#1292 Keep Taking Showers
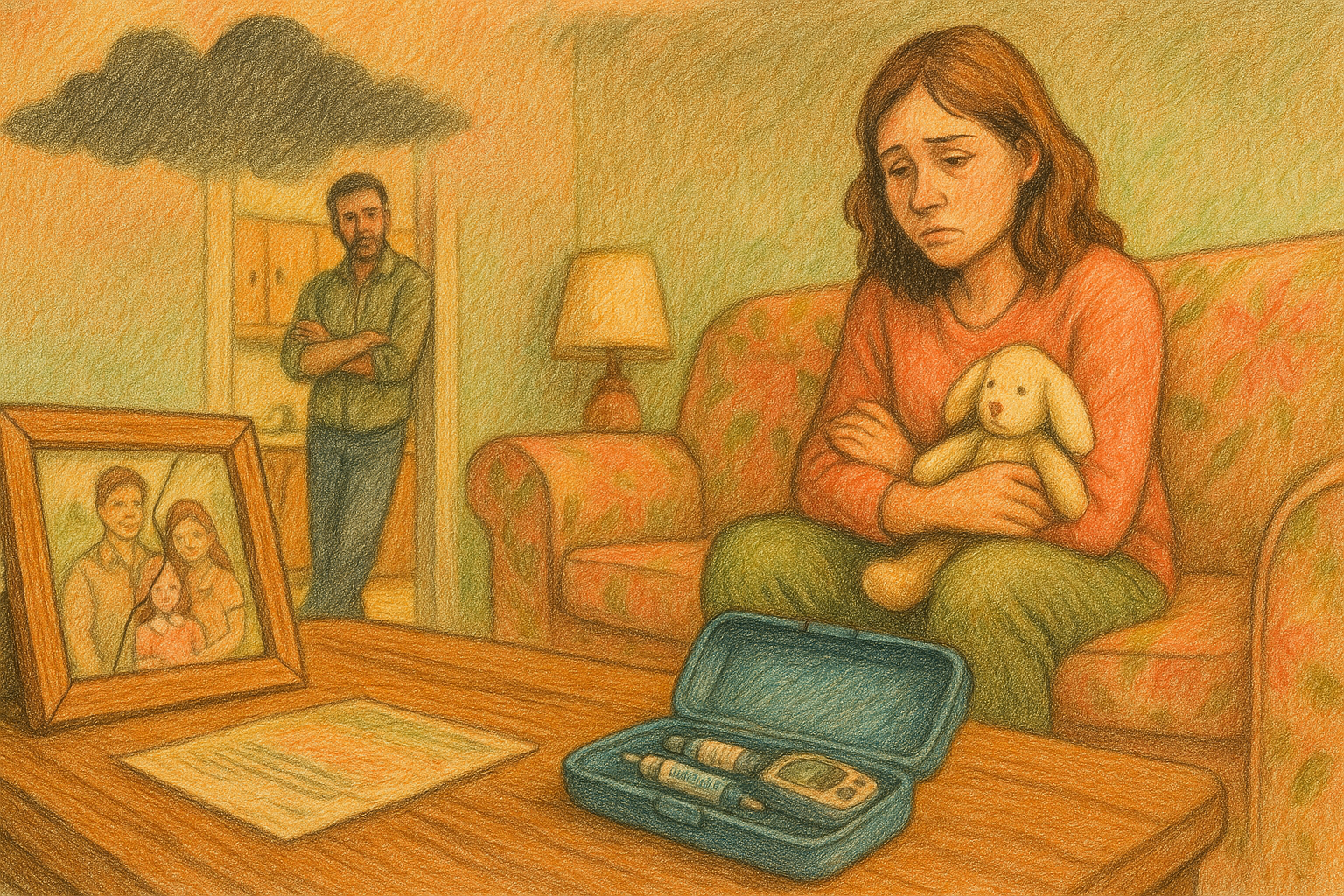
Jason, his sons, his sister and his father have type 1 diabetes. We talked about hospice care.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends. The hell was that? Hello friends, and welcome to another episode of The juicebox podcast. I gotta find out what that was. Hold on. I just listened back and realized that you couldn't hear that. So now you're wondering what's wrong with me. But trust me, there was a noise.
Unknown Speaker 0:22
You today
Scott Benner 0:24
I'm going to be speaking with Jason. Now. Jason has type one diabetes. He got it when he was 18. He's now 45 his son Wesley is 12, has type one diabetes since he was two. His son Cooper is 10, diagnosed 11 months old. And his daughter, who is six, well, she currently doesn't have type one diabetes, but there's other people, and we're gonna find out all about it. Please don't forget that nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin when you place your first order for AG, one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. AG, one.com/juice box. Don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juice box at checkout. That's juicebox at checkout to save 40% at cozy earth.com I know that Facebook has a bad reputation, but please give the private Facebook group for the juicebox podcast, a healthy once over juicebox podcast type one diabetes. The group now has 47,000 members in it again. Did you know if just one person in your family has type one diabetes, you are up to 15 times more likely to get it too. So screen it like you mean it one blood test can spot type one diabetes early. Tap now talk to a doctor or visit screen for type one.com for more info. Having an easy to use an accurate blood glucose meter is just one click away. Contour next.com/juicebox That's right. Today's episode is sponsored by the contour next gen blood glucose meter. This episode of The juicebox podcast is sponsored by the ever since CGM, and sure all CGM systems use Transcutaneous sensors that are inserted into the skin and last seven to 14 days, but the ever since, sensor is inserted completely under the skin, lasting six months, ever since, cgm.com/juicebox,
Speaker 1 2:35
I'm Jason. Live in the middle of Iowa, and I'm type one. I'm diabetic. I have two children that are also type one diabetic, and I believe today that Dave and I are going to be talking about my dad, who was also type one diabetic.
Scott Benner 2:50
You want to tell people why you called me, Dave,
Speaker 1 2:53
why I called you? Dave? Well, apparently there was some review of your podcast that referred to as Dave, which is telling you how much they pay attention to the actual content they're listening to.
Scott Benner 3:02
It was a really great review about how fantastic the podcast was and how great I was, and then called me Dave. And I was like, I love that. I it could have been a typo. It could be that this person believes My name is Dave. I don't care. You know, I am maybe one of the few smaller podcasters who don't come on and go, Hello everybody. I'm your host. You know what I mean? And then my name and like, I don't do that because I think, I mean, if you want to really know why, I think it makes you sound like you're small time, right? Yeah, I don't turn on the television and not know who somebody is I'm looking at. I don't need to be introduced to them. I know sometimes, like in older media, a host will come onto a TV show and be like, you know, Hello, welcome to the show. I'm David Letterman, like that kind of thing, but that's just, to me, an old idea. So like, moving forward, they're a huge podcast. I've never once turned one on and been like, hey everybody. My name's Billy, I'm the host today. And I'm like, Okay, if they don't know, they'll figure it out, and if they don't figure it out, they're not listening to you. So anyway, maybe I was wrong, just in case that guy's listening Hey everyone, this is the juicebox podcast, and I'm your host, Scott Benner, not Dave. Oh, hey, Scott. Hey. What's up? Dave, how many people right now do you think we're like, oh, Scott, or is it just him?
Unknown Speaker 4:26
I thought this was Dave, yeah.
Scott Benner 4:27
Well, now on the Facebook group, if you or a couple of other intrepid people call me Dave, then it causes then people are like, that's not Dave. And I'm like, Uh oh, this is gonna go on forever.
Speaker 1 4:37
It get it gets engagement though. It gets engagement though. So people ask them questions.
Scott Benner 4:41
We're feeding that algorithm. That's right, Jason, we're feeding the algorithm making it do something I actually that's a whole job that, yeah, I wouldn't want to take the time and to be boring and explain to people, but getting a Facebook group to serve the people who were in it well is a lot about making sure contour. Conversations are happening. And, you know, every once in a while somebody will ask a question, and it's kind of like a, maybe a, I don't know, a beginner question, and somebody will rush in and go, that question has been asked 50 times, and just search the group. And I every time I'm like, no, no, no, bad not don't just search the group ask the question, because if you start searching the group and shooting the group like it's an encyclopedia, the group will die like the algorithm needs to see people asking questions and answering questions, and it's more human, and I think leads to people understanding things a little quicker. So let's start with you. How old were you when you were diagnosed?
Speaker 1 5:40
I was 18. I just turned 18. It was in October, and actually voted for President for the very first time from my hospital bed.
Scott Benner 5:50
Who'd you vote for? You don't tell me that it was Bill Clinton at that time. Okay. How old are you now? 45 that's insane, isn't it? Yeah, time is terrible. Oh my god, okay, let's run through it. You have two kids.
Speaker 1 6:08
I have three kids total, three. Two of them have type one. How old are they? Our oldest is 12 years old, and he was diagnosed at two and a half years old. And our middle boy, who just turned 10, he was diagnosed at 11 months old. Wow. And our daughter, she is six years old,
Scott Benner 6:28
and you're worried because she hasn't reached 10 or 12
Speaker 1 6:32
yet? Yeah, yeah, she's, she's made it so far, so it's, uh, thankfully, she hasn't shown any signs yet. But we're, we're prepared, yeah? Well, I
Scott Benner 6:40
mean, you'd have to be this point. I mean, if you don't have enough experience to handle it, then who does right, you know?
Speaker 1 6:47
And then your father, type, yeah, yeah. You know, when he was diagnosed, he was diagnosed around three years old. Oh, wow, yeah. So that was back in the stone ages. So
Scott Benner 7:01
you're the one that really pushed the envelope, as far as you all go, making it to 18. Okay, so he was three, yeah,
Speaker 1 7:11
and, you know, just, just to tack on to that, my sister, who is a couple years younger than me, she's also type one. Oh, okay, yeah, how
Scott Benner 7:21
old when she was diagnosed? You remember she, I think was just 14 or 15. Okay, beat her easy. Okay, no, wow. Do you have other brothers and sisters? No, just one sister. Okay, how about other autoimmune stuff? No,
Speaker 1 7:39
I know you're gonna say, but you know, did you No, I don't think there is. You don't think
Scott Benner 7:44
there just is. It's just type one diabetes. You guys are what they call hyper focused. Yes, okay, wow, when you have type one and your sister has type one and your father has type one, when you are getting ready to have a family, what runs through your head about the possibility of diabetes in children? This episode of The juicebox podcast is sponsored by ever since, and ever since is the implantable CGM that lasts six months, ever since. Cgm.com/juicebox cgm.com/juicebox, have you ever been running out the door and knocked your CGM off, or had somewhere to be and realized that your adhesive was about to fall off? That won't happen with ever since, ever since. Won't get sweaty and slide off. It won't bang into a door jam, and it lasts six months, not just a couple days or a week. The ever since CGM has a silicon based adhesive forged transmitter, which you change every day. So it's not one of those super sticky things that's designed to stay on you forever and ever, even though we know they don't work sometimes, but that's not the point, because it's not that kind of adhesive. You shouldn't see any skin irritations. So if you've had skin irritations with other products, maybe you should try ever since, unique, implantable and accurate. So if you're tired of dealing with things falling off or being too sticky or not sticky enough, or not staying on for the life of the sensor you probably want to check out ever since, ever since, cgm.com/juice box. Links in the show notes. Links at juicebox podcast.com, contour, next.com/juice box. That's the link you'll use to find out more about the contour. Next Gen blood glucose meter. When you get there, there's a little bit at the top. You can click right on blood glucose monitoring. I'll do it with you. Go to meters, click on any of the meters. I'll click on the Next Gen, and you're going to get more information. It's easy to use and highly accurate. Smart light provides a simple understanding of your blood glucose levels. And of course, with Second Chance sampling technology, you can save money with. Fewer wasted test strips. As if all that wasn't enough, the contour next gen also has a compatible app for an easy way to share and see your blood glucose results. Contour next.com/juicebox and if you scroll down at that link, you're going to see things like a Buy Now button. You could register your meter after you purchase it. Or what is this? Download a coupon, oh, receive a free contour next gen blood glucose meter. Do tell contour next.com/juicebox head over there. Now get the same accurate and reliable meter that we use. Well at that point in time. You know, I
Speaker 1 10:42
mentioned it to my endocrinologist a few times, and they always said, you know, it's a very low percentage chance of that happening, so I really didn't give any thought to it. And I don't think it, I don't think it would have changed my mind at all. It wasn't a surprise when it happened, but it still hurt, you know, hurt a lot, yeah, I bet two years old, right? Yeah, two two years old, 11 months old. So, yeah,
Scott Benner 11:05
yeah. Arden was just two years old, and I recall it feeling like the promise of my life was revoked. If that makes right, you know what I mean? Because we were a young family, and things were, I mean, we weren't like, killing it or anything, but it was going well, and you could see that we were moving in the direction we intended. We had bought a very small house recently, and I was like, oh, you know, I grew up renting my whole life, and it's like, wow, we're like, we're doing it. You know what? I mean, like, we're getting out of the hole that somebody started us off in, and then that happened, and it felt like it felt like the hole we were in got thrown into a different hole, you know. So how about your wife? Do you think she ever even considered it?
Speaker 1 11:55
I don't think so. I don't think she thought about it at all like it wasn't on her radar. I think part of that's because I've been fairly well managed my entire life. So she only saw a few lows here and there, and didn't really, you know, partake in any of my care for it, because, you know, I'm an adult guy, and I can, I can do it myself. So
Scott Benner 12:13
do you have any hindsight on that? Should you have made her more aware of it?
Speaker 1 12:18
I think so. I think in general, people should do that more often. I think it's important for people to more understand, I think what's wrong with your significant other. You have any idea why you didn't? No, I talked to my mom about this recently and asked her about that, and she she said, I think it's just a guy thing, but I'm not even sure it's just a guy thing. I think it's people in general, because, you know, people are just worried about showing a weakness, yeah, and especially weakness like type one diabetes, where it's not visible most of the time,
Scott Benner 12:51
yeah, it's not, like, the it's sort of the invisible stuff, right? Like, yeah, like, that's why I think anxiety or mental illness is even harder to talk about, because you're like, there's an unseen thing that just tackles me, and I don't hear it coming, and I don't know how to get out of the way of it. And, you know, just once in a while, randomly, my blood sugar might get really low, and right, I could get into a situation where there's nothing I could do about it, and now I'm like, left open to hope that the world around me helps me and gets me back here again, exactly. Yeah, it's tough. Your father not share it with your mother. She
Speaker 1 13:27
did not really partake in any of his care, either, and he was very, very, very private about it. I would say so much so that my sister and I really had no clue or weren't very knowledgeable about how to treat him if he was low. We'd only seen it happen a few times, because he was fine most of the time. And I remember one time, you know, I got home from school probably early teens, you know, sitting on in my bedroom, Dorking around, and I hear my dad's truck pull up in the driveway, and I hear kind of a crash outside. I get up out of my bed, and then he comes stumbling through the door, you know, pale, sweating, shaking. I ran to the bathroom where the glucose tablets were at, and I grabbed one glucose tablet and took it out to him and made him eat it, and then like nothing was happening. So I poured him a glass of water and just dumped a bunch of sugar into it, and he drank that, and eventually he came around. But you know, that's all I knew how to do at that point in time. And it wasn't like somebody came to me and said, Hey, if he's low, do
Scott Benner 14:34
this right. It was more of just
Speaker 1 14:39
do what I thought was right, even though it wasn't enough at that point in time. And you were in your teens at that point, yeah, probably 12 or 13. It's a long time to live with somebody and not understand fundamentally what turns them back on. You
Scott Benner 14:52
know what I mean Exactly? Yeah, look at you, and you figured it out, though, right? Yeah,
Unknown Speaker 14:57
we figured it out. Yeah. Did
Scott Benner 14:58
that get you a puppy? An ambulance that day. Yeah, if you had a puppy out of that or anything, you remember,
Speaker 1 15:03
no, but, you know, I would say that my dad and I's relationship wasn't always incredibly close. And you know, he's not a a guy that's going to come out and say, Hey, I love you. He would say it in other ways, but after he kind of recovered from that low I had went back in my bedroom and I was like, crying, you know, sitting there because I was scared to death, yeah, and he actually came in and gave me a hug at that point in time. And that was, it's something that really sticks out in my mind. Like having a care when somebody needs you, kind of important. Well,
Scott Benner 15:36
you, I guess you learn that being there for somebody is a way to get life is the way to get love from them, right? Yeah, it's because. It's what other ways did you do? You think you were performing as a child that did not result in a hug?
Unknown Speaker 15:52
I don't quite understand what you're asking.
Scott Benner 15:54
I guess the question is, is like, did you do you? Can you look back and see that you tried other things? Did you try being good at sports and thought that that would make him say, I love you and give you a hug. Did you keep the house really clean? Did you like, were there other things you were doing that didn't result in a hug? Plenty, all of them. Yeah, all of them.
Speaker 1 16:12
No, it's, it's, I don't think I was a terrible kid, and I always kind of tried to take interest in things that he may have been doing, whether it be working on this truck out in the garage or working with him during summers. He owned his own business too, and would go work with them. My sister and I would he treated us well when we're out there, you know, paid us free lunch and gave us food and stuff that we wanted. But it wasn't like, oh, yeah, thanks. This is a enjoyable time. I really enjoyed spending time with you. It was on to the next job.
