some names of some recommendations. So she did. I looked up those doctors. I emailed that doctor on my work email, which was really worried that was like, overstepping somehow. I was like, Hi, I am a nurse in the blah blah blah, and I'd really like you to take me as a patient. Because, like, those they, you know, and those are really hard to come by. And, like, basically, they said, This doctor only takes patients by. Like, they go, they look at it, and they decide if they want to take you or not. And I was like, great to, like, audition for this doctor. He ended up taking me as a patient. The first visit we had was in April. So I switched insurance, you know, January, have a visit in April. So basically, between, you know, I was basically on my own. Anyway, from the whole time, you know, they prescribed me insulin, they told me very bare minimum what to do with it, and that was pretty much it. But, like, I really didn't even have a doctor helping me until April, like, basically a month ago. Yeah. So I had my first visit with him, and he had some interesting things to say, which was really, like, surprising. So he immediately started me on a medication called verapamil, which is a blood pressure medication, but they've found has benefit, like, off label benefit of beta cell preservation. Okay, so that was new information. I'm telling my sister, oh my gosh. Like, I have searched the internet, like, for Lata type information. I was like, he knew something that I never have even seen. And she was like, Well, I hope he does. And I'm like, okay, true, true, but I haven't found that to be true. He started me on this medication that supposedly has really good beta cell preservation, and with the idea that, like a lot of the studies they're doing show that, like any beta cell function is benefit beneficial? So that's like, his number one, he's trying to get me t sealed after Kaiser said, No, we're not giving you T cell,
Scott Benner 1:02:08
because it's not just for kids, right? It's, no, it's not. And, like, I said that, I was like, that doesn't sound right to me,
Speaker 1 1:02:15
but it's not. It's not just for kids. They it's, I mean, it's up until 45 so this is technically my last year I could get it. So if I get it, it will be hopefully this
Scott Benner 1:02:25
year, but it's a thing you're up for trying.
Speaker 1 1:02:28
Yeah, it's awesome. Totally, yeah, you too, yeah. And even though, like, at this point, it doesn't feel as dire, last fall, it felt so dire. And I think I was really wrapped up in trying to get it, because I was really wrapped up in, like, trying to stop it from happening. But now that I've been in on insulin for a while, it's kind of like that ship has sailed, and I'm kind of like, well, if it gives me some benefit, then that would be great, yeah? But it's not like I'm expecting, it doesn't
Scott Benner 1:02:53
feel like it's a do or die thing for you at this point, yeah.
Speaker 1 1:02:56
But it felt kind of do or die last fall. I was like, yeah. And then I filled out, like, a whole medical grievance and like that when I really didn't want to, it felt like something I didn't want to do, but I did it anyway. Actually, I really wish I had asked chat GPT to help me with that. And I think my argument was great, but the Kaiser said, No, that's no, you don't we're not giving it to you, really. So he then tried to get me that and like, even though it is not just for kids. I think a lot of the screening that has been done is kids and siblings of type one kids. So I think a lot of the population that is that T cell is being focused on is kids. And if I were to get it at my very big university hospital, I would be the first adults on the adult side to get it. They have done a few kids, but they haven't done a lot. I mean, that, I think the thing with tz is it's so expensive, it's
Scott Benner 1:03:46
tough to, like, it's like, a 13 day infusion or something. Yeah, a lot of people have to, like, go somewhere, stay in a hotel while they're doing it. Like, it's, it can be, yeah,
Speaker 1 1:03:55
yeah, they're doing a lot of home infusion though now, so, like, I could have it done at my house. That's awesome. Yeah, so we'll see where that goes.
