#1283 The Crack
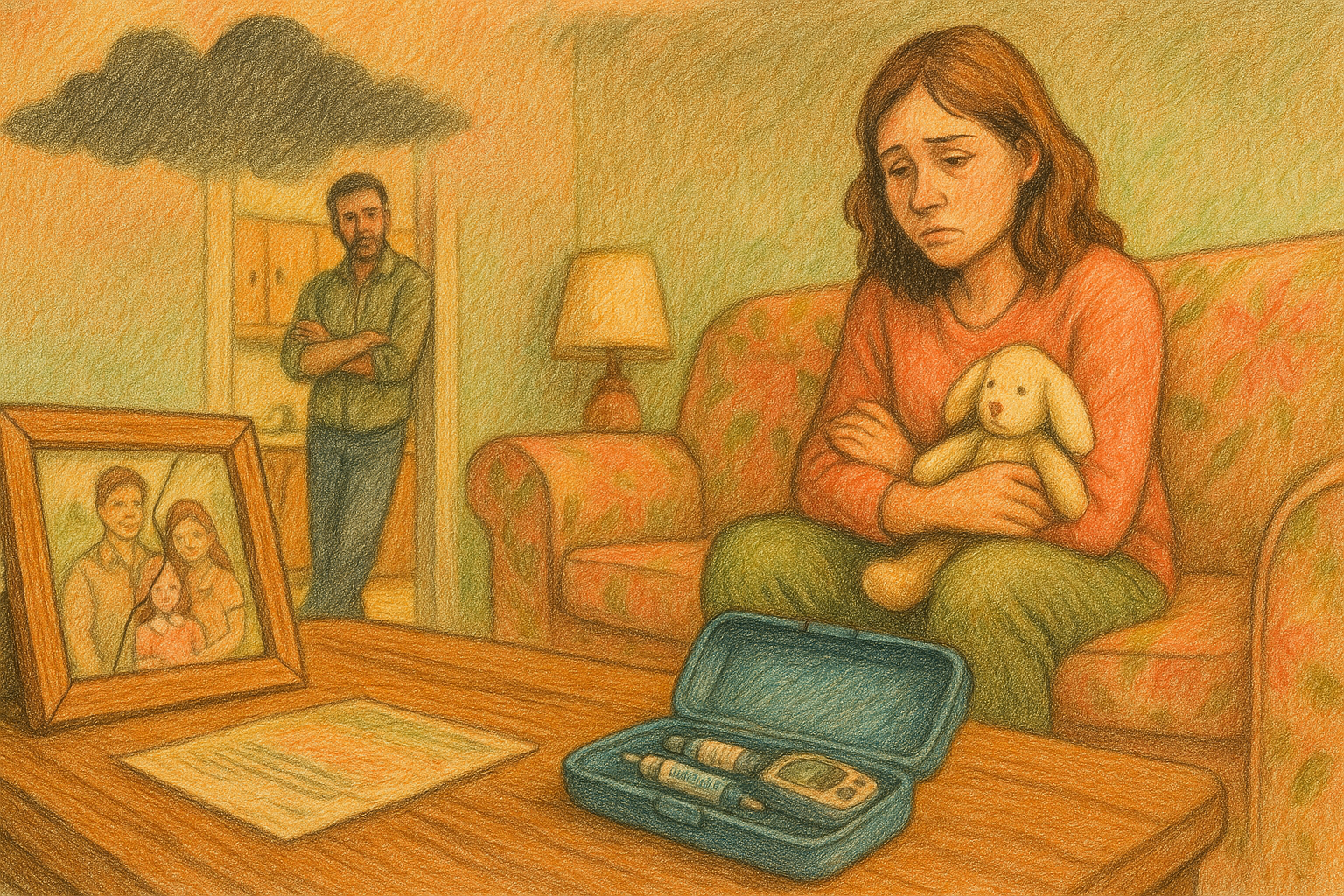
Sarah is from the England. Her mother has type 1 and her daughter Poppy too and was diagnosed when she was 5.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome back to the juicebox podcast.
Let's see what I've got for you today. Oh, this is Sarah. She's from England. She has a son, Aiden, who's 11, and a daughter named Poppy, who's nine. Poppy has type one diabetes. We're gonna talk about OmniPod five raising children with type one and much more. There was a lot of consternation here about what today's episode would be called, but I chose the one you're seeing in your player right now. So blame me if you don't like it. Please don't forget that nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan or becoming bold with insulin. Don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juicebox at checkout. That's juicebox at checkout to save 40% at cozy earth.com when you place your first order for ag one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. Ag one.com/juice, box. If you're looking for community around type one diabetes, check out the juicebox podcast, private, Facebook group juicebox podcast, type one diabetes. But everybody is welcome. Type one type two gestational loved ones. It doesn't matter to me, if you're impacted by diabetes and you're looking for support, comfort or community, check out juicebox podcast type one diabetes on Facebook. The episode you're about to listen to was sponsored by touched by type one. Go check them out right now on Facebook, Instagram, and of course, at touched by type one.org check out that Programs tab when you get to the website to see all the great things that they're doing for people living with type one diabetes. Touched by type one.org. This episode of The juicebox podcast is sponsored by hungry root, the easiest way to eat healthy. Hungryroot.com/juice, box. This episode of The juicebox podcast is sponsored by the ever since CGM. And sure all CGM systems use Transcutaneous sensors that are inserted into the skin and last seven to 14 days, but the ever since, sensor is inserted completely under the skin, lasting six months, ever since, cgm.com/juicebox, hi.
Sarah 2:33
My name is Sarah. I'm from the UK, and I have a 11 year old son called Aiden, and a nine year old daughter called Poppy, and she is my type
Scott Benner 2:45
one. Aiden is how old? 1111, and I, for the life of me, think you just told me your daughter's name is puppy, but that can't be, right?
Sarah 2:54
It's Poppy, like the flower got it.
Scott Benner 2:58
I was like, that would be a horrible name for a child. How old is she? She's nine, nine, right? Sarah, how old are you? I am nearly 45 I would have been alright with Navy said 44 I would have, I would have told on you, you're 45 you're married. I know that because of speaking prior to the recording. You have two kids. Poppy is nine. She has type one diabetes. How old was she when she was diagnosed? She was 554, years ago. Okay,
Sarah 3:28
it's actually her diversity today is exactly four years ago today. Did
Scott Benner 3:32
you do that on purpose when you signed up? Yeah,
Sarah 3:33
okay, I did because I knew I wouldn't forget the date. A lot of people do
Scott Benner 3:38
that. I used to think it was a coincidence. Then one day, I was like, you know, they're probably doing this on purpose. And then I stopped being stupid, because I was really like, people would say it over and over again. I'm like, what a coincidence. And I realized
Sarah 3:50
that I had the choice of dates, and I thought, yeah, I've got to do on that day, definitely, Sarah.
Scott Benner 3:55
We're gonna have to get this out of the way right away. And I'm gonna curse for a second, but it'll get bleeped out. Don't worry. You sound like Mary Poppins. Fidel, now, why?
Sarah 4:09
Okay, that's brilliant. Yeah,
Scott Benner 4:12
where are you about? Where are you from that your accents like this. Okay, so
Sarah 4:16
it's a bit I wouldn't even have noticed it's mismatch, but, so I was born and bred in London. Um, so, but not I'm kind of, what we say is half cockney. Some people think I'm cockney, which is the kind I don't know how to describe that.
Scott Benner 4:31
More of the cock the cockney is more Adele, yes, the Cockneys more adult, yeah, 100%
Sarah 4:39
but then some other people think I'm the Queen's English upper portion, upper crust, they would say, but I'm totally not either. I'm I'm a mismatch. Yeah, no, I
Scott Benner 4:50
heard the mix right away. It's really interesting. Also, I had a girlfriend once that said I was half cockney, but I think she was just trying to be mean. What are we gonna do? Did that not translate? Sarah? Did. Don't worry, it'll come to you later. Now, which is what I told that girl, let's get through Oh my, fantastic. I'm gonna tell you at the very end, because it's meaningless and it drops so dead in the water. I was like, Oh, wow. Somehow that didn't translate. That's fantastic. All right, don't worry about that. We'll move forward. There are Americans laughing right now as they're listening. Love it. Here's what we're gonna do. We're gonna find out a little bit about Poppy's diagnosis. So how did you see it? What were the steps that happened? You know? What was that first couple of days like? Well,
Sarah 5:35
typical, but there's a little backstory. So it was Christmas, 2019 and both children we thought were just being the worst, worst behaved children ever, ignorant, ignoring us, not doing what they'd been asked to do, not coming to the table. When we said teas, really all of this just ignoring us. And we were like, What is wrong with both of you? Both of you are being bone idle. Why are you ignoring us? You're being terrible. Christmas holiday. So turns out they both had ear infections at the same time, so couldn't hear us.
Scott Benner 6:11
Seriously, seriously,
Sarah 6:15
we had, literally, for a week or so during this school holidays, been shouting like unreservedly, at these two terribly behaved children. So they were, she was five and he was seven. And we just thought, What is going on here?
Scott Benner 6:34
Were they not in pain? No, no,
Sarah 6:37
anything. But we just thought, because it had gone on for so many days. We were like, there's got to be something wrong. And I think Chris, Chris, he was feeling under the weather or whatever. So we went to, what we have here is a walk in center, so it's an emergency. You can walk in and you get, like, a little ticket, and you wait your turn, and you see someone within a couple of hours. So he was going to check, and it turned out he had a viral infection. So he was feeling what, you know, man flu. We thought it was, but it turned out to be a viral infection. And
Scott Benner 7:07
we said, Well, why you thought it was the man flu? Meaning you thought he was just being lazy.
Sarah 7:14
Oh, that's a common term over here. Yeah. We call it whenever a guy is like, Oh, I feel like I've got a bit of a cold and, oh, I need to be wrapped up in a blanket. It's like, yeah, that's man Flo there's nothing wrong with you. Just go for it. You
Scott Benner 7:27
think boys do that to get a little time off, a little bit? Yeah, I haven't done that. Should I try that? Like, just walk downstairs and go, like, I can't today and sit on the sofa.
Sarah 7:37
Some women will give you some sympathy. Majority of women probably Kelly might not give you. That's the one I picked. No, I don't think she might be wise to it, but this many years, but you've already confessed you don't get ill. So yeah,
Scott Benner 7:50
it's true. I really don't get sick very often, so it would be hard for me to and when I do, I get sick very quickly, and it's over. Also, like, I make this announcement, go to bed, wake up in the morning, and it's gone. So yeah, all right, so he's, everybody's sick. You're yelling at the gear. You're having conversations where you're like, hey, we wrote We raised terrible children. Look at them. Yeah,
Sarah 8:09
yeah. It's funny, okay, definitely, totally questioning our parenting. Just thought it was all going down the pan. So yeah, they said, Can you just have a look at the children, because they have, you know, whatever. And they said, Yep, they both got ear infections, so it gave them antibiotics, sent us away. We felt terrible. Then they went back to school. Aiden recovered his ear infection. Went totally fine. Poppy seemed to carry on. So when she went back to school, they said, Oh, she's having real trouble hearing us at school. We've like trying to, you know, do a little bit of sign language with her, and all this to trying to communicate. She can't hear the teacher. All this, it all kind of happened at once. Then she started getting picked on by some older girls at school. So she started getting bullied, which we did sort out. So since she was anxious about that, so
Scott Benner 8:58
then she started
Sarah 9:00
drinking and obviously urinating loads, and then it just it all happened straight away. So we went back to the doctor. We actually saw a GP, so our general practitioner six times, and every time even I said, my mum is type one, but at that point I didn't know the difference. So I said, my mum has got diabetes, and my dad had diabetes before he died. He was type two, right? I said to them, could this be diabetes? Obviously, just totally didn't know which type just could this be? And they were like, Nope, definitely not. That's not on my radar. It'll be, we'll check her for a urine infection. So checked her, gave us some antibiotics because she was sore, because she was going to the toilet all the time. So they were like, oh yeah. Well, it look, you know, down there. Looks tender, whatever. So I went back every single week, without fail, for six weeks in a row, saying she's not getting better. It was terrible. She was up throughout the night, drinking throughout the night, going to. At the toilet school was saying she's drinking three and four bottles of water a day, right? All of that, so at one point, so the final appointment that we went back and they said, No, we don't know what it is. What we'll need to do is we'll need to send her for blood tests to check her kidneys and something else. And the waiting list for those blood tests will be three weeks.