Scott Benner 16:42
Do you do that as a father? Do you tell your kids that you enjoyed spending time with them? I
Speaker 1 16:48
try not to do things that happened with my relationship with my dad, so I try to spend time with my kids. I try to instill that I love them all the time, give them hugs all the time, and I'm there, I'm the primary type one caregiver in our house, so we have a lot of connection that way. And our daughter, she takes advantage of all this and always wants to go to the grocery store with me, because she'll know that I'll buy her a candy when we check out. So
Scott Benner 17:20
buddy, isn't it? Like, I just realized that you're talking like my son full knows that I love and care about him, and so if I said to him, like, I'm doing, I have a project this weekend, I was like, Hey, I'm gonna be working on something this weekend I can use your hands for. And he goes, I'm probably busy. And he wasn't. It wasn't shitty. It was just like, No, I'm alright. And I realized now, like, if he, if he was, like, running around, going, I hope that guy loves me, he'd be like, Yeah, Dad, I'll help but instead, he's like, No, thank you. I mean, you do see people manipulate people that way. You know what I mean and that. But that's not what your dad was doing. Your dad was just closed off. Yeah,
Speaker 1 17:57
and I think you know he was, he was 69 when he died, so he grew up on a farm, so it's all about work. That's just kind of his life revolved around. Was working? Yeah,
Scott Benner 18:09
I hear you like, Get up, do the thing. I did the thing. It means I love you, because I'm working hard for you. I didn't leave you, I didn't quit my job. I don't drink during the day, like I'm doing the things I'm supposed to do. It's weird that people can't see the whole picture. They just, they get focused on one, like, aspect of it, and like, I'm doing a good job with this. So right? That means I love you. And you know it, come on the other day I my son's back. Like, he left, he finished college, and he went worked a job for a whole year in another city. He was, like, across the country and gone. And then he said to us, like, I've gotten as much out of this job as I can. If I want to move up, I'm going to have to take a different job, you know, I want to come home and reorient myself and look for work again. And so we said, Fine. And he had saved, actually, very proud of him. He'd saved a bunch of money while he was working. And He came home, and he's home now, and it's, it's the end of March, he's been here for three months, and every day I see him educating himself and applying for work, and, you know, talking to people and making connections, and he's doing all the things he should be doing. And I think every day, God, I hope this kid has some success here, like, I don't want this to drag on for him, because, you know, it might get a little, you know, might get a little bit of a bummer after a while. And then my next thought is, I hope he doesn't get a job, because he'll leave. I just took a second yesterday and I said, Hey, I want you to know that every day I see you, I think, Oh, I hope this works out for Cole today. He's doing a good job. It's going to work out for him. It's coming. I'm sorry if he feels badly about it, I said, but man, my next thought is always, I hope you don't leave right? And like, we didn't hug or cry after that, there was no commercial. And then we came back to the Hallmark Channel and, like, talk some more. Like it was just, like, that was it. And he didn't say much, and we moved on. But I know he knows, yeah, and if he doesn't, Jason, I don't know what to do. You know what I mean? Like, I wouldn't know how to. Adjust it like I wonder if your dad thought
Unknown Speaker 20:01
he knows, and then you
Scott Benner 20:05
were over there going, I wish someone would talk to me about this once in a while. It's interesting. Do you ever talk to him about it? No,
Speaker 1 20:13
not really. He wasn't much of a much of a talker. You know, I kind of see that coming from his side of the family too. It's like my grandma is the same way and his dad was the same way. Really didn't talk about it. It was it's rare on that side of the family for somebody to say, Hey, I love you, and hey, come give me a hug. It's kind of weird now with our kids, my wife and I's kids, when we go see great grandma, my grandma, they always insist on giving her a hug, you know, before we leave and say goodbye. And it's, it's heartwarming to see that, and I can kind of see that tear in my grandma's eye whenever that happens,
Scott Benner 20:50
yeah, I wonder if she's thinking, this is what we should have been doing, yeah, yeah. That's, feels like it's too late, but it's not for her, right? She's getting a
Unknown Speaker 20:58
little bit of it, yeah. Okay, so
Scott Benner 21:02
why were you so well managed? If your father wasn't and also wasn't teaching you about diabetes,
Speaker 1 21:11
I think it came down to seeing him not treat himself well. There was a few times, like growing up, where he would have lows in the middle of the night, and the ambulance would come, I would know nothing of it, like no one told me about it, until many years later that you know, the ambulance came. Paramedics came and took him away because he was low and my mom couldn't help him. And after hearing like those stories, that kind of made me want to do better, because I knew it could be avoided with a little bit of effort. Yeah, and also, when my sister was diagnosed, she was diagnosed me, like a year before I was she struggled really hard with it too. That also kind of made me say, this is a my mom. I can't rely on my dad to do this. This is this is me. I have to do
Scott Benner 21:59
it. So you did your sister figure it out? Uh, she wasn't
Speaker 1 22:05
nearly as bad as my dad was with it, but she definitely struggled. She struggled with burnout quite a bit, and she kind of saw the opposite of my dad, you know, she saw the lows or heard about the lows and didn't want to be low so she kind of rode, you know, 131 4150, a lot of the time.
Scott Benner 22:27
Is she having any trouble now?
Speaker 1 22:31
No, she's she's pretty healthy. I don't think she has any any side effects from type one at all. So when
Scott Benner 22:38
you were figuring it out for yourself. Did you ever go to her and say, like, did you try to trade war stories or tips and tricks, or did that not, was that not a thing you guys did together? That
Speaker 1 22:51
really wasn't a thing. I think the one thing I do remember she got moved over to Humalog before I did, you know before that, it was regular, NPH, and when she got moving over to human log, she told me, Oh, this is, this is great. Like, you know, you can actually take it at 15 minutes before you eat. And so then that was, like, the one thing, that tip that she gave me that I actually followed and moved on and enjoyed it, you know, I liked that part. But other than that, we didn't, we didn't
Scott Benner 23:20
really talk about it. Were you close in other ways or not particularly,
Unknown Speaker 23:24
not particularly, yeah,
Scott Benner 23:26
just the girl boy thing, yeah, I
Unknown Speaker 23:28
think so yeah.
Scott Benner 23:29
Did that change as you were adults?
Speaker 1 23:31
I'd say it did not change much until our two boys were diagnosed. Okay,
Scott Benner 23:38
then she fell and then comp, then
Unknown Speaker 23:41
it changed. Yeah,
Scott Benner 23:42
does she have children?
Unknown Speaker 23:45
No, she doesn't. Okay, not biological.
Scott Benner 23:48
Do you so what do you think happened inside of her when she saw your children get diagnosed? I
Speaker 1 23:53
think she saw, you know they were so young when it happened. And you know she loves them dearly. So when she sees something that she struggles with, happened to them. I think it kind of opened up that door. Do
Scott Benner 24:05
you think people realize that when their siblings show affection to your children, like when your siblings show affection to your children, that it's probably the affection they have for you, but it doesn't come out because you grow up together,
Speaker 1 24:20
you would agree with that, yeah, for sure. Really something.
Scott Benner 24:24
And if you are very affectionate, you don't feel like you have to get it out some other way. So interesting, right? Hey, cultural, religious, not cold this. But where does the way that your family interacted? Where does that come from? Do you
Speaker 1 24:40
think? I don't think it's cultural, I don't think it's religious. Why it happens that way? I really kind of attribute it to just our family histories. Like neither side of the family is very, very much out there saying things like, you know, hey, I really appreciate you. I love you. It's more on my. Mom's side. It was a lot of getting people, joking around with people, and my dad's side was very, very, don't say I love you. Get the work done. What were their backgrounds? What do you mean by background?
Scott Benner 25:15
Irish, German.
Speaker 1 25:16
There's a bit of Irish in there. Last name is wierman, so you know, it's about as German as you get. I think that's Irish, and German is incredibly interesting.
Scott Benner 25:26
My mom's parents were German, and you're describing them, you know what I mean? Right? It's interesting. Okay, all right, I got it. Well, how do you manage today? And is that different than how you manage before your kids got type one?
Speaker 1 25:43
It definitely is. Today I am using loop. Both boys are using loop, and we're using human logging those in those pods, using Dexcom g6 that all happened because of the boys when Wesley was first diagnosed. He's our oldest boy. I was still MDI and using human log. And Atlantis, the human log was in a pen, of course. And when Wesley was first diagnosed, 10 years ago,
Scott Benner 26:15
yep, you know, I don't think Dexcom was really a thing. Then, was it a thing 10 years ago? 10 years ago. Arden is 10. She had one then, yeah, you just didn't know about it yet. She
Unknown Speaker 26:28
four, maybe. Yeah, I
Scott Benner 26:30
don't that. I don't remember which one it was, but it existed, yeah, and you were MDI till you were 35 Yep. Okay. And doing well, or just, okay,
Speaker 1 26:42
um, a one Cs were right around six most of my life. Yeah, that's good. And I don't think a lot of that was, there was definitely a roller coasters, like it was, it was probably a roller coaster ride up until I got the Dexcom. Okay,
Scott Benner 26:58
you were always like, chopping down highs and stopping lows. Yeah, so your standard deviation probably was off, but you weren't tracking that right. Yeah, couldn't see it, yeah. How do you see it? Interesting, and doctors told you you were doing great. There was no ever
Speaker 1 27:13
a one. Cs were always good. And blood sugars, you know, on paper, when you tested four times a day, looked good. Yeah,
Scott Benner 27:24
if you test at the right time, everybody, you just have to, just have to catch your blood sugar in the right spot. They have a right before, right before you eat, yeah, yeah, yeah. When you're when your blood sugar is falling because you're hungry and and you've used too much insulin at the last meal, and you test and you're like, Oh, I'm 89 I'm really doing great at this, not really thinking if I didn't eat now, I'd be 60 soon. Yeah. What a flawed system. Okay, so what happens, man, when they're diagnosed, do you just go, this isn't good enough for them, or, like, what makes you dive in and and get the rest of it?
Speaker 1 27:57
That's a really good question. I don't remember the exact epiphany moment, but it probably centered around seeing something on social media, and when we dove in, like with Wesley, like we dove in, it was as soon as I kind of figured out what the Dexcom was like, our doctor had mentioned it to us, but, you know, I had done many, many years MDI and just a tester and did fine stuff like, well, what is this technology like? Is it? It's nothing, right? But after seeing online, on social media, you know, seeing what the Dexcom could do, and then what I really saw was the Dexcom g4 attached to a cell phone and night scout and being able to see numbers remotely, I think that's what kind of made me dive in. Yeah. And then after that, it was like hardcore diving in.
Scott Benner 28:56
And so what does he start with? A pump, a CGM or how long was he MDI?
Speaker 1 29:02
He was MDI for maybe a year or so, year or two, okay? And a lot of that had to do with because he was using such little insulin, like none of the pumps OmniPod could not deliver, uh, insulin in small enough amounts at that point in time, right?
Scott Benner 29:19
And that's the same thing that happens to a lot of people. They're like, well, just do shots. Because meanwhile, the shots are, they do a unit at a time. And, you know, if you have half unit noodles and your kids small enough, that's still not enough or small enough. So it's interesting how we were
Speaker 1 29:34
doing, we're doing like you were doing, you know, seeing how much you could, like, pull back a quarter of a unit. Yeah, we did that for a long time. Had syringes that could do half units, and then ends that could do half units, okay,
Scott Benner 29:46
and then probably about the time you're figuring out a pump for Wesley, then your next son is diagnosed. Yeah,
Speaker 1 29:53
we had moved across the state, and I was still doing business, you know, in our Old Town. It's about two hour drive away. I was over there for a meeting. Wife had called me and said, uh, she had checked Cooper's uh finger, because he had went through his diaper the past couple of days, and that morning it was super heavy. And she said, Well, I checked his finger, and it was like, you know, 450 you know, at that point in time, my heart just dropped, and I said, you know, why don't you guys? I'll call my mom and I'll have her come over and pick you guys up and drive over to where I was at, because that's where our other boy had gone to, the endocrinologist at over university of Iowa Hospitals and Clinics, which is, you know, our best hospital in the state for type one. And said, Hey, drive over here. While you're driving over here, give him, like, a quarter a unit of insulin to bring him down. And that's what happened. He came over, and family came over, and we went through that hell all over again, yeah,
Scott Benner 30:56
so soon after the last time too. The thing is, Jason, that's not why you're on the show. I just wanted to get I just wanted to get your background so for everybody, so they knew who you were and what you're living through. But you really wanted to come on today to talk about something completely different. So why don't you express to everyone why you're here? Well, last year, which would be
Unknown Speaker 31:23
January, ish, 2023 my dad and mom. Type
Scott Benner 31:28
one diabetes can happen at any age. Are you at risk? Screen it like you mean it. Because if just one person in your family has type one, you're up to 15 times more likely to get it too. So screen it like you mean it. One blood test can help you spot it early, and the more you know, the more you can do. So don't wait. Talk to your doctor about screening tap now or visit screen for type one.com to get more info and screen it like you mean it.
Speaker 1 31:58
Both got covid. My mom was able to, you know, to kind of maintain she didn't have very bad symptoms. But my dad, because of his type one diabetes and his health history, because of type one diabetes, we should probably talk about that slightly here. I think most of his life, his a one Cs were, you know, 1011, 12, just because of poor management, yeah, and that had a significant impact on his his health. Like he was a healthy guy. If you looked at him, he's tough guy, skinny guy. He had quadruple bypass. And then probably 10 or 15 years after that, he had like four mini strokes, and everything kind of went downhill after that. And after the strokes, he kind of felt worthless, but didn't get around much, didn't try to rehab much, because, you know what? What good was he if he couldn't do work type of thing? What kind of work did he do? He was an electrician. He had his own electrical business, and then he also worked at a company that makes gigantic industrial valves. Okay? He was a hands on person that got down and dirty, right? And you describe him as robust,
Scott Benner 33:16
but with a one sees in double digits, exactly. Yeah. So it's funny as you're trying to talk about his physical characteristics and his health, what I really thought was, I wonder if he would have told you he loved you, if his blood sugar was lower, that very well could be, yeah, I wonder if he would have had more mental clarity and and and seen things differently.
Speaker 1 33:37
Very well could be. You know, kind of mention that, like, after he kind of switched from MDI the majority of his life over to OmniPod five, he seemed to take a lot more interest in type one, and he seemed to soften up a bit, and as a 1c, had dropped down to like, seven, yeah, plus
Scott Benner 33:58
he had something to focus on again, and a thing that he needed to be good at and learn and, you know, right work at. Yeah, it's interesting. Listen, there's a chameleon sitting behind me in a cage right now, because my kids grew up and I don't have anything to take care of. So I got very like, stir crazy very quickly, just trying to take care of all you guys wasn't quite enough for me. I was like, I needed something alive in front of me to, like, work on and study and and, you know, figure out what it needed. So, oh, all right, well, did that give you some time with him? I'm gonna say no. You know, my dad's
Speaker 1 34:35
the type of guy that would if you needed work done. He was there immediately. So we had an old house at that point in time, and he would come over frequently to kind of help me with things around the house and share His love with me that way. And even after he had a stroke, his first stroke, like we had a huge windstorm roll through town, and it like knocked over trees all over town, and our big tree and our. Backyard. It fell over, and he came over even, you know, suffering the consequences of a stroke where he can't move half his body very well with chainsaw. And we're, you know, chopping the tree apart and taking it down. And he was just trying to do his part, you know, trying to help me and the family. Yeah, wow. Well,
Scott Benner 35:21
I mean, listen, clearly he loved you. He just didn't, yeah, yeah. He just didn't say it the way you were hoping for, right? But look, look what it did for you. You're really open with your children and your family, I bet, with your wife too. And you know, don't worry, that'll slingshot the other way, and your boys will be quiet, strong men who won't say anything to anybody. You'll just bounce back and forth through all of eternity getting back to your dad's health. And really the reason you wanted to be here, you know, your note to me is very simple, just that, you know, talking about hospice care and type one diabetes and being older with type one was something you want to talk about, and I know we don't talk about it enough. So I'm very interested, what, what was the, you know, what was the course, what, what happened? So after, after, my
Speaker 1 36:11
dad was in the hospital with covid, he was there for the probably a week or so, and just was not getting better, and we didn't go see him. So I was just talking with my mom over the phone, because I didn't want to get covid. Yeah, my mom had said, you know, this is not looking good. You know, I'd call him every day, talk to my mom every day. And my dad really wasn't able to talk while he was in the hospital doing this. He had his OmniPod five on. He's working great. And my mom said, you know, he's not eating much, and he's got a super flat line, and it's like at 100 all day long, all night like, well, that's great, but we need him to eat. You know, kept saying we as soon as you can, you gotta probably get over here and after his, after his 10 days of being quarantined, my wife and kids and I went over there and saw him, and he's just kind of laying there, kind of comatose, not really knowing what's happening. He'd look at us every now and then, but quickly, you know, close his eyes and just go back to sleep.
Scott Benner 37:10
The hospital staff, because
Speaker 1 37:11
he was on his OmniPod five, they would not deal with that like they wouldn't touch it or interact with it. So my mom had to do all the, all the stuff on it, whenever something would happen, she had to change the pods, enter carbs, if he was eating anything, or do any corrections. So she was left in charge of that because the hospital staff refused to be involved, refused to be involved with it. And they also wanted to know, you like, how much insulin he was getting for different things, you know, whatever. If he feed some crackers or whatnot, they wouldn't know how many, how much insulin he was getting for those crackers. You know, it's kind of hard to say to my mom, you know, you can't really tell him how much insulin he's getting because the algorithm is algorithming. It's doing its thing, right? So they had no clue or idea on how to deal with a pump in that setting, probably
Scott Benner 38:03
Jason. They probably don't understand how to deal with it out of that setting, either. But yeah, yeah, we'll learn about that here shortly. Yeah, and they, and they weren't interested. The bigger, the bigger point is, is that they're not interested. They're going to chart what they need to chart, but like, they're not going to touch it. They're not going to learn about it. That's not going to be a focus for them. When you said he was kind of comatose, like, this is after 10 days with covid, after his quarantine period, yeah.
Speaker 1 38:30
Like there towards the end of the his covid stay for 10 days, like he just would not recover and kept sleeping more, just laying down more, not sitting up much, not opening his eyes, not talking.
Scott Benner 38:43
What did you think was happening at that point?
Speaker 1 38:46
Part of me, you know, was hoping that he would make it through and be able to, you know, return to somewhat normal life where it was at that point in time. But the other side of me knew that this is probably his last, last little bit of life that he's going to be spending in this hospital. Yeah.
Unknown Speaker 39:04
How long ago was this?
Unknown Speaker 39:05
Just last year, January, okay,
Scott Benner 39:07
did you cognitively understand that his heart attack and his strokes were from from high blood sugar support management? Yes, okay,
Unknown Speaker 39:15
like 100% All right. So
Scott Benner 39:17
you know, there's still other things happening inside of him that are also being impacted by that, and have been for decades, and now, exactly I know this comes along, and it's stressing every system, right? You know, what did you mean by? I'll find out more. What happened next
Speaker 1 39:32
after his 10 days, it kind of deciding shortly after that that they're going to call in hospice care, because, you know, he's struggling to breathe, he's not eating, he's he's not he's not trying to live. The hospital staff decided to move over to hospice care, and my mom said, Yes, that's, it's, it's his time, like it's going to happen. So let's go ahead and do that. And once they moved him over to hospice care, you. They, you know, stopped all medications besides morphine and that unfortunately included insulin. Stopped giving him insulin after his last pot expired, and really didn't take any care or concern about his blood sugars. At that point in time, they would check his blood sugars, but you know, it'd be every three four hours, and there's no response to the high blood sugar until I showed up at the hospital.
