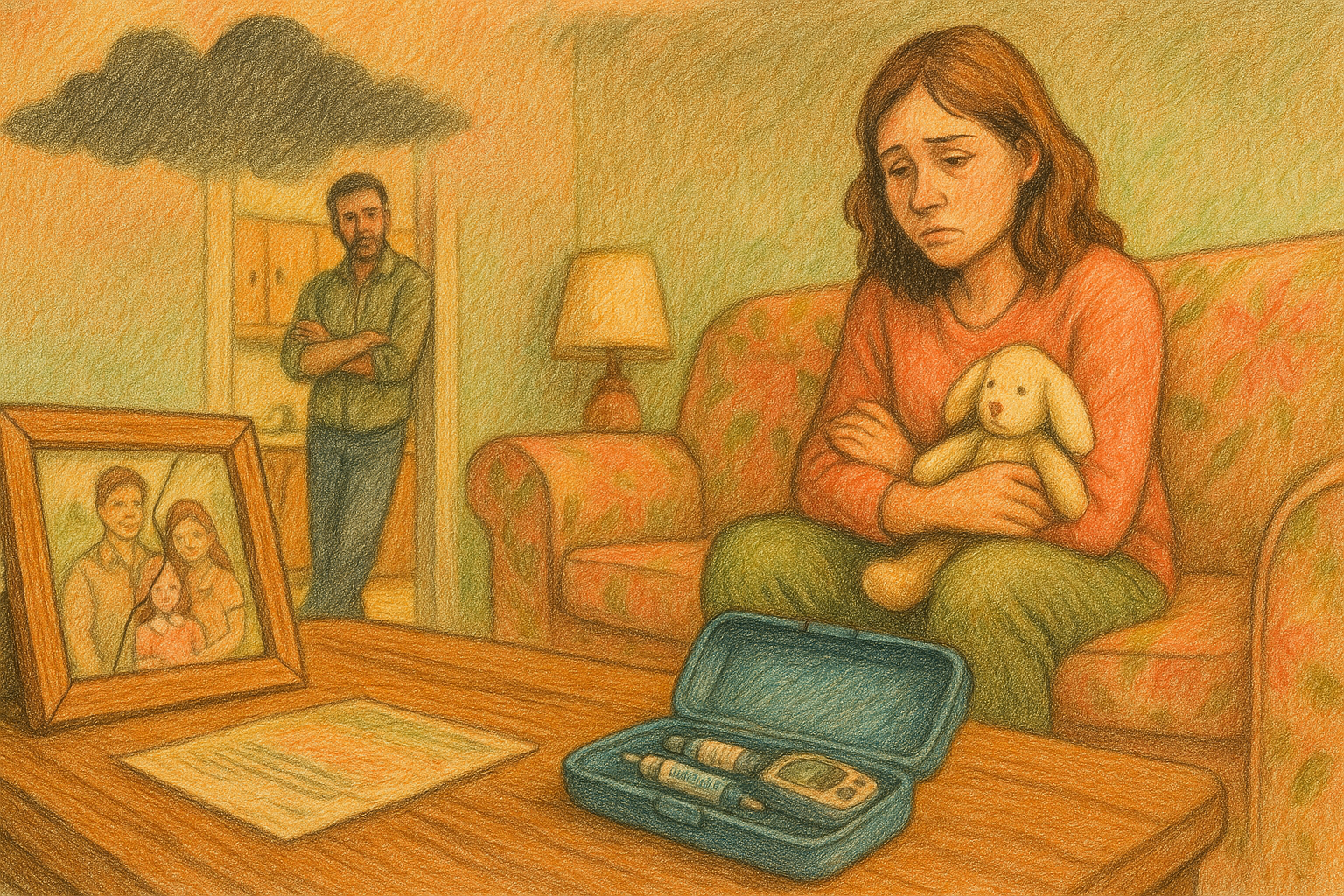
#1295 Alyssa and her Daughter’s Diabetes
Alyssa and her daughter have type 1 diabetes.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome to another episode of The juicebox Podcast.
Today, I'll be speaking with Alyssa. She's 30 years old, and she has type one diabetes. She was diagnosed at three years old. She also has hypothyroidism. Alyssa has three children, 12, three and six weeks old. Her 12 year old also has type one. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan when you place your first order for ag one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. Ag one.com/juice, box. Don't forget to save 40% off of your entire order at cozy earth.com. All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40% at cozy earth.com and if you have type one diabetes, or are the caregiver of someone with type one like Alyssa, go to T 1d exchange.org/juicebox, join the registry and complete their survey. When you complete that survey, Your answers will help type one diabetes research to move forward, you can do all of that right from your sofa in about 10 minutes, T 1d, exchange.org/juicebox
this episode of The juicebox podcast is sponsored by the Dexcom g7 made for all types of diabetes. Dexcom g7 can be used to manage type one, type two and gestational diabetes, you're going to see the speed, direction and number of your blood sugar right on your receiver or smartphone device, dexcom.com/juicebox, this show is sponsored today by the glucagon that my daughter carries, gvoh hypopen. Find out more at gvoke glucagon.com forward slash juice box. Hi, Scott.
Alyssa 2:08
My name is Alyssa. I am 30 years old. I'm a type one diabetic, and I also have a type one child. Okay.
Scott Benner 2:15
How old were you when you're diagnosed? I was three, seven years ago, yep, 27 years like starting a day off with easy math, your child. Your child has type one. How many kids do you have? I
Alyssa 2:28
have three kids. I have a 12 year old, a three year old and a six week old. Oh, my God,
Scott Benner 2:33
really? Yeah, yep. Which one has diabetes? Uh, my three year old, your three year old. Does any other autoimmune I
Alyssa 2:41
also have hypothyroidism, and then my husband has pulmonary sarcoidosis.
Scott Benner 2:47
Okay. When did he find that out? Actually, about
Alyssa 2:52
four or five months after our three year old was born.
Scott Benner 2:55
No kidding. What is that due to his life? So
Alyssa 2:59
he periodically has to get his lungs scanned and checked. He gets nodules in his lungs that could build up into scarring if it's not treated and taken care of. So he does periodically have to go onto like prednisone or other treatments
Scott Benner 3:13
I see working for him so far. Yeah, yeah. It's
Alyssa 3:16
been working pretty well for him. He gets scanned every once in a while. You know, if he starts to feel sick and stuff, he he'll get it more so in his chest, so he has to be careful, you know, when he gets sick, to make sure that he treats his lungs correctly,
Scott Benner 3:29
yeah, pulmonary sarcoidosis? Yep. I can't believe more people are saying sarcoidosis on the podcast.
Alyssa 3:39
Yeah. I heard an episode not long ago, yeah, talking about sarcoidosis. I was like,
Scott Benner 3:43
Get out of here. But that person said it was like, I know you're making this up, but they weren't, yeah, okay, all right, it is a rare disease. The cause is unknown. Yep, inflammation, I see they call it autoimmune, yes, yeah. All right, well, then there's maybe no wonder your three your three year old, got type one, right? Yeah. What about on your family side,
Alyssa 4:10
nobody else has diabetes. I did have, I guess, a great grandfather who maybe had type two diabetes, and that's about it. And on my husband's side, my mother in law also has type two, but no one, besides my daughter and I have been type one, no more, even thyroid, celiac. I've got some distant family members with thyroid, yeah, okay. And no, nobody has celiac.
Scott Benner 4:32
Just interesting to see how the tree grows, you know? Oh, I
Alyssa 4:36
know. And I know, once you know you have one autoimmune, you're more likely to get another one. So I didn't actually have issues with my thyroid until after or during my pregnancy with my
Scott Benner 4:45
three year old during during it, it popped up at first. Yeah, yeah.
Alyssa 4:49
So I had to take some Synthroid while I was pregnant, and then after I delivered her, I actually had an overactive thyroid, and they thought I had Graves' disease. Yeah, but it turned out that was not the case, and I ended up, my thyroid ended up not producing what it was supposed to, and I ended up going back on Synthroid, and I've been on it since I see is it working for you? Yeah, yeah. I have not had any issues, you know, since after having her,
Scott Benner 5:14
great, that's excellent. And then you still had another baby, because yes, would you have a room open or something like that.
Alyssa 5:22
No, my daughter was diagnosed three days before her first birthday, and we had been talking about trying to have another baby, you know, before that, and then, unfortunately, you know, when she was diagnosed, we kind of said, I'm not sure, not sure if we're gonna have any more. We'll wait and see. And we did. We waited a couple of months, and then we started having that conversation again. And of course, like a weight, heavy on us, you know, if we should or should not have another child. Because, of course, you know, we were worried that if we have another child, you know, someone don't also have diabetes in our family. But we did end up trying to have another baby. And unfortunately, we did have a miscarriage at the beginning of the year last year. Oh, I'm sorry, yeah, and then, but we ended up about within two months later, getting pregnant with our son, who was just born six weeks
Scott Benner 6:07
ago. Okay, well, congratulations, and You named him Scott, I imagine,
Alyssa 6:12
no, his name is Elias, all right.
Scott Benner 6:14
Well, that's fine, okay, that's lovely. Good for you. Congratulations. Very nice. Thank You that we done, or we want more kids? No, we're done. Yeah, I don't know how you're paying for these three, but good luck. Yeah,
Alyssa 6:28
no, we are done. We went back and forth, but, uh, I ended up getting my tubes removed when I had him by
Scott Benner 6:33
hand. Did you just kind of reach in and go like, hey, while you're in there, let's get rid of these. Okay. Well, when
Alyssa 6:38
you So, when you have a planned C section, they give you, you know, the option if you would like to have your tubes tied or tubes removed. And so we kind of went back and forth, but we were like, No, we're definitely, we're definitely done three. Three is a nice handful. What
Scott Benner 6:50
was the, what was the benefit of removal over time?
Alyssa 6:53
So it was our doctor explained it. He they just removed them. Now, I guess, I guess it's easier. I don't really know what the benefit is, necessarily. But he said, rather than tying them, that it was just easier to remove them for him or you. I mean, it might, it may, it may have been him. I don't really know. I'm going to be honest though, I don't really know the difference. How
Scott Benner 7:13
about that? No side, like, there's no like, like, you're not going to grow a mustache now or something like that. Or like, no,
Alyssa 7:19
no, I still have my I still have my uterus, my ovaries, so, yeah, so I don't know.
Scott Benner 7:23
I don't know what all those things do. So that's why I'd ask questions, right? I understand how to get to them and everything, but after that, I'm a little lost. Okay, so you were diagnosed at three years old. I was Do you remember anything about growing up with type one?
Alyssa 7:39
Yeah, mostly my growing up with type one is very different than, like, what my now daughter is growing up with, because I was on shops for a very long time, and I didn't get a pump until I was 10 or 11 years old.
Scott Benner 7:51
Okay, and do you remember it as oppressive or just the thing you did?
Alyssa 7:56
It was tough. I mean, there was the insulin back then. Was also different, because I was diagnosed in 1997 so 97 so there was a lot of like, you have to eat this amount at this meal, you know, and snacks have to be this amount of carbs, not as much freedom for eating as I know today. You know, even on shots children have so definitely that that was definitely difficult. Was that regular in mph, or was, I'm gonna be honest, I'm not exactly sure remember, yeah, I don't, I don't remember I had to eat on
Scott Benner 8:24
a schedule, though. Yes, I did, yeah, it was probably that, okay, yeah. And then they moved you to a pump where they were probably, like, the insulins faster. Now we're gonna give you humologue, or something like that. Yes, yeah. So
Alyssa 8:34
I was on, I believe it was humologue, because I got a pump in 2005 it's very interesting. The way that I got my pump very different than today. My doctor had only prescribed one type of pump. So I'm going to be honest, up until a couple of years ago, like until I started doing my own research, I didn't even know about all the different types of pumps that were out there. I was put on a Medtronic pump, and they were like, That's what everybody in our practice gets. And so they actually had me and several other kids, we had a three day hospital stay. So in order to get the pump, I did have to stay in the hospital for three days where they kind of did, like, the initial pump training, like, taught my parents how to put the pump on me, like, how to actually do the dosing for it and calculate everything right.
Scott Benner 9:17
That's interesting. It was like, was, like, sleepover camp at the hospital, yeah,
Alyssa 9:23
yeah, it was. It is very interesting, especially, like, now, I mean, I'm in an OmniPod now, and, I mean, I did my own pump training, like, at home,
Scott Benner 9:33
I know, right? I used a YouTube video on the internet. It was fine, yeah,
Alyssa 9:36
yeah. I mean, essentially, I used a little manual and watched some of the videos on their website, and that was it, probably
Scott Benner 9:42
back then, though, there were a few people who could actually explain it to you, it was probably easier to bring patients to the information than vice versa. Yeah,
Alyssa 9:50
yeah. I have a feeling that's what it was. But like I said, we were all, I mean, all of us, there was, I think five or six of us that all were kind of doing the pump training and getting started on the pump together. There, and we all had the same pump,
Scott Benner 10:02
okay, yeah, because that's, that's the one they gave you, that's the one they gave us, right? And did that actually make your life? I mean, usually what people say is, I didn't have to eat on a schedule anymore, and that was a big deal. That
Alyssa 10:13
was the biggest difference, was not having to eat on a schedule, or, like, not having to eat if I didn't want to eat, which was nice,
Scott Benner 10:19
yeah. Can you talk about that a little bit at being a child and being told, I don't care if you're hungry or not you're eating right now?
Alyssa 10:27
I mean, it was definitely very difficult. It made me like as a child. I mean, not want to eat. I mean, the typical, you know, kid wanting control. It made me, you know, not interested in eating. There was probably some bribery on my parents part, because they needed to make sure they'd already given me the insulin they needed to make sure that I ate it, right? I know that was definitely probably hard for them too, especially now that I'm a parent of a type one. Yeah,
Scott Benner 10:50
I was gonna say now you understand it from both sides, right? Yes, are your parents definitely alive? Yes, they are. They are. Do you know was it difficult for your mom specifically or dad, that your child got type one. If you take insulin or sofony ureas, you are at risk for your blood sugar going too low. You need a safety net when it matters most, be ready with G vo hypo pen. My daughter carries G vo hypo pen everywhere she goes, because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that, I trust low blood sugar emergencies can happen unexpectedly and they demand quick action. Luckily, jivo hypopin can be administered in two simple steps, even by yourself in certain situations. Show those around you where you store GEVO kypo pen and how to use it. They need to know how to use jivo kypo pen before an emergency situation happens. Learn more about why GEVO kypo Pen is in Arden's diabetes toolkit at gevok, glucagon.com/juicebox, gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma, or if you have a tumor in your pancreas called an insulinoma, visit gvoke, glucagon.com/risk, for safety information. You can manage diabetes confidently with the powerfully simple Dexcom g7 dexcom.com/juicebox, the Dexcom g7 is the CGM that my daughter is wearing. The g7 is a simple CGM system that delivers real time glucose numbers to your smartphone or smart watch. The g7 is made for all types of diabetes, type one and type two, but also people experiencing gestational diabetes, the Dexcom g7 can help you spend more time in range, which is proven to lower a 1c The more time you spend in range, the better and healthier you feel. And with the Dexcom clarity app, you can track your glucose trends, and the app will also provide you with a projected a 1c in as little as two weeks. If you're looking for clarity around your diabetes, you're looking for Dexcom, dexcom.com/juice box. When you use my link, you're supporting the podcast, dexcom.com/juice box. Head over there. Now
Alyssa 13:19
I'm not I think for both of them, it was definitely very difficult, you know, and even now, you know, we all have those moments, you know, where I feel like, Oh, I can't believe this. I'm, you know, super frustrated. Or, you know, something feels not fair. You know, my mom definitely is the one that I talk to, you know, because she, as a mom, also understands, yeah, that that feeling.
Scott Benner 13:39
How many kids did your mom have?
Alyssa 13:42
Just me,
Scott Benner 13:43
just you okay, oh, yeah. Then she just, probably, I'm trying to imagine 10 years from now, Arden telling me that her, her three year old, has diabetes, you know,
Alyssa 13:52
yeah, yeah. And definitely, I mean, when, so, when she was actually diagnosed, you know, the morning of, I mean, I called my mom in a panic because I also have a 12 year old. We knew we were going to take her to the hospital, obviously, but I needed somebody to come take my older daughter. Yeah, and definitely, that was a hard phone call to make. I mean, I'm going to be honest, I don't remember what I even said to her, because in that moment, I feel like we went into survival mode of we have to get to get to the hospital.