Scott Benner 1:04:03
Can I run something past you? I've been working on something that I haven't really told anybody I've done yet, but I've set up a private like circle community for the podcast, which I'm getting ready to make more available to everybody. And I, you know, I'm not gonna charge anybody to use it, even though it's a pretty significant cost for me to run it, and I'm doing it because the platform now comes with its own AI agent. I can feed it all of the content from the podcast, and then when you ask the AI agent a question, it only answers you from what's been on the podcast. So like so I just asked it, what should I do if I suspect Lada and doctors aren't listening to me? Yeah, and it said, If you suspect you have latent autoimmune diabetes and adults are Lada and feel like your doctor's not listening, here are some steps you can take to advocate for yourself. Educate yourself. Learn as much as you can about Lada. Understanding the symptoms, progression and differences from other types of diabetes can help you communicate more. Effectively with healthcare providers anyway. It goes on document your symptoms, tells you about how to do that, request specific tests, seek a second opinion, clearly communicate leverage support networks around you, tells you what they might be consider going to a diabetes educator instead of your regular doctor. And then I said, Okay, great. Can you educate me? And it said, certainly. Here's detailed overview of Lada. What is Lada tells you a lot. It tells you what the symptoms are. C peptide test, antibody testing, differences between that and type two, how you would treat it with monitoring, insulin therapy, lifestyle modifications, challenges in diagnosis that's just pulling from. Oh yeah, the small sips, bold beginnings and Pro Tip series. I haven't even uploaded everything yet. Yeah, I'm trying to be way ahead on this, because I think this is the way a lot of people are going to figure things out, and I figure maybe help them get to the answers, and at the same time, giving them a community to talk about it in is my idea. So,
Speaker 1 1:05:56
yeah, every time I listened to a lot of episode, it was like, like, I just felt so like, heard and not so alone, you know, like, because it's just like the stories are the same. And I mean, my story, honestly, is not as dramatic as a lot of stories, like a lot of people end up in the hospital in DKA. I kind of credit my I credit myself at least a little bit with like that. I was trying to monitor really hard. I was trying to do my best, but and, you know, I think I did what I did, and they did what they did, and I think we
Scott Benner 1:06:28
are and we just make the best of it. Listen, I know a person who's going through this right now privately, and parts of their life are falling apart like it's not like they've got relationships that are coming apart. It's a weird position to put somebody in, like, you have a thing kind of, maybe we're not really gonna do anything about it. Just watch it, like, that's like, whoa. What am I? Like, you know, and then, like you said, like the running around trying to fix it, or bargain your way out of it, or ignore your way through it, or whatever ends up happening to you. Like, none of that's valuable. None of it. Yeah,
Speaker 1 1:07:02
and I think, you know, there's always this question of, like, Is it easier as a kid or as an adult, like to be diagnosed? I don't think that's a really helpful question, but I see it thrown around a lot, and I think for sure, it's harder for kids, like, that's my opinion. It is hard as an adult, because, you I think there's a lack of, like, empathy for adults. Like, there's this, like, well, you there's like, a kind of a, maybe it's, maybe it's me, but like, I do feel like, I feel like I could have prevented this, or I should be doing more. And like, because it is so confused, in general, with type two. And like, the narrative around type two is that you can reverse it. So it's like, this constant, like, explaining to people that you can't reverse it, and it's like, I didn't do this to myself. And then I'm like, why am I even explaining this to anybody? Like, why do I even feel the need
Scott Benner 1:07:53
to, like, it's a pretty human trait to not want people to think you messed up. That's for sure. Yeah,
Speaker 1 1:07:58
yeah, yeah. I guess that that is a big part. You just really but then you just feel so kind of pathetic. Like defending yourself, like, over and over. Like,
Scott Benner 1:08:06
also that one human trait, right there is probably the thing that stands in the way of there being better communities for people with type two diabetes. It's a
Speaker 1 1:08:14
big issue. And I will say working in healthcare like diabetes really is thrown around as, like, an accusation. There's so much stigma. And like, the unit that I work in, there's so much, like, sigh, uncontrolled diabetes. You know, people just say this, and they don't even really know what they're saying, and they just say it as this, like, indictment against somebody. And now I just get so bothered by it. I'm like, imagine, you don't know what's going on with this person?
Scott Benner 1:08:40
Yeah. I mean, listen, when you watch a thing unravel and eventually fail. When it eventually fails, it normally fails because of, like, some lack in, in human understanding, compassion, desire, like, something, at some point a person fails, and that's where the thing goes off the cage. Like, like, how crazy is it that a medical person would like come in, smile at you, do the whole talk up, then walk out in the hallway and look at a friend and go, there's another one in there with the diabetes? Yeah? Because that person, probably mom, probably has diabetes, or somebody in their life does, or they might end up having it one day, and then, you know, once it's too late and they understand it's you can't go back.