Scott Benner 40:33
So I've watched a hospital manage my mom to the end of her life. So if once they decide you're not coming back from this, they start removing all the things that keep your body going. And it's interesting when you're when you're older and you've been sick for a long time, you don't think of it that way while you're alive, and you're going like this, pills for my blood pressure, this pills for my you know this, and you know my lipids and this is happening, and what you really, like, begin to understand in that time is that you have been artificially kept alive for so long. Like you weren't gonna die, like, if you stop taking all your medication and doing all the things you're doing, you weren't gonna, like, just shut off, but the end of your life was going to be sped up without your heart medication or etc, whatever else you're taking. And then it's such a weird feeling when someone says we're going to discontinue those things. And you think, but those are the things that are keeping her healthy, right? And then you're like, oh, even though I knew this is what we were doing, I didn't know this is what we were doing, right? Like, we're gonna take away all the things that are keeping, keeping this person alive, and to to to hasten the end of their life. You're trying to get to it faster, because it's just seems cruel to, you know, if, if the end is the end, and they're struggling, or, you know, why? Why would you keep that going any longer than you had to? Right? So you get to that situation, but the taking away the insulin, and you not live with it like, what is that about there in
Speaker 1 42:11
my eyes, from, you know, being type one myself, from my, from my point of view, like a high blood sugar is insanely uncomfortable, especially when you get up to like, 400 or 500 you know, you get that, that thirst sensation that's unquenchable, like you have to drink something. In my eyes, when he was in hospice, you know, they wanted him to be comfortable. You know, they're shooting him full of morphine to make him comfortable, a little bit of insulin to bring him down to a normal, somewhat normal level would make him more comfortable. I don't think it's like a blood pressure medicine or something like that, that you know you don't feel it when you take it. You don't feel the results of it. You're not going to be uncomfortable if you don't take that medication for a day or two days or three days, but if you're doing multiple days or multiple hours without insulin, and that blood sugar is, you know, 400 500 600 that's incredibly uncomfortable, yeah, and I don't think anybody really thinks about that. I don't think the hospital staff thinks about that. I'm not even sure if his doctors thought about that. And I would be curious as to, like an endocrinologist thought on that, like, Is that comfortable? Is it something that should be dealt with? Yeah,
Scott Benner 43:29
but he was on morphine, right? Yep. So do you not think that they were just trying to hasten things by removing the insulin? I don't think
Speaker 1 43:39
that crossed their mind, like them, thinking of DKA wasn't on their radar.
Scott Benner 43:45
And did you speak to them about that, or was that just your feeling? I
Speaker 1 43:48
spoke to them about that adamantly, and that kind of explained my point of view, and we finally got them to come in and just give some small correction, small corrections throughout this last few days and kind of get them down to a moderately okay level. But it was hard. It was really, really difficult to get them to do anything. And when they decided, you know, hey, we're going to do something, well, we agree to giving him insulin. You know, it took him two, three hours to come back in with the insulin to give it to them. It was really slow.
Scott Benner 44:25
Can you describe your state of mind during this time?
Speaker 1 44:28
I was extremely pissed off, because I'm used to, you know, I'm used to dealing with type one diabetes like now, like you deal with it now. You don't let us sit you don't, you don't do that. And just seeing how slow the process worked, there it was infuriating.
Scott Benner 44:47
You think you were mad because you couldn't help your dad, and you were looking for a way to help him. Yes, yeah. Did they ever say to you were mad? Edging the end of his life. Now we're not going to give him insulin.
Unknown Speaker 45:02
Yeah, that was their their perspective on it.
Scott Benner 45:06
What was yours though? Like, you knew that was happening. Were you okay with this? The what, what was being done?
Speaker 1 45:11
I wasn't okay with it at all. Like, I just can't, like, even, even if he was on morphine and out of it, not really aware of what was going on around him. I can't imagine your body not saying to you, hey, you're really thirsty, your mouth is really dry right now, and you might have a headache, you might feel like you gotta puke, you might feel all of these things, but you can't do anything about it, because you're you're locked in this bed, and you're locked inside your body, right, just sitting there, and you can't do anything about it.
Scott Benner 45:43
Were you okay with the idea that he was dying like, like, and that the plan was he was in hospice now to get to the end of his life, or did you think he should be fighting
Speaker 1 45:53
after seeing him in the hospital, after he kind of had his quarantine from covid, like, I knew that it was coming, like I could see it coming. I think kind of, I made it a little bit easier to deal with, but I still didn't want him go through that process and suffer from type one diabetes still.
Scott Benner 46:12
Yeah, okay, so that's really the aspect of it. Like, not that you're okay with his passing, but you're okay with what we're doing. I know what we're doing. He's he's gonna pass away. We're managing towards that. But just like emotionally, psychologically, you couldn't stop taking care of his diabetes,
Unknown Speaker 46:29
right? Yeah,
Scott Benner 46:32
you know. Why do you have any thoughts about it? You go to a therapist. Anything? No,
Speaker 1 46:37
no therapy. I just listened to that episode of the podcast with the therapist on it. So that's mine. Oh, yeah, sure. I'm
Scott Benner 46:43
sure she'd be thrilled that that's your therapy.
Speaker 1 46:47
Hey, the ground, the grounding method helped me tremendously. So thank you for recording that episode. Oh, did
Scott Benner 46:52
it really? Oh, that's fantastic. Yeah, good. I'm glad. Oh, you're stuck in this conundrum where the plan is we're going to take away my dad's stuff. He's going to pass away, but I can't let it be as his insulin. So did you, you talk them into giving it to him eventually?
Speaker 1 47:06
Yeah, we, we talked to him. I really had to push like my mom was, you know, out of it. She had just recovered from covid and dealing with, you know, her husband passing away, or in the process of passing away, she was just kind of there, nodding her head, agreeing with everything, and not necessarily always remembering what she agreed to. But I finally convinced her to say, we really need to do something about this. Can you please ask, you know, the hospice care people and the doctor or nurse whoever to come in and let's talk about this. You know, I kind of, when they came in, you know, I kind of put my foot down. I said, you know, having a blood sugar this high is not comfortable, um, and you guys want them to be comfortable, so we're going to do something about it. And, uh, eventually, you know, that, they said, okay, and then, you know, three hours later, they come in and do something about it.
Scott Benner 47:59
Yeah, it's tough, because they don't get very assertive. But, like, they could have made the argument that DKA could could help him pass away, right? It's such a weird thing, like you're turning the body off, you know what? I mean? Like it the person's dying to begin with, and you have all these artificial things in place to keep that from happening. So they take them away. It's interesting. They must have seen you must have been really pissed, I guess, is what I'm saying. Yeah, you must have scared them into doing it. And they probably thought he's going to die one way or the other if we give him this insulin or not. So let's just make the family happy and do this. Yeah?
Speaker 1 48:32
And that's kind of like my point of view on hospice, is that, yeah, make make the patient, the person dying, happy or comfortable, and you gotta make the family comfortable. Also, they gotta be comfortable with the process. Him suffering from high blood sugar along with dying wasn't something that I was willing to really compromise too much on,
Scott Benner 48:55
yeah, well, and you didn't. So after you got the insulin, what happened afterwards? They keep managing the insulin he wasn't obviously eating where they and they took his intravenous or his IVs away as well, right?
Speaker 1 49:09
Yep, yeah. They took all that away so they would just come in, you know, every however many hours in between, checking his blood sugar, coming back, you know, 3040, minutes later, to give him a small correction dose. And of course, you know, I agree with, agreed with them, that we shouldn't try to bring him down to a normal level, because he can't eat or drink anything at this point in time. So it's just try. Hey, let's use them close to 200 so they they'd come in quite a bit, quite a bit, quite frequently after that, and just give him small correction doses.
Scott Benner 49:43
How long did he? Did he last after that?
Speaker 1 49:48
So he was in the hospital like a total 25 days. 10 of those were heavy covid stuff, and then 15 of those were two. Kind of all downhill from there, type of thing. Yeah, and I think it was in hospice care for probably just shy of a week.
Scott Benner 50:07
How were you there all the time? Or how did you guys manage the that?
Speaker 1 50:12
No, we weren't there all the time. We went over there. That's a like an hour drive from our house to where there the hospital was at so we drive over every day and see him, because we know we have three kids that are still in school at that point in time, yeah. So we had to kind of maintain a somewhat normal life. And you know, my dad being the workaholic guy, he would have agreed with that. He would have been okay with that, okay
Scott Benner 50:38
with it. He would have been like, what are you doing here? Staring at me. Yeah,
Speaker 1 50:42
that's that. That's exactly what he would say, yeah,
Scott Benner 50:46
make some money. Help somebody. Yeah.
Unknown Speaker 50:48
Help somebody. Do
Scott Benner 50:49
something. How they're going to know that you love them if you're not working exactly? Oh my gosh. I have nothing but sympathy and and respect for the the process. I can tell you that in my mom's hospital room, at one point, I sort of just went to a corner where I wasn't in her sight, even though I don't know that she could have seen me to begin with, and I don't know how to explain that, I silently screamed and gritted my teeth so hard I thought they were gonna break, because I was had come to the realization that there was nothing left to do, right, you know, and that was a terrible feeling for a person like myself, you know, who you know seems to be minded towards caring for people to begin with. And you know, just as her son and, you know, and my brothers were there and I, I had grown up in a very hybrid situation where I was parenting my brothers and their brother at the same time. So now we're, you know, now we're there, and I'm in my 50s, and my brothers are, you know, in their 40s, and I still feel like, on some level, those are, they're my like they need me to say something or do something, or be something, and at the same time, I'm having my own very personal, you know, experience. And it was, it
Unknown Speaker 52:08
was very
Scott Benner 52:10
upsetting. Is not the right word, but I thought I was going to break my teeth while I was silently screaming it through my chest, is what was happening. Yeah, you know, it's just maybe, I mean, I don't see how anything's worse than this, you know,
Speaker 1 52:25
yeah, it's a it's a weird trip to uh, lose a parent. It's uh, it's just something you don't, you can't know about until it happens, right?
Scott Benner 52:35
It's not something you can prepare yourself for. So if it happens to you too early in life, I can see where it would really just get to you in a different way. And even though I was 50 and had lived through my kid getting diabetes and all the other things that had happened, I do think I was more prepared for it because of that, but I'd say that when it's over, your perspective levels up again. And I thought I had some pretty high perspective from living through type one diabetes, and, you know, every day realizing that a little too much of this at the wrong time. And you know, that could be it like, even last night, I'm still trying to adjust Arden's insulin back properly, because she's using that. GLP, yeah, and she got into the mid 50s last night at like, 130 in the morning, and I let it go for a couple minutes, and like, she's not seeing this, I texted her, and she didn't answer me. So I got out of bed and I walked into another room so I wouldn't wake up my wife. And I called her just to arouse her and get her awake. And she texted me, and I said, Hey, just like, drink a half of juice. But in those couple of minutes, like the couple of minutes where you're like, she'll be okay, she's low, but she'll be okay, okay, she's not taking care of it, like, she's not waking up. I'll wake her up. I woke her up. That's good. She drank something. I see her blood sugar coming back up. That whole time is only like, 10 or 12 minutes, you know. And in that time, like, standing there with my phone in my hand, I thought everything in my house looks so normal right now, like everything looks like every other day I walked downstairs and let the dogs out while I was doing this, like, but is Arden gonna die right now? Like, you know what I mean, like, and I don't think about it that way, day to day, but last night, I was probably just the right mixture of woozy, a little asleep, a little awake, where I didn't, you know, manage myself that way. And I thought, wouldn't it be weird if, like, everything was so normal in the world, and she just disappeared, and you know what I mean? And and then i She's like, texting me. She's like, I drank it. I'm like, Okay. And then I was like, Yeah, she'll be fine. But a lot of people don't live in that space, you know, and so I thought I had some pretty massive perspective about what's important in life and what were to focus and those sorts of things. Then my mom died, and I thought, Wow. I didn't think I was going to be able to level up. But here it is, I hope. Nothing else terrible happens, because I'm good with where I'm at now, as far as perspective, I don't need any more, you know, but I don't know. Maybe more will come. Still, Jason, I'm not sure. Yeah,
Speaker 1 55:10
something that similar thing happened to me too. Like, you know, the past year my dad's health, it's just been terrible, and watching him kind of start falling down that ladder ramped up my anxiety. You know what really kind of got my anxiety really wound up is thinking, what, what if I get low and I die? Or, what if I get low and crash the car and die? Who's going to take care of my family, like, who's going to be there for them? And that's a it's a hard, it's a hard thing to think about. Do you think you're
Scott Benner 55:42
examining your mortality in that, or do you think you're reacting to the idea that your father's gone? Because you know before that, if you would have died, he would have taken care of your family.
Speaker 1 55:52
I think it was just it's amplified by him having these health issues and seeing him being the guy that if you needed something done, you call him at that point in time. You know, I wasn't able to call him anymore because he couldn't, couldn't do these things for us anymore. So it's kind of like I'm stepping up into that role.
Scott Benner 56:12
Yeah, it's me now. There's nobody behind me anymore, right? Yeah, the way that happens to me is I imagine everybody I've ever been related to, standing in a line at a cliff. They fall off the cliff as they die. And then my mom, my mom went off, and I was like, Oh, I'm next. Like, there's no one in front of me in this line anymore, right? You know, that was the thing that got me. I was like, there, you know, it's my dad and my uncle and my aunt and like all these people, even though I wasn't even that close to them, like all these like all these people, like, I felt like if they were alive, I was going to be alive, because age and chronology, you know, etc, even though that's completely ridiculous, I'm sure the guy standing on that bridge in Baltimore didn't think they were going to die right before that, yeah, but um, but in my mind, that's always what comforted me. I'm like, there's more people to go before it gets to me. And then my mom, my mom passes away. And I'm like, there's no one left standing between me and the edge of this cliff. And, yeah, that's when you start doing things like, you know, trying to put away more money, and talking to your kids about stuff that you're like, they're probably like, Why the hell are they explaining this to me, like, that kind of stuff, you know? Yeah. And actually, it's funny, my dad left my mom, and I can look back and see that he was planning it for a while. And the one way that I really like, like, this kind of touch point for me is I was like, I don't know, I was 12, and he drugged me into the basement one day to explain how the fuse box worked. And, like, I remember the time thinking, like, this is cool. My dad and I are doing something together, you know what I mean? And like, trying to understand the fuse box. And I felt like I did understand it. And I was like, Oh, cool. Look at me. Like, there's they were the old screw and glass ones, you know. And, well, you know, your dad's electrician, like, and I was like, Oh, wow. And then I look back some years later, and I think, oh, he was just explaining to me how to take care of the house because he was going to leave. And I don't know that it's any different with dying, except maybe you don't plan to die, you know what? I mean? Yeah, yeah. So, yeah, I've
Speaker 1 58:16
been, I've been slowly doing that, like, ever since I started really feeling that anxiety, like slowly dropping those little hints or knowledge on my wife, like, you know, if you need to take care of this with loop, this is where you should go and look at it. You want to look at it? And she'd say, No, of course, but,
Scott Benner 58:34
but you're thinking, look at it, in case my body explodes and I'm not, unexpectedly, that's right, yeah. Now that's, uh, how are you making out getting through that anxiety?
Speaker 1 58:45
Well, you know, after learning about the grounding method from the juicebox podcast, subscribe, turn downloads on that stuff. I that that episode on grounding, I probably have listened to that 10 times. No No kidding, I've kind of picked out things within that, those grounding methods that kind of really helped me, and I've gotten pretty good at making it happen quick when I start to feel that anxiety, come on. So, you know, I can usually just look at something, and I kind of start describing it in my head. I would feel how it would touch, how it would feel when I touch it, what it smells like. And it kind of calms me down to a point to where I can let my mind move on to something else.
Scott Benner 59:29
It's episode 913 it's called the 54321, method. And it's just Erica, who's the a licensed marriage and family therapist who she has type one diabetes for like forever, like over 30 years, and I have her on to talk about this kind of stuff. It's where I like, where we pick a topic, and then normally it devolves into me talking about how I feel. She and I did this, this grounding method. What is it? It's five things. You can see
Speaker 1 59:59
we're. Things You Can that's, it's like, see, touch, you know, feel them, something, those five things, just to get your mind to focus on something else. And they and I really, I just kind of picked out of those methods, just like, What things would feel like if I were to touch them, just the general shape of things and things like that. That kept that really helped me.
Scott Benner 20:00:21
Yeah, the 54321, method involves identifying five things. You can see, four things, you can touch, three things you can hear, two things you can smell, one thing you can taste. And by doing so, it shifts your focus from anxiety provoking thoughts to a present moment.