Scott Benner 14:20
How did you figure out that the hospital is necessary?
Alyssa 14:25
My daughter had been soaking through diapers, you know, overnight, because she, like I said, she was less than a year old, she'd been soaking through diapers overnight, like waking up frequently, which was unusual, because at that point, you know, she was almost a year old. She had not been waking up during the night frequently before that, but she started waking up super fussy during the night. You know, I figured maybe she's going through a growth spurt, you know, again, she's peeing through diapers. So we sized up in the diapers, thinking like, oh, maybe the diaper is too small. And, you know, it's just she's not able to hold everything. She was diagnosed on a Saturday that. Friday, I went to pick her up from my mom's house, because my parents watch her when she's not at preschool, and she was very thirsty, very fussy. You know, she had kind of been getting sick on and off, so I thought maybe she's getting sick again. I don't know. She came over to me and I hugged her, and I like smelled her breath. I know a lot of people say they smell a sweet smell. I didn't smell sweet smell. I almost smelled like acetone.
Scott Benner 15:23
Yeah, that's the other thing. Some people smell it as sweet, and some people smell it that way. It's just, it's the ketones, right? So, yes,
Alyssa 15:31
yeah. So I said to my mom, was like, Do you smell something on her breath? Like, do you, do you smell that? And she was like, No, I don't, I don't smell anything. And I had been worrying, obviously, as she would be, you know, getting thirsty and thirstier, I'd been worrying, and her one one year appointment was coming up, and I was going to bring it up to her doctor. But I didn't, I didn't truly think at that age, you know, that that would actually be possible,
Scott Benner 15:53
even though you were, even though you were three, yeah. I
Alyssa 15:57
mean, I figured if she was diagnosed, that maybe we would have more time before she was diagnosed. Maybe
Scott Benner 16:02
was that hopeful? Or,
Alyssa 16:05
I think, I think it was hopeful that that wouldn't be the case, I see, because I, I definitely had a feeling. And so we went home, you know, that night, she was still super fussy, and when she woke up in the morning, you know, she had peed through her diaper, and was, you know, her whole bed was wet, like I looked at her face and like, now, of course, looking back, I know they say Hindsight is 2020, like looking back when I looked at pictures of her face, like her eyes almost looked like sunken in. And I don't know how I didn't like see it in that moment, but my husband had left with our older daughter, because it was her, you know, almost her first birthday. We were doing a little smash cake at home. I had my husband go get the cake that I had ordered from the store while he was gone. You know, she was thirsty, so I gave her a cup of water. She downed the whole cup of water in 30 seconds, yeah. And she was just crying, like, very fussy. And I was like, this is very unusual. And so when he got home, I was like, I have to just take her blood. Like, I'm probably wrong. I'm probably being ridiculous, but I will just feel better if I just take it and make sure that I'm, you know, being ridiculous, right? And we took it, you know, we went into our room and took it, and it was over 500
Scott Benner 17:16
so then that's the moment you we knew. You call your mom and you're like, I've got to go to hospital, and all this is happening. But it happened to the onset was pretty quick, though, right as far as length of
Alyssa 17:26
time to say, Yeah, I mean it, it felt like it was, we had covid Back in December before she was diagnosed. And I feel like kind of that whole, like, 30 to 40 days after, was when we started seeing, like, diapers, being soaked through, getting fussier, waking up during the night. And then she did have days where she was like, super duper hungry, and then other days where she didn't want to do anything.
Scott Benner 17:51
Yeah, okay, well, that's about how it goes. So yeah. And then on eventful. Or did they do the thing where you have diabetes? So I don't have to teach you anything.
Alyssa 18:00
So her, when we got we live in a small town, I did not think about the fact that our small town does not actually have a children's hospital attached to the regular hospital. Yeah, I think because, again, when I saw that 500 number, like, I just panicked. And, you know, we went straight to our local hospital, you know, and I walked in and I said to the woman at the desk. I was like, I was like, you know, she asked why we're here, and I said, my daughter has diabetes. And they're like, Okay, she has diabetes. And I was like, no, no, she's going to be diagnosed with diabetes. I know she has diabetes. And they're like, how can you know that? And I was like, because I took her blood at home, and it was over 500 Yeah. And very quickly we were brought back, you know, to a triage room.
Scott Benner 18:39
We had the same exact confusion. What that that you went to the emergency we went in the ER, went up to the person's desk, and they said, Hey, why are you here? And we said, Our daughter has diabetes. And then they stare at you because you don't think about it like from the perspective of people who have diabetes who also end up in the emergency room. No. And then there's that pause where everybody's mind works for a second, and then one of us goes, Oh, no, sorry, we're diagnosing her right now with type one. Yes, yeah, it's exactly, it's exactly what happened to us. And
Alyssa 19:07
they kind of were like, Oh well, it could be something else. And I'm like, no, no, I have type one, and her blood sugar was over 500 it's not anything else. Yeah. It's like, I know. It's not Well,
Scott Benner 19:17
it's good because it saves time, and it also keeps them from tripping down other roads, which you hear people's stories all the time that that happens, you know,
Alyssa 19:25
especially of like, sickness, the flu, yeah, oh,
Scott Benner 19:29
it might be this. Let's check this first. And you're like, can you just check their blood sugar?
Alyssa 19:33
And that's the thing. So when we actually got back to the room, they're like, well, we need to check for all these other things. And I'm like, you can check for whatever you want, but this is, it's diabetes. Like, I know what it is. She's probably a DKA,
Scott Benner 19:44
yeah, yeah. Stop, stop looking around. It's right here in front of us. Yes. So we have protocols, yes. Well, have you been listening to the cold wind episodes? I have been Yes. Well, then you know what's going on. Yes,
Alyssa 19:57
I do. And, like, truly, I'm not surprised. Surprised about some of the things that I hear on those episodes. Unfortunately,
Scott Benner 20:03
yeah, me too.
Alyssa 20:04
I mean, like, I said, we went back and they were like, well, we have to test for all these other things too. And I was like, you can test for whatever you want, but it's diabetes, and she needs, like, she needs to be put She needs an IV. Like, we need to, we need to get moving. She's little. Let's
Scott Benner 20:19
go, yeah. I
Alyssa 20:20
mean, yeah. I mean, she was less than a year old. She was 20 pounds, right? Check
Scott Benner 20:24
her blood gasses, at least, before you start talking about other things. You know
Alyssa 20:27
the problem? The problem was in our local hospital, because they do not have a children's hospital. They really are not trained well with pediatrics, so they could not get an IV in her to get fluids in her or get anything started. Did they move her then she ended up taking a helicopter to our children's hospital that's about an hour away. The problem is, though, is like to get that started. I mean, we were in the local emergency room for probably about five hours by the time that they were actually able to get the crew to our hospital and back to the other
Scott Benner 21:02
hospital you live in, Mayberry or something. Let's go.
Alyssa 21:06
We live in a very small town in North Carolina. Gotcha
Scott Benner 21:08
pretty far from other things. Yeah, yeah. I
Alyssa 21:12
mean, we're, we're about a couple hours from some of the bigger cities I see. So unfortunately, you know, like I said, I if I like, now, knowing what I know now. Like, whenever we have to to go to the emergency room with any of our kids, we don't go to our local one. We go to the one with the Children's
Scott Benner 21:26
Hospital. Yeah, because they probably Alyssa, they probably had to sober up the crop duster pilot to get them into the helicopter, and that probably took hours to coffee and water, walking them around and
Alyssa 21:35
everything. My husband and I though we were like, we were, I mean, we were super frustrated, because we were like, listen, I understand it's very difficult to get an IV in her. She's really dehydrated, we know, but somebody has to be able to do this. Is there no one here that can do it? I mean, there were several people that tried. They tried seven times to get the IV in the arm. Oh, my
Scott Benner 21:53
God. I wonder, what else I wonder, what else they can't do? That's what I would be wondering, actually.
Alyssa 21:59
So the only people that were able to actually get the IV in, and this was the only IV that stayed in, like, throughout her whole hospital stay, even at the Children's Hospital, was the flight crew. When they got there, you know, they saw she didn't have any IV, and they were like, we can't take her up without any IV in her and so they were able to get one in her foot. That was the only place that they were able to actually
Scott Benner 22:19
keep one in. So not an undoable thing. Just you needed the right person to do it. Yes, yeah, gotcha, yeah. Well, how much was that helicopter ride? By the way,
Alyssa 22:28
that was a whole nother thing. So obviously, after everything was said and done, we were back at home. We had gotten a letter from insurance that they were that they didn't want to cover. Here we go. Wait. I was like, Oh, my God, what do you mean? You don't want to cover it. And I was like, I know my insurance does cover air ambulance. So in the end, we did. We paid it. We paid a small deductible. It wasn't terrible.
Scott Benner 22:53
It was $25,000 or anything like that. No, our poor our portion ended
Alyssa 22:57
up being about 200 What did they
Scott Benner 22:59
want from you? It was, I mean, it was, well over 2000 Oh, 2000 that's not bad. Well, I guess, though they did the crops at the same time they were going to the hospital. So it's probably like, like a ride share, almost, right? Yeah, it was,
Alyssa 23:10
I mean, I mean, what they what, like, the original bill, I guess that they were going to send us was 2000 I'm sure what insurance was willing to originally cover was probably more than that. But what our end was going to be was about 2000 we were like, No, I don't, I don't think that's because I actually had to look more into my insurance policy after that, like, as to how much is actually covered?
Scott Benner 23:30
Well, now I'm wondering if how they price these things, because they're people on here that were charged 10s of 1000s of dollars for life flights.
Alyssa 23:38
Yeah. I mean, like I said that it could have been more the bill that I had gotten finally got to you, yeah, yeah, by the time it got to me, would have been about 2000 gotcha. Oh, which is not what we ended up paying. Yeah. Oh, that's interesting. I don't know how much it was before insurance. I'm going to be honest, I
Scott Benner 23:54
don't remember a lot. I bet probably I like, how people are, like, it's all worth it. I'm like, oh, Jen has a lot of money
Alyssa 24:00
well, and so it was taking so long to get the the air ambulance that I was like, what if we just, like, take a regular ambulance? It's, it's an hour away, yeah, like, the time that we spent waiting here. And they were like, well, if something happens on the road? And I was like, but
Scott Benner 24:15
what if something happens here? You people are inept, but that's the thing. I'm like, what if something happens here? Nobody
Alyssa 24:20
can get an IV in her. Yeah,
Scott Benner 24:21
why don't we just take one of your inept nurses and put them in this the Winnebago, and we'll head over. Like, I mean, that's very interesting.
Alyssa 24:28
Yes, yes. And I'm like, I at this point, I'd almost prefer regular ambulance, because at least we'll get there, we're moving Yes. And there's nothing more irritating to me than staying stagnant. So I can't just sit here.
Scott Benner 24:39
That's really something okay. So we've get the diagnosis. We go the hospital. She's obviously okay because she's home, she's doing well, yes, I want to kind of fast forward a little bit to the juxtaposition between what you were accustomed to growing up, what you know now as an adult, and then what you learned you know subsequently from from this. So we. Know what it was like for you growing up a little bit. We know you got a pump around 10, but was a pump just a way not to use shots? Or were you being thoughtful about it? What were your a one C's through your 20s, and where are you now? As
Alyssa 25:13
a child, I was very frustrated with the shots, and I was done with them, so definitely, the pump was a way to not have to take shots anymore and to have more control over, like, what I could eat, what I did or didn't have to eat, that was kind of what it was for as a teenager and as a young adult, definitely like what I know now very different, because my control with a pump is so much better than it could have ever been with taking shots. Okay, I'm gonna be honest. I don't know what my ANCs were as a child. They were probably in the lower sevens as a child. But now, as an adult, especially now as an adult who's had several children, my ANCs are now sitting in the fives with a pump.
Scott Benner 25:53
Oh, wow, that's great. That's with OmniPod Yes, yeah. So
Alyssa 25:57
I was on omnipodronic Up until my daughter's diagnosis, I had actually inquired with my endocrinologist about an OmniPod, because, again, I didn't really know much about other pumps. I didn't know about other pump types because I'd been on a Medtronic, you know, for most of the time that I was on a pump. Yeah, I didn't mind the tubing, of course, because to me, it was still better than shots. I definitely was interested in OmniPod because they were tubeless. And so I inquired with my endocrinologist, and I ended up right before she was diagnosed, like, two weeks before maybe getting, like, the kit that comes with the PDM and, like, the one month sample, right? And of course, it came, and I was like, I don't know why this is coming. I didn't really, you know, I just thought about maybe looking into it. I don't know that I really want to switch. I don't know that I'm ready, mainly because I think I was worried about changing to something new, yeah. And right before, actually, the night before, two nights before she was diagnosed, that's when I put on the first OmniPod and, like, actually programmed it and tried it, wow. And yeah, and it was, I mean, it was great. I definitely loved having no tubes like that was that was the biggest positive of changing from Medtronic to OmniPod. Once my daughter was diagnosed, I ended up going back to my Medtronic for a short
Scott Benner 27:09
time because you knew it well, and you felt overwhelmed. No,
Alyssa 27:13
because when we were in the hospital, when she was diagnosed, we were when we were actually in the children's hospital, she was in the PICU to start, and then when we were moved to the pediatric floor the morning that we were going to get discharged. You know, we had been giving her shots, but her blood sugars were still, you know, in the three and four hundreds, even with shots, because she was so small and her doses were so small, but an insulin pen can't get doses as small as someone that tiny would need, right? So she would be eating a meal and not getting an insulin for it, because she wasn't eating enough carbs to technically get insulin for it. Yeah. And so that morning, I woke up and my parents, they live pretty close to us. I called my dad, and I was like, I need you to go to my house, and I need you to get my Medtronic supplies. I need you to get all the stuff. And he had helped me with the Medtronic pump as a child, so he knew exactly, you know, which supplies I'd need. And he's like, why do you want your pump and all that other stuff? And I was like, because I need to put the tubeless pump on Jillian. I need to, she needs to be on a pump. She can't be on shots. She's too small the doses. I can't make the doses small enough, and she won't eat enough.
Scott Benner 28:22
So you gave her the and they let you do that. That all was okay. So no, I was gonna say that doesn't sound right, but go ahead. No. So,
Alyssa 28:32
so that morning, you know, she was taking they were giving her her long acting in the morning when she first would get up right before breakfast or right after breakfast. And that morning, we woke up and I was like, You're not giving her her long acting. My dad, you know, is on his way. He's bringing me my tubed pump. I'm gonna take off this pump right now. We're gonna change the settings in the PDM and make it so that it's applicable for her. And they were like, well, you can do that when you go home. And I was like, No, I'm not doing it when we go home, and if you give her that long acting insulin, I can't do this until tomorrow, because that long acting insulin is supposed to act for 24 hours, yeah? And I was like, I'm not waiting until tomorrow. I'm not giving her shots for the rest of the day. Today, we're going to put a pump on her. That's not, you know, hospital that's not hospital policy, not protocol. And I said, I don't care.
Scott Benner 29:19
That's very good, and you got it done? Yeah. I mean,
Alyssa 29:22
they were definitely, there was a lot of pushback, because they were like, once, you know, once you do that, you know, none of the nurses will come near her. They will not touch anything with pump. I was like, that's fine. I don't want
Speaker 1 29:31
them to, oh, different, scary. Yes, different, yes. I
Alyssa 29:35
mean, that they were like, they're like, We don't, we don't, you know, the the staff here doesn't know how all the different pumps work. I was like, that's fine. I know how this works, yes. So
Scott Benner 29:44
I got Google. I'm all good, thanks. Like, no, don't get
Alyssa 29:47
me wrong. Like, she's tiny, and her doses obviously were much smaller than mine, right? So I needed help as far as making sure that I'm programming it correctly and making sure that I have the correct basal rates in but I. As far as, like, being able to give her insulin or being able to calculate carbs, like, that's nothing new for me. Yeah, so that's fine if they don't want to touch it. And we were going to be discharged that afternoon anyway. So I was like, No, and we waited, and, you know, my dad got there, and they were pushing back because, you know, we'd passed the mark from the day before, when she'd gotten her long acting insulin. So they were like, if we keep waiting, you know, her blood sugars are going to go up. I'm like, I understand that. We're going to put the pump on her. You are not giving her that shot. Yeah,
Scott Benner 30:30
nice, you dag out there. You put it on, and she's been wearing, she's been wearing one ever since, ever since. Yep, do you recall what her starting basal rates were?