Speaker 1 1:09:19
Yeah? Yeah, I use chat GPT because then my new endo set me up with Omnipod, and he happens to be like an expert with Iaps trio. So he set me up with, he built it for me. Awesome. So it's exciting. It's been, it's really new that I'm using it. It's really cool. And I'm still, I'm just, for the first time, feel hopeful and like, happy and like that, somebody is taking care. You get
Scott Benner 1:09:47
a little help, right? I mean, are you able to give away, not giving up on but giving away that feeling of like, I've done something wrong and there's more I should be doing. Like, is that, is that lessening for you, or is it still holding on to you pretty
Speaker 1 1:09:58
good? I think it's still. In there somehow, like coming up on my meet, like my appointment with him, like waiting, there's so much like anticipation. It was like, had to wait so long for this visit, like I had. I kept thinking, what's he gonna say? Is he gonna say you should watch your diet? Like, it's still like, is in my head, like you should, you could have done something better, you you should have been able to do this without insulin. You know that's not true. Then I do know that's not true. It's just
Scott Benner 1:10:30
it's hard to it might be therapist time. Claire,
Speaker 1 1:10:33
yeah, so that's another part I did. I did, like, last year, when I was with Kaiser, I recognized that I was having a really hard time. I was, like, really depressed and like, having a hard time. So I was like, I don't want to do therapy, but I guess, oh, that was the thing when I saw my primary, when I first went in 110 pounds, saying, I feel like I'm trapped. I can't eat, but my blood sugar is high. And she was like, Do you want meds? Oh,
Scott Benner 1:10:57
she wouldn't give you insulin, but she'd give you a psych med. Yeah,
Speaker 1 1:11:01
yeah. And I said, No, I don't think that's necessary. I think maybe counseling would be a good idea. And she said, Okay, I can refer you to that. And the other thing that she did this is, I'm like, rehashing. It's hard not to rehash the like, bitterness. But like she said, you know, after talking about my blood sugar, then she was like, but I am worried about your weight loss, and I'd really like to try to figure out what's going on. And I was like, I think it's my diabetes. And she was like, I'm gonna do a full workup. We're gonna do labs, we're gonna do imaging, just to make sure there's nothing else going on, like cancer.
Scott Benner 1:11:36
So instead of elevated blood sugar leads to weight loss. She said, maybe you have cancer.
Speaker 1 1:11:42
Yeah. She was really trying to figure out what was going on with me. She didn't know. I
Scott Benner 1:11:46
don't know what to say. I'm gonna give up. I know. Well, listen, I say this all the time. I'm happy to say it again. You guys out there, I know there's some great doctors. God bless you. Keep going the rest of you. I really appreciate you making my podcast so popular with your inept use of your profession, if everyone would just do their job, nobody would listen to this.
Speaker 1 1:12:06
Yeah, I know it was like and then later I went back and I read her visit notes, and she wrote that I had OCD tendencies and was too
Scott Benner 1:12:14
focused on my blood sugar. Do you get to leave notes? Yeah, I
Speaker 1 1:12:18
did. I left a few notes about it. I left my feedback for Kaiser, very strongly. I used her name, and I said, I want to make sure that this doctor name knows that she made my life worse.
Scott Benner 1:12:31
See, you're as polite and pointed, I would have been like, I just want everybody to know this lady's a and I don't have OCD. She went from ignoring my elevated blood sugars and them being a reason for my weight loss to I need 10s of $1,000 worth of tests to prove that I don't have cancer.
Speaker 1 1:12:48
Yeah. But then the funny thing was, so then I did the labs, and she said, depending on the labs will do imaging. And so then at my next visit with her, I said, so we did these labs, and you talked about, you were worried about something going on. What's the plan with that? Are you still worried about that? She's like, we'll talk about that.
Scott Benner 1:13:02
What she meant, I don't remember who you are, yeah, yeah.
Speaker 1 1:13:05
No, she I was like, so I was like, so you're not worried about that anymore. Or are you worried about that? Remember how you were worried about that? She was like, but she's like, why don't you go and see your Endo, the Endo, and then we'll touch base later. And in my mind, I thought I am never looking at you again. I
Scott Benner 1:13:19
don't know how more people aren't assaulted. Jesus, I'm sorry. I mean, like, I didn't do it to you, but I'm so I hope the podcast has been helpful in some way for you.