Speaker 1 20:00:36
And it works for you, huh? It most definitely works for me. That's very cool. Well, it's
Scott Benner 20:00:40
a shame you're not gonna have any more kids, because I think we could have got a Scott out of you, for sure, but I
Unknown Speaker 20:00:49
would have named him Dave, go with it. Yeah, you
Scott Benner 20:00:51
know what, honestly, would have been the way to go. Well, I'm grateful that that it helped you. I wish you knew. I wish you guys all knew that most of what the podcast is is the thoughts that I have standing in the shower in the morning. And I think I bet you people would want to know about this. There's no production meeting or anything like that. Nobody's telling me what the like do or say. I just one day I got it in my head. I was like, I heard about this method. I watch people do it. I thought, boy, that makes sense. And then I listened to some people online talk about it. I was like, Wow, this helps a lot of people. I'm going to ask Eric if she knows about this, and like, really was the extent of it, and to hear that it made it all the way to Iowa and to you, and that it was valuable for you while your father is passing away and and you know, afterwards, it's very heartwarming for me. So I appreciate you sharing that with me, because, you know, day to day, it just feels like I sit in this room and click on things and, you know, and talk and make sure this thing's in front of my face when I do it. That's right, yeah, but to know that it actually works out, like I'm working on something now for the podcast, for like, later, it's a lot of work. Like, I'm not gonna lie to you. It's like a lot of me sitting here and talking to myself, I'm not gonna tell you what I'm planning yet, and it's hard. It's hard to get the energy up for it. It's hard to have an engaging conversation by yourself in a room, one of those things, like, anybody that can do that. I have a lot of respect for stand up comedians like even get feedback, you know, from a crowd. But even though you can make the argument that they're on their own up there, but I am not getting any feedback, so I have to kind of imagine how you feel while I'm doing it. And I slowed down on that project because it's just such a slog. Yeah, you know, you saying this to me, honestly, will help me get energy up to to finish it up and get it out to you guys. It's a ton of I almost curse, but it's a ton of I'm gonna curse anyway. It's a ton of work, and I don't get any like, nobody at the end of the day is like, you're doing a good job, or try harder, or do this differently. I just, I'm like, on my own to figure out what it is anyway. I appreciate it very much, and it'll be helpful to me. So thank
Speaker 1 20:02:59
you. Yeah, well, keep, keep taking showers, Scott, and keep coming up with good ideas. Well,
Scott Benner 20:03:03
hell if I stop taking showers. We have bigger problems than the podcast falling apart, right?
Unknown Speaker 20:03:09
Keep taking showers.
Scott Benner 20:03:12
Oh, my God, Jason, you just named the episode. Yeah, there you go. Well,
Speaker 1 20:03:17
we need you to keep coming up with good ideas. And I'll, I'll keep, I'll keep posting in the Facebook group. Try and help people and help you come up with ideas. You're definitely doing, like a real job. You gotta think of like all those like podcasters, YouTubers, these jobs didn't exist 10 years ago. Yeah. So it's hard to, I think it's hard for some people to say that what you're doing is a job, and you deserve compensation for it. You definitely do, and I think you're doing a fine job of it. And thank you. You know, top of the game, type of type of job, and I think you deserve to be paid. And however you get that money? You get that money?
Scott Benner 20:03:54
Well, I'm not human trafficking people like P Diddy, allegedly. So Right?
Unknown Speaker 20:04:00
So you're just taking money from OmniPod and Dexcom and cozy Earth. And
Scott Benner 20:04:05
I'm older, so I'm still slightly embarrassed to be a podcaster, not embarrassed, but like, there's a little piece inside of me that's, like, you don't really that's not a real job. Like your dad, it's your dad would think I'm doing a weird a real job. Yeah, yeah. And my dad, you know, it's funny, my father, while not an electrician, did all the electrical work at the rubber molding plant that he worked at, like so your dad and my dad were pretty similar people as far as what they did for a living. He worked in an industrial situation, big, heavy machines that it was his job to take care of and keep them running. And then when that, when nothing broke, they would just point him to the floor, and he'd go work on the floor. And, you know, like he was the maintenance supervisor. But I also, there were days he came home where he just, you know, he did the grind too, like he, you know, they put him in front of a machine and said, you know, make 10,000 of these things come out of here by the. End of the day. I think if I would have told my dad, you know, that I'm gonna do this, I think he'd be like, What do you mean? Like, you know, like, go do something. Like, go work on something. My mom never understood exactly what I was doing. Like, she was older by the time I was really at it, and she's just like, she knows I talk to people, like, through the internet. Like, that's basically what she understood about it. And I think my kids make fun of me because I feel like I have a 12 year olds job. Like, you know, like, it's funny. Like, to older people, you're not really working, and to younger people, they're like, oh my god, are you and are you on tick tock right now? Like, I get notes all the time. Please stop doing this. Like, or they'll send me, they'll send me links of myself, like, trying to get people to listen to the podcast. Like, don't do this ever again. I'm like, and I'm like, look like, if you can get people to listen a different way, like, let me know what it is. But right now, this is how the world works. And you know, I'm stuck standing in front of a light, talking into my phone, telling you that episode, whatever came out today, and you should check it out. Yeah, anyway, I appreciate you very much. Is there anything we didn't talk about that we
Unknown Speaker 20:06:07
should have? I don't think so. I think we, we hit the hits all the bases. Aaron got him. Yeah,
Scott Benner 20:06:12
well, I'm so glad you said keep taking showers, because I was like, I was down to, like, using the word hospice in the title. And I was like, Oh
Unknown Speaker 20:06:19
God, no one's gonna listen to that.
Scott Benner 20:06:23
Just gonna be like, No thank you. Not on a Tuesday, but it's just very important conversation. Jenny said to me the other day, we were doing a just a pump. I think we did, like a pump and CGM overview. I think we did, that's how much I do this. And during that, she said, Are we going to talk about, you know, older type ones and how these, none of this technology is made for their fingers or their eyes, you know, or their ability to work on stuff? And we, you know, we talked about it for a minute, but like, there's not much to talk about. Like, because what are you saying to a pump company like, go make something for a person at the end of their life, and they're gonna say, oh, they'll get somebody to help them with it. Like, we can't just make a product for that small number of people, but it's still a big deal. Like, you know what I mean? Like, you're gonna get older one day and your fingers are gonna shake, and, you know, if you're lucky, they're just gonna shake. And how are your eyes gonna be? And how are you gonna understand that? Could you understand? Do you think you could have taught loop to your father, absolutely not, yeah. So you know, when that becomes the standard of care and algorithm, like, how do you, I mean, he made out okay on OmniPod five, though, right?
Speaker 1 20:07:32
Yeah, he, he did. But I think a lot of that had to do with my mom helping him his like, I think a lot of that comes down to his mobility, too. Like him being an electrician for the majority of his life, his hands were beat the shit, yeah, so they could hardly register when he touched a touch screen. You know? That thought he was dead already, and so she had to do some of the button pushing for him when it wouldn't work for him, and he didn't have the dexterity in his hands to put pods on. So she had to do that for him. Yeah. So it kind of, you know, shows that some of these things are need to be taken into consideration with an aging population, or a population that doesn't have the that mobility or ability anymore. Listen,
Scott Benner 20:08:20
I worked in sheet metal from the time I was 16 until I was in my 20s, and you know, it wasn't even that long, and the skin on my hands is still like, it's hard to put into words, like I haven't done a real job in a long time, and my fingers are still very dry all the time. Stuff slips out of my hands a lot, if that makes sense or not, but whatever Spider Man has, I have the opposite, you know, and it's I was always touching, you know, this is back before people paid attention to things. My hands were like, we used to wash our hands and paint thinner.
Unknown Speaker 20:08:53
Great, yeah, my dad did that, yeah,
Scott Benner 20:08:55
you know, of course. Like, how do I get this grease off me quickly so I can go eat lunch? Paint thinner, yeah, you know. And then they finally came out with that soap that scrubbed it off. And, you know, you're like, oh, wow, look at the advancement here in my life. I'm not using paint thinner anymore to clean my hands. There are still days I think I'm just gonna wake up with lung cancer one day and I don't smoke or bleed, an unhealthy life at all. But I worked in that place long enough I'm like, hopefully it's not going to get me. But, you know, I don't know that it can. I mean, I worked in the industrial situation before people were like, you know, wear your personal protective gear.
Unknown Speaker 20:09:33
They were right, yeah,
Scott Benner 20:09:35
I made $5 an hour.
Speaker 1 20:09:38
Well, maybe that's why, man, that's why you have your good podcast voices from breathing in all that you shouldn't be breathing in.
Scott Benner 20:09:43
Wouldn't that be great? The thing that propelled me at the end also got him. We'll need somebody to write that on my tombstone. Anyway, Jason, nothing like talking about death with a with somebody at 9am this was great. It was Yeah. I really did appreciate though, and I appreciate you. I imagine you know that, but thanks very much
Unknown Speaker 20:10:04
for doing this. Yeah, no problem. It was a pleasure.
Scott Benner 20:10:07
Hold on one second.
Did you know if just one person in your family has type one diabetes, you're up to 15 times more likely to get it too. So screen it like you mean it, one blood test can spot type one diabetes early. Tap now talk to a doctor or visit screen for type one.com for more info. Arden started using a contour meter because of its accuracy, but she continues to use it because it's durable and trustworthy. If you have diabetes, you want the contour next gen blood glucose meter. There's already so many decisions. Let me take this one off your plate. Contour next.com/juicebox a huge thank you to ever sense CGM for sponsoring this episode of the podcast. Are you tired of having to change your sensor every seven to 14 days with the ever since CGM, you just replace it once every six months via a simple in office visit, learn more and get started today at Eversense cgm.com/juicebox, hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast. The episode you just heard was professionally edited by wrong way recording, wrongway recording.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1291 IDU: How do GLP meds work
I don't understand… Why the type 1 guest from episode 1230 doesn't need insulin anymore. What did the GLP do?
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome back to the juicebox podcast. Ready to have some fun?
Jenny's back for another episode of I don't understand. Did you like the last one? I hope you did, because there's gonna be more of Jenny and me and other people not understanding things and us figuring it out. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan. This episode of The juicebox podcast is sponsored by the Eversense CGM, an implantable six month sensor. Is what you get with ever since, but you get so much more exceptional and consistent accuracy over six months and distinct on body vibe alerts when you're high or low on body vibe alerts. You don't even know what that means. Do you ever sense cgm.com/juicebox, go find out this episode of The juicebox podcast is sponsored by us med. US med.com/juice box, or call 888-721-1514, US med is where my daughter gets her diabetes supplies from, and you could too use the link or number to get your free benefits check and get started today with us. Med
Today's episode is sponsored by Medtronic diabetes, a company that's bringing together people who are redefining what it means to live with diabetes. Later in this episode, I'll be speaking with Mark. He was diagnosed with type one diabetes at 28 he's 47 now he's going to tell you a little bit about his story, and then at the very end of the episode, you can hear my entire mini interview with Mark. To hear more stories from the Medtronic champion community, or to share your own story, visit Medtronic diabetes.com/juicebox and check out the Medtronic champion hashtag on social media. We're gonna do something here today. We're gonna try to figure this out together. Because I don't understand this, and I don't know if you do either. Okay. Now this is actually coming from a listener, so I'm gonna read, I'm gonna read their their question. But okay, truth be told, I don't understand this the way I should. I don't think you do either, and let's see if we can figure it out together. Did you hear episode 1230 with the gentleman who had type one diabetes diagnosed at age 50, and now at age 58 on Manjaro is not taking any insulin at all
Jennifer Smith, CDE 2:40
I did. I listened actually. I did listen to that episode. That's perfect, because
Scott Benner 2:44
this gentleman says, with regard to podcast number 1230 where the T 1d guest says he has been completely off of insulin for two years due to being on a GLP one medication. How does his body get nutrients without insulin? Does insulin only Shepherd glucose to muscles and cells. So now this person right here, their confusion is where my I don't understand, comes in, because what they think is, well, that guy's not making insulin anymore, because that's what I was told about. Type one. Type one means don't make insulin, which we all agree about. But then, if this guy was type one, how is he not taking man made insulin, and if he's not, how come all this stuff isn't happening to him? So my question is, Jenny, I don't understand how this happened to that guest on that episode. Do you understand why he doesn't need insulin anymore,
Jennifer Smith, CDE 3:33
not at an in depth way, but I think one, his diagnosis was at age 50, correct. So he was diagnosed as an adult. So Lata, what we do know about diagnosis as adults, and it differs adult to adult, is that they have a tendency to actually have more beta cell reserve. And the expectation is that, and if I remember correctly, he still wears a CGM, even though he just uses the GLP one right now, right? So he did say that he can see excursions in his blood sugar, but his body fixes those excursions like his blood sugar might go up to 171 80. It does it on its own and brings it back down to the goal, target for the most part. Again, generalizing people without type one that have fully functioning beta cells, their blood sugar is not going to go up to 180 it is not it takes a lot of excessive, really simple carb to get it to nudge above target, yes, right? So he's having excursions. He doesn't technically have to take insulin, but I also expect that most of the time he's not eating, you know, six plates of sushi. He's probably eating a really well balanced diet. He exercises, if I remember correctly, from the episode and. So his beta cells that were in reserve, along with the impact of the monjaro, which is the only dual hormone, right? It's a GLP one and it's a GI P, yes, so it's the one on the market that has the heaviest impact on insulin sensitivity and weight loss and glucose management. So when we consider the kind of GLP one he's on, the fact that he was diagnosed as an adult, likely has a beta cell reserve, that would be my again, tip of the iceberg, understanding as to why he's not having to inject or pump insulin at this point. Yeah,
Scott Benner 5:41
okay. So that that is exactly my expectation, that, in truth, the poor guy might very well need his insulin again at some at some point. Yeah, right, but it is not so the so the story gets confusing, like it's confusing to this person, because, you know, I'm confused as to why this guy isn't starving because he's not taking insulin. He's on a GLP medication that suppresses appetite. Everything about it is confusing. It's exciting to see someone needing only one dose a week of GLP and that he's off insulin. I just want to understand how this works. So this guy is being very reasonable. I've seen people not be reasonable around this conversation, right? I
Jennifer Smith, CDE 6:21
have seen that as well. And I also think, in terms of the gentleman's question, the idea that type one totally and completely destroys every single little, teeny, tiny beta cell that you have in your body. It's not really the case, right? I mean, the only true measure of that would be a C peptide. And I don't know that he commented on his C peptides. I don't remember in the conversation if he did or not, but I would expect that with this down shift in delay in digestion, the body's ability to not have these major excursions in blood sugar, I would expect that again, those betas that are in reserve for him. He probably has still diagnostic of type one, but he probably has more C peptide visible than other people. Again, his time of type one has been very short, comparative to other people as well. So he it's not that he's not getting insulin. He is his betas that are there are still making it. And so to answer the guy's question about, How is he getting nutrients, his body is shuttling it in because his insulin receptors are working better. His cells are responding better to glucose and metabolizing the glucose better with this GLP one assisting with all of that, right? Right now
Scott Benner 7:44
we're going to hear from a member of the Medtronic champion community. This episode of The juicebox podcast is sponsored by Medtronic diabetes, and this is Mark.
David 7:53
I use injections for about six months, and then my endocrinologist in the Navy recommended a pump.
Scott Benner 7:59
How long had you been in the Navy eight years up to that point, I've interviewed a number of people who have been diagnosed during service, and most of the time they're discharged. What happened to you? I
David 8:09
was medically discharged, yeah, six months after my diagnosis, was it
Scott Benner 8:13
your goal to stay in the Navy for your whole life, your career? It was, yeah,
David 8:16
yeah. In fact, I think a few months before my diagnosis, my wife and I had that discussion about, you know, staying in for the long term. And you know, we'd made the decision despite all the hardships and time away from home. That was what we
Scott Benner 8:30
loved the most, was the Navy like a lifetime goal of yours. Lifetime goal.
David 8:34
I mean, as my earliest childhood memories were flying, being a fighter pilot,
Scott Benner 8:39
how did your diagnosis impact your lifelong dream.
David 8:42
It was devastating. Everything I had done in life, everything I'd worked up to, up to that point, was just taken away in an instant. I was not prepared for that at all. What does your support system look like? Friends, your family caregivers, you know, for me, the Medtronic champions community, you know, all those resources that are out there and help guide the way, but then help keep abreast on you know, the new things that are coming down the pipe, and to give you hope for eventually, that we can find a cure.
Scott Benner 9:07
You've probably heard me talk about us Med and how simple it is to reorder with us med using their email system. But did you know that if you don't see the email and you're set up for this, you have to set it up. They don't just randomly call you, but I'm set up to be called if I don't respond to the email, because I don't trust myself 100% so one time I didn't respond to the email, and the phone rings the house. It's like, ring. You know how it works? And I picked it up. I was like, hello, and it was just the recording was like, US med doesn't actually sound like that, but you know what I'm saying? It said, Hey, you're I don't remember exactly what it says, but it's basically like, Hey, your order's ready. Order's ready. You want us to send it? Push this button if you want us to send it, or if you'd like to wait. I think it lets you put it off, like, a couple of weeks, or push this button for that. That's pretty much it. I push the button to send it, and a few days later, box right at my door. That's it. Us, med.com/juice, box. Or call 888-721-1514, get your free benefits checked now and get started with us. Med, Dexcom, OmniPod, tandem freestyle, they've got all your favorites, even that new islet pump. Check them out now at us. Med.com/juice, box. Or by calling 888-721-1514, there are links in the show notes of your podcast player and links at juicebox podcast.com to us, med and all the sponsors. Right? So my, my kind of layman's expectation is he's lotta. So latas typically develops in individuals over 30, often between the ages of 30 and 50 symptoms, initial symptoms of lot of may resemble those of type two diabetes, and include, you know, everything, etc, but diagnosis, lot of can be challenging to diagnose and listen. We've had people on the podcast talking about this forever. There's always people diagnosed type two and there are lot of lot of meaning a very slow onset of type one diabetes. Wasted diagnosis. Auto antibodies, presence of auto antibodies, such as the GAD go, God ready, glutamic acid, Jesus, can you say that mic acid? What's the decarbolus thing?