Alyssa 30:39
I think we started off as just like, is either point 05 or point one per hour. We might have done alternating. She was on, like, an extremely small amount. I mean, she was already, she was also much smaller than than she was now. She was on an extremely small amount at the beginning. And we kind of just started her as basic of a level as possible to figure out where we needed to go from there. Yeah. And her endocrinologist, you know, is wonderful. She she was in the hospital that day, and I in the middle of this back and forth with you can't put a pump on her here. No, yes, I'm going to. I definitely yelled at her endocrinologist, and later apologized.
Scott Benner 31:14
Why'd you apologize?
Alyssa 31:17
Because I probably should not have yelled at someone, but in that moment, like I felt like I was not being listened to, so I felt I needed to yell,
Scott Benner 31:26
I hear you. I hear you. Well, nice of you to apologize, and they weren't listening to you either. Is that right? No,
Alyssa 31:31
but my daughter's endocrinologist, actually, she has her own children with diabetes, so she was like, you don't need to apologize to me. Like, I understand, I understand
Scott Benner 31:40
why? Oh, that's really lovely. Actually, that's, yeah,
Alyssa 31:43
I her endocrinologist. That's, she's been her endocrinologist since that day, and we love her. How do you know about me? So after my daughter was diagnosed, I did join a couple of groups on Facebook, of, you know, moms and dads of kids with type one, and I had been seeing the juicebox podcast to come up a bunch of times. I saw, you know, tagged a couple of times. I think I'd posted about my daughter once or twice, and somebody had put that recommendation in there. I ended up taking some time off of work after she was diagnosed to kind of get a hold of everything that was going on in our lives. And while I was home with her, I ended up starting to listen to the podcast when we were in the hospital. And obviously the days after, you know, her numbers were very up and down, definitely running a lot higher than even I was comfortable with as a type one. And, you know, they kind of said, like, Oh, she'll, you know, she'll run higher. It's okay if she runs, you know, at 200 or above 200 having, you know, been pregnant with her, you know, a year before. Obviously, I hear 200 and I'm like, OmniPod, that's so high, right? What do you mean? It's okay if she runs, you know, her target was 250 I'm like, What do you mean, her Target's 250 that's so high. How can that be? I was definitely afraid because of, you know, the education, of course, that we still, we still did get some education in the hospital. I was, you know, afraid of giving her too much insulin, because I did not want her to go low or go too low. And so I started listening to some of the very earlier episodes, you know, both with insulin, things like that. And I started listening to some of the things that you were saying. And I was like, well, this, this makes sense. This. Why would I want her to run higher? I wouldn't want that for myself. So just because she's a child, it doesn't mean that she should be running high. Did they ever
Scott Benner 33:28
tell you why they set the targets that high? No, I
Alyssa 33:32
have a feeling, personally that it has to do with you know, if you do have somebody who does not have any background knowledge, you know, I understand in the beginning, maybe it's safer to run higher so that you're not overdosing on insulin. As someone who does have background knowledge on how insulin works, I definitely felt it was way too high.
Scott Benner 33:52
Was there any honeymoon for her at all? Slightly like
Alyssa 33:56
she definitely needed a lot less insulin during the first like six months to a year, okay?
Scott Benner 34:01
But no, no. Like, wild swings. Like, need a bunch. Don't need it. Like, didn't go back and forth. Oh, that's nice, actually. No,
Alyssa 34:08
no. And that's the thing. Like, I know that they did, they did talk to us in the hospital. They're like, well, she could go through a honeymoon, and it is kind of nice when she does, because then she won't need as much insulin. And I'm like, I don't feel that's nice, because then I'm going to be giving her, you know, a normal amount of insulin, or what I think is a normal amount, normal amount of insulin, if she's still producing some insulin. Yeah, can be way too much. There's
Scott Benner 34:26
no indicator light on your forehead that says not so much today. Yeah, no.
Alyssa 34:30
So, I mean, I know that a honeymoon period, I guess, can be good, because you don't have to take as much insulin, but you don't know it until after you've already given it, till
Scott Benner 34:39
you've taken too much insulin. Yes, and you're trying to get a you're trying to get a two year old to eat,
Alyssa 34:45
yes, and honestly, like, that was our, that's has, I mean, even, even now, has been our biggest challenge is, like, making sure that she eats to cover what we've already given her. Yeah,
Scott Benner 34:55
did you breastfeed? I did not. Okay, so that wasn't an issue with it. Yeah. Know,
Alyssa 35:00
but she at the time, I mean, she was still, like I said, it was three days before her first birthday, she was still drinking from a bottle, and she still had formula. Yeah, calculating those carbs are kind of complicated, yeah,
Scott Benner 35:09
I know they when people talk about trying to calculate for breast milk, it sounds like they're going crazy while they're talking about it. And, you know, yeah, no way to know how much. Not imagine,
Alyssa 35:17
I cannot imagine trying to calculate the carbs because it was hard enough on formula where, you know, we looked up the nutrition facts, but the way formula reacted in her body, and the way it was absorbed in the body was not necessarily even the same as regular milk. Yeah, that interesting, yeah. I mean, and we did see a difference when we switched, because obviously, soon after she turned one, we started switching to whole milk. But we, and we did see a difference. But the formula, I mean, the the way it would spike her blood sugar, was kind of crazy, right?
Scott Benner 35:45
Yeah, oh, I hear you, but you made it. Do you feel like you made it through that? Do you feel like that part's over now? Yeah?
Alyssa 35:51
I mean, I definitely feel like, you know, those first honestly, like the first six months probably were the hardest. Okay, even being on a pump, being on a pump definitely made it easier. Because, you know, it was much easier to make changes, you know, to see things as they were happening. Yeah, definitely those first six months were very difficult because, you know, I mean, she was so little, she didn't necessarily understand the pump changes, taking off the pump, she, you know,
Speaker 1 36:18
getting poked all the time, right? You wear a CGM or no? Yes, I do. And did you put one on her?
Alyssa 36:24
Yes. So when she was a helicopter lifted to the Children's Hospital, we were not allowed to go with her. We had to drive separately, because, I guess it's insurance on their part, they had two nurses and her in and the person who was uh, right, driving the helicopter, flying the helicopter, sorry that we're in the actual helicopter with her, and we had to drive, you know, the hour, to the Children's Hospital. And while we were on the drive, on the way up there, I went online and started filling out the forms on OmniPods website, as well as dexcom's website to get the ball rolling with being able to get those devices for
Scott Benner 37:01
her, that's different when you understand what you're talking about, huh? Yeah, I
Alyssa 37:05
mean, and of course, you know, I saw on there, you know, it says approved for ages two and up. And I was like, well, she's not even one. Like, I don't even know if they're gonna let me do this, right, but, you know. And again, in that moment, I looked at my husband, and I was like, if they say that, you know, she can't have it because she's not two, and she has to be on shots for the next year. I'll just put my pump on her, and
Scott Benner 37:26
I'll take shots. And you're gonna do that, and you're gonna do the shots, of course, yeah?
Alyssa 37:30
I mean, I definitely would, yeah, and I don't like shots, but I would rather myself take shots than my child.
Scott Benner 37:35
Yeah, that's lovely, too. I think that people don't understand that, you know, it says, you know, for two and above, but that just means the FDA tested it for two and above, and then your doctor, your doctor, just writes it off label. And mostly that's okay. And yeah. And
Alyssa 37:53
so when we were in the PICU The following morning, one of the endocrinologists had come in, and she had talked to us, you know, about if we wanted to try a pump. And I was like, I already filled out the information on OmniPod. And she was like, Oh, well, you know, we were thinking maybe one of the tubed pumps instead, because those can get, you know, even smaller doses. And I was like, she's a year old. I really don't want her to have tubes. She's an active one year old. I don't a tube really would not be productive for her. She would end up pulling it out or ripping it out accidentally, rolling over. We
Scott Benner 38:21
were thinking that. She's like, Oh, was that? Is that what you were thinking? Yeah, here's what I was thinking in the car on the way over here. Already took care
Alyssa 38:28
of it. Thank you. Though, yes, she was like, she was shocked that we had already, like, filled out everything. I was just like, I didn't have a doctor's name to put on. I was like, obviously, like, I put my information on there. I didn't have a doctor's name, you know, at the time, because when we were traveling to the Children's Hospital, I had no idea who the doctors were. But doctors were, but I was like, you know, as soon as I get the information from them, I'll forward it to you, because I want this prescription put in as soon as possible. Wow. And it happened, huh? It did. I mean, she ended up getting a Dexcom because that was a Saturday. I think we had a Dexcom on her by the following, like, Thursday or Friday, like, we got the Dexcom pretty quickly. It's awesome, actually, by the end of that week. Yeah,
Scott Benner 39:02
now I'm excited when people find technology and information early on, because it just, it's such makes a big difference. Yeah, it's an easier path, and it's a healthier path, and really wonderful. Well,
Alyssa 39:12
that's the thing we knew. I mean, her ANC at diagnosis was a 9.1 which compared to some other stories that I hear like it's not as high as I guess it could have been, right? Yeah, it sounds like you got it pretty quickly, yeah? But I think she was, I mean, she wasn't DKA, so not, yeah, maybe because she was so little, it happened quickly. It did, yeah, I think so. And, you know, we did get her ANC down pretty quickly with
Scott Benner 39:38
the pump. It's beautiful. What did you learn for your or maybe you didn't, but like, has her diagnosis changed? Anything about how you take care of yourself?
Alyssa 39:47
I feel like it reminds me that even when I am not pregnant, I need to make sure that I am taking care of myself as well. Obviously, you know, before I got pregnant with her and then. While I was pregnant with her, and then while I was pregnant with my son, definitely had, like the best control, because I knew how important it was. But even on, you know, in between having children, or even now at postpartum, like definitely a priority to make sure that my numbers stay in range as well.
Scott Benner 40:16
I'm doing a little math here you were young when you had your first right? So
Alyssa 40:20
my first daughter is actually adopted. Oh, she is biologically my husband's daughter, and I adopted her in 2020, Oh,
Scott Benner 40:27
I see so you, you've given birth to a three year old and a six month old. Yes, 12 year old, six week, six week old. Oh, six week Geez. Yeah, my brain doesn't work in those small numbers like that. All I know is I see a 12, a three and a six written in front of me in descending order, and my brain's like, why is the six not above the three? So she's not yours? Biologically, biologically.
Alyssa 40:49
No, no. So no. So my husband and I, when we started dating, she was just under two years old. And so once we were able to we got the adoption process started. Unfortunately, covid pushed adoption process back a little bit. But my
Scott Benner 41:03
point is, is that you so you live for 24 years before being pregnant with diabetes? Yes, and you don't remember when you were younger, that's fine, but what was your management like, and where were your numbers? Young Adult? Yeah, young adult and etc.
Alyssa 41:19
So definitely, when I was in college, I mean, I did not pay attention to diabetes the way that I pay attention to it now, I definitely did not make it a priority. Even when I first got married to my husband, did not make it a huge priority. I don't, I don't really have a reason why, other than it had always been a part of me, and I was just kind of like, oh, this is another thing, another thing we have to deal with, but definitely, you know, once we got married, and once, especially once we started talking about possibly having children in the next few years, that's when I was like, Okay, we really need, you know, I really need to have better control. I was not on a CGM for a long time, and once I got on a CGM, that kind of made the huge difference for me, in my control, what
Scott Benner 42:01
what did, what changes? So, yes, you have a CGM and that, and that helps. But like, I mean more like, daily steps, attitude, like, what kind of stuff shifts there when you go from, I'm just gonna do this, because it's the thing I do to I need to do it really well.
Alyssa 42:18
I definitely think the conversation about wanting to have kids, definitely the way that I looked at numbers, the way that I looked at food, and started doing things like pre bolusing, I had not really done that much as a young adult, but once I knew, you know, that I wanted to have children, and I knew the type of control that had to that I had to have in order to have children, that's when I realized, like, okay, even if I don't really want a CGM because I don't want another device on my body, I have to have that device on my body because I have no idea what's going on in between meals. I wasn't really taking my blood in between meals. Yeah?
Scott Benner 42:51
So you understand that it's necessary to be pregnant? Did you also understand it was necessary for your good health? But just ignored that part of it kind
Alyssa 43:00
of, yeah, and especially as a young adult, I didn't really think too far into how's this going to look 30 years from now for me.
Scott Benner 43:09
So knowing that that was your reaction, is that something you're already thinking about for the baby? What do you mean for your three year old? Do you like, wonder if that's going to be her attitude when she gets older? And like, how do you work with that? I
Alyssa 43:21
do sometimes, and I definitely we are. My husband and I both try to keep positivity, as far as you know, especially when she's not interested. She doesn't want her blood sugar taken, or she doesn't want to do a pump site change things like that. We talk a lot about being healthy, not necessarily like, I want her to know the way we're trying to keep her healthy now is something that I want her to carry into, you know, when she's a teenager, young adulthood, for her overall health.
Scott Benner 43:50
Yeah, I think that's really valuable, actually, just to keep that message up, this is what we do because this is what we want. This is why we want this. Yes, this is what we do, you know, and then just over and over again until, hopefully it becomes part of her.
Alyssa 44:07
I hope so. I mean, she definitely, I mean, even at three, she definitely is not happy about pump site changes and Dexcom changes, but we've she started becoming more involved in them, like when I change my pump, I have her help me when it's time for her to take her old pump off, because that's the part that she doesn't like. We help. We have her help, like, pull it off and take the patch off with her. Yeah, that's
Scott Benner 44:28
got me. It's all you can do. It's very slow. It's a very, very slow process. So yeah, and will she, well, how about you? Are you using an algorithm?
Alyssa 44:37
So I, she and I are both now on OmniPod five. I have not been using the algorithm, mainly because while I was pregnant, I it didn't get me in as tight of control as I needed to be, right? And so being postpartum now, I'm also not using auto mode, just because postpartum is definitely very difficult on blood sugars. Yeah, I was taking a lot of insights. One by the end of my pregnancy, and so using auto mode until I get my settings my manual settings correct to me does not feel very beneficial.
Scott Benner 45:08
So are you are you very sensitive right now, or do you need more
Alyssa 45:13
so right after I gave birth to my son, definitely very sensitive those first like two to three weeks now, I'm seeing over the last two weeks or so that I'm needing more insulin here and there, like for food,
Scott Benner 45:26
heading back to where you were before pregnancy. Yes, okay, all right. Well, I say, do you imagine you'll go into auto mode?
Alyssa 45:33
I would, yeah, I definitely would like to, because my daughter is in auto mode most of the time, and it really does work very well for her, so I know eventually that I would like to I just like I said, I want to get those settings correct before I switch to that reasonably
Scott Benner 45:47
stable too. Yes, back to normal, I guess, yes. And but for her, you like it a lot.
Alyssa 45:53
We love it. We like I said, we started on the dash back when she was diagnosed, because the five wasn't out yet. Yeah, and I got the five the summer after she was diagnosed. I was 2022 and I started in auto mode. I really liked auto mode back when I was using it, and I knew that I really wanted her, but I believe it was that she wasn't using enough insulin, maybe when it first came out, that she wasn't able to get it right away by the time we got to, like, late 2022 or any little bit of honeymoon that we had, was kind of on the downward trend. So she was using more insulin, and we were able to get the five for her. And honestly, the five made the biggest difference in getting her ANC down and, like, her time and range greater during the day. Excellent.