Speaker 1 1:13:28
Good. It has. It has been so helpful. I was thinking about like, you know, what is it why I started listening to it? And I was like, I hear a lot of people say the same thing, like, I felt just compelled to keep listening to it. I think, in a time in which I felt just very alone and like confused, it just, I don't really like the Facebook groups, not yours specifically, but just in general, I don't like the vibe of the Facebook vibe, but I really like the podcast. I like the people's stories, how different everybody is, how different everybody's situation is. For me, it was really helpful. Like, hearing people who had so much going on and still had such a positive attitude and were just getting through all of the things, and I thought, Gosh, I only just have this one thing, like, get it together, not in a bad way, but just sort of like, you know, but like, it's different when you're all going through the same thing, you know. Like when somebody who's not going through it's like, just be fine. You're like, Screw you. But like, when, but when my sister tells me something, I can like, able to like it like I can hear it, because I know she's going through it, she understands, yeah, and I forgot to mention my new endo has type one himself. That should be helpful. So, yeah, also, so that's helpful. And then so I did that therapy through Kaiser. That was not helpful at all. The person was not helpful. I found myself having to explain, like, why diabetes was stressful a lot of the time, you know, like, I just haven't explained a lot, you know, like, she was just like, oh, okay, well, what you should do is, like, not be so stressed about
Scott Benner 1:14:54
that's the thing I joke about, you know, I get on the podcast, I'm like, hey, you know you should, you should calm down. Because I know that's. A ridiculous thing to say to somebody who's experiencing stress,
Speaker 1 1:15:03
yeah, yeah. Or, like, I was like, I'm really stressed out, because I tried to spell out all the things that doctors had done, like that they were wrong about, and that I was right about, and that I really felt like stressed out, that I had to watch every move and I had to, like, I felt this. I was a little, I mean, I was a little crazy, like, I felt like I had to know everything, because it didn't feel like they were doing anything, you know what I mean? So like, I was really hyper focused, because I felt like if I wasn't, then something was gonna get
Scott Benner 1:15:35
missed. That's not baseless, because a lot is being missed. Yeah, I'll take you back all the way to, like, Arden being four years old, and me going into the school to say, like, look, we have to start. Let's set up now how we're gonna handle it when she gets here for kindergarten next year. And they were like, they laughed. They literally laughed at me. And by the time I left, I was like, Oh, they think I'm crazy. The difference between you and I is I'm a bit of an asshole too. So like, I'm like, You seem like a nice person. Go. They think I'm crazy. They don't know what they're talking about. You take it more to heart when somebody says something like that to you. Like you're like, Yeah, I do. I have no ability to, like, care what they think. By the way, I care of what plenty of people think when they're making sense or they're exhibiting that they care or understand something or whatever. But like, if you're just gonna look at me blindly, know nothing about type one diabetes, and then tell me I'm overreacting, like I've been living with it for two years at that point, like I'm not over, I'm telling you, but bare bones needs to happen. You're in the same situation really, like you're not crazy, like you're you're in a really bizarre situation that a takes time to, like, get through personally and psychologically. B is supposed to be assisted by a physician. And every physician that you run into seems to be a dick. Yeah, I'm not crazy. I'm like, I'm looking around. And, you know, none of the things that are supposed to be happening are happening right now,
Speaker 1 1:16:55
right? And it's hard enough to go through it, and you do feel like, yeah, I have grief about just the diagnosis, like the lack of, you know, like a lot of as an adult, you're like, I love I live my whole life with this freedom about things, and now all of a sudden, like, everything feels different, and that's hard, but like when you're going through those feelings of grief, like with any chronic illness, or you know it, or you know, things that happen in life, but then you're also feeling like You're having to micromanage. You're having to become a doctor in your spare time. You're having to check everything that's happening, reading medical journals, like struggling, and then arguing with people, and then they keep they keep arguing with you, and you're like, at what point are you gonna, like, realize that it's irritating. You're not doing a good job. You just feel so kind of like you're just in battle mode, and it feels, yeah, exhausting. Advocate
Scott Benner 1:17:43
for yourself. Oh, I advocated for myself, and the person told me to go away, or ignored me, or just pushed me off to another doctor and then wrote my notes that I have OCD because I care about my blood sugar. And
Speaker 1 1:17:53
then she was like, you're stressed out. I'm like, I'm stressed out because my blood sugar is high. She was like, stop looking at blood sugar.