Unknown Speaker 11:15
That's pretty good
Scott Benner 11:18
antibodies. These are typically found in type ones and indicate an auto immune response. That's really what I think most people stick to. If you have auto antibodies. This is auto immune. Your type one like it gets into the
Jennifer Smith, CDE 11:32
and then there are several more. I think there are four or five that are typically they this is a insulin antibody or auto antibody. There's a zinc transport there. There are a couple of them that have specifics to type one, not only the GAD, yeah. So again, regardless, he clearly was diagnosed with type one. At least one of these was positive, right, right? And
Scott Benner 11:56
your C peptide level is an indicator of your insulin production. Is that? Right? Right,
Jennifer Smith, CDE 12:01
correct. So when insulin is made in the beta cells, sort of the there's a piece of protein that's attached to, kind of move it out, and it's shaped, kind of like a C shape, is my understanding. So when it gets cleaved off and it enters circulation, that C shape remains there as an indicator of your own pancreatic insulin production, which is why, when you start injecting insulin, you can still get a C peptide level tested, because the insulin that you take via injection or pump doesn't ever put that C peptide into your body,
Scott Benner 12:33
right? And that can lower and decline over time. And that's our expectation when somebody comes with Yes, with Lada, because that's exactly what you know. What I'm looking at here is over time, individuals with LADA will typically require insulin therapy as their beta cells are gradually now, this says destroyed and and their ability to produce insulin decreases. I do. I believe in the destroyed word there, because there are definitely people you could, you know, they could drink GLP in their ears, and they're not. They're still going to need all their insulin, right, correct, like, so. So for the guy in episode, in the episode that we're talking about, I guess I should have it here, 1230 he was diagnosed at 50. He was using all the insulin by six years in like, he was really he was using a lot of insulin, which indicated to him and to his physician, I have type one diabetes, like I just do, they end up putting him on Manjaro for weight, and he suddenly doesn't need insulin. But he's also, to Jenny's point earlier, having excursions at meals that are higher than a person without diabetes would have, right
Jennifer Smith, CDE 13:40
and higher than somebody who was taking insulin to cover or clear some of that carbohydrate or food, right? That his betas are clearly not doing everything, but enough to clear it so that he's not sitting high for eight hours, right? I'm assuming that his excursions, along with his endocrine they look okay, if
Scott Benner 14:04
I remember, possibly it's only over an hour, an hour and a half, he pops 180 and comes right back, doesn't get low. And that's that. So what he's saying is, is that for however long this is going to work for me, this is magical, you know, and everyone would type one, and who's listening to this, I would assume would trade one shot a week for that situation over, over what they're in right now. Agreed, the confusion becomes, and you can tell by this gentleman's question is that, what is it? It's the um, it's older type ones, really, who think of it this way, right? Like, because, what is it? Do you think it's that argument between type one and you're old enough to know this. You're not old Jenny, but you're old enough to know this, like, okay, old head type, type ones, they don't want to be thought of as type twos,
Jennifer Smith, CDE 14:51
right? I guess in in general, yeah,
Scott Benner 14:53
because back in the day, if you have type two diabetes, you don't control yourself. You're overweight. That's your fault, right? That was the narrative. And type one defense of that was, I can't help this. This is auto immune. This just happened to me, and Don't lump me in with people who aren't taking good care of themselves, right? When that gets into the zeitgeist, and that's how people think my concern has been, and I'm using this episode to clear it up. I hope is that now that we're in the future and we're learning new things, we don't want to jump on this poor guy and say, because I saw him take it after the episode, you know, you're not a type one prove to me that you had auto antibodies. Blah, blah, blah. I'm like, just listen to the guy's story and like, I don't understand how nobody listens to type to episode 1230 and thinks, wow, there's a lot to learn about this. GLP, well,
Jennifer Smith, CDE 15:43
and I think to go right along with it, while it wasn't a complete loss of insulin use, I know that you've It was either an episode or you've talked to somebody who has a teenager whose insulin needs have come down like 90% of what this person was using now, being on a GLP one, so again, not completely off of insulin. But you can see, even in this person with, I don't know if she has longer diabetes than this gentleman or whatever, but diagnosed as a as a child, she probably had more B to cell initial destruction, and so has enough left to assist, along with what the GLP one is contributing, but still needs some insulin. And if
Scott Benner 16:31
she gets years like that, then good for her, then good for her, yeah, not just good for her, like her happiness, but her health and her longevity. It's going to help a lot of different things. So let's go into this gentleman's question a little deeper. The guy we're talking about needs insulin. He's taking a basal insulin and a meal time insulin. He's got type one diabetes. Obviously, it's going to be a very slow onset, like, probably what he was taking six years in, wouldn't have managed him well, 10 years from now, even you know, as possibly as his possibly as his beta cells continue to degrade,
Jennifer Smith, CDE 17:04
especially considering he was already having a weight management issue, and that was the reason you said the mole jar was started given to
Scott Benner 17:13
him to begin with, right? So, so, so then my question is, what changed? What did the GLP do? Like, I know it increases insulin sensitivity, but, but how? Like, what does that mean? Do we even know that part, or do we just know it happens
Jennifer Smith, CDE 17:27
the insulin sensitivity part? Yeah. Like, how
Scott Benner 17:30
does the GLP, like, magically? Because it feels magic, like you need insulin and now you don't, or you need even when you need less. Like, forget this guy for a second, right? My daughter takes a GLP medication. She's using significantly less insulin than she was without it. Okay, right? Why? What
Jennifer Smith, CDE 17:47
happened? Well, I mean, the GLP ones work several ways. One is for those who do still have some beta cells, or essentially, you know, type twos who have beta cells, but it's really the use of insulin and whatnot. That's the problem. These GLP ones do help with release of insulin. So for him, if his insulin resistance was cleared up because his weight came down and he had enough beta cell response then that his body wasn't having to overcome the resistance, then that could be a piece of it, in terms of the GLP ones helping to trigger the insulin release actually, and maybe more in the correct way, and usability improves. Obviously, GLP ones obviously also block glucagon release from the liver, and so, you know our response, it's a big reason that we actually have the idea of pre bolusing and understanding insulin use around meal times, because we do have this release of like stored gluco so to speak, and output of the liver. And if we block that, we are going to have lower post meal blood sugars, which is, again, probably a piece of why. Maybe his blood sugar goes up, but he responds very well. And now that he's had enough insulin release and his body is sensitized to the insulin, we have to remember that these meds also slow gastric emptying or delayed digestion, so the slower the things kind of sneak into with somebody who may have better insulin sensitivity. Now it allows the insulin that their betas are producing to actually gain traction right to work. And then, of course, you know whether this is helping him or not, and I can't remember whether he spoke much about it, but obviously the satiety factor with all of the GLP ones, most people, that's a big thing they talk about is, gosh, I feel like my head is clear from not considering food all day long anymore, like I can eat when I want to eat, or I choose to eat, but I'm no longer. I. I no longer so hungry, so to speak. Yeah,
Scott Benner 20:04
the episode that went up today I told you about before we started recording, so it's not on here. It's called, I'm getting the name for it. But this one is with a mom of a young type one daughter, and it's called Ken, GLP, meds, impact mental health. Oh, episode 1254 because this little girl is bipolar, and a mixture of lithium and GLP medications took away so many of her issues, it's like it's almost insane. But during one of the during a part of the conversation, the mom said that you could not keep packaged food around the house, because she would just attack it and just eat it. And she's like, what the GLP med has done just specifically to that kid's desire for sugar is amazing. But I want to say this sincerely. It's going to sound like I'm joking. If I had a private plane when we got done recording it, I'd get on it. I'd fly to where you are. I drive to your house, I'd give you a big hug. I'd tell you you are a national treasure. Have lunch with you. Let you give me some of that weird food you eat. And then I would drive home and let me tell you why. Let me tell everyone why. While Jenny was just saying what she said, and she is looking at me in the camera, she is not reading. She right, you know. Okay,
Jennifer Smith, CDE 21:19
I have nothing because I know that podcasts get recorded. Well, when nothing else is open on the computer screen, I have learned so. Scott, thank you. Jen. Jay is
Scott Benner 21:29
like, it doesn't open anything because I don't want anything to crash. Well, while, while Jenny was doing that dummy over here, went to chat GPT, and I said this, how do GLP meds remove the need for man made insulin be technical, but at a fifth grade level, that was so that I could understand it. And it said, and I am not kidding everything, you just no more or no less. You just pulled that right out of your ass, okay? And it was exactly Jenny is as smart as chat GPT when it comes to diabetes. That's all I wanted to say, boosting insulin production, lowering other hormones like glucagon, slowing down digestion, helping you feel full. And the wrap up was, GLP, one meds help your body make more of its own insulin, lower extra sugar, slow down sugar spikes and reduce how much you can eat. Your blood sugar stays more stable because your own insulin and these other effects are working better. You might not need as much man made insulin to keep your blood sugar in check. God, damn, you're a fcking brilliant person. I love to
Jennifer Smith, CDE 22:30
know the medication, because it's I mean, thank you very much for
Scott Benner 22:34
Oh, seriously, Jenny, I could have lined up 1000 people and asked that question. I would have got no
Jennifer Smith, CDE 22:43
well, thanks. Seriously, it's such the new I mean, honestly, this
Scott Benner 22:48
episode of The juicebox podcast is sponsored by the only CGM you can take off to get into the shower the ever since CGM, ever since cgm.com/juice, box. Well, I mean, sure you could take the other ones off, but then you'd waste the sensor and have to start over again. But not with Eversense. Eversense is a six month wear implantable CGM. So if you want to take a shower without anything hanging on, you pop off the transmitter, jump in the shower. When you get back out, put it back on, and you're right back to where you started, come to think of it, you could do that whenever you wanted to. Maybe it was your prom night or your wedding day. Maybe you just don't want the thing on for a little while, but you don't want to go all through the hassle of taking it off and having to restart it and, you know, starting back over with, like, wonky numbers, and having, you know, all that that goes with it when you take off a CGM and put it back on. Oh, but you don't have to do that with the Eversense CGM, because Eversense is the only long term CGM with six months of real time glucose readings. This gives you more confidence, more convenience and flexibility. The Eversense CGM is there for you when you want discretion, a break, or maybe just a little adult time ever since cgm.com/juicebox, pop that transmitter off, pop it back on, you're right back where you started, without any wasted devices or time.
Jennifer Smith, CDE 24:13
I've also, you know, GOP ones have been on the market for a long time, despite them really gaining ground because of the new formulations that really do have a lot more power than the older versions had, but the older versions still worked. I mean, they were, they were what we had initially, that we, you know, the victos and the by durians and those types of things. They they did a good job, just not what our current day does.
Scott Benner 24:42
I was having this thought this morning because it became so popular for weight loss, we ended up and listen, there was a lot of bitching in the media and everywhere else about it. But in the end, it ended up being a good thing, because instead of target, using it for one thing and finding a lot of very similar. Are people. There are people with all different kinds of health implications across the world who needed to lose weight. So we basically spread it out over everybody. And that's why you're getting back these like, Hey, um, I'm getting pregnant on this. Or my again, more I'm hearing about people saying their airs danlers syndrome is, like, I know I never say that correctly, but like, like, they're having lessening facts. Now, I got a girl here that says that, you know, a significant amount of her bipolar issues are cleared up. I mean, come on, right and then, and the guy from the episode we're talking about, he's gonna listen, if you want my opinion about what happened to the gentleman episode 1230 which you should really listen to, is that he is going to get a much longer honeymoon than he was going to and need less insulin during it than he was doing fantastic right
Jennifer Smith, CDE 25:51
on so many fronts, you know, glucose, glucose management ties into so much in terms of long term health. It does a cardiovascular health, brain health, I mean, all the things that are now being studied and understand, understood about true glucose management, whether you have diabetes or not, it's tied into a lot of body function. So you know, if we can sensitize our bodies in multiple ways, this doesn't necessarily mean you throw out all of the good lifestyle habits that you've been trying to put into action keeping them. In fact, exercise, by far, is the top the tip of the pyramid of anything good that you can do for your body, for like an ongoing health into your later years, even as little as walking every single day, right? But if we keep those things in the picture, along with something that could help when those lifestyle things aren't doing enough for us, then great. Yeah.
Scott Benner 27:00
I mean, listen, you say lower your inflammation prior to GLP, if you tell somebody, you would tell them to eat low inflammatory foods and blah, blah, you can't eat enough of that goddamn food to help you if you have a real problem. I mean, come on, you know, use fermented. Okay, great. Like sauerkraut and myself. You think if I ate sauerkraut, I'd have lost 50 pounds? No, okay, you know, I don't have diabetes. I have no my doctor told me all the time, like I actually was told by my endocrinologist, I don't foresee you ever getting Type Two Diabetes, like at your age, where you're fasting glucose is and everything I see from you, you just don't present as somebody who's gonna end up with type two and I'm like, Oh, great. I'm still significantly overweight, unhealthy, etc, and so on. But I wasn't doing any of the things that classically people would say, oh, it's because he's doing this. Like, I really don't live a much different life right now than I did before. While we're looking for, like, spreading out over people who needed to lose weight and learning things. I was getting iron infusions yearly, maybe twice a year. Some years or I would fall apart and die. My ferritin level was going down into the single digits, right? That doesn't happen anymore. My body is absorbing iron now, and I'm fine. I haven't needed an infusion in a year and a half, and
Jennifer Smith, CDE 28:19
I wonder there, you know, just in in that small, little, narrow, I wonder if it has to do something with the way that these meds slow digestion. I wonder if it's your body now has enough time to completely absorb what it needs to and so you don't have to medically manage your irons, yours,
Scott Benner 28:39
yeah, and keep in mind that, prior to that, my fartin drops, and the doctor, so first of all, they think you have cancer right away, because if you're of a young enough age, and it looks like you're losing, you know, iron, they just so I gotta go through all that. I scope one way I get scope, the other way, well, Oh, you don't have cancer. Good, good. Congratulations, thanks. I'm still having all these problems, right? Maybe have celiac don't eat gluten for a month. A month later, nothing changes. I'm like, Look that that wasn't it. You know what they said after that, take an iron supplement with vitamin C. It helps it uptake it faster. So I did that. You know what? That did? Not a lot, nothing. Yeah, right. And so I was going to be one of those people that they were like, Hmm, don't understand. Bye, bye. Like, you know, like, that was it? Like, we did all the things that we understand. We go off and think I took the GLP because I went to when my kids, my second kid, went off to college. I went to my kids endocrinologist, and I said, Hey, yo, I did it. I raised those kids. They're good people. They're not going to murder anybody. Now, I
Jennifer Smith, CDE 29:42
have time for me. I
Scott Benner 29:42
need to stay alive, right, right, right, like and, and she looks at me. She knows me. She'd been helping me with things, right? And she didn't know what was happening still. And I said, I need to lose weight. And she looked at me and said, why? And we were standing face to face. See, and I said, and she goes, I said, you don't see. And she goes, No. She goes, Scott. She's like, you could lose weight, but you don't look like that's your problem. And I said, Well, that's very nice. And I stood up. I don't know if I've told this in the podcast, I stood up, I took off my sweatshirt, and I said, I'm gonna get on a scale in a minute. You guessed my weight? And she guessed my weight at about 175 pounds, which, by the way, is well under, yes, is eight pounds less than I weigh right now, and I've already lost 48 pounds like so when I told her my weight, she goes, Oh God, we'll get you a GLP medication. And the stuff that came after it, she didn't say, I'll get you the GLP medication. And, by the way, you won't need iron infusions anymore because this, she didn't know that was going to happen. No, yeah, right.
Jennifer Smith, CDE 30:42
I think that's, I mean, you bring up a good point there. I think that again, despite GLP ones having been around for a while, this new generation of them being so much more impactful, there are so many things being discovered and found that are, let's call them positives, yeah, or other health related things. Now, I do think that longer term, we need a lot of evaluation and study and everything, because you know, you're putting something in your body that technically, while, while it is a hormone that your body would normally make for whatever reason, environmental, food system, whatever's happening in our today's life, body, there's something that's not working the right way. Otherwise people wouldn't be responding. I think people like you, as an example, would it really be responding if your body was actually doing what it should be doing? That's my
Scott Benner 31:46
only point. Is that for me and for many other people, your body's not doing something, and this medication is is covering for it, somehow covering what do we care? Like, like, I Why do you like? Just listen, I know this isn't like. I'd spread it on everybody. I'd sprinkle it over top of us and be like, let's see what else it fixes. We're gonna figure that out. Like, it's the baseline stuff. Like, Oh, I lost weight so my knees don't hurt anymore, and I'm not gonna have to have a hip surgery or something. Like, that's nice and all. And don't get me wrong, it's amazing. But listen, this is new. Recent studies have highlighted the potential of GLP one agonists such as ozempic and reducing the risk of dementia, particularly Alzheimer's disease and people with type two diabetes. A large study involving 88,000 participants showed that those treated with GLP one agonists had a significantly lower risk of developing dementia compared to those using other diabetes medications like sulfonylureas and DPP four inhibitors, the reduction in risk was 30% compared to sulfonylureas at 23% compared to DPP four inhibitors. Come on. Like,
Unknown Speaker 32:53
yay. Like,
Scott Benner 32:55
you know what I mean? Like, you mean I don't have to be overweight, and when I'm 85 I'm not gonna be like, banging my head on a wall, like, you know what I mean? Like, this is wonderful. Jenny, for 20 years, I heard people say inflammation is the problem, but they didn't know what to do with it. After that, it feels like we know what to do. Now a little better, a little better. Yeah.