Scott Benner 46:37
Oh, I'm glad. The reason I asked, and because the way we're talking about is, I just got back from visiting Arden on her spring break, and we were with her for a week, actually, like probably a solid seven days, and she's doing so well, you know, but there's just no doubt that the combination of an insulin pump, a CGM and an algorithm is a big part of why she's doing. Well, yes, you know, because of every time that you do that thing where you guess carbs and don't get them quite right, or you get, you know, really active, and don't think about it like all the stuff that happens that, you know, if you stop, and if you're listening to the Pro Tip series, you're like, Well, if you're going to exercise an hour and a half before you turn your basal down, like, like that. You're not really doing those things. Like, that's how you do it, but you're not doing it once you go, you know when you're living it. And the algorithm just, it just saves you over and over again. You know it just, it's constantly working on your behalf and trying so hard to keep you from being high and from being low. Arden's gonna come through college having a slightly higher a, 1c while she's there than she would at home. But, I mean, she's gonna have a low six A, 1c eating college, you know, eating at college, college food, yeah, doing her thing there. You know, cooking for herself sometimes, but then for three days in a row, just like, you know, during her finals. I think she DoorDash during her finals, like five days in a row, and, you know, like, that stuff's all happening, and she's gonna come out of college with like, a six two, probably this year. I think that her great, yeah, her first year as a freshman, she swung a six four while she was by herself. And then she comes home and it goes down just when, you know the food gets better and you're get some stability to your day, right? And then this time she went back, and it's a little lower. In fairness, she's taking a GLP medication now too. So she's using, uh, less insulin. Her hunger is not exactly the same because the GLP, you know? So there are other impactors, but at the same time, who cares? Like, like, it's helping her, and she's helping her. Yeah, it's amazing. And your kids, you know, she's three, so 15 years from now, I'm hoping it, you know, the OmniPod five algorithm, or whatever else exists, is better and better. And you know, hopefully the sensing technology is better and allows the algorithms to be more aggressive. And, you know, that's what we're hoping for, because that's what I hope to Yeah, you know, of course, because that part, like I'm talking to you, you're a reasonable person. Do you know what I mean? You're intelligent and thoughtful and reasonable. And when I say to you, did you take good care of yourself? You went,
Alyssa 49:19
I mean, mostly. And that's the thing is, like, I did not think about, like, the overall impact it would have later in life, right? Like, thankfully. I mean, I've had diabetes for 27 years. I've not had any complications, and I'm very thankful for that. But I'm hoping that, you know, my daughter, who's had an even lower a 1c than I ever had, you know as a young child, I'm hoping that she also, you know, gets to 30 years, 40 years, 50 years of diabetes, and does not have any complications either. Yeah, enjoys
Scott Benner 49:48
benefits of that, of that management style, exactly, yeah. And hopefully, who knows? I mean, there's no way to know what comes in the future, right, but yeah, you know, so we don't use. Think about things as quickly as they're happening, you know, which is, is, you know why you hear people say, like, oh, I don't want an older doctor because he's doing it, like, 15 years ago or that kind of thing. But, you know, you're regular and mph growing up. Then you go to Humalog and Lantis, probably, I'm guessing, right? And then, you know, on a pump, just because it avoids shots, picks a guy on a podcast to be like, hey, you know, if you know, if you thought about, like, timing your insulin, like this, and doing these things and like, so all that takes a lot of time, but now things are speeding up so quickly, like, right? Like, with AI, I was listening to this guy be interviewed the other day, and forget, what was he talking about? Energy, maybe, like, like, electricity and like, like, he's like, he's like, in 10 years, we're going to be powered by electricity, like, by the sun and by solar and, like, batteries and, and I'm like, how so fast? Like, that was my question when he was in the interview. And I don't know if this will really happen or not. Alyssa, that's not the point. The point is, is that he's like, AI, is that's the point. And he started talking about computers, training computers, and how much quick, more quickly, that will make us get to something. And then, you know, almost as a throwaway in the conversation, he said, and that's gonna happen in medicine too. Yeah,
Alyssa 51:11
I wouldn't be surprised. Oh, I'm
Scott Benner 51:13
like, Oh, I hear it. Like, okay, so right now, you come out of grad school with like, this harebrained idea about how a cell works, and you're going to dedicate your entire life to figuring that out. Now, you're just going to point the AI at it, and it's going to run simulations, and they're going to crash, and it's going to weed them down, and you're going to take a lifetime's worth of work and squeeze it into, you know, I don't know how long a year a weekend, like, I don't know how quickly it's going to work like, what is going to happen to health care in the next decade, and then how will that translate to diabetes? I mean, I hope, I hope so. I hope it does super exciting. Actually. It's definitely, I
Alyssa 51:52
mean, the improvements that I've seen you know, since I was a child, definitely right. I can only imagine
Scott Benner 51:59
how lovely would it be a list if none of you had type one diabetes when the machines took over and killed us all? Wouldn't that be
nice? At least I don't have type one and that thing steps on your head. I'm just going, I'm going over Terminator. I don't know exactly like how it'll go down, but, you know, I honestly, I think it's, I think it's amazing. Like, you know, I've brought it up on the podcast a couple of times, but I read this news story once about how Tesla the car people like, they're teaching their cars to drive, right? And they couldn't find computers that were fast enough to crunch all the data that they were getting back from the cars, so they built their own supercomputer to do it. And I was like, right on. I don't know if I even care about that or not, but let's go. You know what I mean? Like, they were like, these computers we have right now are not fast enough to take the data and do this with it. We'll actually design a faster computer. And I was like, Yes, I want more of that. I want more people thinking that way. You know what I mean. So that will translate to healthcare. It'll translate to everything. Because, you know, then suddenly a research hospital will be using computers. Like, there could be a world where none of us work one day and it's okay, like, where you get up and just like, feed your mind and your soul, and, you know, you live your life because things are taking care of things. And I might like that. I have to tell you, I had a week off, and it was pretty goddamn relaxing. So yeah,
Alyssa 53:28
and you don't take a lot of weeks off, do you? I
Scott Benner 53:30
really don't. I jumped back on with Jenny yesterday. We recorded an ask Scott and Jenny episode, like, the day after I got home, and I said to her, I'm like, well, let's see if I remember anything about diabetes. Like, because, you know, I I was sleeping a little later in the morning, getting up, walking around. It was warm outside. I did have a bit of a problem, Melissa, where I don't want to say what happened, but I had some money stolen out of my hotel room. And, gosh, that was unpleasant, but I let that go. I was like, I'm not I don't care. Like, I'm so relaxed, just gonna let this go. We actually had a really movie like moment this week, my wife accepted another position at a different company, and we were sitting at a rooftop restaurant in a hotel on like a warm southern day when my wife got a phone call and got this job offer and she accepted it, and I was like, this is the most cosmopolitan thing that has ever happened to us, because if we weren't here, this would have happened in our kitchen. So but instead, we're like, you know, sitting at a glass table with these big, heavy chairs, and, you know, there's an umbrella and it's sunny, and my wife's on the phone, like, hello, and I'm like, oh my god, this is like, like Anne Hathaway should be in this scene. Like, you know,
Alyssa 54:49
like a scene out of the movie, I
Scott Benner 54:50
swear to you. I was like, this is makes it so much more exciting, like this. Anyway, congratulations to my wife, who will have accepted this job six months. To go when you hear this amazing, yeah, she's very excited. Yeah, I think that things move the way they moved. Like, you can see it in our lifetime, right? Like, like, I can see it in your story. Or when I talk to somebody who's 50 years with diabetes, talk to Jenny, like, you know, and you can see the the pros and the cons. I don't know what good or bad it's going to come of all this, right? Like, like, using Jenny as an example, I think Jenny's a very healthy eater because, A, I think that's how her parents were inclined, like, right? But B, because she got put on that insulin where she needed to eat at every certain time, so she's, she's a very, like, you know, a regimented eater because of that. Now, I've also talked to people who will be like, I have an eating disorder because they put me on this regimented plan and by like, so it's a lot of personality too, right? Like, a lot of this stuff definitely is, yeah, a lot of the stuff, you can't really do anything about that
Alyssa 55:54
side of it, you know, the eating disorders and stuff like, definitely a reason that we are very careful about how we frame eating food and what needs to be eaten versus what you want to eat. Yeah, with our with all of our children, really? I mean, no, of course, you don't, not just, not just Jillian, but all of our kids.
Scott Benner 56:13
You don't know which person they are when they're that little like you know, so that there's a lot of care that goes into that. The way you disseminate information and talk about things, the words you use, that kind of stuff, yeah,
Alyssa 56:24
I mean, and the thing there, I can't remember which episode it was, but I know there was one episode when you talked about pre bolusing for Arden, and you talked about giving, you know, giving a certain amount of insulin that, you know, if she didn't eat anything, anything, you would give her juice box. That's definitely the mentality that my husband and I have, you know, we pre bolus, you know only 10 to 15 carbs which she may eat, that she may eat more than that, right? But at her age, like, we're not exactly sure. There are some days where she sits down and she wants to eat everything on the plate, and there are other days where she's like, I
Scott Benner 56:54
don't want to eat this. I'm
Alyssa 56:54
going to go play. Yeah. But as long as, I mean, as long as we're within 10 to 15 carbs of pre bolus, we know we can cover it with the juice, rather than forcing her to eat something she doesn't want to eat. Isn't
Scott Benner 57:03
it awesome to think that a little girl in North Carolina is doing a thing that I thought of 15 years ago in a gymnasium in New Jersey? Yeah?
Alyssa 57:12
I mean, yeah, because it has made the biggest difference for
Scott Benner 57:16
her. Yeah, I'm glad. I'm going to be mushy this week making the podcast, because I didn't talk to anybody last week, so all my, all my emotional stuff, didn't get to come out. So like, I'm gonna, I'm gonna have that going on. I'll probably cry in the next 48 hours, making this podcast for freaking sure, because I spent the last week defending myself against my family, because also the loss of that money was probably my fault. Listen, I took a, I don't know how you would put it down there, but I took a lot of hot poker to the ass over that for my family. They're like, Oh, look what you did. And I'm like, Yeah, okay, I got it, yep, just to hear you say that, like, this little thing, like, you know, this thing you heard on a podcast that I said, even I don't know, God, Arden's, I was gonna say it was a very old episode. I don't know which Arden it was. Arden's 20 in a couple of months. I did this when she was like, I don't know, six or seven, so maybe 13 years ago. And then I talked about on the podcast, like, 10 years ago. And here we are, you know, present day. And you're like, oh, what I do is, and I'm like, Oh, my God, that worked for you. That's so touching. You don't know how fulfilling that is to hear. You know, yeah,
Alyssa 58:25
I mean, yes, I can imagine. Because, like I said, it made, it makes a huge difference. Rather than trying to force her to eat food, you know, that she's, she's not hungry for she
Scott Benner 58:35
could be one of those people who, if that happened, ends up having an adversarial relationship with food one day.
Alyssa 58:41
And that's definitely something we think about a lot, and try very hard to make sure that we are not creating
Scott Benner 58:48
Yeah. I think it's important, you know? And it's funny too, because that's not why I did it, right? Like, the reason I did it the first time was because I wanted Arden to play basketball without her blood sugar getting too high, yep. And it took people coming on the podcast who had eating disorders to talk about why that was so important to them, you know, like, like, why food and talk the way it's spoken about? And you know that need to eat, or, like, I don't eat and when I'm not hungry, and and how that can, like, reshape some people's minds. And, yeah, like, I had to learn enough about that to speak about it the way I do now, too. And it's been, like, a really wonderful process. I'm starting to get to that point in my life, Alyssa, you're not going to know this, because you're really young still, where I start feeling like, oh, this is, like, the last third of my life, yeah. And I'm just starting to understand everything, yeah.
Alyssa 59:37
I mean, like, I said, it definitely made a huge difference for us.
Scott Benner 59:41
Yeah, I'm glad. I'm very glad, and I appreciate you sharing that with me. Is there anything we haven't talked about that we should
Alyssa 59:47
have? I don't think so. I think we kind of covered everything that I'd want to talk about. Mainly, you know, the biggest reason that I wanted to come talk to you was because I see so many, you know, even on the juicebox group, sometimes. And of parents who, you know doctors are telling them, No, you can't do that, or that's not how we do it here, then obviously that was something that we were told too. But I just think it's really important, whether it's for you or for your child, that you are advocating for what you think is best for yourself or for them.
Scott Benner 1:00:17
The only reason Arden is wearing an OmniPod is because when somebody said something to me, I was like, No, I'm gonna do this, you know, I appreciate your input, but I here's how I see it, here's
Alyssa 1:00:28
how we're gonna do it, yeah? So, yeah, I mean, and that's, and that's how she ended up on a pump, you know, in the hospital, right?
Scott Benner 1:00:34
No, of course. And you even filling out information, you know, on the car, right? Yeah, that's fantastic. I love that idea. Your husband was probably like, all right,
Alyssa 1:00:44
no, I mean, my husband definitely. He knew about diabetes, obviously, because I had already had diabetes for so long, he knew about it, but he, he never, you know. He didn't give me insulin. He did not fully understand the carp calculating things like that. So when we got the, you know, the little bit of education in the hospital, which was a small amount, it was more so for him, because that doing it for her was definitely a new experience for him.
Scott Benner 1:01:13
Is he very involved in it? Now, yes, he
Alyssa 1:01:15
is. When he and I are together, we definitely still talk things out like, okay, her numbers, you know, rising. You know, should I give her an extra point two? What do you think? Or, you know, we didn't, we didn't pre bowl us as well as we wanted to. So her number is going to rise. Should we maybe give a little extra? How much do you think? But when, like, when I'm not there, like when my husband takes her to the grocery store or is picking her up, you know, at the end of the workday, he is making the same decisions that I would make for myself or for her,
Scott Benner 1:01:42
that's great. Oh, that's wonderful. And yeah, and would you do you allow him to know more about your diabetes now? Or is that still about definitely,
Alyssa 1:01:52
so when I was pregnant with her, he definitely learned more, mainly because I had to have such tight control while I was pregnant with her, and then obviously, once she was diagnosed, he learned more about the way that I manage my own diabetes see
Scott Benner 1:02:08
so if he sees you not taking good care of yourself, does he say something? Yes, he
Alyssa 1:02:14
does. He actually, he's the only person who follows my Dexcom. And how do you feel about that. There are some days where I'm like, Yes, like, I know, I know, I know, I know. You're You're right. I need to, you know, my numbers, my numbers rising. I need to take some insulin, or, Oh, I'm low. I need to have a juice. And there are other times where I'm like, I already gave the insulin. You don't need
Scott Benner 1:02:33
to say it to me. Leave me alone. Yes, yes.
Alyssa 1:02:37
He's the only, he's the only one who follows my Dexcom,
Scott Benner 1:02:40
I'm telling you right now, all week long, Arden, like we were together, like we stayed together. I mean, six of the, yes, all six nights in, like, in two different hotels, because we kind of traveled around a little bit, absolutely fine. She, you know, there were times where she'd be like, Hey, here's my phone. Might do this. I don't want to do it this time, but it's so cool to watch you, you know, like the idea was, I want to take care of lunch, and I, you know, I'm very careful about how we talk about it. Like, as she gets older, obviously, I'm not upper ass about it and everything like that. Yep, you know, she was very open to speaking about it, because I was like, alright, and listen, this is a good opportunity for us to be together, to make some adjustments to your settings and stuff like that. As we were doing all that. She's all good with it. And then we were gone for 48 hours, and we were on the phone, and I said, Hey, did you have trouble shooting the GLP? Because she's not a big fan of the needles. She goes, leave me alone. And I'm like, and I'm like, Well, what happened? We were having such a good rapport last week. I was like, I was like, I was like, No, I'm just, I know you don't like the needles, you know. So I was wondering if it went okay. She goes. You're trying to make sure that I took it. And I have to be honest with you, unless that is what I was doing. So I'm gonna have to get even more stealthy. I guess in the future. It was interesting how she was okay with it when we were together and everything felt a little more like parent child. It feels like she's younger when we're together, like that, and then the minute we're gone and she's living by herself, she's like, I don't need your help, old person, yeah. And I was like, Oh, I got it. It's so cool. But anyway, we're I'll tell you what. I'll tell you this the first time I'll say this in the podcast while we were down there, she has some pretty significant problems with her dorm room, like the actual physical room, like humidity in it, and temperature and mold, and, you know, it doesn't surprise me in the self ants and roaches and mouse, okay, that kind of stuff. So thanks. So she's like, I'm getting an apartment. And I'm like, okay, so you know, you take basically the amount of money you're spending on room and board at the school, and you go, Okay, well, that's the amount of money we have to get you into a different place, you know? And so we looked around, looked around, and actually found a studio where she wanted to have a roommate to get a bigger place, but it's hard to find somebody who can commit to like both years and everything like that. And so we ended up landing on a studio. So Arden's gonna be living by herself, like, completely by herself, starting, you know, in September. Wow, yeah. So it's scary at the same time, like, you know, like, all right, well, it's gonna be what it's gonna be. So although during the tour, my wife asked the realtor, person from the apartment building. She goes, How do emergency services get into the building after hours? It's not a bad question to ask. Yeah. The woman looked at her like, what do you plan on having happen? She's like, they have their own key, so if you were to call 911, from your apartment, they can come through all the security and go right to your apartment. And Kelly's like, Okay, thanks. And she's like, okay, that's fine. And then there was this weird pause, and I said, Arden's just a big heroin fiend, and we like to be able to, you know, she nods out sometimes. And Arden's like, what are we doing? I was like, Oh, we're having fun. And so the girl like, you know, they don't hear you right away, because no one, there's no person on the planet who says to an apartment realtor, I have a heroin problem. So, like, that's not a thing they're accustomed to hearing. And so she react, well, I watched her brain process it, and then she turned back to me and went, what was that? And I was, like, I was just kidding. She's type one diabetes, and we just want to make sure, like, if there's a problem, like, she can get, like, the emergency service kind of access. And she goes, okay. And I was like, Oh my God, that's that old joke where, like, people come up to you and go, I don't know. I guess who's Guess who's pregnant or something like that. Yeah. It's like, not me. And you're like, oh yeah. So I just made, I made it worse, and then I made it better. And she was like, oh, diabetes, that sounds way better than heroin addiction. I was like, yeah, right, it's gonna be fine anyway. That's one
Alyssa 1:06:46
of the biggest benefits. Though, if you follow her Dexcom, yeah, you'll be able to see, I mean, if there is a problem and she's not answering,
Scott Benner 1:06:53
I mean, it's 100% that's, I don't know how, I mean, I guess we do know how other people do it, right? Like they keep their blood sugars higher, that's just, yeah, what they end up
Alyssa 1:07:04
doing. And that's the thing. When if her CGM like, when it's warming up that two hours, I'm like, Oh my God, this feels like it's forever. I don't this. This is taking forever. I just want to see what the number is like.