Scott Benner 1:17:58
I'm like, the right answer. It's no, you got it wrong. Yeah, you know, I'm on a tightrope over a volcano. I gotta look at the rope. Okay? Like, can you move the volcano? That would be helpful? Like, like, don't tell me to ignore something that needs attention and you're not willing to give it attention. That's
Speaker 1 1:18:14
crazy. And then say I'm crazy for being upset about it. And like, they would, they told me, parameters are, like, if your blood sugar is not less than 182 hours after you eat, then, you know, blah, blah, blah. And I'm like, my blood sugar is not less than 182 hours after I eat. They're like, that's fine. I'm like, so what's the point of the numbers you're giving me? And they're like, every once in a while, like, if you have a piece of cake, I'm like, I'm not saying I had cake. I'm saying I had plain pre
Scott Benner 1:18:37
carbs, not cake. Why is nothing making sense? You know what? Between you and I, Clara, I know your name's not Claire. I hope she chokes on her coffee too. So yeah, and maybe spills a little bit about herself at the same time while she's joking. I mean, really, I genuinely try so hard to remind myself, like there are great doctors there. You could have intersected a physician. None of this would have happened.
Speaker 1 1:18:58
Yeah, every once on the podcast, I'd hear somebody be like, Oh, this happened, and they referred me to Endo, and they did this. And I'm like, Oh, awesome. Oh, man, like that
Scott Benner 1:19:07
would have, what would it have been like, I would have met somebody who understood their job. Yeah,
Speaker 1 1:19:12
I do think about that, though, and I wonder, like, how it would have or, like, I look back at my a one CS before, and they were 5.6 for quite a while, it didn't flag to me because it was in their green range, like, after my pregnancies, it was 5.6 a couple times. And now looking back, I'm like, Oh, 5.6 that was in some
Scott Benner 1:19:34
zone on those I yeah, I probably don't complain about it enough, but people who don't know what they're talking about, they're just like, green, good. Green's good,
Speaker 1 1:19:43
yeah, well, I mean, you can only know so much. Like, at that point, you know, I had two little kids thinking about, like, No, I know, I know. But yeah, they never said anything. But I do think about, like, what would have I done if, like, that 5.6 they had been like, you should watch your diet. Like, you know, three years, four years before that. That's, again,
Scott Benner 1:20:01
no, that's not what would have happened if, if you would have asked me five or six years ago, if you would have said to me, Hey, Scott, my a 1c has been 5.6 for a while, what do you think about that? I would have said, is there any history of type one diabetes in your family? And you would have said, Yeah, my sister and I would have said, Hey, I think you're a lot of like, that's not hard if you ask chat GPT that it would have said that if you went in there right now and said, Hey, pretend I'm a 42 year old female. My a 1c has been 5.6 for the last 18 months, and my sister has type one diabetes. What do you think I should do? It would tell you you should go do all the things that you're supposed to do. That's the thing. I put up an interview recently with a young girl. She's like 26 right? She's got all of these problems, and she lists them out. A lot of them sound like hypothyroid, right? And I said, Hey, you ever been tested for hypothyroids? Yeah, no, it's good. My, my tests are good. I'm like, you have access to those tests? She says, sure. She pulls them out. Her t4 is like 2.6 and I said, 2.6 with all these things, you have a thyroid issue. And then I talked to her for a little while longer, and I was like, you're anemic. And she's like, right? And I'm like, All right, well, we maybe don't trust the high TSH because you're anemic, but let's get a an iron infusion, get that fart and up, and then after it's up, we'll rerun the thyroid labs if you're still 2.6 and I'd like to see you do a thyroid replacement. Now, there you go. Clara, I barely got through in high school, okay. I never went to college. I am not a physician, and it took me eight minutes to help her. I
Speaker 1 1:21:29
feel strongly that my providers were very lazy, and they just were doing the absolute bare minimum, and they were just had an extreme lack of interest in my health or my well being like that was my feeling, and that is what I told Kaiser as at my exit interview. But they're like, why are you leaving? And I'm like, basically, I found your doctor.