Scott Benner 10:21
I'd like to introduce you to your partner in eating healthy. Hungry root. The easiest way to eat healthy, hungry root has the best fruits, vegetables, premium meats, kids, snacks, soups and stews, baked goods and so much more. Hungryroot.com/juicebox you can save hours of planning, shopping and cooking by letting hungry root deliver food you'll love right to your door, and hungry root is here to support your fuel and goals. Do you need more vegetables, less sodium? Hungry root can make that happen. If you're ready to dig in, use my link, hungryroot.com/juice box. Links in the show notes. Links at juicebox podcast.com How many times have you thought it's time to change my CGM? I just changed it. Then you look and realize, my God, it's been 14 days already. A week, week and a half, feels like I just did this. Well, you'll never feel like that with the Eversense CGM, because Eversense is the only long term CGM with six months of real time glucose readings, giving you more convenience, confidence and flexibility. So if you're one of those people who has that thought that I just did this, didn't I why? Well, I might have to do this again right now. If you don't like that feeling, give Eversense a try, because with ever since, you'll replace the sensor just once every six months via a simple in office. Visit Eversense. Cgm.com/juicebox, to learn more and get started today. Would you like to take a break? Take a shower you can with Eversense without wasting a sensor. Don't want anybody to know. For your big day, take it off, no one has to know. Have your sensors been failing before 10 or 14 days? That won't happen with ever since? Have you ever had a sensor get torn off while you're pulling off your shirt? That won't happen with ever since? So no sensor to get knocked off. It's as discreet as you want it to be. It's incredibly accurate, and you only have to change it once every six months, ever since cgm.com/juicebox, what is this? The Is this the norm in this situation, in this healthcare situation? It
Sarah 12:35
seems to be they, they didn't in any way. So they, all they were doing was they checked her. She gave five urine samples. They never once checked the checked it for sugar. They just checked it for infections, which I just find bizarre, and they didn't bring a finger. And they just thought when, when I said, would this be diabetes? They just looked at her, and obviously she was a slight, tiny little thing, and thought, No, this obviously, was you thinking type two? So at that point, after six weeks, I was like, I cannot. I can't let this go. I can't wait another three weeks for blood tests. So I ran my mum. So my mum lives like a mile away, and I said, Can you bring your blood testing kit around? I can't. Something is nagging me. I can't let this go. I can't wait three weeks. I need to test her blood sugar, yeah. And so my mum was poorly at that time. She was like in her 80s anyway. So my sister, who lived with her, brought it round. So she brought her clinic, but tested it and again it had that high, which obviously so high that it can't read a number, yeah. So then just obviously I knew, I phoned our emergency care, 111, they said, go straight to A and E, which is accident and emergency, which is your emergency room. Just go there straight away. So I rang my husband. So my husband's a police officer. He works, so we're in the Midlands. He works in Birmingham, which is about an hour, 45 minutes to an hour's drive away. So I rang him and said, This is the crack we've she's got diabetes. We are going to an E right now get home. So he drove straight home. We went because I don't drive. So we waited for him to come home. He stayed with Aiden. No, he didn't. My sister stayed with Aiden, and we took her to the hospital. And yeah, within 15
Scott Benner 14:19
minutes, Sarah, you don't drive because you're a fancy lady, or because you don't have two cars. Or why exactly? Oh, I
Sarah 14:25
wish. Oh, okay, so there's another element in the story. I don't drive because I'm visually impaired.
Scott Benner 14:31
Okay, I didn't know that. It just seems strange in this day and age that you don't drive. That's all,
Sarah 14:36
yeah, yeah, yeah. I would love to be able to drive. But no, it's not on the cards.
Scott Benner 14:40
Also, I might call this episode the crack. You said that a minute ago. Do you know that I did say that? Yeah, I don't know. I assumed it meant, like, here's the skinny. This is what's going on, or something like that. So it means that's the this is the deal. Yeah, here's the situation, here's the situation. That's the crack. Oh. I don't know why, but I love it. And you said it. I was like, Oh, I'm gonna call the episode unless you say some other British thing, which you very well could.
Sarah 15:09
Okay, I'm sure I've got plenty. So
Scott Benner 15:12
we've got your husband coming from across town. I like that. You try to get your 80 year old mom to come over with a meter. She was like, I'm old. No, yeah. And so don't, you can't wait to be like. Just not wait to be so old that when somebody says something to you, you go, no, no, I won't be doing that. She
Sarah 15:31
actually said that. She probably didn't. I don't remember. I was too polite.
Scott Benner 15:35
I just, I can't wait to be old like that. You don't even just like, I'm like, I don't care what you think. But um, but okay. So got the meter find the blood sugar high, which, in the meters we have here is like over 500 actually
Sarah 15:47
have it. So it was, so when she was at the hospital, it was 576 Yeah. Okay, so, so 32 UK, wow.
Scott Benner 15:55
Now we do We? Are we waiting for our husband to get back to pick us up, or do we just find a different way to go? I'm trying to figure out, does he take that long drive to meet you at the so
Sarah 16:06
they said, Go to accident emergency. Now I rang him and said, Do you want me to wait? And he was already in the car, so he was home with he obviously broke the speed No, he didn't break the speed limit.
Scott Benner 16:18
That wouldn't happen. There weren't lights and sirens and driving very quickly. No, no,
Sarah 16:23
no, he did. He couldn't have taken a siren home with him. No, but he was probably home within half an hour. So we thought, they didn't say, I mean, I don't know, in hindsight, maybe I should have just gone on my own, but I didn't. I waited for him and we went together.
Scott Benner 16:35
No, of course, did they call them Bobby's where you are? Where's the economy? Yeah. Well, he's a Hang on. Let me think he's a police
Sarah 16:46
officer. He bobbies. Yeah, Bobby on the beat, yeah. I suppose they would. They would refer to them as that. Yes,
Scott Benner 16:51
that's all. I want to know. If my television watching is accurate or not. That's all, yes. Okay, yes. Alright. We get to the what did you call the emergency room. What do they call
Sarah 17:02
it? A na accident and emergency? Okay,
Scott Benner 17:04
you get there, Are you pissed the whole time that you've been trying to tell a doctor this for weeks? Or do you does that go
Unknown Speaker 17:12
out of your head? So it
Sarah 17:14
was just so it was so traumatic. So they they couldn't even, what were they doing? They were doing their toes. I don't know what they were doing. They couldn't get blood out of wherever they were trying to get it. So they end up doing her toes. And it was just all
Scott Benner 17:28
a horrible situation. But,
Sarah 17:32
yeah, no, they just only diagnosed her. They got her on a ward as soon as possible. I so at this point, obviously I know they're like, it's type one, it's insulin forever. I'm like, All right, okay, that's my mum is then. So I then clicked, my mum is type one. My dad was type two. I think he got type two in his 60s. But then and he managed to last that. He said, he said, his words last 20 years on diet and exercise before he then had to use insulin. So when he passed, he was on insulin as well, but I didn't know which. I knew they were different types. They both had different types, but I didn't know which, all right, obviously. And so this is a
Scott Benner 18:10
bit fascinating, Sarah. So we're going to take a left turn for a second. Your mom was how old when she was diagnosed
in her 30s? Ah, okay. But
How old were you then zero, right? So you were so so your entire life. Your mom's had type one diabetes.
Sarah 18:25
Yeah, yeah. She was diagnosed in her 30s after her third child. I was her fourth child, 42 Hold on
Scott Benner 18:38
a second. Your mom was a player.
Sarah 18:40
She had. She spent her whole life having kids. I think so. Do you want the story? God damn right. I do. Go ahead. Okay, so she got married at 17, okay, to my dad, who was, at that point, 26
Scott Benner 18:55
Oh, okay.
Sarah 18:56
I know, to me controversial, but in those those days, so hang on. Let me think, oh, do I know the year? So hang on. She would now be, she passed when she was 84 which was three years ago, 87
Scott Benner 19:11
so she would be 87
Sarah 19:14
she got married 75
Scott Benner 19:15
years ago. So, like it was the it was 1950 maybe, yeah, yeah, about well, so he, he had a job, so he was a good choice.
Unknown Speaker 19:25
He'd just come back from
Sarah 19:26
the army, okay? And he was a family friend of her mum and dad's, so they, like, loved him and all that. So the fact that he was 23 and she was at 17 wasn't
Scott Benner 19:35
wait 23 or 26 No, hang on, 23
Sarah 19:39
he was six years older than her. He was 23 she was 717. Did I get it
Scott Benner 19:43
wrong? You said 26 the first time, but that's 23 you know, it's funny. It's not any better. If a 23 year old came after my 17 year old daughter, he'd leave here with a stick on the side of his head. So, yeah, but okay, absolutely. 1950 they they get married, they make a baby, right? Away, yep, since
Sarah 20:01
she had my brother when she was 18. Okay, so they got married in the January, he was born 13 months later in the February. I
Scott Benner 20:10
hear what you're saying
Sarah 20:13
right away. Cracks on. Yeah.
Scott Benner 20:14
Wait, what was that? What was that saying? They cracks on. I don't know what the you're talking about. Doesn't matter. Okay, so did you hear that thing I did with that kid, the British kid, like a year ago,
Sarah 20:29
I have listened to every single episode. Oh, within 18 months,
Scott Benner 20:34
his accent was so thick that I was proud of myself when I understood what he was saying. Do you remember him?
Sarah 20:40
Oh, because there's only been so I've listened to all of them, obviously, but there's only been about 10 British that
Scott Benner 20:45
I think of he was on a reality TV show. Oh, yeah,
Sarah 20:49
I know him. Yes, I know him. And I went and googled him afterwards and found out who he was.
Scott Benner 20:53
Yeah, handsome boy. Am I wrong? A boy? He's a handsome boy. I
Sarah 20:57
said, well, too young for me. Well,
Scott Benner 21:00
I didn't say, well, not well, not too young for your dad, but go ahead. Okay. Now, so, so your mom and dad are knocking out kids. Tell me how many they had, and you were the Go ahead,
Sarah 21:11
four. So she waited 10 years, then after that. So I think they learned their lesson, having had one so quickly they thought, yeah, I think we should chill out now that was
Scott Benner 21:23
expensive and painful. Yeah, definitely okay. So she took a 10 year break and had another one at 2728 Yes, yeah, 27 and 30.
Sarah 21:36
So she had two close together. So I had two sisters. Have two sisters. So she had one at 27 one at 30 and then within a couple of years of her, of my second sister, she got type one. Okay, so that would have been in so my sister was born in 69 so early 70s, she was diagnosed, right?
Scott Benner 21:58
So there you go. So your mom, because that's the first thing I thought was like, was she, you know, she wasn't cranking out kids with type one, so she gets type one after her third that, am I guessing that slowed her down, but then she wanted to try one more time for a baby. Or did she get pregnant with you by mistake? I was sorry. I was conceived in
Sarah 22:20
by accident when my sister was, she says, dying in hospital with meningitis.
Unknown Speaker 22:26
Oh,
Scott Benner 22:27
they're just trying to get get rid of a little stress. Maybe
Sarah 22:31
it's not true. So, yeah, my sister got meningitis when she was 12, and was in hospital, critical. And they were, you know, she was in hospital for ages, and her my mom came in and told her the funny story my sister retells it so well, but she came in and said, Oh, guess what? You know, we thought I was going through the menopause, but no, looks like I'm pregnant. And her response was, you're already lining up my replacement. What is going on? I haven't even died yet. She she didn't. She recovered. Obviously, she recovered. She's fine.
Scott Benner 23:04
Sounds to me like your dad was like, I am feeling very stressed about this kid in the hospital. Yeah, you know what would help mother so and you can't get pregnant. You're so old, but then boom, here you come. Okay, I guess, nice, jeez. Okay, your visual impairment your whole life. Or,
Sarah 23:22
yeah, Googling it, I have thought that maybe it there. It has, has something to do with type one back then, as a mum having type one and visual impairments on the children. But it's never been as cut and dried as that. They've never really said that. It's just speculation. I
Scott Benner 23:40
mean, so this is really interesting, because your mom lives a long life with type one. She lives 50 some years with it, yeah, but you're unaware of her management in my mind, like, because it's not, it's not front of mind for you. So, like, did you not see her taking care of herself? That is the whole reason I asked about this, yeah. So she
Sarah 24:02
was, I think, in my mind that now, having known, obviously living with poppy for four years now, and knowing all the stuff, she must have been on a constant roller coaster. She must have been because the management that I saw, or that I remember she she was told many years and years ago, she was told she was brittle, which, again, I think, was them giving up on her to a certain extent. Yeah, would, when my dad was around, he would very much take, not ownership, but he helped her out immensely. I know that. I know he would. He would always be like, you know, oh, that's a fistful of a potato and this kind of thing, he would know, oh, that's one unit, that's two units, that's three years he would look at a plate, and he would do very much like you it wouldn't be how many grams of carbs, it would be, how many units of insulin is it, right? And he majority of the time when he was there, he would do it. He would do it for her and tell her how much to dose. I did have a handle on it, but many times so in when I was growing up, I would come home to and find her unconscious. As a child, it never, kind of, I don't think if it affected me and scarred me or that kind of thing. It just was like part of life, like, oh, mom's low again. I need, oh, she's had a Hypo.