Scott Benner 1:07:16
How did my parents, all those years, they weren't thinking about it. It was a different thing. How
Alyssa 1:07:20
many? I mean, they woke up a lot to take my blood. But I was like, I cannot imagine.
Unknown Speaker 1:07:25
Yeah, no,
Scott Benner 1:07:26
I know. Make you crazy. Well, the g7 now is 30 minute warm up.
Alyssa 1:07:30
I know, I know. And we want the g7 so she's, yeah, she's using auto mode until it hooks up with the algorithm, or we're
Scott Benner 1:07:39
not switching. I gotta be honest. I think it's gonna be pretty soon. So, you know, I
Alyssa 1:07:43
really hope so. Yeah,
Scott Benner 1:07:44
but I mean, by the time it to be perfectly honest, by the time this comes out, I would expect that OmniPod five works with Dexcom g7
Alyssa 1:07:51
I really hope so. I mean, my mother in law has a g7 and I saw how small it was, I was like, Oh, that would be so great. Because, I mean, my daughter, my three year old, so small.
Scott Benner 1:08:00
Yeah. No, I understand. I mean they, and they try so hard to make that stuff tiny. I'll never forget I was working with OmniPod, like writing for their blog, like years ago, and Arden had the original OmniPod. So if you can imagine how big OmniPod dash or five is right now, like the other, the original Eros pod much bigger. Well, the real it was bigger and but it was still such a like an accomplishment, like this, insulin and the batteries and all the technologies in such a small place, you know? And then they moved to the pod got smaller. And I remember a person working at OmniPod said we used to have a picture of Arden hanging up here with an OmniPod on to remind us that it it wasn't as small as we thought it was like to kind of keep, keep us thinking about that, which I thought was really cool, and that's,
Alyssa 1:08:46
that's interesting, that you say that, because, like me wearing an OmniPod, it does seem so small, yeah, but on a tinier person's body, it doesn't seem as small. No,
Scott Benner 1:08:55
right? Yeah. And Arden was skinny and little, and she'd have it on, and they, they, I, there's a picture of her somewhere, and it was hung up, and the woman said, I would look at that and think we got to make that thing smaller, if we can smaller. Yeah. So this is really interesting, but anyway, I'm so happy that you guys are doing well, and I appreciate you spending your time with me for the last hour talking about thank you so much.
Alyssa 1:09:15
Thank you so much.
Scott Benner 1:09:16
Hold on one second. Okay,
the conversation you just heard was sponsored by Dexcom and the Dexcom g7 learn more and get started today at dexcom.com/juicebox a huge thank you to one of today's sponsors, gevok, glucagon. Find out more about gvoke hypopen at gvoke glucagon.com, forward slash juice box. You spell that, G, V, O, k, e, g, l, U, C, A, G, o, n.com, forward slash juicebox. OmniPod. If you're newly diagnosed, check out the bold beginnings series. Find it at juicebox podcast.com, up in the menu in the feature tab of the private Facebook group, or go into the audio app you're listening in right now and search for juicebox podcast. Bold beginnings. Juicebox is one word. Juicebox podcast, bold beginnings. This series is perfect for newly diagnosed people. I want to thank you so much for listening and remind you please subscribe and follow to the podcast wherever you're listening right now, if it's YouTube, Apple podcast, Spotify, or any other audio app, go hit follow or subscribe, whichever your app allows for, and set up those downloads so you never miss an episode, especially in Apple podcast, go into your settings and choose, download all new episodes. Hey, what's up? Everybody? If you've noticed that the podcast sounds better and you're thinking like, how does that happen? What you're hearing is Rob at wrong way recording doing his magic to these files. So if you want him to do his magic to you, wrongwayrecording.com you got a podcast. You want somebody to edit it. You want Rob tickets for the 2025 juice cruise are limited. I'm not just saying that they actually are limited. We have a certain window to sell them in, and then that's it. Juicebox podcast.com. Scroll down to the juice cruise banner, click on it. Find a cabin that works for you and register right now. You are absolutely limited by time on this one. I'm so sorry to say that. It sounds pushy, but it's the absolute truth. Juice cruise 2025 I hope to see you there. We're gonna get a tan talk about diabetes and meet a ton of great people who are living with diabetes. It's kind of gonna be like floating diabetes camp, but you won't have to sleep in a log cabin. You'll get a tan, and it's not just for adults or kids. It's for everybody you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1294 Weekly News 8/26/24
For the week of August 26, 2024
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
OmniPod, Hello friends and welcome back to another episode of The juicebox podcast.
This is the diabetes news that I found interesting for the week of August, 26 2024 nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. When you place your first order for ag one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. Ag one.com/juicebox don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40% at cozy earth.com if you'd like to help out the podcast and type one diabetes research. Go to T 1d exchange.org/juice, box. Join the registry, take the survey. All you need to be is a US resident who has type one diabetes or is the caregiver of someone with type one if you're those things and you'd like to help. T 1d exchange.org/juice, box. It should not take you more than 10 minutes. I've done it myself. It's very easy. They ask you some questions. You know, all the answers. You answer the questions, and just like that, you've helped some news today out of Washington, DC, from the FDA, by way of Acton, Massachusetts. Acton, of course, where OmniPods are made. OmniPod five now has approval for use with type two diabetes. Wow. Let's see insulin. Says more than 30 million people live with type two diabetes in the US. 6 million of them require insulin. Of those two and a half million use multiple daily injections. The company is hoping to bring the OmniPod to those people. Here's what their study you know, you gotta submit your study to the FDA, see what they say. The results demonstrated glycemic improvements with the use of OmniPod five compared to prior treatments of insulin injections or pump therapy in adults with type two diabetes. So you're gonna get some automation for people with type two, that's going to be kind of awesome here. Sorry, there was let's see what outcomes included significant reductions in a 1c reductions in time in hyperglycemia and reduction in total daily insulin dose. Insulin also reported a large improvement in time and range without increasing time in hypoglycemia. That's pretty awesome. Well, people with type two diabetes using insulin automation is now available to you. I don't usually do this, but use my link, omnipod.com/juicebox Get started today. We'll stay with the theme here of devices being repurposed for other uses. OmniPod five for type two diabetes, and now Dexcom has launched something called the Dexcom stello. Now this is an over the counter. CGM, right. I'm just gonna read your press release. Today, Dexcom announced a significant product launch as another continuous glucose monitor is hitting the market. Dexcom launched its stello over the counter, OTC CGM biosensor, small wearable sensors specifically for people with type two diabetes who do not use insulin. Stello features a 15 day wear based on the g7 platform. It offers a software experience tailored specific for non insulin users. So Dexcom, can you get a stello at dexcom.com/juice, box? I didn't know that this, uh, this news report was going to turn into, please use Scott's links, but let's take a look here. Yeah, just go to my link, dexcom.com/juice box. Then when you get there, I mean, click on the Dexcom logo in the top left. It's green. It'll take you to the front page and you can check out Stella. They'll see how you came in. Okay, so that's what we've got so far. For news this week, I'll be back. I like the stello thing is good. You know what? I mean, people the type two. Let me see if I can find out more about this. Stella is currently available for purchase@stello.com so go to my link and then click on that, you'll see it either as a single pack of two sensors with a total wear time of up to 30 days for $99 or through a monthly subscription of $89 a month, it includes two sensors every 30 days. This is FSA and HSA eligible, all right. Well, if you have type two diabetes and you want to check out Dexcom, check out the stello, and hopefully one day insurance will cover this too. But for now, it looks like it's over the counter and out of pocket. Over the counter, though, means you don't need a prescription. That really is pretty great. I guess we're going. Stick with devices almost exclusively. This week looks like there's a partnership between Medtronic and Abbott. Looks like the collaboration is aimed at integrating Abbott's FreeStyle Libre CGM Tech with Medtronic insulin delivery system. Abbott will develop a CGM sensor based on its FreeStyle Libre technology that will work exclusively with Medtronic, automated insulin delivery system and smart insulin pen. This integration will enable automatic insulin adjustments to help. Yeah, we know how it works. Well, that's interesting. So you're going to take Abbott's glucose sensing technology based on libre and make a CGM that only works with Medtronic stuff. That's interesting. I wonder why they did that. We're gonna learn more about that at some point, aren't we? For clarity, this is the future stuff like the new simplara CGM from Medtronic is not made by avid as far as I know. Huh? I do wonder, we'll have to get somebody on and talk about that. I wonder why they did that. I mean, maybe you're just going to use people's, you know, strength, or maybe Medtronic looked and said, Look, Abbott makes great CGMS. We'll do that. And we don't have to make them, or they're going to make them and not, I don't know, and I can't find out right now, but I'll try to find out in the future. For you. I am going to finish up this week with a publication from the American Diabetes Association. It's called effects of SARS cov two, infection on incident diabetes by viral, excuse me, by viral variant findings from the National covid cohort collaborative, N, 3c, how about that? Clear as mud? Let me break it down for you. The study aimed to understand if the risks of developing diabetes after covid 19 differed across different viral variants. So they looked at different variants of covid to see if one or the other gave you a greater risk of developing diabetes. Data from the National covid cohort collaboration showed that the risk of new onset diabetes was elevated across all SARS cov two variants, those are ancestral alpha, delta and OmniPod, the increase in diabetes risk was similar for all variants, but showed a delay in onset with the OmniPod variant after 180 days, despite the milder severity of recent variants, the risk of developing diabetes post covid remains high, highlighting the need for continued monitoring. The research supports the integration of diabetes prevention strategies in a post covid era. That's interesting. The findings suggest that people recovering from covid 19, regardless of the variant, are at an increased risk for diabetes, making ongoing surveillance and diabetes prevention important components of care. That's what they say. The study specifies that the increased risk of diabetes after covid 19 includes both type one and type two, but most new diagnosis were of the type two variant, the incident rates of both types increased across all viral variants. Excuse me, with the highest rates observed during the OmniPod. Like we said, The study used data from a large cohort to assess the risk of both types of diabetes. If you're newly diagnosed, check out the bold beginnings series. Find it at juicebox podcast.com up in the menu in the featured tab of the private Facebook group, or go into the audio app you're listening in right now and search for juicebox podcast, bold beginnings. Juicebox is one word. Juicebox podcast, bold beginnings. This series is perfect for newly diagnosed people. You
I've been doing these news segments for a few months now, and they're really well received. I want to thank you for that and let you know if you see any news about diabetes that you think is interesting, head over to juicebox podcast.com and send it in through the link. There's a link in there. How to contact me. You'll find it when you get there. I know you will All right, guys, I'm out of here. Do me a favor if you need or want anything that is sold by one of the sponsors, please use my links when you do that, you are supporting the production of this podcast, helping to keep it free and plentiful, and you're just helping me out. I pay my electric bill with this money. I keep the podcast going. I'm not saying buy something you don't want, but I mean, if you're getting an OmniPod, then go to my link. You know what? I mean, that kind of thing you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1293 The Fighter
Sandy has had type one diabetes for 63 years.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome back to the juicebox podcast.
Boy, I love this episode. Sandy is 70 years old. She's had type one diabetes for 63 years, and she and I had a fabulous conversation. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. Lots of people with autoimmune seem to have trouble with their thyroid, and that's why I've made the defining thyroid series, juicebox podcast.com click on defining thyroid the menu to find out more. A diabetes diagnosis comes with a lot of new terms, and you're not going to understand most of them. That's why we made defining diabetes. Go to juicebox podcast.com up into the menu and click on defining diabetes to find the series that will tell you what all of those words mean. Short, fun and informative that's defining diabetes. When you place your first order for AG, one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. AG, one.com/juicebox, one.com/juice box.
This episode of the juice box podcast is sponsored by Dexcom. Dexcom.com/juice box. Get the brand new Dexcom g7 with my link and get started today. This show is sponsored today by the glucagon that my daughter carries, gvoke hypo pen. Find out more at gvoke glucagon com, forward slash juice box.
Sandy Schwartz 1:53
Hi. This is Sandy Schwartz, excited to be invited to do a juicebox podcast with Scott and tell you all about my 63 years with diabetes.
Scott Benner 2:09
Sandy, seriously, 63 Yeah,
Sandy Schwartz 2:12
I was seven and I'm 70 now. So you can do the math? Well,
Scott Benner 2:16
I you assume I could do the math, but yeah, that's amazing. Seven years old, 60 through your 70 today. Wow, yeah, it
Sandy Schwartz 2:23
was Barb barbaric back in the day. By
Scott Benner 2:26
the way, I have a feeling I don't know you, but just from your intake form, I feel like you're a little you might be a little salty. I like that. I think we're gonna have a nice time together. So tell me, what do you mean barbaric?
Sandy Schwartz 2:41
Well, my father used to sharpen my steel needles in his wood chop, and I would help
Scott Benner 2:46
him, like, on a stone and or and Sam, like, literally take a steel needle and make it sharper for you, exactly. And
Sandy Schwartz 2:58
you know, there was one walking shot of insulin a day. There was no carb counting, although, after a couple of years, I went to Barnes Children's Hospital in St Louis, and they taught us something called the tag system. Have you ever heard of that? You're the first person to ever say that I have the book somewhere so the everything had a tag. And rather than explain it, we came home from the hospital to Memphis, and I rode my bicycle to the local Five and Dime, which is all that we had in the 60s and aka 711 now, and I bought two Snickers bars, and I came home and my mother made dinner, and I brought the Snicker bars to the table, and she asked me, What are you doing? And I said, Well, I added up your dinner and it's equal to these two Snickers.
Scott Benner 3:57
So I'm skipping dinner, and we're going like this today,
Sandy Schwartz 4:01
right? So I guess that was the beginning of carbohydrate counting.
Scott Benner 4:05
When do you think that was? Now, let me make sure I'm right. You're born in 54 353, and you're diagnosed, what? 60 Yes. Okay, so at what point do you think someone brought this tag system up to you? Probably 1963 64 Okay,
Sandy Schwartz 4:25
I have it somewhere. I'm going to send it to you. I'm
Scott Benner 4:29
googling it right now. Hold on a second. See if I know bacon
Sandy Schwartz 4:32
had a tag. Everything had a tag. So it wasn't just carbs, but it was the beginning of thinking that you could exchange more than green beans for broccoli.
Speaker 1 4:45
Sandy tab T, A, B, T, a G, G. Tab system, diabetes, T,
Sandy Schwartz 4:53
a G,
Scott Benner 4:54
yeah, I'm not seeing it. I mean, I guess it's just something that nobody ever talked about on the internet. I guess I. And that's okay.
Sandy Schwartz 5:00
Look up Barnes Children's Hospital. I'll try. They developed it. I'll find it and send it to you. It was very interesting. Thank
Scott Benner 5:08
you. I wonder too You're you talking about sharpening the needles? How frequently do you remember that happening? I don't remember. Would they get would they get sharpened after they started to hurt because they weren't because they were kind of like pushing instead of piercing.
Sandy Schwartz 5:26
I was seven. I don't remember. I just remember going into my dad's wood shop and helping him sharpen these needles that I was going to be using to take insulin. I very quickly learned to take care of myself as much as possible. I came home from the hospital. I've written about this on juicebox and how it changed my relationship with my mother, but I saw how much pain it caused her. And so at seven years old, I said, Give me that thing. I'll do it. Of course, she drew up the insulin. I'm the one who injected it.