Jennifer Smith, CDE 33:18
I mean, they're only, I think the biggest thing that I'd like to see with these medications is the right kind of education in use of them. You know, in terms of prescribing, as a prescriber, you're a caregiver, and you should really be checking in with your patients. You should really be checking in and saying, How are things going? You know, you start them on this a weekend, there should be a follow up, even a quick message, right? They How are things going? Let's see, how are you feeling, etc, because some people may respond better to one than another, yeah, you know. And if there's not enough information given up front about how you might feel, is this normal? When should I call if it's not feeling back to normal or whatever? I think on the case of clinicians, they really need to do a lot of self educating about these to know what's appropriate and how to help people use them to their advantage. Yeah, they
Scott Benner 34:19
also have to understand what they're what they're actually doing for people. Because right one of the bigger problems with the glps right now, as it's being reported, is that the dropout rate is like around two years. So you know, my opinion of that is that this medication may be doing a lot more for you than you understand, and just because you didn't continue to lose weight or didn't get to your goal weight might it might
Jennifer Smith, CDE 34:41
not be, might not be. The only thing that it was helping Exactly, right? And doctors
Scott Benner 34:47
need to understand, like, Listen, if you are one of the people who takes it and you're nauseous and vomiting constantly, it's not for you, obviously, like, but I'm not talking about just force yourself through it. But right? I made it through some side effects, like. There was, there was a a fair amount of time in there where I was like, I'm never gonna have a solid bowel movement ever again in my entire life. And like, but I was losing weight to the point where I was like, You know what I actually thought? And this is nothing technical, obviously, this was my thought. I'll let you go. Yeah, it took me this many years to get this fat. I wonder what horrible things were happening inside of me then that I never, like, I never batted an eye against I didn't, I didn't go out and, you know, eat greasy food, because I used to eat greasy food, I don't anymore. I didn't go out eat greasy food, come home, have distress in the bathroom, and then go, Well, I'm never gonna eat greasy food again. Like, like, I'm like, I struggled through that to get to my next french fry. I better, like, I'll try this, you know what I mean, right? And I stuck with it. Now I don't have that problem anymore. But I mean, if you're really impacted by it in a way that you just can't function, I understand it's not for you that's fine, but for everyone else, like, we gotta keep paying attention to this, I think. Yeah, so, to answer the gentleman's initial question, I don't understand why this guy doesn't need insulin. He does need insulin, and his body is making it right now. Yes,
Jennifer Smith, CDE 36:03
that's it. That's the bottom line, without all the biochemistry and physiology and all the stuff, yes, that's the bottom line. I mean, we
Scott Benner 36:13
made a good podcast episode here. I'm
Speaker 1 36:14
gonna let you go. Thank you. Of course, you I
Scott Benner 36:23
want to thank the ever since CGM for sponsoring this episode of The juicebox podcast, and invite you to go to ever sense cgm.com/juicebox to learn more about this terrific device, you can head over now and just absorb everything that the website has to offer, and that way you'll know if ever since feels right for you, ever since cgm.com/juice box, Arden has been getting her diabetes supplies from us med for three years, you can As well us med.com/juice box, or call 888-721-1514, my thanks to us, med for sponsoring this episode and for being long time sponsors of the juicebox podcast. There are links in the show notes and links at juicebox podcast. Com to us, med and all of the sponsors. Mark is an incredible example of what so many experience living with diabetes. You show up for yourself and others every day, never letting diabetes define you, and that is what the Medtronic champion community is all about. Each of us is strong, and together, we're even stronger. To hear more stories from the Medtronic champion community or to share your own story, visit Medtronic diabetes.com/juicebox Once, there was a time when I just told people, if you want a low and stable a 1c just listen to the juicebox podcast. But as the years went on and the podcast episodes grew, it became more and more difficult for people to listen to everyone. So I made the diabetes Pro Tip series. This series is with me and Jenny Smith. Jenny is a Certified Diabetes Care and Education Specialist. She's also a registered and licensed dietitian and a type one herself for over 30 years. And I, of course, am the father of a child who was diagnosed at age two in 2006 head now to juicebox podcast com, go up in the menu at the top and click on diabetes pro tip. Or if you're in the private Facebook group, there's a list of these episodes right in the featured tab. Find out how I help keep my daughters A, 1c, between five, two and six, two for the last 10 years without diet restrictions. Juicebox podcast.com start listening today. It's absolutely free. Okay. Well, here we are at the end of the episode. You're still with me. Thank you. I really do appreciate that. What else could you do for me? Uh, why don't you tell a friend about the show or leave a five star review? Maybe you could make sure you're following or subscribed in your podcast app, go to YouTube and follow me or Instagram. Tik, Tok. Oh gosh, here's one. Make sure you're following the podcast in the private Facebook group as well as the public Facebook page you don't want to miss. Please do not know about the private group. You have to join the private group. As of this recording, it has 51,000 members in it. They're active, talking about diabetes, whatever you need to know. There's a conversation happening in there right now, and I'm there all the time. Tag me. I'll say, hi, hey. What's up everybody? If you've noticed that the podcast sounds better, and you're thinking like, how does that happen? What you're hearing is Rob at wrong way recording, doing his magic to these files. So if you want him to do his magic to you, wrong way. Recording.com, you got a podcast? You want somebody to edit it? You want rob you?
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1290 Hello, It's Me
Adelle has type 1 diabetes.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome back to the juicebox podcast.
On today's show, I'll be speaking with Adele. She is 12 years old and has had type one diabetes for a little under two years. At the time of this recording, Adele has some Hashimotos and eczema in her family, and we're going to talk about that as well as how type one diabetes impacts her life. Please don't forget that nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan or becoming bold with insulin. Don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40% at cozy earth.com when you place your first order for AG, one with my link, you'll get five free travel packs and a free year supply of vitamin D drink, ag one.com/juice box. If you'd like to save 40% off of your first purchase@hungryroot.com use this link. Hungryroot.com/juice box. That's all you have to do. Hungryroot.com get your food there, let them make it for you. What do you bother them with cooking for what are you a chef, yes. Chef, does anybody watch the bear on Hulu? Thank you? Chef, no. Chef, thank you. Chef, this show is sponsored today by the glucagon that my daughter carries. Jeevo hypo pen. Find out more at gvoke, glucagon.com, forward slash juice box. This episode of the juice box podcast is sponsored by us. Med, us. Med.com/juice, box, or call 888-721-1514, get your supplies the same way we do from us. Med, this episode of the juice box podcast is sponsored by the Eversense CGM, an implantable six month sensor. Is what you get with Eversense, but you get so much more exceptional and consistent accuracy over six months and distinct on body vibe alerts when you're high or low on body vibe alerts. You don't even know what that means. Do you ever sense cgm.com/juice? Cgm.com/juicebox, go find out. Hi, I'm Adele. Adele. How old are you? 1212? You have type one, yes. For how long
Adele 2:34
I've had it since May 20, 2022, so that would have been one year and nine months.
Scott Benner 2:41
Wow. A year and nine months. Were you 10 when you got it? Or had you? Yes, yes. What? Wait, yeah, yeah, okay,
Adele 2:50
oh, yeah. 10 years old, it says
Scott Benner 2:53
you have notes. Yeah,
Adele 2:55
you think of some important information. That's
Scott Benner 2:58
okay. That's good. You, uh, brothers and sisters, yes,
Adele 3:01
I have a sister. Um, she's 10 right now.
Scott Benner 3:04
Does she have any autoimmune stuff? Um, no. Do you have any other autoimmune stuff besides type one?
Adele 3:10
I don't think so. But I know my grandpa and my uncle on my mom's side have eczema, and then my grandma on my dad's side has this thing that I can't present, um, like a pronounce spell it, H, A, S, H, Hashimotos.
Scott Benner 3:27
Yeah, that's, that's an autoimmune issue. That's a thyroid, okay? And who was that? Oh, yeah,
Adele 3:32
my grandma on my dad's side,
Scott Benner 3:34
grandma. Oh, wait a minute, your grandma on your dad's side has Hashimotos, and someone on your mom's side has eczema.
Adele 3:39
Yeah, my grandpa and my uncle. Interesting,
Scott Benner 3:42
interesting not to you, interesting to me, to you. You're just like, I don't want diabetes tell me about so you're old enough to kind of remember this. So did you start feeling sick? Did someone say something to you? How did you get diagnosed?
Adele 3:55
Well, like, I, I went to, like, the bathroom, like, in the middle of the night, like a lot. And my mom, like, was, like, noticing that kind of as, like, one of the symptoms. And she also noticed some other things. I didn't really notice a bunch.
Scott Benner 4:07
So what else did she notice that? You didn't notice that
Adele 4:10
I was, like, eating a lot, very hungry. Yeah. And I losing weight,
Scott Benner 4:17
lost weight, peeing in the middle of the night, a bunch. How long do you think this all went on for before she was like, Hey, we should go talk to a doctor.
Speaker 1 4:25
I'm not really sure you don't remember, like, for maybe, like, a few weeks. Okay,
Scott Benner 4:31
okay, did your teachers notice anything? My
Adele 4:34
I feel I'm not sure if I was diagnosed yet, but my t my fifth grade teacher, she kind of noticed that I was like, kind of like, I think moody ish, but I don't remember if I was that like, if I've diagnosed that time, or if it was before my diagnosis. So
Scott Benner 4:48
if people thought I had diabetes every time I was moody, that would be something, moody ish. I don't know what that means, but it's funny. What makes you want to come on the podcast. So
Adele 4:58
I'm like, very. Way out, like, with my diabetes, I'm not like, kind of like, shy, so I kind of thought like, hey, this seems fun. I want to try it. Okay, so you just
Scott Benner 5:09
want to give it a shot. You want to talk to other people about type one and be open about your diabetes. Yeah, okay, oh, let's do that then. So your mom sees all these issues. Do you go to a doctor, hospital. Where do you head? So we
Adele 5:22
did go to the doctor, but then after that, I went to the hospital, like, I immediately went home, grabbed my stuff, and went to the hospital, like, emergency, and then I stayed for one night. That
Scott Benner 5:34
was it. Yes, do you remember what your blood sugar was do? What do you remember about? Yeah,
Adele 5:38
I have that written down when I went to the hospital, my blood sugar was 407, okay.
Scott Benner 5:44
Do you remember a lot about that time in the hospital? I know it's only a day, but were you scared? Was it confusing?
Adele 5:52
I remember not getting to eat for like a while. Eventually, they offered me ice chips, and I thought it was gonna be like something that was just ice cubes. And I was kind of disappointed. You thought you were getting
Scott Benner 6:02
something fancy and you got ice in a cup. Yeah, they didn't do the thing. They let you drink with a straw, though, right? Eventually, have you ever had the the sponge, the wet sponge, at the hospital when they won't? Oh, my God, all right. Well, here, listen, I hope this never happens to you, but if you're in the hospital and they want to restrict your fluids, they won't let you drink. They'll put a cup and a sponge on a stick, and you're allowed to wet the sponge and rub it inside of your teeth and your gums to wet your mouth, huh? Not good. Okay. You don't want that. It's not even a fun sponge. It's like, I don't know what a fun sponge would be, but it feels it's not comfortable, and the sticks plastic. It's all very strange. So what you remember about the hospital is more about not being able to eat and stuff like that. You weren't like, Oh, my God, I have diabetes or, well, like,
Adele 6:47
at first when I was in the doctor's office, I was like, Wait, why are you guys talking about this? And then, like, I just started crying. I was very like, sad at the moment,
Scott Benner 6:56
sad because you knew something was wrong, or sad because you were scared. Do you remember,
Adele 7:02
I think it was like, more or less like me being like, kind of like, kind of a bit of both,
Scott Benner 7:07
okay, yeah, just overwhelming,
Unknown Speaker 7:10
yeah. Did
Scott Benner 7:12
your mom cry when you cried? No,
Adele 7:14
she was, like, talking to the doctor. I was kind of just sitting like next to her, like, why are you guys talking about diabetes like I was just hearing a bunch of words being like, thrown around
Scott Benner 7:24
Adele. I know you guys grew up being on camera, so you're very accustomed to it, but I find when I'm looking at you, I wonder what I look like. Do you ever have that feeling you're like, I'm looking at him, he can see me. But what do I look like right now? Do you ever think that? Because then when you look at you, that's not what you look like anymore. Does that make sense? Kind of right? Because if you like, watch, I'm looking at you, but now, if I look at me, you're not seeing me the same way as when I'm looking at you. But I'll never know what. I guess I could take a screenshot. In my mind, I look very different when my head's turned a half an inch one way or the other. I'm sure that's not even true. Did you go to school on camera during covid?
Adele 8:00
Yes, we, I know we did, like, two days at school, and then the other days, like the other group of kids would go in and we would, like,
Speaker 1 8:08
I think we were on Zoom, I don't remember. Yeah, was this before or after your diabetes?
Adele 8:15
Way before that was like, that was like, covid. So, like, two years before, I think, like, 2020, so, yeah,
Scott Benner 8:21
do you remember? Were you sick at all before you were diagnosed? How many viruses? Or,
Adele 8:27
yeah, I didn't have covid. I
Unknown Speaker 8:29
believe you think you had covid. I'm
Adele 8:31
pretty sure I had covid. Like, when, like, part of that stuff was, like, going on,
Scott Benner 8:35
how was it for you? Did you Was it hard on you? Or was it pretty gentle covid, yeah, it was like, more like a cold, or were you like, wow, I'm really sick. I think it
Adele 8:45
was kind of more like a cold. It wasn't super bad. Okay, okay, so
Scott Benner 8:49
you get diagnosed, and it's scary, and you go to the hospital, you're not there too long. You come home, and is it up to you? Do your parents say? Like, are your parents married? Yes, yeah. So are your parents? Like, well, you, you're a big girl. Adele, like, let's get going. Or were they, like, we'll help you. Like, how much, what was the division of work
Adele 9:08
they like, helped me a lot.
Scott Benner 9:09
Do they still, yeah, okay. Do you want them to? Need them to like them to I do kind
Adele 9:17
of like the help. Like, I could do like those stuff on my own, but it's nice to like have some help, yeah.
Scott Benner 9:23
So what do you use? What kind of gear Do you have? So I
Adele 9:29
have the Dexcom g6 and the OmniPod five.
Scott Benner 9:32
OmniPod five, Dexcom g6 you can change your sensor by yourself on your Dexcom. Yes or no, yes, yes.
Adele 9:41
I've had to do my OmniPod a lot of times, because sometimes it was, like, before dance and stuff. So I had to, like, change it real quick, because my mom wasn't
Scott Benner 9:50
home, right? You know how to change your pod. No problem with that. Yeah, counting carbs. Where are you with that? Yeah, I'm pretty good at it. Okay, like, when you're gonna have a meal, do you like slide the control? Or towards your mom and be like, Here, take care of this. Or do you just do it? Sometimes, nice?
Adele 10:04
Yeah? Because sometimes, like, it's kind of annoying to, like, find the carbs, because, like, and I have to wait and stuff and, like, the worst part, honestly, is, like, waiting the 15 minutes, though, yeah, because I
Scott Benner 10:15
know it's next. How do you eat? Do you have, like, a certain style of, like, eating something you like more than other you're a vegetarian, eat a lot of meat? No, I don't think so. Just kind of eat what mom gives you got you, yeah, what's an average, uh, meal at dinner time? Like, what do you have a lot in the house?
Adele 10:33
You like, my mom, like, makes all these like different things. So there's not really, like an average thing, okay, so she's
Scott Benner 10:39
she makes a lot of different variable things. So you give vegetables good cook too nice. That's good. Sometimes people grow up thinking their parents are good cooks. Then they meet somebody who actually is good at cooking, and they go, Oh my god, I thought like this was here. I'll tell you a secret. My wife thought salt and pepper were spices like that was, like, the how exciting food was in her house, you know what I mean? And it wasn't one year at Thanksgiving, their Turkey was so, like, it was so disgusting. And I was like, Oh, it's great, thanks. I picked around it. Then the next year, I said, Can I bring my own Turkey to Thanksgiving? She was like, No, that'll be insulting. I was like, oh, okay, it's terrible. She didn't know the difference until she got moved out. I think it happens to a lot of people. How about your friends? So you weren't in the hospital very long for friends to come visit. But what's it like afterwards? Now, do you have, like, a close group of friends? How would you describe your friendships. This episode of The juicebox podcast is sponsored by the ever since CGM, ever since cgm.com/juicebox, the Eversense CGM is the only long term CGM with six months of real time glucose readings giving you more convenience, confidence and flexibility. And you didn't hear me wrong. I didn't say 14 days, I said six months. So if you're tired of changing your CGM sensor every week, you're tired of it falling off, or the adhesive not lasting as long as it should, or the sensor failing before the time is up. If you're tired of all that, you really owe it to yourself to try the Eversense CGM, ever since cgm.com/juicebox I'm here to tell you that if the hassle of changing your sensors multiple times a month is just more than you want to deal with, if you're tired of things falling off and not sticking, or sticking too much, or having to carry around a whole bunch of extra supplies in case something does fall off, then taking a few minutes to check out. Ever since cgm.com/juicebox might be the right thing for you. When you use my link, you're supporting the production of the podcast and helping to keep it free and plentiful. Ever since cgm.com/ dot com, slash juicebox. If you take insulin or so faucinyas, you are at risk for your blood sugar going too low. You need a safety net when it matters most, be ready with G vo hypo pen. My daughter carries G vo hypo pen everywhere she goes, because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that, I trust low blood sugar emergencies can happen unexpectedly and they demand quick action. Luckily, jivo hypo pen can be administered in two simple steps, even by yourself in certain situations. Show those around you where you store GEVO kypo pen and how to use it. They need to know how to use jivo kypo pen before an emergency situation happens. Learn more about why GEVO kypo Pen is in Arden's diabetes toolkit at gevok, glucagon.com/juicebox, gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma, or if you have a tumor in your pancreas called an insulin OMA, visit gvoke, glucagon, com slash, risk for safety information. Diabetes comes with a lot of things to remember, so it's nice when someone takes something off of your plate, us, med has done that for us. When it's time for Arden supplies to be refreshed, we get an email rolls up and in your inbox says, Hi, Arden. This is your friendly reorder email from us. Med. You open up the email, it's a big button that says, Click here to reorder, and you're done. Finally, somebody taking away a responsibility instead of adding one. US med has done that for us. An email arrives, we click on a link, and the next thing you know, your products are at the front door. That simple, US med.com/juice, box, or call 8887211, 514, I never have to wonder if Arden has enough supplies. I click on one link, I open up a box, I put this stuff in the drawer, and we're done. Us. Med carries everything from insulin pumps and diabetes testing supplies to the latest CGM like the libre three and the Dexcom g7 they accept Medicare nationwide, over 800 private insurers, and all you have to do to get started is call 888-721-1514, or go to my link, us, med.com/juicebox, using that number or my link helps to support the production of the juicebox podcast.
Adele 15:39
Yeah, like, a lot of people, like, are always asking, but they're very, like, helpful. Like, they always like, like, I know that I have the nasal like, the best, best squimmy,
Scott Benner 15:52
I don't know. Yeah,
Adele 15:53
they're like, very, like, open to helping me and stuff. And like, if my like, phone beeps, they're like, are you okay? Like, do you need sugar or something? So
Scott Benner 16:02
did you explain it to them, or do you think they're learning it as you go along? You did. Yeah, if you asked me to describe my daughter's friend group, it's these four girls. Like, I know who they are, right off top my head, right? It's always the same girls. Like, do you have that situation?
Adele 16:15
I actually, like, I have a, like, a variety of friends. Like, I'd say I have a pretty big friend group. Okay,
Scott Benner 16:21
so there's some people who are closer in your circle, and some people are a little more on the outside, and they know, they know. Okay, so you tell the close up ones the stuff they need to know
Adele 16:31
really, like, I'll tell, like, anyone, like, a lot of people in my school are, like, always asking me questions. And they're like, they're always asking about, like, why I have two phones,
Scott Benner 16:39
yeah, what do they think? You're like, a drug dealer or something? What do they think?
Adele 16:43
No, no, they're just like, confused. I try to explain my best.