Speaker 1 25:17
So we all grew up with it
Sarah 25:21
as part of life, not as a big normally, she would handle it, but sometimes I would have to call the ambulance when I got home from school. So that sounds terrible, but it didn't seem like a big, massive thing, but it was obviously, yeah,
Scott Benner 25:36
it just didn't ring out that way. So I mean, 56, eight, it's in the 80s. I'm trying to so you're when are you born? Give me the year you're born.
Sarah 25:45
7979
Scott Benner 25:48
so she's like
regular NPH, or maybe beef and pork insulin for a little while mixed in there. Yeah, yeah. She did have beef and pork, yeah, and then. So she's just shooting once a day, twice a day, as it goes on for that decade. And yeah, and probably just doing some food exchange, kind of an idea, or that kind of a thing, okay, yeah, and your dad knows more about it than she does. Was she an unstable lady? Did her personality jump around?
Sarah 26:18
I would say she did have bouts of depression, but never diagnosed and never treated. I think she would get herself real, really anxious about certain things, like she'd she'd have shingles a few times, and be super worried and super anxious about things, but we just kind of went through it and just carried on. Okay, I don't know if it was, it was like, like you said, was she altered because her sugar levels were high for such a long period of time? Yeah,
Scott Benner 26:47
was she? Was she angry? Short tempered, foggy, then goofy? You know what? I mean, like, did that bounce around like that? Or maybe not. Maybe those slower insulins didn't give you as much of us. Maybe the swing was more in the number not, I don't know. I'm guessing you know older people with diabetes. But okay, so, so you don't really see it a lot growing up. It's not even a thing you think about. Like, if I would have said to you prior to Poppy, if I would have said to you, hey, tell me five things about your mom. You don't you wouldn't say she had diabetes, right?
Sarah 27:18
Probably not. Yeah, well, probably not. I mean, she did move on with it in and in years to come. She did move on with obviously, faster acting. And she did get a libre so she was checking less, but the way, well, as soon as I was like in the know, not in the know, but as soon as I knew more, I felt like she was not getting decent care at all. I do think that they had, she was a lady, so she lived at 84 Yeah, I think and poppy got diagnosed a year before. So I think they had thought very over the past, however, so since my dad, probably the last five to eight years, they had thought, Do you know what? She's a lady in her 80s. She's not doing a good job, but just let her be. Let
Scott Benner 28:04
her Sarah, 84 if I make it to 84 I'm calling it a I'm calling it a good day. I'm believing. You know what I mean. Don't you think that?
Sarah 28:12
Yeah, yeah, I know, but I know her health was seriously damaged and seriously affected. Yeah, had it not been, well, God, she might have made it to 94
Scott Benner 28:23
Yeah. I mean, she had the if her body had the fortitude to get to 84 in bad shape, you're right, she might have gone farther. Yeah. I mean, it's very interesting, because obviously it's not you know what you would call modern care. She didn't experience any of that. Do you even know about her side effects? Do you know what she was living with, as far as troubles, yeah, what did she have going on?
Sarah 28:42
It didn't really all the side effects generally tend. She seemed to be absolutely fine. She was fit as a fiddle, we say. And she was always 10 years younger than what she actually was. She looked absolutely fantastic, amazing, really fit and healthy until my dad died. So at that point she would have been, hang on. So he was 82 she was six years younger, so she would be 76 Okay, so she had so 70 up until 76 maybe a year after she was she just looked so young. She looked in her 60s. Everyone commented, oh, your mom looks so young. She's got great skin, this, that and the other. She would walk miles and miles and miles. She wouldn't get the bus to somewhere. She would walk, even if it was a couple of miles, do everything in herself, all of that, all that she just was a young 76 Yeah. But then it started to all hit her. So she had neuropathy, definitely in her feet, that was for a while, so she would have to be really careful. She could step on a nail or anything and not even notice until she saw blood gushing out. No feeling in her feet. Her hands were really, really badly arthritic, but she was also she lost feeling in her fingers, and I think probably for best part of 4550 years of fingerprint. With kin,
Scott Benner 30:00
maybe neuropathy. Do just yeah,
Sarah 30:02
all the feelings just gone, yeah. But then she started having so her kidneys. She definitely had kidney problems again. I don't know the exact diagnosis they she wasn't on dialysis. She wasn't on dialysis, yeah, okay, no. They were saying she has got kidney failure, she has got kidney disease. She's got heart problems, heart disease, etc, etc, so she did have all of that. But then that same Christmas, when we accuse the kids of not listening, obviously they had ear infections, she was also diagnosed with Alzheimer's and vascular dementia at the same time, really. So that was, that was the slow decline. I think that was, that was the beginning of the end. Yeah,
Scott Benner 30:45
they also, they call Alzheimer's, uh, diabetes type something,
Sarah 30:49
yeah, I've heard that, yeah, yeah. Okay, so
Scott Benner 30:54
that's her. That's your understanding of her. Poppy's diagnosed. Do you at some point think, oh my gosh, my mom's life is my daughter's life now. Or do you see that it's different when they start teaching you about the management and think maybe this will be different
Sarah 31:11
for her? No, yeah, I didn't see it the same because I thought as soon as they started educating me, I just thought, or I started to educate myself. I thought, this is not the same. This doesn't have to be the same. She doesn't have to have all these problems, because we don't manage it even from day one, my mom in that first year that there's only one year where they were both a lot, well, my mum was alive and obviously, and then it covid Hit. So we couldn't meet up with her very often, but she would wake up. My sister would tell me she if mom wakes up in the morning and she's high, she just doesn't have breakfast, and she'll wait till for hours until she comes down. And I'm like, what? Why doesn't she just have a correction dose? What didn't make any sense to me. And then again, I'd meet her up. We met at the park so she could have a little walk round, and the kids could play on the swings, whatever. And I said, what's going on? Or how are you? Oh, I need to walk around for a few hours because I'm quite high. I'll just walk it off. I was like, Do you not want to take a correction dose, though? And she's like, No, I'll just walk you know, I won't have tea until I come down. It doesn't make any sense to me. Yeah. From Yeah, and I was only like, you know, a couple of months into it, I was thinking,
Scott Benner 32:25
that's not what you should be doing. Were you able to feel any like responsibility to your mom or guilt about her life? Or were you so overwhelmed with poppy that you kind of couldn't think about other
Sarah 32:38
people? I do feel that if I had somehow been more involved or known more that maybe I could have helped her, but I wasn't involved. I didn't know and my sister was her carer. And it turns out, my sister knew absolutely nothing about diabetes at all, and didn't take it upon herself to learn.
Scott Benner 32:56
I don't know how to figure that out, like it's I don't when a doctor or tells you this is how it works. I think most people just believe that. And why would they not? You know what I mean? Like, why would a doctor give you some of the information about your daily disease? You know what I mean? Like, it doesn't make sense. Like, why would you even wonder, did they tell me everything? Yeah, but I mean, I take your point. She's living, she's doing okay. And probably people told her, Oh, you have neuropathy in your feet because you've had diabetes for so long. We expect that. Yeah, you know,
Sarah 33:28
all of the, all of the things they're all said, it's because you've had diabetes for so long. This is why you've got X, Y and Z, yeah,
Scott Benner 33:34
oh yeah, absolutely. And nobody said X, Y and Z for a while on here. So that was good. Good job. Okay, how do you teach yourself about diabetes for Poppy, okay,
Sarah 33:46
so the first let's think the first six months, we were very much drip fed from the hospital, from the diabetes team that we have there. So you have a group of nurses, you have a consultant that you see. Maybe you see the consultant once every three months. But in the early diagnosis, you get weekly, they're doing obviously, it was all covid. So Poppy got diagnosed on the seventh of March, 2020, she was in hospital for three three days. We got sent home. We went into the hospital, had a meeting, they did all the education, all that kind of stuff. And then the 20th of March, everything shut down. So then, from then, they didn't see us again for six months, nine months, it was all remote. So it was phone calls and emails.
Scott Benner 34:31
Was that helpful at all? Like, did you feel yourself understanding getting better moving forward, or was it just the thing they were doing?
Sarah 34:38
No. So, because I had six months with poppy 24/7, I feel like I did get a handle on it, because I watched her every single day for six months like you with Arden when she was diagnosed, you just stare at her. Thought, what is happening inside? Said they were quite helpful. I do have to say, Yeah, they did give they were really checking in. So, like, the first month, they said something like, she can have no snacks in between meals, because we want to work out the ratios, which was really hard, so she could have carb free snacks. So okay, which is why she now hates cucumber, because for a month, she had to eat nothing but cucumber and cheese and whatever they said was low carbs, carb free snacks in between meals. But a five year old, she now doesn't like any of those things, but yeah, that's how they worked out carb ratios. But then I think within, I don't know how long they would do checks so, you know again, if her so they were, she was on lances and Nova rapid injections, if she was, like, going low in the evenings, or that, they would change all the how much collage in the background. They would do it, and they would check in, try this, and we'll give you a call in a week's time. They were doing what they said, they would check in with me. But at some point, I don't know when, but at some point I was like, You know what this is? I can't be listening to them anymore. I need to do this myself. I don't know when it was, but at some point I just thought they're only tweaking it by this little amount, and then it's see what happens for a few days. Well, why do I need them to okay it? I can do that. I can tweak it a little bit and see what happens in a few days. And then if it doesn't work,
Scott Benner 36:21
I'll put it back. Yeah? I mean, feels like common sense, right? Yeah, so
Sarah 36:26
very I'm gonna say maybe a year. I don't know if it was a year, but then she's had, like you said, you have to be your own advocate. We've had to fight for everything that she's ever got, as much as, I think people say everything's free here, as much as it's funded by the National Health Service, it's not just given to everyone on a plate. 100% not. And we've had to dig our heels in many times to get what we needed to get for Poppy, so
Scott Benner 36:57
Sarah, it's free if you can get it. Yeah, yeah, gotcha. Like, if you can get yourself to it, get your hands on it, get somebody to agree to hand it to you, then it doesn't cost anything. But it's not just like you don't wish out into the air and it just arrives. No,
Sarah 37:10
absolutely not. And it does seem to be like we refer to things as a post code lottery here. So depending on what area of the country you are, can very much dictate what you are offered, yeah, and whether you will get it or not. Just
Unknown Speaker 37:25
yeah,
Scott Benner 37:27
I was interviewing this girl the other day from America, she's a nursing student, and she said, Oh, she was talking about something that they teach in school. And she said, Well, it depends on, you know, what part of the country you're in. I'm like, why is nursing school depending on what part of the country you're in. Like, aren't there basic ideas that they all need to know, whether you live in Minnesota or Florida? You don't even mean, I was like, that doesn't make any sense to me. But then you're you say this, like, post cold, what you call it post code lottery. And if you talk to people in Canada, they'll tell you that their diabetes care vacillates wildly depending on the province you live in. Yeah, yeah. Where some places they'll put you on regular and mph in 2024 that's insane. Yeah? So, or you go to another province and they're like, no, here's a CGM and a pump and let's get going. It's really interesting. I've been, um, I'm gonna have to stop doing these cold wind episodes a little bit. I'm gonna need a break for myself, because I'm getting a little cynical listening to them. You know what I mean? I'm like, oh, say that, yeah. So everybody's just not trying. Got it great, except the ones who are up until they burn out and they stop too, like, yeah, all right, great, you know, I'm sorry. So you're making it. You're making it through this process. You're teaching yourself on your own, using the internet, using, I mean, you can't, you can't use your mom. You can't use your sister. Did you try? Did you call your sister and then you were like, oh, hell, she doesn't know anything. It's
Sarah 38:55
a very sore subject, to be fair. But she was trying to do the bare minimum that she could for to with my mom's care. She didn't want to get involved. She didn't want so my mom was with her arthritis were getting worse. She was fighting it harder and harder to do the injections herself. Yeah, my sister didn't
want to do it. And I said, What do you mean? She's like, well, I don't feel comfortable doing it. I
thought, I don't feel comfortable giving my five year old an injection, but you just do it. Hey,
Scott Benner 39:19
I've been married for 27 years. I haven't been comfortable. Once I you don't hear me complaining. I just get up every morning. I go, okay, and I go, yeah.