Scott Benner 6:05
You took over your own care to save your mom.
Sandy Schwartz 6:07
You should be shrink. That was a very good statement. I'll have to discuss that one in therapy. Okay,
Scott Benner 6:15
by the way, I've had a couple of episodes. When it got done, I was like, I might be a good therapist one day, but, yeah, but I'll
Sandy Schwartz 6:21
be your sponsor. Oh,
Scott Benner 6:25
okay, well, keep your mind, this podcast thing falls apart. I'll put it on my list of ways I might be able to make a living.
Sandy Schwartz 6:31
I don't think the podcast is going to fall apart. I think it's the best thing that happened to diabetes sensors.
Scott Benner 6:39
Oh, do you really?
Sandy Schwartz 6:40
I did. I really do. I think that the way you run it, the way anybody can say anything, and, you know, I read something, I'm like, Really, they said that, but nobody jumps on them. I think it's very polite and informative and and supportive for so many people.
Scott Benner 7:02
Yeah, I tried very hard to set that Facebook group up so that it operates the way an adult with common sense should live. Yeah, and not. I can't believe you said this, or it hurt my feelings, or that made me upset, like I don't want people hurting people's feelings on purpose, right? But you know, and we certainly don't let that happen. But you know, there's, there's just listen, there's a good example. The other day, this, this person who I like a lot, and who's been a guest on the podcast, put up a post about something, and one of the responses felt a little harsh, but it was still on point, and it wasn't harsh towards the person. It was just, I'm trying not to give away details, but it was, maybe it would have been upsetting, almost being, like, kind of slapped in the face with a with an honest truth about about something. And, you know, I got, hey, this, you know, this should come down. And I responded back, and I said, I don't see it that way, like, I'm sorry you're upset, but there's nothing attacking about this. It's factual and it's valuable, and we're gonna leave it there. So, you know, that's just sort of how I do it.
Sandy Schwartz 8:04
I think it's a giant diabetes support group for the world.
Scott Benner 8:08
It is really, Yeah, no kidding. 47,000 people right now in it. And by the time someone hears this, it'll be six months from when we record this till somebody hears it. And I can tell you, as crazy as it sounds, yeah, there'll be 4000 more people in there by the time this airs, wow. Yeah. So there'll be more, like 52,000 probably by the time this comes out.
Sandy Schwartz 8:30
Well, good for them. It's good for them. Yeah,
Scott Benner 8:33
it adds 150 new members, like every few days. Wow. Yeah. I'm very proud that you said that because, because you're 70 years old and you've had diabetes for 63 years, like to say that this thing I made feels valuable only second to CGM is really touching to me. So I appreciate that if you take insulin or so final ureas, you are at risk for your blood sugar going too low, you need a safety net when it matters most, be ready with G, VO hypo pen. My daughter carries GE, voc, hypo pen everywhere she goes, because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that. I trust low blood sugar. Emergencies can happen unexpectedly and they demand quick action. Luckily, jivo kypo pen can be administered in two simple steps, even by yourself in certain situations. Show those around you where you store GEVO kypo pen and how to use it. They need to know how to use jivo kypo pen before an emergency situation happens. Learn more about why G VO, kypo Pen is in Arden's diabetes toolkit at G VO, glucagon.com/juicebox, gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma, or if you have a tumor in your pancreas called an. Visit gvoke, glucagon, com, slash risk for safety information. Today's episode of the podcast is sponsored by Dexcom, and I'd like to take this opportunity to tell you a little bit about the continuous glucose monitor that my daughter wears, the Dexcom g7 the Dexcom g7 is small, it is accurate and it is easy to use and wear. Arden has been wearing a Dexcom g7 since almost day one of when they came out, and she's having a fantastic experience with it. We love the g6 but man, is the g7 small, the profile so much closer to your body, the weight. You can't really feel it, and that's coming from me. And I've worn one, I've worn a g6 I've worn a g7 I found both of the experiences to be lovely, but my gosh, is that g7 tiny? And the accuracy has been fantastic. Arden's a one. C's are right where we expect them to be. And we actually use the Dexcom clarity app to keep track of those things. That app is built right in to Arden's Dexcom g7 app on her iPhone. Oh, did you not know about that? You can use an iPhone or an Android device to see your Dexcom data. If you have a compatible phone, your Dexcom goes right to the Dexcom app. You don't have to carry the receiver. But if you don't want to use the phone, that's fine. Use the Dexcom receiver. It's up to you. Choice is yours with Dexcom, dexcom.com/juicebox,
Sandy Schwartz 11:30
well, I will tell you that I've worked in the industry for a long time, and you know, I thought, I thought that I knew a lot about diabetes, I find that I not only learn things, but it has inspired me, maybe where I've gotten lots of days a call, it has inspired me to bump up my game, bump and nudge my game. You bumped
Scott Benner 11:58
and nudged your game. Can you tell me a little bit about what being connected to other people does for motivation? For
Sandy Schwartz 12:06
me, the podcast and Facebook groups have inspired me to like I said, bump up my diabetes game a little and and also to help motivate other people, like I I chime in when I think that I can be helpful. Sometimes I grit my teeth with what I read, but I try to be polite and couch what I say like I have, like I just said about my mother, that you know that we came home from the hospital and she felt guilty, and I felt sad that I quote, unquote, lost my mother. And so when I see these parents who you know are are not accepting the illness, it's I personally have a terrible reaction to it. I just want to get in there and say, look what you're doing to your child. But I know that diabetes treatment today is different than it was when I was seven years old. So if my mother had had this podcast, I would be have been treated differently.
Scott Benner 13:21
Are you saying that a parent that can't accept the diabetes and fold it into life is projecting rejection to the child,
Sandy Schwartz 13:31
rejection to the of the child. No guilt, grief,
Scott Benner 13:39
fear. This is from the child's perspective. If the parent doesn't seem like they've got it and they're not burdened by it, what do you give me the bigger picture?
Sandy Schwartz 13:49
I think the parent feels guilt, fear, sadness, anger, goes through all the grief responses and let me not generalize to me, I felt like, hey, where did my mother go? But I didn't know that at the time I have through thinking and feeling and watching the relationship with my mother, which deteriorated from the day I got diabetes, I think that I wish she had accepted it as well as I have. I think as a kid, you go through it. I mean, you go through whatever you're going through, and you don't know better, you just do what you have to do. And then when you see your parents change so much, or let me personalize it, when I saw my mother change so much, it created a rift,
Scott Benner 14:41
and she never got over that, or was it just set and set in motion, and that's how it felt to you.
Sandy Schwartz 14:48
Then it feels kind of sad to say that. I think I never got over it. I tried really hard. I didn't. I couldn't have said all this. If I'd known all this while she was alive, I would have. I processed it with her, but I think it set in motion that mother daughter stuff times 10,
Scott Benner 15:09
so she had all those feelings that you described you feel like she disappeared from the scenario. Maybe she came back and got it together, but by then you were hurt and you couldn't get past it.
Sandy Schwartz 15:22
I think she saw, I mean, she was always very proud of all the steps I made. And I was giving a talk one time at the Diabetes Research Institute at the University of Miami to a bunch of fellows. And she was in town, and I brought her, and I think that was very healing for both of us. I tried really hard to get through the resentment I felt as a child. And of course, I'm putting adult words to childhood feelings, so I don't know that's the word I would have felt. Then I think I felt sad. I felt like I lost my mother, like, where did my mother go? Who is this lady who's always sad and and scared and and not unlike she used to be?
Scott Benner 16:11
And you can connect that to yourself, because even if you don't realize that the timing is, I got diabetes and then this happened, and then you can put that onto yourself, like you caused it almost by having diabetes. I
Sandy Schwartz 16:24
don't know if that's my personality, but maybe like I didn't feel guilty, I felt sad and angry.
Scott Benner 16:31
Yeah, tell me. Tell me. Tell everybody what you do for a living. Well,
Sandy Schwartz 16:35
I'm a psychotherapist, but I also kind of fell into working with some of the big companies writing physician and patient education materials for a long time. So I see patients professionally, and I have had a personal experience in the diabetes space, manufacturing and that kind of thing.
Scott Benner 17:01
I just wanted people. I just wanted people to know because you answer questions like a psychotherapist. That's why should I change that? No, not at all. I actually Sandy, if Can I be honest? I thought because you're thoughtful when you answer, you're like Erica. You listen to me when I talk to Erica. Okay? So you're you're thoughtful and you're pausing. And I didn't want people to think, Oh, I feel bad saying this. I didn't want people to think it was your age. Ah, you're actually, you're, you're, you're considering your words very carefully,
Sandy Schwartz 17:31
okay, yeah, I'm sorry. It's funny when you say my age, because if you ask anyone who knows me, I do not act my age. I mean, I just came back from a Keith Urban concert where I was in the pit, so get out of here, really. Yeah, six feet from the stage, that's fantastic. I could be up close and personal, dancing and hollering and having a great time.
Scott Benner 17:57
Let me tell you something. I spoke at an orthodox event this week. It's this weekend. It's the second time I've done their event. Really lovely group. And when I walk from my room to the where I have to go speak in the morning, or when I'm done at the end of the day, and I walk back, I have my headphones in, and I'm listening to like Metallica while I'm doing that, and I wore my headphones all the way back into a room, and I sat down, and people were already waiting for me. I was early, but they were already waiting for me. I sat down, and as I took out my my headphones, they all looked at me, and I went, I'm not listening to metallic, if that's what you were thinking. And I watched all their faces, and I think most of them didn't know what I was talking about. And I was like, okay, and I put my just put my headphones on. I was like, hey, so we're here to talk about and I thought, why don't we get going early? But I don't think people would look over at me at 52 years old, driving in my car and and imagine that I'm listening to freight ends of sanity. So, so good for you.
Sandy Schwartz 18:56
I drive a Bronco with the top off, and I Blair, Jimmy Buffet, God damn, I used to work on a scuba diving boat. Scott, oh,
Speaker 1 19:06
you're Sandy, you're a party. I see what's going on here. All right,
Sandy Schwartz 19:11
I was 20. I left Tennessee, I moved to Miami, and I quit school and worked on a scuba diving boat for three years before I decided to grow up and
Scott Benner 19:24
you went back to school after that, I did about that. So, okay, so barbaric in the beginning with these needles. But what are the shifts that you remember? Like, what's the first shift in care that you recall, so
Sandy Schwartz 19:36
short acting and so on? That's I was a teenager, and my if there were endocrinologists, neither my mother or nor I knew about them, I was at my pediatrician's office. Maybe I was no I was older than that. I was maybe 15, and because I was drinking beer. So that's how I know this. But. He said to me, Sandy, how come all my other patients go into DKA and you net, you have never been in DKA. And I said, you know that short acting insulin you give me when I'm sick? Well, I decided that I can take it when I eat pizza and drink beer. So I was bumping and nudging you were. I also, even younger than that, I used to take as much one shot of long acting insulin a day, as much as it took to get low and then back up a unit or two. Oh, so I kind of saved myself without knowing your
Scott Benner 20:39
Yeah, you and I have a lot in common. So you you pressed the the boundaries of what they gave you, and because you didn't have a measurement system, you were like, I'm gonna keep trying this till I get dizzy, and then I'll back it up a little bit
Sandy Schwartz 20:50
Exactly. And the same thing with the short acting insulin, if you can give me this, well, here's another thing. I have asthma, and I take steroids. So if you can give me this short acting insulin when I take steroids, and I can take it for pizza and beer. Yep,
Scott Benner 21:06
yeah. So you figured out what to do with that medication before they knew what to tell you to do with it. Yeah, in the 60s, I feel like that right now with glps, by the way, yeah, like so Arden is taking a GLP, and it's decreased her insulin needs pretty significantly. And she just, she's in the middle of her finals, like today and tomorrow, her last finals day for this for this quarter. And she and I were talking this morning, she was calling to tell me, here's what she called to tell me, she goes, Hey, I almost killed an old lady. And I was like, Wait, what happened? And she goes, she goes, it wasn't my fault. And I go, what happened? So she said, I got in my car to leave class, and she's like, and I've got to go to the printer. I gotta print this out. I gotta go home. I gotta change my CGM. Then I've gotta get back to class and I gotta turn in this other final. And if the printer is not like, she's kind of going online, she's like, but I get my car, I sit I you know, I put my stuff down, I get settled. And cars now, you know, they have cameras, and kids drive them, like video games. Like kids don't look over their shoulders. They like, they access cameras, you know. So she's like, I don't know what made me look forward, even though I was backing up, but I'm so glad that I checked my cameras. Then I looked forward and I said, why she goes? This very old woman was leaning on my car. Oh my god. And she had just been walking through the lot after Arden got in the car, and she's leaning on the car, and doesn't realize Arden is in the car, but she's using it for support. And Arden said, If I would have backed up, she absolutely would have tumbled over, slammed her head on the car and just went right to the ground. And she said, Oh my god, I'm just so happy that I saw her. And I was like, no, no, that that's great. And then, you know, I'm glad everything's okay. She's okay, yeah, she she's like, I let her lean till she was done, and then walk away. And I was like, okay, but, but then I was like, hey, you know your CGM is about done. You got to go home and do your CGM. And she's like, Yeah. She's like, that's on my to do list this morning. And I don't think there was a enough GLP in the pen when I shot it. And I was like, What do you mean? She goes, I'm supposed to shoot a half of this ozempic. We're moving her from ozempic to something else, but there's a transition period. And she goes, but I shot it, and I don't even think there was a quarter. And I said that that's not going to be enough. You know, you're going to need to go to the next pen that I gave you and do it again. She goes, will that be too much. And I said, well, the alternative is, your blood sugar is going to be crazy until we get back to the next injection. So just, just do it. That's a thing like her doctor prescribed it for. But, like, our insurance won't cover that. And if you go to any endocrinologist right now and tell them, like, you know, we're like, shooting, like, half you half milligrams of this and that and Arden's, they'd be like, You can't do that. It's not it's not okay for that. But I'll tell you right now, and you might be listening to this right now and be like, You can't do that, Scott, but five years from now, you're gonna look back on this recording and go, That guy was ahead of the curve, and
Sandy Schwartz 23:55
so that's where you were. So do I? I don't Do I seem like the kind of person that would say you can't do that, Scott, I'm gonna say, give me some Yeah,
Scott Benner 24:04
no, I think you're all in I love that example, because you literally took something that they gave you, and they were just like, look for steroid problems if you're sick, like this kind of stuff. And you're like, Well, wait, all that this is doing is I'm having a high blood sugar, and this is bringing it down quickly. I'll apply this to anything. You know what I mean exactly when you say you think that might have changed the course of your health. What has your health been like all this time?
Sandy Schwartz 24:29
My health is excellent. Sometimes I have survivor's guilt because I've lost so many friends to diabetes. But for people listening to this, they have to realize that we took one walking shot of insulin a day. We had no we had no way to bump and nudge. And luckily, that rarely happens like it used to. But my health, I don't have any of the other medical. Colic syndrome, conditions, so I don't have any high blood pressure, I don't have any high cholesterol, no neuropathy, none of the things that make diabetes hard to treat, except I take steroids on a regular basis. But just like you're doing with the ozempic, you just get to know how much insulin you need for how many Miller grams of steroids, and you do what you have to do. I mean, it's it's a balancing act, but it's not impossible.
Scott Benner 25:33
Sandy, tell everyone listening, if you would have listened to doctors and waited for them to help you, where would you be right now? Do
Sandy Schwartz 25:38
you think Dad?
Scott Benner 25:39
You think you would be dead. I
Sandy Schwartz 25:41
know I would be. So when I was had had diabetes 19 years I went to the University of Florida for graduate school, and right before I went, I went to the ophthalmologist and found out that I had background retinopathy in one eye. And so when I got to Gainesville, I immediately looked up their diabetes program, and I was it was 1979 it was 1978 when I went to Gainesville, but in 1979 I joined a research trial there, and I wore the big blue brick that the first insulin pump that looked like it was, it looked was the size of a brick, okay? And we also did the research on home blood glucose monitoring. We would take our we would stick our finger and put it on a strip that looked like the old test strip. It would turn a color. We we would take our own venous blood with an insulin syringe and put it in a tiny test tube, and right on the test tube, what we thought our blood sugar was, and keep those in the refrigerator, and then we would turn those in weekly. And so I was one of the first six adults to wear a pump, and also to do home blood glucose monitoring. So I went to the ophthalmologist in Gainesville after six months. And I think you can finish the sentence. Yeah, everything. No, no retinopathy. It was gone.