Scott Benner 1:21:47
Nobody helped me, and you won't change it, and they're not going to change and everything listen. I mean, if I had one message for people in medical school, like, if you're an adult, like, really try hard not to be in the part of medicine where you deal with people because, like, it's not for you. You know what I mean? Like, I know people have a bad day once in a while and everything, but you're describing, like, multiple visits this person had a number of opportunities to, like, pull their head out of their and treat you differently, and then they called you O, C, D at the end. Like, so you know, if you're bad with people and you don't really care about their health. Like, why don't you get a different job? Like, let's maybe get a couple more doctors who give a like, maybe that's what I'm seeing, is that the good ones care and the other ones are just, like, I don't know. Like, I'm just trying to make enough money to make a car payment here and get a cool beach house. So, you know,
Speaker 1 1:22:37
yeah, I mean, it's not the right field to go into if you're just trying to live it not for
Scott Benner 1:22:43
you. Quiet life, not for you. It's not, not for the patient. It's, it's, it's probably a great life for them. They're not thinking about a goddamn thing, and they're making a, you know, a couple $100,000 a year. I bet you it's pretty awesome. So I don't know. Anyway, you're being beat by a pot. You know how you were celebrating something ridiculous. I'll celebrate something ridiculous too. I'm a podcaster, and I could figure this out. I know. Okay,
Speaker 1 1:23:06
I felt the same way. I was like, you know, anyway, I felt like I learned everything from the podcast, and the podcast really helped me. I think, I think what I like about the vibe of the podcast in you is like, you have, you take it seriously. Obviously, it's something that's been serious in your life, but you have, like, this positive, like, we can do it attitude. I think that really resonated with me and made me feel like, yeah, we can solve this I can solve this problem. Like there are tools. Because up until then, it was like, Yeah, you got this problem. Don't have anything for you. And
Scott Benner 1:23:40
the people are supposed to have the answers, have, they're literally less than helpful. Yeah, they're just like, that's too bad for you. They might be making it worse, if I'm being honest, right? Yeah, no, of course you can. Like, this is not rocket science. Like, there's, there's just a couple of things to know and about how to use insulin. There's a couple of things to know about food, and there's a few things to know about your testing and your you know your your vitamins and your your you know your your additives that you need for your life and stuff like that. Like, that's pretty much it. And you know you have autoimmune issues, so there might be extra ones. So, like, let's look out for them, because they impact each other. There you go. Is the whole secret. I didn't even need to go to medical school for four years. I'm an endocrinologist now. Yeah, by the way, you're never going to be privy to the private conversations that I've had with two dozen doctors who will tell me privately, you're a better endo than half the people I work with. And I'm not just saying that to say that, like, that's been said to me so many times I've lost count, and that's ridiculous, which what that means it's you're not saying something about me, you're saying something about them. They could do it too. Like, just like I'm telling you, you could do it. What I'm hoping they're hearing is, you know, what, with a tiny bit of effort, I could do this for people. And since it's already my job, and I've got the degree, what the hell, why don't I go for it? You know? I mean, we're already here, might as well do it.
Speaker 1 1:24:57
Yeah? Well, I listened to i. Like I was. I actually not really wanted to listen to any of the episodes with Erica. I remember seeing them and being like, I don't want to hear about therapy. I hate therapy. And then I listened to a few that really like resonated with me. And out of curiosity, I looked her up and saw that she takes a benefit that I have at work, Lyra. So I've been talking to Erica awesome, which has been super helpful. I can't even, like, express like, the difference, like, of the feeling of talking to someone just who understands, like, I don't have to, like, explain things. I can just talk about the things that are bothering me and like, we can talk about that, as opposed to be like, well, this is stressful because, like, you know, and I'm explain a bunch of things,
Scott Benner 1:25:42
I always feel better after I talk to Erica and she's not my therapist, which I think I have to say legally, or she'll like, she gets mad at me, because there are times when those episodes, I'm like, she's like, I'm not your therapist. I'm like, I know, I know, I'm just talking through but no, she's
Speaker 1 1:25:56
good. It's a good ruse you have better on the podcast, how
Scott Benner 1:26:00
I'm getting how I'm getting free therapy. Yeah, don't let her hear that. She's crying already. If she heard you say that it's helping her, she's all like, she's all touched right
Speaker 1 1:26:09
now. So, yeah, it's like, I dreaded talking to the other person, and like, I don't I. I'm like, Yay, it's my time to talk to Erica. And I talked her, and I joke with my sister that I'm just weeding everybody out of my life who's not a type one diabetic like in order to be in my life now, you just have to have diabetes.