Sarah 39:29
So she was reluctant to take on any responsibility, she said, so they so she requested that a nurse would come in to give my mom a couple of injections a day. So they tried to put her on like NOVA mix. Do you know that? Do you have that in states, which is half long acting and half fast acting mixed into one? So she could have two shots a day? Okay, so they tried her on that so that then a nurse could come in twice a day to do it, because my sister was refusing to do it. But then that had her numbers just went all over the shot. But it was a total disaster. So there to go back to slow, slow acting and fast acting. And she was starting to come around to the idea of, I'm going to have to eventually do it, because mom can't do it herself. I was like, if it wasn't covid, I'd be around it. I'd be coming around and doing it myself. It's not but no, anyway, she
Scott Benner 40:16
Yeah, I hear you. I hear the frustration. I understand. I don't want to ask more questions, because it's your sister, but I but I get the I think I get what's happening. I'm trying to get you to something that you brought up before we started speaking, that you want to talk about. This all falls on you. Your Poppy scare. Is that right? Yeah, you're the one that takes care of it, and generally, generally speaking, your husband understands it. Or no, yeah,
Sarah 40:43
yeah. So obviously, the first six months, it was me. He was, obviously, he's a police officer, so he was front line. So he was still working 6070, hours a week during the whole of whole of it. So us, the three of us, were at home, so me and the two kids. So for that six months, I was very much doing all of it. He was involved. So when he was home, he would do the injections, but I would obviously be cooking the tea, I would be carb counting, I would be doing all of that kind of ratio stuff. And then when we started doing it ourselves, so not asking the hospitals for approval to make changes, it did fall to me now, I think because he always says, Oh, you're a maths guru. You're a maths person, da, da, da, and all that that he he won't understand it. He will understand it. He just hasn't, because I do it. Has
Scott Benner 41:31
he ever told you you're better at doing the dishes than I am? I would do them, but you're so good at it. So I'm gonna try that on. My wife. Is what I was, I was just wondering if that works or not. It's like, you know, vacuuming, you just, you have, there's a certain way you do it that I think really makes it better. You get in there. So, okay, so he, do you think that's him feeling like, Oh, God, I don't want to make a mistake. So I've asked
Sarah 42:01
him about this. So with all this, so when I started learning reading within a couple of months of diagnosis, she got the libre because I'd read that she needed something. Now they wouldn't give out dexcoms Because they only gave out dexcoms At that point to kids who were hyper unaware. Now she had did have some hyper awareness from the start, or people who had had really severe hyperglycemic episodes or something like that. So she didn't tick any of the boxes for Dexcom. So this is why they gave her the libre, which, again, is the NHS way of like the poor man's,
Scott Benner 42:37
whatever it's called. They were saying. Yeah, that's what
Sarah 42:41
they were saying back. Then it's a cheap version. We'll give the cheap version. So we had that. We did have that for let me think, let me think a two years until, in a weird way, thankfully, but also not thankfully, Poppy lost her hyper awareness. Now, I think in my mind, it was because she was roller coasting. She was having highs and lows because we couldn't rein in the the libre did not work for her. It was really bad. We went through this time where it was it had such a big lapse. If she was dropping, it would have a massive delay, so we'd have to put her low alarm at something crazy, like 100 so 5.7 it's 5.7 100
Scott Benner 43:21
you want me to look
Sarah 43:23
five, not fives 90, so definitely over 90. But yeah, her, her high alarm was like 5.7 because by the time it went off at 5.7 she was already below 75.7. Is 103
There we go. So yeah, so
if her low alarm went off at 5.7103 we would finger prick, and she would already be three point something. So in the in the 60s, so we it just wasn't working with her. She wouldn't feel it. We told the hospital this, thankfully, and they approved the Dexcom for her. And then, since we got the Dexcom, her hyper awareness has gradually come back, and I think it's because we're she's more stable now. She's got loads of stability since we found the podcast. What? As soon as she got the Dexcom, her a one, Steve said I had coming down, so it was like 6.86 point 6.6 6.5 6.3 as soon as we found the podcast, within three months, it's been in the fives, and it's been in the five for 18 months. Oh, that's wonderful. 5.3 5.4 5.5 it doesn't go above there.
Scott Benner 44:25
That's amazing. Good for you. It
Sarah 44:27
is amazing. Congratulations.
Scott Benner 44:28
Good for you. Thank
Sarah 44:30
you. Thank you so much. You're very
Scott Benner 44:31
welcome. It's but again, not I haven't said it to you. I shouldn't have said again, but I should have said that I try really hard in these moments to do two things. First thing is, is going to sound strange, but I like to separate myself from the podcast, because it's unhealthy for me to feel like I helped all these people. Do you know what I
Sarah 44:51
mean? But, but you are the creator of the information. That's fine.
Scott Benner 44:55
The podcast helped you. It makes me more comfortable if we talk about like that, okay. But the other thing is. I just said the stuff out loud, you did all of the hard work, all the staring, all of the experiencing, thinking about it, going back again. Like, I just sort of, like, I don't know, I just shoved you through a door, and I was like, if you keep walking in this direction, this is going to work out. And you you just, you did it, you know. So, yeah, I appreciate it very much. I'm not trying to be it's such a weird position for me to be in, I know and I and I appreciate it and thank you. I know I did this, but it's weird to say, it's weird to say out loud. It just feels I feel like a dick if I say I don't know, I just do all these years later, it feels weird to have somebody thank you for their health. You know what? I mean, you might not know it's a just an odd situation I'm in. I guess I'm never gonna know why I feel that way, like there's part of me that thinks because I didn't help my friend Mike, I don't want to feel like I helped other people. That's one of the things that bothers me a lot. And I think the other thing is that Arden is a work in progress, as she will be her whole life. I'm not superstitious, but I don't want to take credit for the thing until I know if it worked the whole time, because it would be strange if I was like, Oh yeah, I know what I'm doing. I'm so good at this, etc, however. And then, you know, Arden wakes up 10 years from now and has problems. You don't even mean like, I don't know like, it's just, I don't know how to explain this part. You can do the best that you possibly can, and it's about it's weird, because you could ask me almost any other question, and I'd go on for 15 minutes and talk my head off and be completely clear minded about it. But why can't you take a compliment about the podcast? I don't know. I can do it in writing, like I can do it online and like on Facebook. If somebody's like, Oh, my God, the podcast helped me so much. Blah, blah, I can say, Oh, I'm so happy for you. That's great. I appreciate my pleasure. Like, I'm easy, but when, when I can hear the person's voice, I curl up a little bit. I don't know why exactly. So anyway, I appreciate it. I'm so happy for you and for her, and I don't know why it makes me uncomfortable. Maybe if I make the podcast for 10 more years, I'll figure it. Maybe I should just ask Erica, oh, why don't we just do that? Yep, she'll go, I'm not your therapist, but it's okay. We can still talk about it, because I feel like an asshole right now. Like, like, I really do. Like, I just, I'm like, why couldn't I just say thank you and move on?
You know what I mean? So I don't know, Terry, you didn't want to
Sarah 47:34
fall a lot of a lot of people have that though. It's like, when someone pays you a compliment, loads lots of people that bat it away. It's like, you need to just accept it. Someone say, Oh, you look amazing today. And go, oh, this scruffy thing, this old thing I've just thrown off. It's like, no, just go, thank you.
Scott Benner 47:52
I accept your example. Except I'm not like that in any other aspect of my life. The the other day, I bumped into my doctor, who's like, literally bumped into her, and she's the one who helped me get on the GLP medication, which I've almost been on for exactly a year. I'm 45 pounds lighter today than I was a year ago. Wow. And she saw me, and she goes, Oh, my God, you look so much younger. And I was like, Yes, I do. And then I said it to anybody all day long, who would stand in front of me. There was six weeks where I referred to myself as skinny Scott, and I would say things like, skinny Scott likes fashion, so, so I have no trouble accepting a compliment. In my mind, I didn't do this like I took the GLP and I lost weight. So, yeah, I don't know there's something also
Sarah 48:40
made a conscious effort with thinking about what food was entering your body. I have
Scott Benner 48:45
been doing. I have absolutely been doing that, and I'll take credit for that. I can't take credit for the podcast. It makes me feel weird, and by the way, like I can step out of it and tell you, like, academically, I know what I did. I know I made a thing that's bigger than anything else has ever been, that's reached more people, that's helping more people, that's more accessible and digestible. I know it's academically. I understand the whole thing. I can talk about the podcast like it's not me. I can't talk about me like I'm the podcast. I'm gonna find out why. I'll go to therapy. All right, okay, let's get past this, because nobody gives a what happened to me when I was nine and why I can't take a goddamn compliment about a podcast. So people are like,
Sarah 49:29
Okay, let me tell let me tell you something, which I think adds to our challenges that we've had over the years.
Scott Benner 49:39
You did touch on it earlier. I'm ready. Oh, sorry, no, I thought, I thought you paused like you were waiting for me to say something. Oh, my God, tell
Sarah 49:48
me so I said that I have a visual impairment, right? So this, this actually threw a spanner in the works with Poppy's
Speaker 1 49:55
stuff. So after. Six months, they
Sarah 50:00
suggested to us that she would go on the waiting list again. It's not just handed out the waiting list to get a pump. So we were like, yeah, yeah. 100% put that. Put her down for that, no problem. And they said it would take a year or
Scott Benner 50:14
whatever. I don't know were they making it by him exactly?
Sarah 50:18
I don't know that. I don't know how they justify whatever this waiting list was, but it was going to be a long waiting game. Okay, so when they so we said yes to that. Meanwhile, Poppy was this, I don't know, really sensitive to injections. She was fine having them. We would do them. We weren't chasing her around the house too much. It was fine. She would give in to injections, however, many times, but she would bruise every single time that we did it. And we were like, Is it her? Is it us? Like, you know, they, they say, like, hold, like, keep the needle. Like, totally still hold it in for 10 seconds. We were doing that, and it's still a massive bruise. I'm like, is she moving? She's five. She does fidget a little bit. What is going on anyway, doesn't it didn't matter what we did. She was always bruised with every single injection, so she just looked like a little bruised
Scott Benner 51:08
pin cushion, like you're a flicker.
Sarah 51:11
So we heard about this thing called at the eye port, which I think you got someone else. A few people have mentioned, yeah, is it Medtronic? It's Medtronic.
Scott Benner 51:18
Medtronic makes the I port. I'll say this out loud for Medtronic, because they're sponsors. Now, again, I don't think it makes any money. I don't think there's any business behind but it's such a great thing. I wish they would talk about it more. You know, it
Sarah 51:31
really was good. So we looked at it. We requested it from a hospital. They said, No. They said, We will not pay for that because you're on the waiting list for a pump. So again, hang on, but she's still bruising from injections right now,
Scott Benner 51:44
yeah, but a year from now, she won't be when we get it there, yeah,
Sarah 51:48
so they said no, because you're on the waiting list for a pump, you we will not fund an eye port. Okay, fine. So we self funded it. We bought it ourselves, which is fine, and she was on that for however long, until she finally got a pump. It was a god send, because obviously she couldn't feel the injection. It was very similar to a candy like you change it every three days. She's having her injections just literally slotted in into the hole, which I managed to do with magnifiers and glasses and all this stuff. So I could do that anyway. So when we get to the pump situation, they have a choice. So again, our hospital had the choice of
Scott Benner 52:26
Medtronic or
Sarah 52:30
OmniPod. Yeah. So those were the two options. Now they we went to the little meeting. They had them all on the on the table. So she looks at these Poppy looks at these small little cannulas, and then she looks at the to her chunky omnipot, and she goes, I want those. I want those. And I said, right, yeah, hang on. But what you've got to understand is that tiny cannula is attached to a tube, which is then attached to this massive, massive pump. And she was like, Yeah, that's what I want. Like, okay, I had thought she'd go with tubeless. Okay, fine. We'll see. So you get the trial. So they do a saline trial with it. So we took it home. She was like, she was liking it. She was like, Yeah, we like we like this. I want to do this good. Okay, fine. Got it all authorized, got it all funded, etc, etc, bring it home.
Scott Benner 53:20
I can't see to fill it
Sarah 53:23
doesn't doesn't matter what I do. I cannot get the insulin out of the vial. Yes, I can't get, I don't remember how I how it was. So you had to fill the little reservoir. Then you had to prime the tubing, get all the bubbles through the tubing, get the bubbles out of that, whatever it was, I was not able to do it. Couldn't do it. So we then had to get into discussions with them. Could my husband spill it on a day when we weren't using it like before he got to work or did and they were just like, No. They pulled it. They're like, you're not having it. There's no way around it. You're not having it. She'll have to wait another year for a pump.
Scott Benner 53:59
They couldn't just give you a different pump.
Sarah 54:03
So this is, this is what they said. They said, if it's not that one a hand, they didn't even, they didn't even talk to us about the OmniPod. They just said, If you can't see to fill that one, you're not going to be able to see to fill anything else. It's done. Her pump journey is put on hold until she's old enough to do it herself. And I was mortified. I was like, no, no, no, I'm affecting her health. This is, this is all my fault. This is going to be her waiting until, what? Until she's 1011, 12. I couldn't envisage when she was going to be able to do this all herself. But thankfully, we then got a follow up phone call from them, and they said, actually, there's this other pump that we don't, don't actually prescribe here, but we do have a couple of people on it, and it's called the
Scott Benner 54:47
architect, insight, okay,
Sarah 54:51
pump, and it has pre filled cartridges. There you go. So you literally just pop the cartridges in and. And fill the tubing and it's and it's done. Would you like to see that one? Obviously, I was like, Yes, please. She still had to wait another six or eight months. Brett, seriously,
Scott Benner 55:09
what are they doing? Are they bringing them in? Like,
Sarah 55:11
I don't know this, this time delay. I literally, have you
Scott Benner 55:18
guys heard of Have you heard of, like, overnight mail, just
Sarah 55:24
they they would have given us that we had the Medtronic, Medtronic in our house in the January, but when we had the fafn, had to give it back. We didn't get the other one until the September.