Scott Benner 27:15
Yeah. How about that? Hey, I'm actually looking at a picture of the big blue brick. And in case anyone thinks that Sandy is gilding the lily, here it's about 10 inches long. Looks like it's maybe four or five inches wide, maybe two inches thick. It's got like, almost like tubes coming out of the ends, and it almost feels like pipes coming out of the top. And it hangs on the belt, but the person's belt that it's on in the photo is like pulled down like three inches by the weight of it. And it's really something, but it worked, huh?
Sandy Schwartz 27:46
We set the basal rate with a screwdriver in one unit increments. No
Scott Benner 27:51
kidding. I want everybody to did ever complain that my pump doesn't go down to point? Oh, five. You should. You should. You should stop complaining. That's amazing with a screw, like a little set screw, because, yeah, you were restricting the flow, like a like, like, plumbing, yes,
Sandy Schwartz 28:10
yes, it was on. It was an insulin syringe that fit a glass insulin syringe on the outside of the pump. I put a picture of it on your Facebook page. If you look up my name, you'll see it okay. It was pretty amazing. Wow. And then one time, I rode my bicycle to a party, and my doctor was there, and I kept telling him I didn't feel well. And he's like, Well, what do you feel? And I'm like, I don't know. Just not well. He's like, Do you have a fever? I'm like, No. And he's like, Well, what do you feel? I said, kind of shaky, but not like my blood sugar is low. He's like, Sandy. How far did you ride? I said, I don't know, 20 miles. He's like, Have you had lunch? I'm like, No, I don't have to eat lunch anymore. I'm on a pump. I was hungry, but for 21 years, I never knew what hunger felt
Scott Benner 29:01
like, because you were always eating on a schedule, because
Sandy Schwartz 29:05
long acting insulin you have, you know you're feeding it, it peaks. Yeah, I was feeding my insulin instead of my insulin, feeding me so I was hungry, but I didn't know what hunger felt like. No
Speaker 1 29:18
kidding, did the brand of management that was necessary while you were growing up? Did it have any more impacts on your relationship with food? Hell yeah,
Sandy Schwartz 29:30
yeah. I mean, I have had to change my views on food and lose weight, because as soon as I could eat what I wanted. I ate what I wanted, and I still love carbs and sugar and but I have lost about 50 pounds. I'd love to be on the GLP. I need to lose about 10 or 15 more, but, yeah, my relationship to food was, was altered. But, you know, we can check. Change Anything we want to change, if we try hard enough. Well, I'm
Scott Benner 30:03
but I mean, if you think back to very young Sandy, you know, hearing about the tag method, she's like, I'm having two snicker spars for dinner tonight. So like, you know, I did wonder, and I can't imagine being that restricted and having such a specific regimen for so long, and then somebody telling you this part's over now, and you're not going a little crazy in the other direction, you know, like, just makes sense to me, honestly, yeah, one on the lines of, I don't know, every Catholic girl I knew when, when they graduated from Catholic school, cut their hair or did something very drastic to take ownership of themselves. Does that make sense? Right? Yeah, yeah, that to me seems like the same thing. Honestly, just like, you're like, Oh, I'm finally in control. Let me do something big, you know, right? And then before you know it, those that sugar hits you in those carbs, and they're so good, you know, and and you're on your way. Well, can I ask what made you want to come on the podcast at
Sandy Schwartz 31:04
once? I found you guys on Facebook and started listening to the podcast. I just wanted to be involved. I wrote to you and said, I want to be involved. And you wrote back and said, Come on the podcast. I just, I miss working in diabetes. I think, honestly, I think I don't get the jobs I used to get in diabetes because of my age, which I mean, I still have a brain, and I I like to be helpful, if I can be to other people who live with this disease. I see mostly, most of my caseload is chronic illness and disability. And acceptance, not just of chronic illness or disability, but of life in general, but specifically when you're hit with a lifelong issue, is so hard for so many, and if I can help them get through that resistance and to acceptance, then their life is going to be so much richer. So
Scott Benner 32:12
is that the key? In your opinion, acceptance moving forward?
Sandy Schwartz 32:16
I think acceptance is the key to moving forward in life in general, yeah,
Scott Benner 32:22
I do too, changing, being able to change your expectations, not being so cemented on an idea, and being able to accept that things shift that have nothing to do with your decisions. I think all that's really important. Yeah, yeah, to your point, too. Not just about diabetes, really,
Sandy Schwartz 32:43
yeah, life and life in general,
Scott Benner 32:45
when people have trouble accepting things as you've worked professionally through the years, how do you help them get past that?
Sandy Schwartz 32:52
I think it has to do with expectations, and looking at their expectations, grieving what they've lost and moving through the grief process to acceptance,
Scott Benner 33:03
and that's through talk therapy that you can accomplish that. Mostly,
Sandy Schwartz 33:07
yeah, yeah. If not, I have a hammer I can hit them over that.
Scott Benner 33:12
You just whack them like Bugs Bunny. If they after four times they visit, it doesn't get together.
Sandy Schwartz 33:17
I don't know where that came from. I have never said that I'm like,
Scott Benner 33:22
so this episode, heard my titles already that I have written down big blue brick, which I don't think I'm gonna do. There's a Keith Urban song called the fighter. I thought I might call it and but now I'm thinking I just might call it the hammer, because for the first 35 minutes, people will be like, Why is this called the hammer?
Sandy Schwartz 33:43
I love it. I love the fighter. Tia. It's a great song. Yeah,
Scott Benner 33:46
well, maybe that's the one I'm gonna go with. Actually, is there a certain personality that has more difficulty moving forward than other types of personalities?
Sandy Schwartz 33:55
I have to think about that one, and I'll tell you on the next podcast. Okay,
Scott Benner 33:58
how about this? When people come into the office, can you assess them in an hour and know with reasonability how this is going to go? Yes, yes, and that that's about their build and their makeup, right? It's about
Sandy Schwartz 34:11
their ability to have insight and to be willing to let down their resistance and their fears and look inside themselves.
Scott Benner 34:22
Is any of that contingent on intelligence? I
Sandy Schwartz 34:26
don't think so. I mean, I'm going over clients in my mind, and I'm thinking of a couple that surprised the hell out of me, their ability to have insight. So I would say that you would suppose that it's the it's intelligence, but I think it has to do with emotion too,
Scott Benner 34:50
okay, maybe a less measurable part of who they are. So like, I know people, people love to say emotional intelligence nowadays, like a. A buzz word that people like is emotional intelligence, just you understanding the big picture and then not getting in your own way.
Sandy Schwartz 35:07
My goal is equal parts of head, heart and gut. And so a lot of people are stuck in their head and in their left brain, like the thinking part, not the feeling part. And some people are are angry and frustrated and stuck in their gut, and some people are very emotional and stuck in their heart. And I think if we can somehow rearrange and even to some degree, then we can give up some of the baggage. We can stop obsessing so much. We can stop being so depressed, if we can look at all at the parts that make us operate, as far as our emotions. Does that makes
Scott Benner 35:57
it does? Is there anything about it that's gender specific? Or is it people's experiences and that lead to during their growth times?
Sandy Schwartz 36:07
I think that men are more self protective initially than women, but breaking through that resistance, I think we're all pretty equal.
Scott Benner 36:16
Everybody can get through it,
Sandy Schwartz 36:18
no, and not everybody can. But equally well, yes,
the opportunities there and the opportunity. Thank you. Okay, thank
you. Yes.
Scott Benner 36:27
Is there truth to that idea that people can get stuck at a chronological maturity depending on where they're kind of like traumas come from, like, if something terrible happens to me when I'm 14, am I kind of stuck at 14 till I worked through it, or is that just kind of pop psychology?
Sandy Schwartz 36:44
No, I think it's true for trauma or drug use. I think my mom got stuck when I was diagnosed with diabetes. Yeah, it took her a long time to accept the fact that I wasn't going to die. And I mean, she never uttered those words, but yeah, I we call it fixated. Yeah, fixated. I just want to
Scott Benner 37:07
say for people listening emotional intelligence is the ability to understand, use and manage your own emotions and positive ways to relieve stress, communicate effectively, empathize with others, overcome challenges and diffuse conflict. That's from help guide.org if I have a lower emotional intelligence, but I have a good therapist, they can get me there if I want to get there, right? If
Sandy Schwartz 37:31
you're open to getting there, yeah, if you're not too resistant, if you're not holding on to the past that or or maybe you don't even know it. Maybe you're just too repressed to open up. Well, I was gonna
Scott Benner 37:45
say, Are there people who express that they want to get past something, but then their actions keep them there?
Sandy Schwartz 37:52
No, no. I think once you once it comes from your sub or pre conscious, to your conscious, you've broken the you know, you've broken the jar open. I think once you express it, you're on the other side of the hill, the good side. Yeah, yeah. So
Scott Benner 38:12
people who want change can change.
Sandy Schwartz 38:15
I believe so, yeah, don't you? Do you believe that?
Scott Benner 38:18
Oh, absolutely. I also think that it correlates right with diabetes to that thing I say to people like you get what you expect, like if you expect high blood sugars, as crazy as it sounds, there's these tiny variables in your thinking and your actions that you'll never even notice that are pushing you towards high blood sugars. Right? If you expect to be more in control, you make these little micro movements and decisions that get you there. And it's not a thing you'll see happening, but it's about attitude. It's about who wants it more, you know, who can stick with it long enough do the work not give up that kind of stuff. Eventually, one day, you pop your head up and you're like, Wow, I'm good at this, you know, and but you don't see it happen like that. Yeah, no, I really believe that. I just think that it's funny because I took a very technical thing and then had an emotional reckoning from it. Then the technical thing was I started to see wherever I set Arden's high alarm is where I could keep her blood sugar, which didn't make any sense. If the alarm was at 250 then her blood sugar was frequently 250 I made it 200 then her blood sugar frequently didn't go over 200 so I was like, Ooh, 181 50. Once I was just I was off to the races then. And then I eventually pushed it down to 120 and then I get what I expect, like I saw the technical side of it, which just really is, if I'm being clear, once you have your settings right and you know what you're doing a little bit, you react to those alarms. Your reaction requires less insulin, because it's happening at a lower number. If you use less insulin, you have less of a chance. Below, so you have less of a chance of a rebound high, and that's what keeps your stability there. But the truth is, is that once I saw the technical aspect of it, I realized that there's a bigger picture of unseen forces. And the way it came out of my mouth one day was, I think I'm getting what I expect. So I think you get what you expect, and that's it like, if you say to yourself, I'm going to get up every day and do 10 sit ups and you actually do them, your stomach will get harder, like it's just, you'll get what you expect. You just have to do it.
Sandy Schwartz 40:29
I love that. And probably the best thing I've gotten personally from juicebox is setting those, those high alarms. I mean, I never put it in the term. She just put it in. But I've been lowering them and lowering them. And my a 1c has come down and down. It's never been high. But I'm like, What the I mean, he's right.
Scott Benner 40:56
That's fantastic. What were target a one CS through your lifetime. I mean, I'm imagining the ADA has moved them a number of times through your life, right? Well, there was no
Sandy Schwartz 41:05
a 1c when I went to Gainesville, there was something called a glycosylated hemoglobin. The norm for that was around eight instead of six. And my first glycosylated hemoglobin after 19 years of diabetes, pumping and nudging and using short acting insulin for steroids and food and everything I tried to do was 18, really, and the norm was eight, and I had to get used to hypoglycemia, shaking, sweating, anxiety at 120 then 110 then 100 once I went on that pump, because you get what you expect, and the other way too. Scott,
Scott Benner 41:52
yeah, your body expects high blood sugar, so it makes adjustments to blood vessels and and a lot of different things trying to keep you alive longer at that higher blood sugar, and then suddenly you bring that blood glucose down, and then you have low signs and symptoms at numbers that are not actually low,
Sandy Schwartz 42:10
exactly. Yeah. It's amazing, if you think about it scientifically. I mean an 18 glycosylated hemoglobin is like, A, 15, A, 1c, yeah, no. I mean, I made good grades. I was in graduate school, you know, there was no 504 plans, and I never even thought about my mother, never thought about not sending me to school, but she didn't know what my blood sugar was. So you get what you expect. I mean, I expected to make good grades, and I did. So went out
Scott Benner 42:42
there and found a way to do it. And also, once you felt low at 120 you didn't say, Oh, I better make my blood sugar higher. You said, I better get through this, because I have to keep bringing my blood sugars down.
Sandy Schwartz 42:53
Well, the doctors told me that I was like, I can't handle this. And they were, yes, you can. So it wasn't all me. I had a little help from my friend,
Scott Benner 43:04
wonderful. Yeah, you get by with a little help from your friends. Exactly. Hey, the ADA is telling us right now that less than 7% for many adults. However, a 1c is individualized, and your doctor may give you a higher or lower a 1c goal, depending on your needs. Way to not say anything. Ada, congratulations. Lot of words, lot of words, lot of words. No guidance, yeah,
Sandy Schwartz 43:28
yeah. But listen to me, I think it's dangerous for people to try to have lower like, sugars when, when they don't know what they're doing like I have a friend who died because she got sent home from the hospital, not with type one, with type two, and was on hospice, but her daughter kept giving her her short acting insulin, but she couldn't eat. I mean, so with you know, it works the other way too. What you don't know can hurt you.
Scott Benner 44:01
Yeah, I am not a fan of just saying one thing my thought here is that we don't want to do least common denominator education. So the way I always think of it is, you know, in a class of 20 kids, there's, you know, two or three exceptional kids. There's a handful of above average kids, there's average kids, there's below average kids. There's a couple of kids who are really struggling. And I understand the desire to not want to leave the ones at the bottom of the line like behind, but at what cost is it to the rest of them who could take in more information? And isn't there a way to give everybody what they need, instead of just saying the safest thing, which is, hey, you know what? As long as everyone sees below seven, you're fine, because then people are going to come along and say, well, the ADA says, under seven, I'm fine, you know? And I say, well, the person standing over there doesn't have diabetes. There anyone sees like, 4.8 4.9 right now? So. That's pretty significant difference from seven to 4.9 and they say, well, can show me studies that say that seven is bad. And I'm like, I don't know if there's studies about that, but, you know, show me studies that say it isn't and they're gonna say, Oh, it's fine, because, you know, we've done studies, and people are okay, but you don't know what they're accepting is okay. You know what I mean, like, I don't know the answer to this question. Like, is a seven, okay, six, okay. Is five? Okay? I don't I honestly don't know. All I can tell you is that I try as hard as I can to put my daughter as a 1c as close to normal as I can without putting her in danger. That's what I'm doing. And you know, like, if they got explained to me that way, then I think that everybody on the spectrum of desire and understanding could make their own decision. That's how I feel about it. But makes sense? Yeah, they say seven is okay. So that's what they say. Family growing up, did you were you ever been married? Have children, anything like that? I
Sandy Schwartz 46:00
never got married. I had a son when I was 40, after 33 years of diabetes on my own by choice. I'm not gay. It wouldn't matter if I was, but I'm way too independent. I'm working on that now. Never Say Never Scott I think you might still get hitched if someone can handle me.
Scott Benner 46:24
Well, you didn't like being tied down to another person. I
Sandy Schwartz 46:28
didn't know how to be. I dated, I had long relationships. I had a lot of fun. I'm working on learning to be I'll tell you when I get there.
Scott Benner 46:42
What are you working on being? What are you trying to get to, where I
Sandy Schwartz 46:46
can share more, where I can trust more, where I can let go more, where I can I mean, I have great friendship with men and women, and I've had great, quote, unquote, more than just friends with men. I've just never shared my space for very long.
Scott Benner 47:07
Can you self analyze and tell me why that's hard for you? Yeah, but that belongs on another podcast. Okay, can I guess or do you not want to talk about it?
Sandy Schwartz 47:17
No, you can guess. I just it's go ahead,
Scott Benner 47:20
you get and you don't have to answer, but I've done a lot of these. Did you have any sexual abuse in your past? No, never, nothing like that. Okay, nothing, nothing. Was your dad a problem?