Scott Benner 16:47
Okay, so some your friends have varying understandings of diabetes, but do they know enough? Like, if I looked over and Adele was like, Oh, I don't want to hold on. I just don't want to say this and upset you. You know what could happen if your blood sugar gets really low, right? Yeah, okay, all right. So if your friends looked over and you were on the ground flipping around like a fish, you think they would take out that back swimming and shove it up your nose and give it a tug? Yeah? No kidding, I think so. Yeah, cool. Oh, that's really neat. It's nice that friends like that. You know, do you go to the nurse's office for your adjustments at school? Or do you handle them on your own?
Adele 17:20
I handled them on my own. Last year I did on go to the nurse to, like, pre bolus, but I'm a big girl now. Yeah,
Scott Benner 17:26
you don't need that, right? Yeah, whatever. What would you like people to know like, Okay, I know you've talked to your friends, but do you have a feeling like, when you said you wanted to be open about diabetes? What did that mean to you? Being
Adele 17:39
like, open about, like, diabetes is like, to not be afraid to, like, kind of, like, explain it to people and like, not being, like, trying to hide it or anything,
Scott Benner 17:47
so that that really is, then more about how you feel about it and how you interact with it, like you don't care so much if, if I know about it, you want to make sure that you're comfortable being open about it and talking about it, yeah, okay, why do you not want to hide it? Because, like, I
Adele 18:06
feel like there's really no reason. Like, I feel like, if I hit it, like, it would be like, really weird. Because like, I'd be like, like, people would be like, Hey, why is there a bump in your shirt? And I'd be like, um, no reason, right? So it's like, just easier also to be out about it,
Scott Benner 18:19
yeah. Like, so instead of just changing the subject and walking away or something, you want to be able to say, yeah, it doesn't bother you when somebody says, hey, what's under your shirt there? Yeah, no, no.
Adele 18:32
Like, I'll be fine to be like, Oh, this is my like.
Unknown Speaker 18:35
So are
Scott Benner 18:36
you normally open, or are you, like, willfully trying to make sure that you're not hiding diabetes. Honestly, I'm normally open. Okay, so this goes along with your personality to begin with. All right, gotcha Do I seem very old to you? No, not really, not really excellent. That's good news. I saw somebody recently that said I looked very young, and I've been clinging to that all week, like I just bumped into somebody I hadn't seen in a while. They're like, Oh my God, you look so young. And I was like, thank you. So excited, very, very excited. Actually, you play any sports?
Adele 19:10
Yes, I did do swim team, but that ended like at the February I do dance class, and I'm doing a ballet and I do three clubs, Art Club, International Club, and Baking Club,
Speaker 2 19:22
ooh, I went to baking school, like, I worked in a bakery. I know how to do that. Like, I could make, like, you know, you can make a loaf of bread. I could make 200 loaves of bread, like, literally, all at the same time. I don't know if that's a skill or not.
Adele 19:38
The thing about Baking Club is, though my friends actually, like, started it with, like, our home ec teacher. So that was pretty cool. Like, they kind of started their
Scott Benner 19:46
own club. Yeah, you went to a teacher and said, hey, we'd like to have an after school club. Can you be the person that does it with us? And that teacher said, Yes,
Adele 19:54
yeah. They, um, I wasn't completely part of it, but I did, like, join it after but they, like, they went through like, a lot. But like, I think they started working on it last get it set up.
Scott Benner 20:04
See, you're kind of young, so I'm gonna say something cynical for a second. Does it worry you that teacher didn't have anything better to do after school that they were allowed to? They were able to hang out? No, no, you're so nice. Kind of fun. You're so nice. No, no, I think it's a nice idea. Only adults are laughing at what I just said now, like, like, can you stay after school for free and bake with us some more? I'd be like, I'm busy. But it was, it was very nice of her to her, him, him, him, him. It was very nice of him to do that. That's excellent. Is he younger?
Adele 20:34
He's like, kind of mediocre.
Scott Benner 20:36
Everybody look old to you when you're 12. Not really, I don't think I love this. This is great because sometimes I ask questions you don't know the answers to. It's fun to watch you kind of like, think about it for a second. Adults will just they've been asked the same question so many times that you ask them and they just blurt out the answer that their brain already knows. You're actually thinking about it, which I'm enjoying OmniPod five with dance class. How's that doing for you? Is it keeping your blood sugar pretty stable?
Adele 21:05
Yes, because, like, we use like, activity mode, um, most of the like the time. I believe I know my Anana turns it on. I don't know if my mom turns it on, though, interesting. Like, I'd never, like thought about it. You don't
Scott Benner 21:17
make an adjustment. You're not the one who worries about that adjustment. It's the adult that's with you that does it? Yeah, a
Adele 21:23
little bit more, because I'm not sure if I'm supposed to use it or not. Got it. Okay? Sometimes the OmniPod does, like, get in the way, like, for stretching and stuff. But like, usually it's in a good spot,
Speaker 1 21:34
because, like, sometimes, like, it would just feel weird. Okay, where do you prefer for it to be? Usually, like, on
Adele 21:39
my stomach or legs sometimes, like my arm, like I have my OmniPod on, like this arm right now, sometimes it's a bit weird.
Scott Benner 21:46
So stranger on your arms. For you, a little
Adele 21:49
bit like, I just put this, like a new OmniPod on my arm last night. So
Scott Benner 21:54
okay, how long did you do injections for?
Adele 21:58
Not very long. We got the OmniPod after seven weeks after diagnosis.
Scott Benner 22:04
Oh, okay, so you had, you didn't do injections long at all. Okay, no, did you dislike the injections? Why did you move to a pump so quickly? Because,
Adele 22:14
like, it was, like, available, and it's like, kind of like, like, I think, I think we thought of it as, like, an upgrade. Injections really weren't that bad, though, just like a little poke.
Scott Benner 22:24
Do you know what your a 1c is? Yes,
Adele 22:27
I have the A one history. Oh, yeah. Do you want to know the most? Do you want to know the most recent one? Because there's a lot?
Scott Benner 22:35
Well, tell me the most recent one, then tell me, like, go back like four or five and tell me what it was like a half a year ago or something
Adele 22:43
like that. Okay, so the most recent one is 220, 24 6.3 1128, 2020 2023 6.388 2023 6.85 2320 23 7.0 7.0 so like most of them, were like in the low um, like six points on things. But like that was like one seven and then the two 228 2023 6.2 11, 120, 22 6.37 2020 22 8.25 2020 2216 point zero. So that's actually all of them, yeah,
Scott Benner 23:25
so there was basically an elevated one at your diagnosis. And it looks like you maybe had a honeymoon for a little while, and now you've been figuring out how to use insulin, and you're in the mid sixes.
Adele 23:38
Oh, my, my, A, 1c, I found something that said, March 2024, now, 12 year old, 6/7, grade, A, 1c, 6.3 and then my total total daily insulin, 775, units.
Scott Benner 23:50
So you've been at 6.3 pretty steadily for like, the last nine months. Yeah, that's great. Do you remember having a honeymoon? Was there a time when you all of a sudden needed less insulin? Or is that not a thing that not a thing that you would have known about and your parents
Speaker 1 24:02
would have handled? I feel like my parents would have known that more. Okay, all right,
Scott Benner 24:07
what should adults know about how it feels to have diabetes?
Adele 24:15
Like, if, like, adults were to have diabetes, or just like, kind of what they should know to help me,
Scott Benner 24:19
yeah, as parents, I guess I'm asking you, like, what experiences are you having, or feelings are you having that you're pretty sure your parents don't know about. Sometimes,
Adele 24:30
like, when I'm dizzy or My head hurts, like when my blood sugar is, like, high or low, sometimes I don't, like, always tell them, like,
Scott Benner 24:37
yeah, so you'll keep it to yourself if you're dizzy, sometimes, sometimes,
Adele 24:41
like, if they ask me, I'll tell them, but like,
Scott Benner 24:44
I don't know. Do you know? Why not?
Adele 24:47
Not really any reason. I just like
Scott Benner 24:51
not trying to avoid a conversation about it. No, just you feel dizzy, and it's something you keep to yourself. Yeah. How often does that happen to you?
Adele 24:59
Yeah, well, I know, like, I used to kind of just, like, think, like, if I was dizzy and my blood sugar like, wasn't like, low, I just, like, kind of like, ignore it. But now, like, my mom, like, kind of recently told me that, like, if I am feeling dizzy and my blood sugar is not low, I should still have candy. Is that helping you? Because, like, the um, the Dexcom doesn't catch up to like, um, just like a finger prick.
Scott Benner 25:22
Yeah, I would tell you, if you feel dizzy and your Dexcom doesn't say you're low, you should get your meter out and check your blood sugar. Yeah, okay, and then, but I take what she's saying. She's worried about when you're by yourself, she doesn't want you to ignore
Adele 25:35
sometimes, like I'm sometimes I'm at like, school or dance, so I don't have it. Yeah.
Scott Benner 25:39
I mean, better safe than sorry, right? That I get what I think that's like, I
Adele 25:43
think that's what it's like kind of going for,
Scott Benner 25:45
yeah, yeah. How frequently do you think you're low
Adele 25:48
sometimes, like, some, like, some days, like, not as frequently, but like, recently, it's kind of been a bit frequently. More definitely. Know why? Maybe, like, maybe because of, like, all the exercise or something.
Speaker 1 26:02
What number do you feel low at it differs, like, sometimes
Adele 26:07
under 70, like, maybe like 68 and like under that, I'll feel like a little bit more dizzier, but like a little bit dizzy. But then, like, if it's more in the 50s, I'll feel like, really dizzy. Have you
Scott Benner 26:20
ever gotten to the point where you can't help yourself? Like, been so low,
Adele 26:24
kind of like, yeah. Like, I was like, Oh my gosh, when will the Disney dizziness be over? Yeah?
Scott Benner 26:30
And then somebody was helping you, yeah. Okay, swimming. You swam with OmniPod five and Dexcom, yeah. G6 so there's an opportunity that even people who you don't know are now going to see your stuff. Did you find yourself talking to them about it? Did you find that people cared or did they not even mention
Adele 26:50
it? People didn't really mention it much, but like, Yeah,
Scott Benner 26:54
more conversations or not. Not really, not really. Have you ever been bullied or picked on about it.
Adele 27:00
No, no. Sometimes, like, people would kind of make jokes about diabetes, like, even if it's just on, like, YouTube, Pinterest, or, like, just people saying it, I'll get a little bit offended, even though, like, they say, like, kind of you shouldn't be, like, getting offended that.
Scott Benner 27:16
Well, that's interesting. So if, if you see somebody joking about it, it feels offensive to you. Do you, are you actually bothered by it, or do you think you're supposed to be bothered by it?
Adele 27:25
It's like, in between, like, I'm it's not like, I'm gonna like, it's like, I'm a bit bothered by it,
Scott Benner 27:31
kind of, but you don't hold on to it, like you're not mad about it a day later, or something
Adele 27:36
like that. Like, some of the jokes kind of would be like, kind of, like, when people say I'm eating too much sugar, I'm gonna get diabetes. Yeah, like, I sometimes, like, I'm like, I don't think that's how diabetes works, not
Scott Benner 27:49
how I got diabetes. I got it the old fashioned way. My pancreas stopped working. Well, okay, but not upsetting. Like, you know, oh my gosh, I need help, or, like, you're not overwhelmed by it or anything like that. Yeah. Okay. How is it with you have a sister, right? Yes. Okay. Do you guys talk about your diabetes at all? Does it come up? Like, what's the interaction between the two of you? Like, regarding that sometimes, like,
Adele 28:18
she can't it's like, kind of like, annoying. But, like, not really, like, any conversations. Like, she used to, like, kind of ask my mom and me about it, but I think she knows more now,
Scott Benner 28:31
annoying because she's asking questions.
Adele 28:34
No, like, more or less, kind of, like, I It's like, kind of weird, like, it's kind of like, like, sort of embarrassing to me. Like, like, when I'm, like, taking care of my diabetes, like, with my mom, or, like, my sister, but like, then, like, I'm, it's less embarrassing when it's like, it's kind of cool for me, like, when it's people, like, who are not my family, and like,
Scott Benner 28:59
okay, embarrassing because it's taking up time, and everybody's just sort of standing around waiting for this park to be over. Like, do you feel like you're the center of attention?
Adele 29:09
Not necessarily. I don't know. It's kind of hard to explain.
Scott Benner 29:12
Yeah, no, I understand. That's why I'm that's why I'm asking. Because I don't think people would think about stuff like this as frequently you think your sister feels like you get more attention than she does?
Adele 29:22
She has said that before, yeah. She was like, um, you're it's also because, like, I'm the older sister. She's like, she's like, Adele's the older sister. She has diabetes, like, she's spoiled or whatever, but I'm like, I'm really not
Scott Benner 29:37
just have diabetes. Do you Do you ever say anything to her, like, I don't know. Like, why don't you get diabetes, and then you can have all the attention too, and then see, that wouldn't be good, right? Do you feel badly that she feels badly? Or do you feel annoyed that she's I'm
Unknown Speaker 29:53
kind of annoyed
Adele 29:54
because, like, I feel like she's kind of overreacting. I. She doesn't really fully understand either. And to
Scott Benner 30:02
her, it doesn't seem that way. No, no. To you, I'm
Adele 30:07
not totally sure, like, what my sister thinks, like all like about all of it. So you're
Scott Benner 30:11
not totally sure what she I don't I'm not sure what anybody thinks. So you have any questions for me?
Adele 30:16
Not necessarily, like any questions. I don't think,
Scott Benner 30:19
do you know, like, the podcast, I would
Adele 30:22
I, like, I wanted to start listening to it, but, like, I haven't yet, because I, because I went on the app to, like, do it, and then I kind of, like, got confused. Like, I don't know it's a kind of setup, weird.
Scott Benner 30:34
Yeah, I'm not in charge of that part. But do you want to talk about, um, like, what do you want to listen to? Like, management stuff, about, stuff about, stuff about, like, taking care of diabetes. Do you have questions, or did you want to hear people's stories? People's stories, yeah, you don't want to listen to, like, how to bolus for a meal and stuff like that. Sounds kind of boring, right? Yeah, it is a little boring. People's stories. Well, some of them are not age appropriate, and some of them are, some of them are really very much. So that's interesting. Yeah, those podcast apps are, I don't know why they're set up the way they are, but it's just what we're stuck with. If you ever get interested and you want to listen to conversations about managing basal insulin and your diabetes and stuff like that that you might be, you know, looking for more information. There's lists of like the Pro Tip series and and stuff like that that you could listen to. So that should make it a little easier to find the episodes. Okay, all right. What else do we have going on? Do you have worries about the thing on what happened are you? Are you quacking? What is that? Oh, it
Adele 31:35
was just one of my pre so I have these pre bolus alarms for school, and I forgot to turn them off for today?
Scott Benner 31:40
Do you not have school today?
Adele 31:41
No, how come? Because it's parent teacher conferences. Oh,
Scott Benner 31:46
that day where they pretend they're doing something and you get a day off. That's nice. Who cares? They should do that all the time. Do you ever, yeah, exactly. Do you ever think about the future with your diabetes, like, as you get older? Do you have concerns or thoughts about that?
Adele 31:59
I'm just like, a little bit scared to start taking care of all the by myself, because, like, some locations it's hard for me to, like, put on, like, my arms, like, I'd have to be like, and like, I'd be like, struggling, yeah,
Scott Benner 32:11
you'll figure it out. It'll really be okay. It really will be so worried about placement of pods, stuff like that, you're too young to you're not thinking about, like, dating, right? No, no, no, really, are there kids you think are cute? Or are we up to that yet? Or no, maybe, maybe, oh, I see, yeah, don't say their name. It's fine. I think we know who you're talking about. Okay, so, okay, so that's the thing, but not for now. You're more worried about where to put the devices
Adele 32:41
I have, like, seen, like diabetes, like YouTubers. So I know there's like, um, so there's this young, like, young like, so there's a toddler on, like, a middle like, um, um, like, a teenager, I think. And then there's like, an adult. And like the toddler, like her mom, like does, like her stuff, and then the teenager, like her dad helps her. And then like the like, grown adult, like,
Unknown Speaker 33:09
so do you kind of, like,
Adele 33:11
interesting for me to watch?
Scott Benner 33:13
Do you search out diabetes content on social media? Yeah, sometimes,
what are you looking for
Speaker 1 33:19
when you're doing that, kind of just like, just seeing other people like and how they handle it.
Scott Benner 33:25
Does it make you feel comfortable that they're okay? Or are you looking for suggestions? Just sometimes,
Adele 33:31
just kind of like, hey, like, they have diabetes too. That's kind of neat. Just looking
Scott Benner 33:35
for somebody who's similar. Do you know anybody in real life who has diabetes? Actually,
Adele 33:39
yes. Fun story. I actually just meant, like, the my crew. Teacher, so crew is, like, this like thing we have, like, in our school. It's pretty new, unique, I think. But like, basically, just like a bunch of kids, and we kind of, like, circle up and talk about stuff. Oh, I thought it was growing teacher, um,
Scott Benner 33:57
I'm sorry, when you row, when you row, it's also called crew. And I thought, Wow, you look young to row, but that's okay. Okay. Now, okay, so tell me more about this. You guys get together and talk, sorry. And
Adele 34:08
then, like, my crew teacher, her, um, her, like, friend, like, so she's a Spanish teacher. And then there's like, a Spanish teacher in the high school. He's a dad also, and he, like, came in one day and like, I told my teacher about like, this podcast. Because, like, I was excited. She was, like, telling him about it. And he was like, um, like, they called me over. And he was like, hey, my my daughter actually just got diagnosed with diabetes, so she's in eighth grade, and I got her like, phone number, and like, kind of started talking. Because, like, I'm like, if she wants to talk about anything, yeah.
Scott Benner 34:41
Oh, that's fantastic. Isn't that nice that you could could meet each other like that? Do you think you'll meet in person one day?
Adele 34:47
Yeah, we were actually just texting her, like, how we should meet someday. Nice. That's
Scott Benner 34:51
excellent. How old is she And how old are you?
Adele 34:53
She's like, in eighth grade, so probably, like, 1314, Oh, you
Scott Benner 34:56
guys are the same age. Then, okay, what do you like doing? In, like, in your free time, not like school, not act, not like planned activities, like dance. But what do you enjoy with your free time?