Scott Benner 55:35
Why did you tell them the truth when they told you they were going to take it back? Why didn't you say, Oh, don't worry. You know what? My husband's gonna do it. Because
Sarah 55:42
there was no physical way for me to do it when he wasn't here. Yeah,
Scott Benner 55:46
I know. But like, why didn't you just lie to keep the pump and then, I don't know, pay a neighbor to do it, or a homeless person or something like that? I don't know. Yeah, we just didn't think. We just, it was just, yeah, horrible. It was,
Sarah 55:58
it was horrible. UK, there's
Scott Benner 55:59
heroin users everywhere. Can you just walk out on the street and go, Hey, I'll give you and go, Hey, I'll give you $1 if you put this needle, they'll be great with a needle, like, they'll be able to, you know what? I mean, yeah, I don't know anything about England. Are there heroin
Sarah 56:11
users? No. I mean, I mean, my husband comes across them a lot, but that's his job.
Scott Benner 56:16
I'm saying he could have found one that would have been able to do this for you. Like, yeah, I just felt like in a world where you fought so hard, you gave up really easy, it felt like, is it because you felt bad about it being your fault?
Sarah 56:27
It's because there was no other option. In my mind. There wasn't anything else. If I if they're saying you cannot do this, there is physically, is no way you can do this. I was like, there is no way I've screwed it up for her. I'm wondering
Scott Benner 56:40
I could be wrong. I'm wondering if it didn't take out your resolve because you felt like it was your fault because of the visual impairment, like, did it like, sap your resolve? You know what I mean? Yeah,
Sarah 56:51
because I would fight about everything else. Yeah, that was my point. I just Yeah, I think it did. I think it did. Isn't it interesting?
Scott Benner 56:59
I can figure you out, but not me, yeah? Like, yeah. I don't know why. I can't take a compliment, but I'm like, Hey, I wonder if this is what happened with you. Okay, so what do you end up with? It works, good, yeah. So
Sarah 57:11
we went with the extra it was, it was a godsend. It was fantastic. And I was doing all the tools of, like, you know, temporary basal and extended bolus and all of that. We use all of the tools, even though, again, they were like, Well, you probably won't use these. Yeah, I use them. I used everything. If that pump can do something, I'm going to use it, right? So I went all in with that. And she used that for about a year, until, no 18 months. But after a year, we find started finding this problem with you would call tunneling, yeah, every like two days, we wouldn't get past two days. On the third day, guaranteed, something is going what wrong? Why are her numbers going up? This is not working. So we started the hospital. Just thought it was a bizarre thing. Like, surely this is not the only we're not the only family for this to happen to they were like, Oh, well, we can try a different length. I'll try different length cannulas. That was it. So from six millimeter to eight millimeter, I think it was, they changed that, and then it was still happening. After a few months, we were like, it's still happening. We just have to change our pump site on day two, otherwise we have problems. Oh, well, yeah, they didn't know what, what was going on. We'll try with us these different cannulas. We can try the true steel cannula, or 45 a different angled cannula, all of this. And I was like, Do you know what? This doesn't make sense anyway. So they were trying to push us to do all of these different things, different cannulas or different lengths, and change all of this. But then Poppy started saying, Do you know what this pump is really annoying me. I was like, What do you mean? Before she'd carry it in, like, a little kind of like her belt thing around her. Never had any problems. She would wear it during PE at school, do trampoline, but never had a problem. But she just started saying, it's getting in the way. It's always banging on me. It's always there. It's big. I can't sleep in certain positions the tubes there, you've had it for a year and a half, and you've never said this before. And she was like, well, it's bothering me now. So I thought, right, you know what? This is the ideal opportunity for us to kick off and say to the hospital, we're not happy with this. So the first bite, obviously, I said, right. You know what, all these cannula problems we're having, she started to say this pump is irritating her. It's getting in the way, it's cumbersome, it's inflicting she says it's affecting her happiness, because it's affecting her life, the way she can live her life. First thing they said was, well, you're in a four year contract. So she's still got to have it for another two and a half years. By
Scott Benner 59:35
the way, isn't it free? Who are you in a contract with
Unknown Speaker 59:38
the pump company? Apparently,
Sarah 59:40
they're in a contract with them. I don't know who's in the contract with who good. So that was the first pushback I didn't have that. I was like, Well, if she's not happy with it and it's still it's affecting her quality of life and her happiness, then we need to find a solution, don't we? Plus the cannulas are not working, whatever it is. How? However you want to look at it, we have a problem. So they went away with that. Thankfully, they came back and said, well, actually, there's been some issues with that pump and that they are recalling some of them. So really, we would want to actually encourage you to get off that pump sooner. So yes, we will authorize you to come out of that contract early.
Scott Benner 1:00:21
Nobody knows what they're talking about. Sarah, no one ever knows. Forget health care for a second. It's all let me. Let me tell you something I told my son the other day, the world is being held together by bailing wire, duct tape, bubble gum and a little bit of luck. Okay, so, like, there's just no one knows what they're doing. They just say something that they heard someone else say or that they think they're supposed to say. No one has an original thought. They don't take the reins. I mean, some people do, don't, get me wrong, but, but a lot of people don't, and then you end up in these situations where they say things to you, like, you can't,
Unknown Speaker 1:00:58
uh, you can. You know, have
Scott Benner 1:01:01
you tried this? Try that. Try this. We don't know. Like, no one knows anything. They don't understand what to do next. Is very frustrating. I just you know, especially when it comes to health like this. So what'd you do? Did you just, like, Did you you go crazy? Did she get Did you finally try to drive and just drive the car right through the right through the building, exactly? Stop being exactly. Give me what I need. Oh, my God, no. So how does this how does this all work out? Like, how do you end up? Because I'm assuming you end up with omnipot,
Sarah 1:01:30
yeah. So thankfully, I had started listening. So this was all I'd started listening to you in the October of 2022, and this is all happening February. February was when she started having all the issues. So in my mind, I'm already an OmniPod person, but obviously that's not my decision to make, and within reason. So she's What is she? Then, seven?
Scott Benner 1:01:58
No, yep, seven. So she's seven
Sarah 1:02:01
and a bit. So by the when she starts saying, all this or this pump is not getting on, I'm not getting on with this pump, it's music to my ears, because I'm like, I already want you to have OmniPod, but the hospital was trying to push T slim. Clearly, they were all in the new whatever, the new control IQ, and that they were loving it. They'd approached us. They'd approached us and said, like, we're we're loving this. This is the new way forward. Once you finish with Rosh, we want you to go on this. And then we had all these problems. And they said, right, we want you on this control IQ, it's all singing, it's all dancing. And I said, Okay, we're gonna have the same issues with me filling this. And they were like, Oh, well, no, it should be fine. I actually posted in the juicebox group stay in any visual impairment that we're looking at. Tea slim, yeah, tea slim and omnipot, what? And loads of people helped with both. There were like filling tools and filling aids and all this for the tea slim. But lots of people said just the omnipot is just, you don't even need to be able to see to do it. So we did get the demo using your link. Thank you. Of course, OmniPod, com, forward slash juice box. Went and got the demo. We went and got the demo pod.
Speaker 1 1:03:08
She loved it. She was like,
Sarah 1:03:11
I can't even feel it's on. I think we put one on her. They send you two. I'm sure they sent us two, yeah. So she could trial it for like, six days, rather than just three, she had one on her tummy, on her butt, and either way, she was like, I could sleep on it. It's not in the way. It's amazing. So we went straight back to our hospital team. We're like, yes, she wants this. We want it, sort it. So that was February or March. And so again, they dragged their feet, and she finally got approved for it, and we got it, they still made us do a saline trial, even though she was already on a pump, a functioning tubed pump. What is the actual point? But anyway, so that's them. That's what they do. That's
Scott Benner 1:03:55
the point. The point is, that's what they do. There's no thinking. We
Sarah 1:03:59
don't need to do that, yeah, because she's already worn at one No, no, she had to do a second time. Anyway, June, she got that. June 2023, and then she got moved over to the OmniPod five in the August. So she literally only had a dash pod for like, two months. And then we went on OmniPod five. And again, it's not affected her, A, 1c, at all. It was in the low fives. It's still in the low fives. They said, Oh, well, you might not get as good results with the OmniPod five as what you were doing. I was like, Well, no, not if I leave it to do what it wants to
Scott Benner 1:04:35
do, but I don't, and you've been having good success with it, yeah. Well, with it, I help? Yeah, I saw somebody the other day. They're like, Oh, this isn't keeping my blood sugar where I want. I'm like, Are you bolusing? Like, we just think it was going to be magic, you know, like, it's, it's, and not just OmniPod five, by the way, all those algorithms, right? Yeah, do it yourself. Tandem OmniPod, they all, they need you to intervene. So. Times there's, there's variables about the food that you can't translate to the pump just by saying a carb count sometimes, you know. So that's really so one
Sarah 1:05:09
thing, one thing I have to sing the praises of, for the OmniPod five really about was, again, something you helped us with. So she does on a Monday night. She does Taekwondo, which is 90 minutes martial arts. And there's an adrenaline rush in there, and we didn't know what it was. She only started it about a year and a half ago, and the first few times she went, I was like, What is this? What is happening? What is going on? She walks through the door and she skyrockets. She hasn't had her tea for two hours. We did the right but I didn't understand what what it was. And then I then I worked out it was adrenaline, but I didn't know how to deal with it, until you said bonus for a juice box. Because if, if she doesn't have the adrenaline, you can just give her the juice box. And that was like
Speaker 1 1:05:53
light bulb moment. That
Sarah 1:05:56
is what we did. We actually had to bonus for two juice boxes. That's how much adrenaline she had. Wow. But we would do it.
Scott Benner 1:06:02
Sometimes you have to catch it, and sometimes you don't, right, yeah, yeah, yeah.
Sarah 1:06:06
But since so when she changed, so we did that for about nine months, it was working. She we just have to bowl us with two juice boxes the minute she walks in, leave them on the side, because they don't stay either. It's a drop off. It's not sit and watch them. It's, I'm going. So the teachers know she's I text her. We tell all about texting diabetes if she needs to do something, I've text her for that hour and a half. But yeah, so we did that for about nine months. Then she got the OmniPod five. So September, her first lesson, I was like, What do I do? What do I do? I don't know. Should I still put in that, put in that two juice boxes, or should I not? And I was like, I'm really gonna have to sit on my hands. This is so hard not to. I don't want to just watch it, because I don't want her rocketing up to 250 when I know she doesn't need to. But I thought, Okay, I did sit on my hands, and nothing happened. She She didn't go above 140 interesting. But the whole and I was like, That can't be right, how, how, how. So I stayed there for the first week, and then after that, I just dropped her off and touch wood. Apart from this one week, it has handled it every single time. Wow. And she does drop at the end, though. So the last 510 minutes, she starts to plummet. Little bit of juice. I just Yeah, little bit, or she's got glucose tabs. So it sorts out adrenaline, but it can't, it can't sort out growth hormone. There's no chance in hell that it can sort out
Scott Benner 1:07:31
that's a lot of impact. The adrenaline also spikes and kind of it goes away very quickly too. When the adrenaline is gone, the lift from the adrenaline is gone, which is why you're seeing a low afterwards, because they can't it. Can't know. It's expecting that high to come back the way on the curve that it expects, and then it the generally goes away, and you drop really quickly. It's hard, hard to deal with, but it sounds like you're doing a really good job with it.
Sarah 1:07:55
Yeah, most of the time again, now this, we've mastered it. I think most of the time. Sometimes I'm like, why is it doing that? But, and, no, I do know better than you most of the time, Mr. Algorithm, but yeah, it's definitely a godsend. I wouldn't go back to the sleepless nights 100% not. It's definitely, it's definitely, yeah, you can use it to your advantage, and you can work with it and not fight against it, excellent. It's not magic. I would, I would love it to have overrides, like you talk about with Luke, with the, you know, plus 130 you know, plus 30% for and all of that. I would love it to have that. And I hope that's something that will come in the future. It and it lower targets. I do think it does have to have that moving forward.
Unknown Speaker 1:08:39
Yeah, yeah.