Sandy Schwartz 47:31
My dad was a problem and that he was so loving and so kind and so attentive
Scott Benner 47:38
that you can't meet a guy as good as your dad? Consciously,
Sandy Schwartz 47:41
I would not say that, okay. Subconsciously, maybe Okay,
Scott Benner 47:45
all right. Well, that makes sense. Have I ruined Arden by being an attentive father? I guess we'll find out. Is that what you're
Sandy Schwartz 47:52
saying? No, I think it was more than that for me. But I What did she say? Ask her. I
Scott Benner 48:01
mean, she's got a boyfriend, she seems to be okay, so Okay, well,
Sandy Schwartz 48:04
then I guess the answer is, right, there, people are different. We're all different. Yeah,
Scott Benner 48:09
so you dated plenty, you had plenty of relationships. Some were even long term. You just Were you ever with somebody that you thought that I am going to marry this one
Sandy Schwartz 48:16
if they had gotten their act together?
Scott Benner 48:20
Oh, okay, you're not type A though, right? No, no, not at all. So you're not expecting other people to be perfect,
Sandy Schwartz 48:27
no, but I had very co dependent relationships where it was, I mean, you know, it can be 6040, but it shouldn't be 9010, so Okay, all right, couple
Scott Benner 48:38
people. So there are a couple people on the way, if they would have pulled it together, you would have done it. But would have done it, but you didn't you when you said you purposely had a baby, did you meet a guy and say, Hey, I don't want you involved, but I need, I need some help. Or did you get a donation? How did you do that? Okay,
Sandy Schwartz 48:53
now you have to put me on the after hours.
Scott Benner 48:58
Okay, go ahead.
Sandy Schwartz 49:00
This is not about diabetes. Do you want me to tell you?
Scott Benner 49:03
I mean, if you want to tell me, I want to know. If you don't want to tell me, You shouldn't say,
Sandy Schwartz 49:07
oh, yeah, I first I tried with friends, both having sex and the turkey baster method, and then I went to the doctor, and the doctor said that I needed to take some medicine because I was too old. Here we go to that age. To me again, I was 40, and so I started taking the medicine, and my turkey baster wasn't working. And then the doctor said to me, why don't you change doctors? And I was working at the University of Miami, and I said, because this one's free. And she said, Do you want free or to have a baby? So I changed doctors, and the doctor said to me, why are you doing this with friends? And I said, because, oh, he said something else to me that I haven't thought about till just now. You're a good therapist. And he said, Well, I want, I want. You to look at these sperm bank donors. And I'm like, but I want to know the person. And he said, Well, that's going to be a problem for you later on, or it could be, why don't you look at these? But he also said to me, when I first met him, he said he was sitting behind his big mahogany desk and in this luscious office, and he says to me so you're 40 years old, or you're going to be 40 years old, you're single, you've had diabetes for 33 years, and you work on a university income. Tell me why I should help you. And I said, you know that lady that was sitting in the waiting room with me, and came in before me. He's like, what does she have to do about it? I said, she lives in a big house, she has a husband, she has no chronic illnesses, and I don't know why my life should be any different than hers. And so he said, Okay, when do we start? Oh, wow,
Scott Benner 50:58
very nice. When you said Turkey based you, did you mean that euphemistically? Or?
Sandy Schwartz 51:03
No, it worked. I mean, it didn't work for me, but you can look that up. Oh,
Scott Benner 51:07
I don't need to look it up. Sandy, you're not the first person that said that to me. I've made a lot of podcasts, so, like, I just didn't know if you were just euphemistically talking about in vitro fertilization, or if you were actually at home using a collection from a friend and doing it on your own that, yeah, yeah, we had a whole conversation about that. One of the other episodes, you can cut that part out. Why would I cut that part out? Sandy, that's fantastic. You misunderstand me. If you think I'm cutting that out, that's really what happened in your life. I don't think these conversations are valuable if people are stilted, so you need to be open to say what actually happened to you and what you've done, and you know what's helped and what hasn't
Sandy Schwartz 51:49
I think my life is a person that has diabetes, and I think too many people identify as and this is not a used word anymore. It used to be, but as diabetic, I would never identify as diabetic. I am a person. I have a lot. I wanted to have a baby. I wanted to work on a scuba boat. I wanted to be a therapist. And I happened to have diabetes, and it's important to me to take care of it the best I can. So I it's probably my number one goal, because if I didn't take care of my diabetes, I couldn't have a job. If I didn't have a job, I couldn't have a baby, I couldn't have a house, I couldn't have a car. So taking care of diabetes is number one, but I do not identify as a diabetic. I understand
Scott Benner 52:43
the distinction. I do. Yeah, it's funny. It's and it's not the word as much as it is. The connotation is that, right? Yeah,
Sandy Schwartz 52:51
I'm a person with diabetes. It's not the first thing. Like, I don't go to a job interview and say, Hi, I'm Sandy Schwartz. I have diabetes. But sometime after I get the job, I say, we need to talk about this, or before I get the job, when it's offered to me, I'm like, if you want to use me to get money, you can say I'm disabled because I have diabetes, but it's not the first thing that comes out of my mouth.
Scott Benner 53:16
In Arden's day to day life, she is always aware of her diabetes and always taking care of it, and yet, and I say this frequently when I do speaking events, if I brought her up on the stage in front of a bunch of people and said, Hey, tell everybody about yourself, I think she'd talk for a half an hour and never mentioned that she has diabetes,
Sandy Schwartz 53:36
then you've done a good job. Oh,
Scott Benner 53:38
I appreciate that. Thank you. I think that's a goal for everybody too. You don't ignore it, but you don't bask in it, either, if that makes sense. And
Sandy Schwartz 53:47
since most people who get type one diabetes have parents that are helping them, then it's important for them to make their children's lives important in addition to taking care of their diabetes. Yeah, no, 1,000,000%
Scott Benner 54:05
Sandy, is there anything we didn't talk about that we should have?
Sandy Schwartz 54:08
I don't think so. Do you think so? I
Scott Benner 54:10
think this was terrific. This is one of my favorite interviews I've done recently. Actually,
Sandy Schwartz 54:15
I think you're terrific.
Scott Benner 54:16
Oh, thank you. Do you know you cursed in the middle of it?
Sandy Schwartz 54:19
I cursed a few times
Scott Benner 54:22
you surprised me with the one. I don't know why you're you're just like, you're like, a fucking and I was like, Oh, you caught me by surprise. I love saying, by the way, fucking mother, they're all my favorites, but I you took me by surprise. I wasn't expecting it. So we're gonna call this one, the fighter. Is that good? I love it. Excellent. I do too. What's the next concert you're going to? Well,
Sandy Schwartz 54:45
I'm in mourning for Jimmy Buffet, and when he died, my feelings of immortality died a little bit with him. So there's a big, a big event in Hollywood. Bull. I don't know if I can get a ticket. I don't know what my Knox concert is. I'm, like I said, I'm I I've been to like, 40 buffet concert, so no kidding. You're a paradigm big time. I mean, I lived in South Florida. I worked on a dive boat. I saw him first in 76 at the Orange Bowl opening for the Eagles, and fell in love. I've been to political rallies with him. I followed him around the country. I'm a huge carrier.
Scott Benner 55:30
No kidding. See you say the Eagles, and then I know I'm gonna get in the car and put the eagles on and listen to them for a month. Well, I
Sandy Schwartz 55:36
saw buffet when I was I mean, I saw the Beatles when I was 13. Did you really wear in Memphis, Tennessee, at the Coliseum? It was the first time my mother let me go anywhere with a friend. She dropped me off and picked me up. Do
Scott Benner 55:50
you still remember it? I remember it? Yeah, the Beatles changed the whole world. Huh? That's wonderful. What else have you done that that everybody would be like, Oh my god, I can't believe you were there for that. Do you remember the moon shot? Of course, Kennedy. You remember Kennedy being shot?
Sandy Schwartz 56:06
Oh my gosh, we had to line up outside the whole school, the elementary school, and the principal came out with a big megaphone and told us we were going home because it was a sad day in our country. MLK,
I live in Memphis,
Scott Benner 56:21
yeah, so I was gonna say, what was that like?
Sandy Schwartz 56:24
We were sequestered in our homes. My father took home the cleaning lady with a gun. He carried it. I was the first time I knew we had guns, and he took drove her home. My uncle's store was Ramsay. I mean, you know, yeah, yeah, it's
Scott Benner 56:44
crazy. Wow. My gosh, you've seen like everything. Can I Can I ask a quote? Wait, you have can I ask a question? Has nothing to do with anything? Sure, go for it. How long into your life before you realized that everything's repeating, like politics, entertainment, fashion. You hear a kid talk about politics, and they're like, you know, I think these people are all out for themselves. And you go, Oh, you figured that out, did you when's the first time you realize? Because it happened for me in my 30s. And I was like, Oh, we're just on a cycle, and new people are born and they think they're discovering something, but it's something the rest of us and history have known forever and ever. It's the first time they're seeing it like, do you? Do you agree with what I'm saying?
Sandy Schwartz 57:30
Oh, yeah. I mean, you know, I should have saved my bell bottom Pana worm a
Scott Benner 57:37
couple more times, a number of different in a number of different decades, right?
Sandy Schwartz 57:42
But think about what you're saying. I mean, I don't want to get into politics, but, I mean, you know, there was a time not too long before I was born, it seems to be where there was so much division and anger, and that seems to be repeating, and that's pretty darn scary. Yeah,
Scott Benner 58:00
I think there's, like, more than one cyclical thing happening at the same time, right? Like, so there's a place where, like, I don't know, communities cycle. There's places where states cycle, where the country cycles, where the world cycles, like, it's all like, but in the end, it's, it's only powered by by humans and their responses to things. So they're going to be very similar over and over again. What changes is, you know, the materials the cars are made out of, and the technology we have and stuff like that, so it looks a little different, but it's really the same. And that's why, when people get to a point where, like, I'm so scared, like, it's, you know, this is it. It's the end. I'm like, this isn't the end. Like, it's just gonna happen again and again and again, it's going to keep happening like this. I find it fascinating. I find it fascinating because if you can see that you can live a happier life, and if you can see the repetition in diabetes and learn to accept it and be ready for it and not shocked by it, you can lead a better life. So like nothing should be surprising to you after you've seen it a couple of times, I guess is what I'm saying. That's an interesting analogy to diabetes. Everything is the same. I don't care how different it looks. People, ideas, processes, they're they're all, everything's the same, right? Well, if you stop and listen to this podcast, the parts of it. When I'm not talking about diabetes, I'm still talking about diabetes, right? You know,
Sandy Schwartz 59:24
I get that.
Scott Benner 59:27
How about new music? Do you know who Gary Clark, Jr is? I'm sorry. I don't Don't be sorry. How hard is it to discover new music when you're when you're not around friends as much as you used to be and out in clubs and going to places. Excuse me, speak for yourself. No, you know what I mean. It's harder for me to discover new music. I'm contingent on my son, like my daughter telling me about newer music, and I try to keep up. And there is plenty of new music that I hear that I like. I don't do that thing like. It doesn't sound like what I grew up with, so I don't like it. It's hard to be introduced to it like I'm. Working. I get up in the morning, I take a shower, I eat something, I make this podcast. I do a bunch of work. I eat something again. I do more work. Like, I'm not, like, in my car at high school, I'm not bumping into 500 people. Or, like, have you heard this? Like, you know, interesting. Yeah, I agree. Yeah. All right, my last question for you, I promise, did covid scare the Holy hell out of you? No, Did
Sandy Schwartz 20:00:21
it scare you? No,
Scott Benner 20:00:22
I'm asking, because of diabetes and age, did you think it's going to get me? Or what would you even if you thought that, would it scare you?
Sandy Schwartz 20:00:30
No, I'm more like, go with the flow. Take care of it when it happens. I mean, not that I wasn't careful and didn't get my, you know, vaccine still now, but not much scares me.
Scott Benner 20:00:44
Is there a time in life and maybe you haven't hit it yet where you just say to yourself, what happens? Happens like whatever, like, I can't live forever. So if this is it, this is it, or is that a freeing feeling? Or do you not think of it that way? That is my life the whole time. Oh, yeah, did you think you weren't going to live this long at some point? At some point, well, my
Sandy Schwartz 20:01:09
parents I wouldn't live past 40, which is why I had a baby when I was 40. I mean, no, I ironically, you're calling this episode The fighter. I never thought I would it. Would I that's what I said. A little bit of my mortality died when buffet died, but I still got a lot. I mean, the day Jimmy Buffett died, I probably had 200 texts when
Scott Benner 20:01:36
I woke up. Tell me Jimmy Buffet's death, because he's a contemporary makes you feel mortal, no,
Sandy Schwartz 20:01:41
because what he stood for,
Scott Benner 20:01:46
oh, I see, hey,
Sandy Schwartz 20:01:49
go ahead, tell me what just his free and easy lifestyle is, is me 100%
Scott Benner 20:01:57
Yeah, and he was Still, he still died. Yeah. Hey, did we just figure out why you didn't marry anybody? Because I wanted to marry Jimmy Buffet, well, no, because do you think you didn't have children until you were 40, or get married because you thought you were going to die and you didn't want to start a family and then leave your family. And I'll go a little further, the way you felt like your mom left you.
Sandy Schwartz 20:02:21
I don't know about the mom part, but after I was diagnosed with diabetes for years, I had a repetitive dream. I was this child sitting on the front steps of our house, and this boy would come up to me and sit on the steps and say, you want to get married? And I would say, Well, I have to tell you I have diabetes, and he would run away.
Speaker 1 20:02:46
Okay, so you're afraid of rejection. Maybe. Did it ever happen? Sandy, did a boy ever say no because of diabetes? No,
Sandy Schwartz 20:02:54
no, no, never. I mean, it was part of who I am. Yeah, love me, love my
Scott Benner 20:03:00
fool, and men have loved you despite diabetes, with
Sandy Schwartz 20:03:04
diabetes, not despite Okay, okay,
Scott Benner 20:03:07
yeah, okay, all right, that's all. I just wondered, like, you just said that all of a sudden, and I was like, Oh, I wonder if that's what happened to her. If she just didn't is your child? I forget do. Is it a son or daughter? I don't know. My
Sandy Schwartz 20:03:19
son was in the trial net. He has no markers. Every now and then. He's 30 years old. Every now and then I test him, because I see him drink two Gatorades in a row. And
Scott Benner 20:03:33
so I'm never gonna stop. I'm never gonna stop being a parent. Is that what you're telling me?
Sandy Schwartz 20:03:36
Well, you can't help but notice it, right? Yeah, any other
Speaker 1 20:03:40
autoimmune for you? Celiac, thyroid, anything like that?
Sandy Schwartz 20:03:45
No, I have probably intrinsic autoimmune asthma. I have that's the only other autoimmune because of the long term steroid use. I have osteoporosis, the worst you can have but no, I'm lucky. I'm very unluck. I'm lucky. I mean, part of it is trying to control my diabetes, but like I said, I didn't have any control for 19 years. I think most of it is genetics. And I'm just at the jackpot
Scott Benner 20:04:18
genetics. And you pushed insulin hard. When you were younger,
Sandy Schwartz 20:04:21
I did push insulin hard. I was not afraid of it. Yeah,
Scott Benner 20:04:25
about that? Okay, let's leave it at Lucky. Then I like that as an ending. Thank you so much for doing this. I really, genuinely appreciate it. You can absolutely come back whenever you want to. This
Sandy Schwartz 20:04:34
is fantastic, once things change, I'll come back. Okay, all right,
Scott Benner 20:04:38
hold on for me one second. Okay. Okay,
a huge thanks to Dexcom for supporting the podcast and for sponsoring this episode. Dexcom.com/juicebox go get yourself a Dexcom g7 right now using my link. A huge thank you to. One of today's sponsors, gevok, glucagon. Find out more about G vo hypo pen at G VOQ, glucagon.com. Forward slash juice box. You spell that, G, V, O, k, e, g, l, U, C, A, G, o, n.com, forward slash juice juicebox, Hey kids, listen up. You've made it to the end of the podcast. You must have enjoyed it. You know what else you might enjoy? The private Facebook group for the juicebox podcast. I know you're thinking, uh, Facebook, Scott, please. But no. Beautiful group, wonderful people, a fantastic community. Juicebox podcast, type one diabetes on Facebook, of course, if you have type two, are you touched by diabetes in any way? You're absolutely welcome. It's a private group, so you'll have to answer a couple of questions before you come in, but make sure you're not a bot or an evildoer. Then you're on your way. You'll be part of the family. I want to thank you so much for listening and remind you please subscribe and follow to the podcast wherever you're listening right now, if it's YouTube, Apple podcast, Spotify, or any other audio app, go hit follow or subscribe, whichever your app allows for, and set up those downloads so you never miss an episode, especially in Apple podcasts, go into your settings and choose download all new episodes. The episode you just heard was professionally edited by wrong way recording, wrong way recording.com, do.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!