Adele 35:07
So I like plan stuff with my friends. I go on call with my friends. I play, like, video games, watch stuff. I also hang out with, like my neighbors, because I have some neighbors that are like, kind of like my age, a little bit younger, and then my sister. We all, like, hang out all the time. Do video like, right down the road for me, do video
Scott Benner 35:25
games make your blood sugar go up? No, I don't think so. You don't get that like, crazy excitement.
Adele 35:32
No, no. Sometimes, like, when, when I'm with my friends, like, I was hanging out with my two, like, two of my best friends, and my Nana was like, You guys are making her blood sugar go hide because you guys are, like, so excited, yeah,
Scott Benner 35:44
adrenaline can make it go up this. So what kind of games do you play when you play video games?
Unknown Speaker 35:48
So I
Adele 35:49
play, um, this, like Roblox. It's like an app, like, on my phone. So
Scott Benner 35:54
I know, yeah, I know what it is. That's what you are. Yeah. Are you jealous that I can sit back and go and sit up because my microphone moves, or no, because you're like, all having to sit up. And I'm like, sometimes I sit back. I got a comfy chair. All right, nice. What are your favorite subjects in school? Do you think about college?
Adele 36:14
So like, I do, like, I like Spanish and then science, but I actually do want to be a diabetes educator when I grow up.
Unknown Speaker 36:21
When did you start thinking about that
Adele 36:23
a little bit after I got diagnosed, and, like, more or less last year? Okay, so, yeah, I, like, always talked about it kind of, were
Scott Benner 36:34
you science oriented before that? But like, good at science,
Adele 36:38
and I wasn't really thinking at first, like, I wanted to be, like some sort of Doctor, vet, but, yeah,
Speaker 1 36:44
okay, so it's still in like, the same field,
Scott Benner 36:47
yeah, no, that's great. Well, that's excellent. So you're, you'll be working and thinking about that as you, as you make your way through school, things could change. Maybe they won't. But I was just talking to, I think my interview with a doctor goes up next week. He has type one diabetes, and he's an endocrinologist. And I asked him, would you be an endocrinologist if you didn't have type one diabetes? And he said, I don't think I would be so pretty interesting. You don't know how it'll shape your life. You know, all kinds of different things that could happen along the way.
Adele 37:18
Oh, yeah. I just thought of a question. Oh, um, when we did like, when we were, like, in Florida for the type, like, the touched by type one conference, you know, like the, like, the podcast that was recorded at the end. Yes,
Scott Benner 37:29
what did I ever do with that? Oh, Adele, I did not like the way that audio sounded. So I'm sitting on it. I don't know. You see the room didn't sound very good. I apologize, Yeah, makes sense, yeah. Did you enjoy that day at touch by type one? Yeah,
Adele 37:44
it was kind of like the first taste of, kind of doing a podcast thing.
Scott Benner 37:48
Oh, okay. Did you like it, like when we sat and talked, and even now, like you're, you're enjoying this, yeah? So you were telling somebody you were excited about it, what? What made you like? What? What makes this an exciting thing? Because I do it every day, so I'm not that excited, right? Excited right now. So, like, what? What makes it exciting? Like,
Adele 38:06
a lot of people see it, and how I could kind of like, share, like, my story, and, yeah, kind of like, it's like being it's like a new experience for me.
Scott Benner 38:15
Yeah, oh, I like that. Is it going well? Like, are you having a good time? Yes, yeah. I
Adele 38:21
kind of like, just being, like, ask questions, getting to talk about it and stuff, nice.
Scott Benner 38:25
What if I made this your podcast? What would you ask me? Like, just flip it around for a second. I'm a guy. I make a podcast. I have a daughter. She has diabetes. I have a son. I have a wife. Like, what would you ask me if you had to, like, if you had to drive the conversation,
Adele 38:42
I would probably like, just like, ask, like, about, like, how, like, you take care of her, like,
Scott Benner 38:47
like, kind of, yeah, when she was 12, or now, like, just, like, throughout everything, throughout everything. Well, that's a big question, isn't it? Gosh, we, we've had so many different changes about how things have worked over the years, different technologies. She's a different person. As she grows up, I've got more knowledge, and hopefully as I go on, I get better at it and calm her. I used to be more like, like, I didn't know what I was doing, and then I had to figure out what I was doing, and I would have, like, these big feelings when stuff would happen, like, if a blood sugar, like, was like, crazy, I they said you could see it on my face, like, and I don't do that anymore. Like, I don't get like, oh, like, you know what I mean? Like, like, irritated or annoyed or sad, when you see a number, it's not right. But I used to do that. I don't do that anymore. Nowadays, she's in college. I have not looked at Arden's blood sugar yet today. So it's noon. I haven't looked at it. Let me see it's Oh. Do you want to guess what it is?
Adele 39:51
I'm gonna say like 141, 50 1060,
Scott Benner 39:59
i. This is here. That's the last 12 hours of her blood sugar. Oh, that's pretty good. Top line is 120 and the bottom line is 70. That's pretty cool, huh? She was up late working. She stayed up till at least three o'clock in the morning working on a project at school. And it looks like, looks like she got up to 169 and then got it back down pretty quickly, like 169 is the highest blood sugar she's had in the last 24 hours. She's doing well. I have talked to her this week about her diabetes. Not much. To be perfectly honest, I helped more with saying stuff like, Hey, did you go grocery shopping? Do you have food in the house? Like, you know, I know you're busy, but have you checked on this? Like that. That's kind of stuff I've you don't want to have to go out and get fast food, like that kind of stuff. Do you take your vitamins? Like stuff like that. I've been doing I do that stuff. You know, not as much involved anymore. She's very good at counting her own carbs and handling her highs and her lows. I did send her five pounds of gummy bears the other day. Did you know you can buy gummy bears in five pound bags? No, what do you treat your lows with? Like,
Adele 41:14
sometimes, like gummy patches. But the thing we use the most, but we ran out of, are these things called, like, high Chews. They're like, four carbs each, and they just like, they work well,
Scott Benner 41:23
you like those high Chews? Arden uses Albany. This is how you say it. I'm gonna, I'm gonna look it up real quickly so they don't say it wrong. She uses, yeah, Albany's world's best 12 flavored gummy bears. They come in five pound bags. You can get them on Amazon for $15 so she was, she left for college with so she's been gone now, January, February, she's been gone eight weeks since she left last time to go to college. I think, I think she left with half of a bag of these. So, like, probably, like, you know, two pounds of them. And she just uses them a couple at a time. And she also says her roommates hit them pretty hard too. So they get hit by, I think everybody in the there's four girls there. And like, a week ago, she just said, Hey, I'm almost out of gummy bears. That was, like, the most like, contact I had with diabetes for a while, so I sent her more, and I actually think they arrived today. So that was one of the things I've done this week. Yeah. I mean, that's about it. Like, you know, reminding her if she if she seems to forget, but she's pretty good at it by now. So, like, I will tell you this when she was 12, if I would have asked her, What are you worried about? She'd be like issue, I guarantee would have said, I don't know how to get something on the back of my arm by myself. I don't know how to like, you know, I don't know how to do this, I don't know how to do that, and none of that stuff is a problem anymore. So one day, you'll just know how to do all that too. I think I'm pretty sure. What do you understand about diabetes and your health, like, not just your health today, like, not not just not being dizzy, but like, long term, like, as you get older, what, what is your understanding of all this? I'm kind I'm kind of confused. Like, you know, if you eat junky food, you'll gain weight, right? Yeah, you know, if you don't exercise, you'll get stiff. What is it you understand or don't unders? Do you understand about your diabetes and your long term health, like why it's important that your a 1c is a certain number, why you don't want high blood sugars or super lows?
Adele 43:34
Not really understand the a 1c really, but I know most of the stuff. I think so
Scott Benner 43:41
for you, the A 1c is just this idea of a target, and we're trying to get it lower, but somebody doesn't tell you, like, hey, we want your a 1c to be lower, because they don't do that, right? No, it's just a thing you're supposed to do. Okay? Well, Oh, that's interesting. What would happen if you got way too much insulin? Do you know my
Adele 44:03
blood sugar would be going lower because, like, too like, too much insulin, too
Scott Benner 44:09
much insulin. What? What would happen if you didn't stop it from going lower? Do you know
Adele 44:12
I would, like, eventually, like, pass out because, like, yeah,
Scott Benner 44:17
like, you'd have a seizure eventually. What happens if your blood sugars are high for years? I don't really know. That's interesting. Okay, all right, so I'm not your mom, so it's not my job, although your mom's probably gonna send me a note and be like, hey, but they're real. They're real important, long term reasons why you wouldn't want higher or bouncing around up and down, blood sugars, and if, I mean, I'm not your uncle, so I'm not going to tell you, but there is an amount of insulin that could kill you. You know that? No, no, am I the one telling you this? All right, hold on a second. Don't forget. Say it again. Okay, say it so. Oh. Gosh, I'm sorry. All right, hold on. If you had, like, I don't know how much insulin you get during you said, like, 70 units, right? And that's spread out over your entire day. Some of it's basal, some of it covering meals, etc and so on. You get low blood sugar if you have too much insulin. So if you have too much insulin, and you don't have enough like, either like, you know, stress or food to, like, push it back up again. Your blood sugar keeps getting lower. You get dizzy. You eat some food, it goes back up. You understand that. But if you gave yourself, if you gave yourself way too much insulin, and didn't do anything about it, you would get dizzy, pass out. And if somebody didn't do something about it, you're not that would be the end of it. No one's ever told
Adele 45:44
you that before. Um, nobody ever told me that, but I kind of knew it.
Scott Benner 45:48
You knew it. Okay. Well, thank God, because I felt like an Can I curse you're only 12. I felt like for saying that right now. And I was like, Oh my God. But then I could see on your face you were like, I think I know what he's saying. So, so, like, is that a thing you've, like, ever consciously thought about? Like, like, I know why this is important, or is it just the thing you used to kind of out of sight, out of mind? I've
Adele 46:10
never really thought about it because, like, I know how to, like, treat low blood sugars, like, and like, I know like that. I need to have candy. Like, if it's low, yeah, going low, or too much insulin, like, my mom, like, my mom or nana will be like, oh, like, I over, like, I put in too much, like, insulin Here, eat this.
Scott Benner 46:27
Do you think they know? They do, right? Like, you're probably, probably, yeah, I hope so. All right, so it's a story I just know about this kid who had diabetes for a few years and, all right, well, you know this, so it's okay to tell you the story. So there's this kid, right? And he's got diabetes for a few years, and one day, his mom has to, like, leave the house, and she leaves her the kid's older brother in charge, and they had just given the kid a bunch of insulin, and he was eating. So the mom leaves, and the the slightly older brother is in charge, and the kid doesn't want to finish eating his food. And the and the brother, the other brothers, like, you have to eat this. And the kids like, I don't want it. I'm not hungry. And he's like, You have to eat this. And I guess the the older brother kind of panicked a little bit, and when the kid resisted eating the food one more time, he said, If you don't eat this, you're going to die. And the kid didn't, like no one had ever discussed with him, like, the ramifications of wildly using too much insulin and not, you know, covering it. The kid like, fell apart. Like, you handled it really well just now, but you knew already, like, you know what I mean. But this kid, like, was like having an existential crisis. Like, right? Like somebody just explained something to him that he had no idea about. Then they the family had to wrestle with the idea that the kid felt like they kept that from him. Do you know what I mean? Like that, it was like a important part about his life that nobody shared with him. I don't know you. Seemed like you knew what you were talking about, about diabetes and everything, and I was just like trying to pick around to see what you knew. I definitely regret saying this to you now, because you're not my kid, but I mean, your mom said you could come on, so whatever, you're okay, right? Yeah, yeah, you're not free. You look completely fine, like, I I'm upset now, and you're like, I don't know what you're upset about, but do you talk about your diabetes on social media?
Adele 48:19
I don't really have, like, a ton of social media. I have, like, Snapchat, but like, I don't really talk about that kind of stuff, a ton on there.
Scott Benner 48:28
So it's not like, you're not doing, like, like, here's a picture with my CGM like, you're not, you're just being yourself. You don't necessarily need to be a person who has diabetes. I like,
Adele 48:38
could do that. Like, look, look at this new patch. I could do that, but really, I don't do it much. Yeah. So like my mom, I think, I think, like, my mom has, like, diabetes, like social media stuff, though, does she like on Facebook?
Scott Benner 48:52
My daughter doesn't hide her stuff, but she doesn't, on purpose, share it either. Like, sometimes, like she's in fashion school, so she'll do a lot of, like, get dressed, get ready with me. Videos. You must know what those are, right? Where, like, people put clothes on. Yeah, yeah. I know you're like, yes, old person. I know what it is, but she does that kind of stuff, and she doesn't make any effort to hide her diabetes. She's never, never tries to hide it, actually. But she also wouldn't do that thing where she was like, here, look, this is my insulin pump. You know what I mean? Like, I don't think she wants to be, yeah, famous is the wrong word, but she doesn't want people to know her for her diabetes. She wants you know that is that kind of how you feel about it? Yeah, I'd say so. Like, it's okay if they see it, but you're not going to go out of your way to show it to them. That makes sense. Yeah, yeah. Here's a picture. I wonder if I can show you this. Can I screen share?
All right, ready?
Adele 49:55
I'm I'm not sure if that's a cap on here. Oh yeah, yeah. I see a button. Honestly. It.
Scott Benner 50:00
I'm going to show it to you. Okay, so can you see her? Yeah, okay, so you can see how her pods on her arm, so she's not making any effort not to show it off. It's just like she's not trying to hide it. And you can see that's an outfit she wore to class. So she's not trying to hide it, but she's also not, like, pushing it forward. Does that make sense? Okay? Well, I was like, I'm gonna stop sharing now. That's so weird, because it's like an Instagram thing, and it just keeps repeating over and over again as it repeated the third time. I was like, Oh, my God. All right. Any other questions for me? I don't think so. Have I not asked you anything that I should have is there anything that we should have talked about that I didn't bring up, like, what's on that list over there? I don't think there's really anything else we did. Okay, yeah, did you have fun? Yeah, yeah. Was it less fun than you thought it was gonna be? No, not really. No. That's cool. So it's about what you expected. Yeah. Do you know what I'm doing now? I am gonna go. I'm gonna go have a sandwich, and then I have to drive about two hours to this place where I'm gonna talk to a group of, like, 400 type ones all weekend. Oh, so I'm gonna do a talk this afternoon in about I should probably get going about three and a half hours. I'm gonna give a talk in about three and a half hours, and then do another one tonight, and then a couple tomorrow, and then one on Sunday morning, and then I'll head back home. So I'm there's an event for people with type one diabetes, and I'm one of the speakers. So I have to, I have my bag all packed. It's in my car already. The last thing I was doing today was talking to you before I left. So I appreciate you. Let me move the time. That was nice of you.
Unknown Speaker 51:42
Thank you. Yes, of course. Cool.
Scott Benner 51:45
So do you think you'll let your mom listen to this?
Unknown Speaker 51:47
Of course? Yeah, I
Adele 51:49
don't really think I could stop her either.
Scott Benner 51:51
I mean, you know, I It's a good point. What should we call this episode?
Unknown Speaker 51:54
I don't really know.
Scott Benner 51:56
Well, your name's Adele. We could just call it Hello, that would be good. Hello. It's me. That's not bad. Do you hate
Speaker 1 52:03
that? Honestly, no, no, that's actually kind of neat. You're good with this singer,
Scott Benner 52:08
yeah, your name, yeah, I like how you're like this singer, that woman who has my name,
Adele 52:15
yeah, when I search up my name on Google, that's what pops up.
Scott Benner 52:17
Oh yeah, when I search up my name on Google, nothing comes up. Nobody's name Scott, just nobody. It's like Name a famous Scott. Go ahead.
Speaker 1 52:25
I have an I have an uncle, Scott. He's not famous. Name a famous Scott.
Speaker 1 52:29
I don't know Scott terrible.
Scott Benner 52:32
That's why nobody famous has his name Scott, because it's just a terrible name. Adele, you were lovely. Thank you for doing this. I appreciate this very much. This is a nice chunk out of your your free day. What? What is the rest of Adele's day? Look like?
Adele 52:45
I think we're gonna go to the mall, and I might hang out with my neighbors.
Scott Benner 52:49
Big plans. I'm doing what I just told you. I don't like the food at the place I'm going, though, so the last thing I'm doing is taking food with me. My wife's like, you're gonna insult them. I'm like, I'll hide it in my room. I don't want their food. It's okay. If they hear it, they'll understand. Not you so much, because I'll tell you about it a second. Okay, we're done. I'm gonna stop. Okay, hold on one second, but you stay there.
This episode of the juice box podcast was sponsored by us. Med, us. Med.com/juice, box, or call 888-721-1514, get started today with us. Med, links in the show notes. Links at juicebox podcast. Com, I want to thank the ever since CGM for sponsoring this episode of The juicebox podcast, and invite you to go to Eversense cgm.com/juicebox to learn more about this terrific device. You can head over now and just absorb everything that the website has to offer. And that way you'll know if ever sense feels right for you ever sense cgm.com/juice box. A huge thank you to one of today's sponsors, G VO, glucagon. Find out more about G vo hypo pen at G VO, glucagon.com, forward slash juice box. You spell that, G, V, O, k, e, g, l, U, C, A, G O n.com forward slash juice box. If you're newly diagnosed, check out the bold beginnings series. Find it at juicebox podcast.com, up in the menu in the feature tab of the private Facebook group, or go into the audio app you're listening in right now and search for juicebox podcast, bold beginnings. Juicebox is one word. Juicebox podcast, bold beginnings. This series is perfect for newly diagnosed people. A diabetes diagnosis comes with a lot of new terms, and you're not going to understand most of them. That's why we made defining diabetes go to. Juicebox podcast.com. Up into the menu and click on defining diabetes to find the series that will tell you what all of those words mean, short, fun and informative that's defining diabetes. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast. If you're not already subscribed or following the podcast in your favorite audio app, like Spotify or Apple podcasts. Please do that now. Seriously, just to hit follow or subscribe will really help the show. If you go a little further in Apple podcast and set it up so that it downloads all new episodes, I'll be your best friend, and if you leave a five star review, ooh, I'll probably send you a Christmas card. Would you like a Christmas card? The episode you just heard was professionally edited by wrong way, recording, wrong way, recording.com, do.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!