Scott Benner 1:08:40
I mean, I mean, I hope, I hope they continue to refine it. I hope they all continue to refine all these algorithms. Honestly, they're going to have to, because one of them is going to do it, and they're all going to think, oh, we can't, we can't, not make ours better. They're going to have to keep trying. You know, I think it comes slowly, obviously, but you're used to slow, because it takes you a year to get everything. So it doesn't really matter we didn't really talk about the one thing that you asked to talk about and keep getting distracted. No, don't be you're doing great. Do you want to I'm a little low on time, like, do you want to go over it, or do you want to let it go?
Sarah 1:09:14
Yeah, there were, there were two things I wanted to incorporate, which I don't think we're going to have time to do both of them. But one thing that I think is not talked about as much as it needs to be, and I'm sure lots and lots of people feel this, is the fact of burnout, or the fact that in most situations, one of you has to take up more of the slack of diabetes than the other. So I do hear lots of people say, Oh, we've got a 5050 split. And I do half, and I and the other does half. And I think really, is that possible? If you're you know is, are you both working part time, or, if someone's working full time, and the other one isn't, how the hell do you get a 5050 split? I don't know many families. Who have a 5050, split in parenting? I'm not, you know, one parent will majority, do the majority of something. Okay, so I'm not set. So, for example, you know, the mom, for example, the mum. The mum might sort out all the school uniforms, and she knows what shoes she needs to buy them, and she knows that they you know, or she'll do all the meal plans, or she'll do the school lunches or whatever. Or again, if it's stay at home, dad, he'll be doing all of those kinds of things. He knows what uniform needs to be bought, booking school clubs, booking activity. I can't envisage that. It literally is a line down the middle 5050 with every parenting situation. And why it would be diabetes, I don't know. Yes, I was at home with poppy for six months. So obviously, I got a handle on it more than Chris, because he was at work 24/7 Yeah, when I started learning so reading the books, looking on the internet, found the juicebox. Listen to all the podcasts. And, I mean, listen to them, as in, I beasted myself with them, and listen to all of them in less than a year and a half. Wow. So I was listening to five six hours a day. I'm actually up to speed now. I got up to, I'm all caught up the other way, like last week. I was like, I have to finish all of these by the seventh of March, when we're recording. And I did, but now I'm like, don't have Scott in my ears five hours a day. What's going on?
Scott Benner 1:11:19
Is it strange for you to be talking to me? Yeah,
Unknown Speaker 1:11:23
because I'm
Sarah 1:11:24
only, I'm only listening to hearing you, like, for an hour, one hour a day now. And I'm like, It's really weird, but you're not
Scott Benner 1:11:31
there. I'm gonna go tell my wife that there's a person in England that is upset that she can only hear me for an hour a day. And then I'll, I'll time how long she laughs for, and then I'll get back to you and tell you, Okay, she'll be like, You know what she'll say? You should tell her to move here and live with you. That's exactly what she'll say. I'm amazing. I'm genuinely touched that you've listened to the entire podcast. That's really something, and it's, honestly, it's helping you, right? What's Poppy's a 1c last one, 5.3 Yeah, good for you. That's wonderful. Congratulations. That I feel good about, isn't that interesting that I'm like, Oh, that's nice. I can feel nice about that. Okay, yeah, all right, so you're saying that it's not a 5050, split in your house. But what did you tell me do? How much of what you told me before we started recording? Do you want to say here? This is how I feel. I feel like it's assumed that I've got it like, for example, this gets home from work. I'm doing
Sarah 1:12:30
the tea, so I'm cooking the tea. So obviously I'm carp accounting, doing that. But if I need to go out of the house for any reason, it still does fall to me. So many, times I've gone out. I need to so I work from home, but I need to go. I need to go out. I've gone to the shop so and, and it's I'm getting the phone call, or I'm getting the text, or what do I do in this? And I'm like, you do know what to do in this situation, because you've done it before, but you feel like you need to check with me. How many cards is this okay? Well, if I was at home, I'd be reading the packet. So can you not read the packet? Why do you need to ring me to ask me what that is when you can find that information yourself.
Scott Benner 1:13:06
So there's one of two. There's one of two thoughts here, like, is he just nervous to make a mistake and hurt her, or are you lording over him and you don't realize that he doesn't want to make you upset? So
Sarah 1:13:19
that's what. Yeah. So I've asked him about this. I have said, and I told, I told him before today I did say I am going to be speaking to Scott about how I feel the burnout,
Scott Benner 1:13:27
and you seem to be enjoying yourself. Yeah, okay,
Sarah 1:13:31
you don't do as much as I he said. And he said, No, I fully get it. So it's majority on you. And you know, I work full time, and I haven't got the time, I haven't got the time to look at it as much as you look at it. So therefore I know I'm not on the same page as you. I'm not up to speed as much as things with things as much as you are. Okay, my opinion is, if you listen to all the pro tips episodes, you would be up to speed. But he has listened to maybe three of them, and I did, did harp on about it, and he has made the effort to start, however, yes, yeah, I do appreciate he's got a 70 hour a week job. He can't. He's got a 45 minute drive to and from work, which I said, Well, that's two podcasts a day, yeah, but he doesn't, well,
Scott Benner 1:14:12
I agree with that, by the way. Also, is he not in a police car all day? No, oh, he's on on foot,
Sarah 1:14:20
he's in, no, he's in the station interviewing. Oh, okay. Oh, okay. I
Scott Benner 1:14:24
see. So you can't listen to a podcast while he's working,
Sarah 1:14:27
right? It's just the drive to and from work. But he says he doesn't get signal. I said you don't need signal. You can download it onto your phone, and then you can listen to it without internet. But he hasn't managed to, hasn't managed to master that. He hasn't
Scott Benner 1:14:39
figured out the internet yet? No. So do you think he doesn't want to and you're upset by that, or do you he says
Sarah 1:14:47
he does want to. I think he does want to. He says, he says he does think that he's going to get it wrong. He said, if she's with me for a day, I know it won't, her numbers won't be as good as when she's with you. I'm like, Yeah, but why not?
Scott Benner 1:14:59
What feels pressure by it Don't,
Sarah 1:15:03
don't feel pressured, and don't feel like I'm gonna berate you or criticize everything I want you to try. All right, so
Scott Benner 1:15:10
Sarah, two things. I've been married for 27 years, so let me give you my thought here, if I told my wife, don't feel pressured when she felt pressured, she'd leave me. And if that's for sure, she'd be like, Oh, is that your advice, idiot? And that would be the end of it. And so, like, I get your point. Like, just try. You'll be okay. You know that you have that comfort, right? Just listen to the like, the bowl beginning series. Like, he could certainly, like, commit to that, and then once he gets through that, give him the pro tips, and then he'll be okay, then he'll feel more confident, and he'll try the things that you're talking about. Like, he doesn't have to make me, he doesn't have to listen to the whole goddamn podcast. He could listen to some of the series. They would probably help him. Yeah. I mean, I think you listening to the podcast literally straight through. Listen. I haven't said this in a while, because there's like 1150 episodes now, but I absolutely believe if you go back to the first one and listen to this podcast, you're gonna have an A, 1c, in the mid fives. I really do think you will. And it's not because the secrets, the secrets are dripped through, but it's the way you pick up the information by listening long term and becoming immersed in it for a while. And you don't have to do it forever. You know what I mean? Like, I mean, it took you a year or so, that's what by the way, I really appreciate that. But, like, you know, I know what a commitment it is, but look how it paid you back. I mean, really, what are we talking about? You listen to a podcast for a year and a half and now your kids, a 1c is 5.3 on an algorithm that some people will tell you can't get a 5.3 a 1c that easily, you know? So you understand what you're doing. You literally became me in a year and a half as far as diabetes goes. So what it's amazing you do. So that's it. Tell him to listen to the series. Also tell him you won't have sex with him if he doesn't do it. Doesn't do it. That's pretty much the fastest way to get this done. Seriously, I don't know why. Again, I've said this before. I'll say it again. If I was a girl, I'd have everything I wanted. So I don't know. I don't understand when you guys are like, I can't get him to do it. I'm like, Sure you can. You could make me like, I would hit a homeless guy with my car if I was told to for sex. I mean, I wouldn't kill I wouldn't kill them. No, I wouldn't kill them. But, I mean, I'd like, you know, I don't come a little, like, if I knew they were going to be okay, you know what I'm saying? Like, there's not a lot anyway, use your power, okay? And then, by the way, don't pay at the end. The end go. I shouldn't have had to have done this, although your mom would have, she was a player. A player. So has your mom not been gone long enough for us to joke about her? I apologize. Oh, then that's fine. Yeah, all right. Is there anything we haven't said that we should have and do you want to hear the three titles I have written down my possible tidro Show episode. I
Sarah 1:18:02
have one, one thing that I will try and condense as much as possible for you. Go ahead, Poppy started to get anxiety, which I think again, is a thing that we would never want our children to have. But when she was diagnosed, she used to have school dinners, and we were very much like nothing's going to change. Diabetes doesn't change. Make your life change all this. So we wanted her to stick with the school dinners, not have to say, No, you must have had lunches now, because diabetes doesn't make you have to change anything. So we were adamant that she stuck with it. But it was really hard. So the teachers had to learn how to look at what she was going to eat on her school dinner. Carb count. All of this. It was a work in progress, and they did as the best they could. Okay. However, after a while, it materialized that she told me, and I mortified me, she'd always been really good at, you know, they would put her insulin in to put her to the end of the queue, so she had a bit of a pre bolus time, and then she would eat her food. Now she told me that she was forcing her food down because she knew she had to, because of her insulin, and that it made me feel so sad. It's gonna
Scott Benner 1:19:14
make me cry. I don't know why, damn it,
Sarah 1:19:16
I felt so guilty because I just thought I was like because I said, you've always been a really good eater. Because she that was it. She got ill. She had a little tummy infection, and it was making her have a an upset, sore tummy, so she didn't want to eat at school. And so they'd rung me and said she only wants to eat half of her lunch. We've already dosed for it. And I was like, right, okay, that's fine. Just can you get her to have a juice? Yeah. So it was not, it was not a problem, but the same thing happened the next day, and then she was crying, and she was like screaming, like, I can't eat this. My tummy hurts all of this. It's like, okay, don't worry. It's fine. And when she came home, she said, You forced me to eat I didn't. I just said, could you possibly try to eat this and have a juice if you can't? I said, what? I. Don't know why this is happening, Pops, because you've always been really good with your food. It's just she told me. I said, I've forced myself to eat food at school. And I was like, What do you mean? She's She said, I know that if I have insulin, I have to eat it. So even if I'm full up, and even if I don't want to eat it, I will make myself eat it. And I thought, I can't I can't believe this has been happening, and I had no clue. So eventually then, so we said, we said, spoke to the teachers. We found out she did have a urine infection, which had caused her to have a stomach ache. So I said, right when you take her down to lunch, if she only wants to eat half a portion, just dose for half a portion, let her decide before you tell her she's got to eat all of it, right? Well, it seemed to be like all the staff in the in the cafeteria were like, eagles. They were watching her. And they were like, flocking around her and going, you have to eat that Poppy. You must eat that like, really putting pressure on her. Oh, my God. And this was making her really, really, super anxious. Someone is we'd always said to her, Carrots. Carrots are carb free. Now, I know they do have a tiny amount of carbs, but the amount of portion that they give them at school, like a teeny, tiny bit of carrot, we just in, in her mind, Carrots are carb free, right? So this dinner lady had come over and gone, do you need to eat your carrots? And she was like, where? But they're carb free. She like, you need to eat those or you're not going out to play, and it just sent her over the edge. So is that with that? Was that? Was it we we said people need to stop talking to her about her lunch. And the same thing, they said, no, okay, no, but I want to talk to her about her lunch. And then the next day, someone said, she said, um, I only want half that portion of peaches. And the lady had said to her, my three year old would eat more than that. You need to eat more than that. Oh, Jesus. So it was, it was
Scott Benner 1:21:44
just all this more people who don't know what they're doing. It's, I told you, it's everywhere. Also that really made me upset. I don't know, but it really hit me hard when you said that. Jesus, yeah. So
Sarah 1:21:53
I just thought, right, you know what? We drew a line. We just said, Right? Geralt pulled it. No more. School dinners, packed lunches, straight to Pat lunches. And she now it's fine. The problem is totally gone. She makes her own pack lunch every evening, so she chooses exactly how much is going to go in her lunch, and she knows she's going to eat it. Yeah. And then we told school, so I had to speak to the headmistress. I said, I don't want anyone talking to her about what she's eating. They all need to back off. So she's allowed to use her phone during lunch now. So now during lunch is they they put her insulin in. At lunch, they set a 15 minute timer. She goes out to the playground, she goes in and eats. She texts me, saying, all done, or if there was a problem, she'd say, I couldn't eat my blah. And then I would say, right, okay, that's half a juice, or that's a go and have that instead. So no one is in the picture, other than her and me. We text, that's good. She does her own. No one else is involved, and it's alleviated so much of it, yeah, it's all gone now. No, I'm happy she I was like, this was a slippery slope into problems.