Scott Benner 1:26:29
I hope I can get a grandfather and I don't have Yeah, thank you. That's fine. Oh, listen, I don't want to be a bummer at the end here, because I have to go. But yeah, there's a lot of times that cash doctors are going to be they could end up being more valuable than institution positions. And, you know, it sucks to say that, because the idea is like, you know, keep trying. Do you find the one you want? But like, what do you do once you've tried the second one and the third one, you're like, This is just this ain't going anywhere. You know what I mean, especially if you're doing it for mental health, you're already not in a great place. And you're like, Oh, I tried one. I'm talking to him. This is valueless. Like, what if you would have kept going with the Kaiser dog? Kaiser doctors like and had a couple of more bad experiences. So yeah, there are bad
Speaker 1 1:27:07
doctors and good doctors in all the networks. So it's not like Kaiser is the only there's, I'm not saying there's anything inherently bad, but like, and in any of them, it's like, anyone that's good is not taking patients. You're like, great. That's not helpful to me. Well,
Scott Benner 1:27:19
that happens real quick. The good ones people find out about, and then they don't have a spare half a second in their life.
Speaker 1 1:27:24
Yeah. And also, they stay with them. They don't leave the doctors that have availability, like have openings, and like, this endo that they referred me to, I had an appointment the week after, which terrified me. I was like, you have an appointment in a week? I thought endocrinologist had, like, a long waiting list. I was like, this is kind of scary. That's
Scott Benner 1:27:40
so funny. You said that my wife was like, Hey, I we're looking for an ENT for Arden, like, when she was sick last week. And I said, I know where I'm going to take her already. I'm going to use the guy that just fixed my nose. I liked him, etc. And she goes, Oh. And I just talked to a friend of hers and her friends, like, oh, I have a friend who's an ENT. He can see her today. And I my wife's like, it's good news you can see today. I said the same exact thing. I think this is why you like the podcast, because, because you're skeptical like me, I was like, Why the hell has he got an opening today? Yeah. I was like, Does no one want to see him? And maybe I'm completely wrong, but stands to reason that the shelves that are empty at the grocery store, that's the stuff people like eating.
Speaker 1 1:28:12
Yeah, yeah. Well, I'll say my new window is really great, and I did have to wait a long time to see him, but he also spent two hours on a Zoom meeting with me on a Friday night setting up my trio. And that's awesome. I feel really lucky to have new, new
Scott Benner 1:28:27
people make sure his name's on my list Juicebox docs, if it's not there, sending me an email and I'll add them to it so people can go find him take up the rest of his free time.
Speaker 1 1:28:36
Yeah, and he is a pediatric and adult endocrinologist. Awesome, awesome. Awesome.
Scott Benner 1:28:40
That's terrific. Okay, well, Clara, I really appreciate you doing this with me. Thank you so much for sharing your story. All right. Hold on one second for me,
summertime is right around the corner, and Omnipod five is the only tube free automated insulin delivery system in the United States, because it's tube free, it's also waterproof, and it goes wherever you go. Learn more at my link, omnipod.com/juicebox, that's right. Omnipod is sponsoring this episode of the podcast, and at my link, you can get a free starter kit. Terms and Conditions apply. Eligibility may vary. Full terms and conditions can be found at Omnipod, Comm, slash Juicebox. I start every day with a delicious drink of ag one, and I'm ending today's episode by reminding you to go to drink ag one.com/juicebox. Subscribe today to try the next gen of Ag, one, if you use my link, you'll also get a free bottle of Ag, d3, k2, that freaks of nature, Sun stick a 30 day supply of Ag, one, five, free travel packs. I mean, there's so much in it. Just go look drink. AG, one.com/juicebox, you. You us. Med, sponsored this episode of The Juicebox podcast. Check them out at us. Med, Comm, slash Juicebox, or by calling 888-721-1514, get your free benefits check and get started today with us. Med, hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox podcast.
The episode you just heard was professionally edited by wrong way recording. Wrong wayrecording.com.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!