Scott Benner 1:22:55
Oh, an eating disorder, for sure. Yeah, yeah, on its way, because all these other
Sarah 1:22:59
people were telling her what she had to do, looking at her cross, examining her, forcing her, and I was like, I can't this cannot happen.
Scott Benner 1:23:06
Yeah, oh, I'm glad you figured that. I'm glad she spoke up. I'm glad you figured that out. I'm glad you shared it. Yeah, no, thank you. Okay, all right, all right, I'm a little long, but here are my four choices. You're gonna help me pick. As you know, the crack is on my list. Things you don't know are on my list, cooking, the tea, spanner wrench. All singing, all dancing. I'm leaning towards spanner
Sarah 1:23:35
wrench, wow, because you spanner wrench, because you
Scott Benner 1:23:39
use the word Spanner, and it threw a spanner into it. Here you would have said, in America, you would have said, you throw a wrench into it. I know that a spanner wrench is a spanner wrench because I was a fireman, and that's the wrench name to open the hydrants. The only reason I know the word Spanner. So what are we going to call this episode? Cooking the tea is probably obvious though. Maybe we want that one. What do you think? Oh,
Unknown Speaker 1:24:07
well, we
Sarah 1:24:09
didn't get to the ones that I thought that you were going to choose, because we haven't go ahead. I didn't incorporate into with Poppy's anxiety. So what she does every night now so that she's not worried about the next day, because she she, she always says, Oh yeah, that was it. She sometimes if she can't sleep at night, and it's not to do with blood sugar levels, but sometimes she's had occasional evenings where she can't sleep and she's just floating and turning for a while. So she has this ritual she does every night. So she says, I need energy for tomorrow, don't I? She always asks me this at bedtime, Mommy, I need energy for tomorrow, don't I? And then I will be able to eat tomorrow's lunch, and everything will be a fantastic day. And I want to relive the day, because it will be so good. So energy for tomorrow was, was my energy? I didn't
Scott Benner 1:24:54
even get to it, yeah, but you didn't say it. That's okay. We'll say, I like you. I It's on my. The list, we'll see what happens, Sarah. Thank you very much. You were really fantastic. This was wonderful. I appreciate you taking the time. What time is it? Where you are right now?
Sarah 1:25:08
It's now just gone, half past three.
Scott Benner 1:25:11
Okay, all right, well, it's only 10.
Sarah 1:25:12
I'll ask you one question at the end.
Scott Benner 1:25:14
I don't see why not go
Sarah 1:25:17
ahead. One thing we're really struggling with, and I haven't mastered this, is if her blood sugar is on the low side before a meal. So say she's ticking over at like 75 4.2 ish, nice and flat. But if you give the normal pre rollers time, so we give 1520 minutes, if we give 1520 minutes, she's going to go down and hit
60 or something. Do you instead of
doing because what? Obviously, if we shorten the pre bonus time, she'll rock it out. So do you shorten the pre bonus time and then add on extra so a super bonus? What would I do there? We can't, I can't seem to work it out. Because if she's 4.2 I know she's gonna drop massively if we give a 20 minute bolus,
Scott Benner 1:26:04
why don't you just cut? Have you tried, first of all, have you tried just cutting, just a few minutes off of
Unknown Speaker 1:26:08
it? She still seems to go quite
Scott Benner 1:26:12
down to 60. And is she dizzy
Speaker 1 1:26:13
at 60? No, she would not fit.
Scott Benner 1:26:17
And how long does she stay there? Only a minute or two until the food hits her right? Yeah,
Sarah 1:26:23
maybe two rotations of the Dexcom. So
Scott Benner 1:26:25
then, if I take the number 60 out of this equation, are you comfortable with her bolus? Yeah, it's the number you're uncomfortable with.
Sarah 1:26:33
It's the number, because the hospital nagged me at about numbers, and I'm so paranoid about not having any threes. They hate the threes. They hate the 60s. So
Scott Benner 1:26:43
all I can tell you is this, when I see Arden bolus sing, and she goes to like, 65 like, in that range for a couple of minutes after a big bolus, and then I watch it come back up again, I think, Oh, this is going to be a great bolus. She's not going to get high after this. Yeah, that's how I think about now, if you're getting lower than that, if she was dizzy, I would, if any of that was happening to Arden, I would, I would change my tune about that. And if you're telling me that making it a little shorter results in a spike, then again, I would do that. Now, if it really bothers you, she could bolus. Have a bite or two of something and wait 20 minutes, and that might be enough to balance it out. But, I mean, that seems a little cruel to let her start eating and then tell her to stop again. Yeah, I would say that if she's not getting lower than 60. Have you ever checked it with a finger stick to make sure? Yeah, and she's about 60
Sarah 1:27:41
and about that, yeah, it doesn't generally go below that, yeah.
Scott Benner 1:27:45
So this is not advice, and I'm not a doctor, but I wouldn't change anything
Unknown Speaker 1:27:48
about that. Probably.
Scott Benner 1:27:50
Yeah, okay. But I mean, otherwise, you're gonna have to the, I mean, the other thing you could easily do, it, mean, it's a pump, right? So if it's, if it's a, let's just make up a number. If it's a four unit pre bolus, you could put, you could put three units in, and then wait 20 minutes, and then bolus the fourth unit and then eat. Okay, that would probably work, because then you you weaken the pre bolus a little but not enough to it would still stop the spike, and then the secondary bolus would only be a few minutes behind it. That might be the best idea if you're trying to avoid the number, okay, split the bolus a little bit. That makes sense. Yes, yes, I'm not a doctor. Thank you. Thank you very much. Did you enjoy this? Yes, oh, good. I'm glad absolutely all right. Hold on one second for me. Okay, okay, Sarah, we're recording again real quickly. I meant to say something to you when you said about Poppy being anxious. Have you checked her thyroid levels? Hang on. Let
Sarah 1:29:01
me think, yeah, her last one was 2.2
Scott Benner 1:29:03
okay. TSH, 2.2 Yeah. Has it been rising?
Sarah 1:29:11
I don't know what the one more before that was. So that was, what month are we in? Now, that was October. They only do it once a year. Yeah, I haven't got the one from a year ago. See if
Scott Benner 1:29:21
you can get them to sneak in another one, because if her TSH is going up, if she's having thyroid issues, anxiety could be a part of that. Okay. And if she's having trouble sleeping or feeling does she feel rested after she sleeps? She feel tired? No,
Sarah 1:29:36
she says she's okay. She just occasionally has had it. We attribute it. We attributed it to once she had a fizzy drink, and we think she's, like, super, super sensitive to caffeine, and she couldn't get to sleep that night. But it does just seem to happen, like once every few months, she just cannot sleep. And I suppose that happens to all of us. Oh, yeah,
Scott Benner 1:29:56
that's fine, but the anxiety, if that. Sh keeps creeping up, or you see any other thyroid symptoms, please like, get that addressed and see if that doesn't help the anxiety.
Unknown Speaker 1:30:07
Okay, okay, I will do all right, thanks. Sorry.
Scott Benner 1:30:17
If you're ready to try America's most loved food delivery service, just check out hungryroot.com/juice box. Plan start as low as $69 per week. You can skip a week or cancel at any time. Hungryroot.com/juice box. I want to thank the ever since CGM for sponsoring this episode of The juicebox podcast, and invite you to go to ever sense, cgm.com/juicebox, to learn more about this terrific device, you can head over now and just absorb everything that the website has to offer, and that way you'll know if ever sense feels right for you. Ever sense, cgm.com/juicebox, a huge thanks to touched by type one for sponsoring this episode of The juicebox podcast. Check them out on their website, touched by type one.org or on Facebook and Instagram. Hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast, if you have type two or pre diabetes, the type two diabetes Pro Tip series from the juicebox podcast is exactly what you're looking for. Do you have a friend or a family member who is struggling to understand their type two and how to manage it? This series is for them seven episodes to get you on track and up to speed. Episode 860, series intro. 864, guilt and shame. Episode 869, medical team. 874, fueling plan. Episode 880, diabetes technology. Episode 885, GLP ones, metformin and insulin and in. Episode 889, we talk about movement. This episode is with me and Jenny Smith, of course, you know, Jenny is a Certified Diabetes Care and Education Specialist. She's a registered and licensed dietitian, and Jenny has had type one diabetes for over 30 years. Too many people don't understand their type two diabetes, and this series aims to fix that. Share it with a friend or get started today, the episode you just heard was professionally edited by wrong way, recording, wrong way, recording.com, do.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1282 Weekly News 8/12/24
For the week of August 12, 2024
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome back to the juicebox podcast.
Lovely to see you again. This is the News episode for the week of August 12, 2024 these are the diabetes related news stories I found interesting. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. If you'd like to help with type one diabetes research, you can do it right from your home without ever seeing a doctor by going to T 1d exchange.org/juicebox when you get there, just join the registry and complete the survey. This should take you about 10 minutes. Your answers to very simple questions will help type one diabetes research move forward. You need to be a person who has type one diabetes or is the caregiver of someone with type one and a US resident to fill out the survey. T 1d, exchange.org/juicebox, please take those minutes. They will really help when you place your first order for ag one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink, ag one.com/juice box. This episode of The juicebox podcast is sponsored by ever since the ever since CGM is more convenient, requiring only one sensor every six months. It offers more flexibility with its easy on, easy off, smart transmitter, and allows you to take a break when needed. Ever since cgm.com/juicebox, Hey everyone. I did some recording on this file earlier in the week, but then found this news, which I'm moving to the front, which doesn't mean that the stuff at the back is not important, but it's going to sound a little disjointed after this part's over, you'll understand why in a second I've seen an article that I'm just I'm very excited about. This is from qz.com it's quartz titled, getting your hands on zepbound may get easier this year with new single dose vials. Now, for anybody who's been using a GLP off label with their doctors help, of course, to help lower their insulin resistance, who's type one, but you're losing too much weight because you don't need the full 2.5 or five or whatever they're giving you if you know you're having impacts beyond insulin resistance, and you think, Oh, I wish I could just take a little less of this or spread it out a little more. But I wish I didn't have to just do the injector pen every time. I wish I had a little more control. I wish my doctor could help me dose this differently. If you've had that thought, listen to this. Eli Lilly will start selling single dose vials for starter doses of zepbound in the coming weeks. Lily announced on Thursday that it finally is launching single dose vials for starter doses of blockbuster weight loss drug zeppbound, which, of course, is just mandarno marketed for weight loss. The move will potentially help meet stronger demand for the popular drug. I don't care what this article says. That's not why I care about it. The company said its second quarterly earnings report, said in its second quarterly quarterly earnings report for 2024 that it will start selling in the US single dose files for 2.5 and five milligram doses of set bound in the coming weeks. The news comes as the pharma giant said sales of highly sought after diabetes and weight loss drugs during the second quarter outperformed expectations, resulting in their raising their revenue. Outlet. That's money I don't care about that. Sales of Manjaro in the quarter reached 3 billion. Wow. Hold on a second blowing class drugs. I know all that skyrocketing demand frustrated. Zipbound users have been calling on the company to address the supply constraints. All right, look, I don't care about any of this, and this is not advice, medical or otherwise, but if you're a person who's been wanting to micro dose, GLP, this has got to be incredibly exciting news for you. I know that my daughter is using it with a prescription through a doctor covered by insurance, even not ZF bound, but manjarno, and her dose at the lowest dose is it's too much for her, and so we've been trying to figure out ways to to to impact that. But you know, so far, all you've been able to do is just stretch it out, not do it every week, do it a little longer. But all that does is it gives you a bunch of days up front of coverage, and then days in the back and that don't have as much coverage, and then days that have even less coverage, if not none, until you put it in again. It's not a perfect system. I'm sitting here watching it, thinking over and over again. I wish I could just draw this up with a different needle and use less I cannot wait to talk to her doctor about this. This is, I think, really exciting and awesome news. Once again, the single dose vials of zepbound, introduced by Eli Lilly, are available in 2.5 and five milligram doses. These vials are intended to make the drugs more accessible and easier to manage, et cetera and so on. That's it. The article is called getting your hands on zepbound may get easier this year with new single dose vials. Go ahead and Google it. I think it is insanely exciting. While we're talking about Eli Lilly. This is from ABC News. Eli Oli warns in an open letter on Thursday about the dangers of fake and compounded versions of its diabetes, weight loss medications. Manjarno and zepbound companies announced a lawsuit against wellness centers and medical spas advertising the drugs. Eli oh the Novo Nordisk, which of course, is a competitor. They sell ozempic And we govi have also filed these lawsuits to med spas supporting who are selling knock off versions. Looks like they're protecting their investment here, and the warning from Eli Lilly says the company is deeply concerned about the proliferation of online sales of fake versions of its products, and that people should never put products labeled research purposes only and not for human consumption into their bodies. That's just good advice no matter what. Anyway, that's the thing. Go ahead and check that out if you want. ABC News Eli Lilly warns about dangers of fake and counterfeit Manjaro and zebound. And now the rest of this episode is going to be it'll feel disjointed for half a second because I recorded that stuff first. But just get paid. The podcast is sponsored today by ever since CGM, ever since cgm.com/juicebox with ever since there's no need for frequent sensor changes, no more sensors falling off, fewer failed sensors and less skin irritations, and that means more comfort with Eversense. You only need one sensor insertion every six months, and there's no need for constant sensor changes, which means less hassle. There's also no need to carry extra sensors with you, so that's less stuff to worry about, and you can say goodbye to unexpected disruptions from sensors falling off or being knocked off, because the Eversense CGM is implantable and the sensor stays comfortably in place for six months. The Eversense sensor is incredibly durable, and of course, that means fewer frequent unexpected sensor errors that happen before the end of the suggested wear time. But what do you really want to know about accuracy the ever since CGM performs exceptionally over its six month life. If you'd like more details or are interested in getting started, use my link. Ever since cgm.com/juicebox, I'll be telling you a lot more about ever since this year. So make sure you pay attention to upcoming advertisements. There you'll learn about the implantable sensor, the smart transmitter and their mobile application, the Eversense CGM lasts up to six months, eliminating the hassle and discomfort of frequent sensor insertions. Simply put, it makes managing your diabetes so much easier. Eversense cgm.com/juicebox, you let's take a look at the News for the week of August 12, 2024 what do we have here? Oh, want to start simple. Looks like oh my gosh. How do you say this umia Is that it omia Omio, Omio University. This is in Sweden. It's spelled U, M, E, and then it has a funny a with a hat. Anyway, they've done a little study, and research has uncovered that there's a potential link between type two diabetes and Alzheimer's disease. The study found that high blood sugar levels may hinder the body's ability to clear beta amyloid proteins, which are associated with Alzheimer's. This, of course, suggests that better blood sugar management could reduce the risk of developing Alzheimer's. Not a ton with that, but I like there's research in that space. Next we're going to move on to the ever since CGM. Let me find this article for you, and I'm going to finish up here by with, by with I'm going to finish up here by telling you about two trials that I learned about through diatribe. First one is a new trial for the test ozempic for kidney disease and type ones trial name, let's see trial of semiglutide for diabetic kidney disease in type ones. I may have talked about this one before, but I wanted to put it out there again, if I haven't. Researchers are recruiting 60 adults with type one diabetes and kidney disease for the trial, participants will either receive ozempic or a placebo at the end of the 20. A six week trial. Participants will undergo an MRI scan to measure how much oxygen is delivered to the kidneys and used by kidney cells. Kidney oxygen. Oxygenation is an important indicator in kidney function. I'm reading directly from diatribe. By the way,
researchers will also measure uacr, an estimated glomerula, glue, Merola filtration rate, measures the amount of protein in the urine. This is interesting. You should like Google this and find that a diatribe interested participants. You have to be 18 years old and have been diagnosed with type one diabetes for at least five years, have an A, 1c under 9% have a uacr of at least 30 mg G and an E, G, F, R of at least 45 milliliters per minute. And then it says like 45 milliliters minute, 1.73 m2 I'm sure if you have that, you know what that is. And are you stable doses of blood pressure and cholesterol. Are you on stable doses of blood pressure and cholesterol lowering medications? People who have had recent diabetic ketoacidosis or a history of pancreatitis are not eligible for the study. There's a full list of inclusions anyway. This is cool. If I think if you Google new trial tests ozempic for kidney disease and type one diabetes. You're going to come to it. I'm actually going to test that for you, to let you know that will definitely take you to the diatribe article about it. Go ahead and take a look. I think that's pretty cool if you need it. And another study, again from diatribe, new study test. I got it from their website, they're not doing the study. New study tests liver targeting insulin and type one diabetes. If you're an adult who has type one diabetes, you may be eligible to participate. Trial name is phase 2b trial comparing HDV, insulin LIS Pro to insulin lispro in adults with type one diabetes receiving insulin, decludec, o, p, t, I, two. Wow, who named that one trial sponsor is diameter pharmaceuticals, a study researching whether administrating a liver targeting insulin called h, d, v, l, insulin will improve glycemic control by reducing nocturnal hypoglycemia while maintaining or improving HBA 1c and people living with type one diabetes. How does the trial work? Researchers are recruiting roughly 230 adults with type one diabetes, ages 18 to 79 who are on multiple daily injections. Participants will be randomized and either receiving the insulin Lisp bro or insulin or the HDV L, insulin must pro in combination with basal insulin traceba, all participants will wear a continuous glucose monitor. The entire trial will run eight months, inclusive of a screening and follow up periods. This trial will include a screening period of up to three weeks, a run in period of two weeks to access eligibility and to transition to use of the insulin, etc, and the CGM, 12 week dose optimization period, a 13 week maintenance period, a two week transition follow up period, wow. 18 to 79 type one with a confirmed blood C peptide, result of negative point six or less than point six, you have to have been on insulin for six months, are willing to use the designated CDM device and for where to go and forego an insulin pump or automated insulin delivery system through the duration of the study, you need an A, 1c reading between 6.5 and nine, and you need to be using a total daily insulin dose that is 1.25 units per kilogram per day or less. People who have used weight loss medications, dietary supplements for weight loss or glucose lowering, medications outside of insulin 30 days prior to the study are not eligible. Sounds like if you're using a GLP, you ain't gonna be in it if you're interested. Google new study test, liver target, targeted insulin in type one diabetes. And I have one more thing for you. I don't know if this is news or not, but it's a press release. I think it's exciting and a little telling. Beta bionics, who of course, made the eyelet pump, is announcing that they've reached their 10 1000s. 10 1000s, 1000s. Oh, my God, the 10th. I'm tired. I don't want to be judged over this, but I'm not going to edit this out anyway. They've got 10,000 people using the eyelet pump. Again. This is a press release. So grain of salt, because I don't usually think companies say things like that are bad about themselves in press releases. But I don't see anything bad here. I just see an announcement. Pretty quickly, they got 10,000 people on. I let I think that's a pretty hell interesting milestone. Beta bionics, a commercially staged medical technology company, proudly announced that 10,000 patient start on the islet bionic pancreas. Significant milestone marks, a major step. Up towards the company's mission to alleviate blah, blah, blah. I let in case you don't know, and this is from the the the writing here, but I think it's important to say the first FDA cleared autonomous closed loop insulin delivery device designed to be both easier and prescribed for health care professionals, etc, for prescribers and for patients. So if you don't know anything about eyelet, I have a couple of episodes about it. It is a pump that you just tell it, it's breakfast and I'm having a meal. That is, I think I forget. There's three distinctions, smaller than usual average, or larger than usual, or it's lunch, and that you know, smaller average, larger. Episode 934, and episode 1217, so far is I let content, and we have more coming. We have some islet users on the recording schedule. So anyway, congratulations to beta bionics rate in 10,000 that's pretty awesome. I
want to thank the ever since CGM for sponsoring this episode of The juicebox podcast and invite you to go to ever since, cgm.com/juicebox to learn more about this terrific device, you can head over now and just absorb everything that the website has to offer. And that way you'll know if ever since, okay, well, here we are at the end of the episode. You're still with me. Thank you. I really do appreciate that. What else could you do for me? Uh, why don't you tell a friend about the show or leave a five star review? Maybe you could make sure you're following or subscribed in your podcast app, go to YouTube and follow me, or Instagram. Tik, Tok. Oh gosh, here's one. Make sure you're following the podcast in the private Facebook group as well as the public Facebook page you don't want to miss. Please do not know about the private group. You have to join the private group as of this recording, it has 51,000 members in it. They're active, talking about diabetes, whatever you need to know. There's a conversation happening in there right now, and I'm there all the time. Tag me. I'll say hi. The episode you just heard was professionally edited by wrong way recording, wrong way recording.com, you.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1281 Whole Lotta Rosie
Emily is the mother of a 14 year old child with type one diabetes.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome to another episode of The juicebox Podcast.
Today, I'll be speaking with Emily. She's the mother of a 14 year old child who has type one diabetes. There's some other autoimmune stuff throughout her family, and let's see what else. So she's an expat living in the United Kingdom. Her daughter has chronic digestive issues as well as type one, and today we're going to talk to her all about that. Nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. If you have type one diabetes, or are the caregiver of someone with type one and your US resident, I'm asking you, with much love, to go to T 1d exchange.org/juice, box, join the registry, complete the survey you're helping with type one diabetes research. T 1d exchange.org/juice, box. Go complete that survey. Please. When you use the link, hungry root.com/juice, box, you'll save 40% off of your first order. All the details are at the top of the link. Hungry root.com/juice box, and check out the private Facebook group, juice box podcast, type one diabetes. You want to meet people who live with diabetes. You're going to meet a lot of them there because we have 52,000 active members. Us. Med is sponsoring this episode of The juicebox podcast, and we've been getting our diabetes supplies from us med for years. You can as well. Us, med.com/juice, box, or call 888-721-1514, use the link or the number. Get your free benefits check and get started today with us. Med, this episode of the juice box podcast is sponsored by the ever since CGM, ever since is going to let you break away from some of the CGM norms you may be accustomed to. No more weekly or bi weekly hassles of sensor changes. Never again will you be able to accidentally bump your sensor off. You won't have to carry around CGM supplies and worrying about your adhesive lasting. Well, that's the thing of the past ever since cgm.com/juice box. This show is sponsored today by the glucagon that my daughter carries. G vo hypo pen. Find out more at gvoke glucagon.com forward slash juice box.
Emily 2:36
Hi. My name is Emily, and I am the parent of a 14 year old girl with type one diabetes.
Scott Benner 2:43
Your daughter is 14. Emily, how old are you
Unknown Speaker 2:47
47
Scott Benner 2:50
Do you really not know, or you don't want to say, I, yeah,
Emily 2:53
no, no, I, I'm pretty sure I'm 47 you know, you know, like after 45 I feel like you kind of forget.
Scott Benner 2:59
I haven't said this in a while, but there's been twice in my life that I've lived an entire calendar year of my life believing that I was a different age than I was. See, I'm
Emily 3:08
glad I'm not the only one.
Scott Benner 3:11
I just might one day, I said to my wife, like, I can't I can't believe I'm gonna be, what was it 49 can't believe I'm gonna be 49 on my birthday. And she goes, Are you kidding me? And I was like, what? And she goes, You are 49 and I was like, No, I'm not. And I stopped. I was like, 1970 Oh, my God, a whole year of my life happened to me twice. You're 47 she's 14. Married. Any other kids, anything like that?
Emily 3:32
Yeah, married. And I have a 24 year old and a 20 and a 21 year old. Oh,
Scott Benner 3:38
Emily, there's the story, right? There is the 14 year old with a second husband. Or did you guys go to a wedding?
Emily 3:44
No, all, the same, all, all, same, same. What happened? What happened that I have a 24 year old?
Scott Benner 3:53
No, what happened? I get the 24 year old. I'm okay with that. Oh, the seven years between the let, like, seriously, did you have sex by mistake? Like, what happened?
Emily 4:03
Well, okay, so we got, I got pregnant, really young, with our first. And then, you know, after, if you want one, you think, well, let's have another one, right? And so then we had our second. And then I, my husband, went to grad school, and then I went to grad school, and I don't know, we always wanted another one. And then we had Rosie gotcha years later. All
Scott Benner 4:31
right, so I gotcha. So you guys took care. You guys had family first, maybe not on purpose.
Emily 4:38
Yeah, it was a surprise. Yeah,
Scott Benner 4:40
I have a baby like that. And then you took care of yourselves, put yourself in the position you wanted to be in, and then went back again and said, Okay, build a family, build a life. Let's have that, uh, that last baby we're thinking about. Yeah, oh, that's for See, that's a very wholesome story.
Emily 4:56
Yeah, yeah. I mean, I did tell you it's kind of boring, but, yeah.
Scott Benner 4:59
I thought maybe you guys, like, got bored for seven years, then one day, went to a wedding, and the next thing you know, you had a baby. Because that's what usually happens. Little drinky. Little drinky on a Saturday night, feel young for a minute. You know what I mean? I
Emily 5:10
mean my my second kid was pretty, pretty challenging. I felt like I needed a lot of I needed a lot of time in between. And there was a point where they so they're just so, you know, they're non binary, and I sorry, and they use the for their trans FEM, and they, they use they, them as pronouns. Okay, that this is my 21 year old. And sometimes I mix up, though, if I go back, because when they were younger, I think of them as a boy. So if I mess up, it's just because of that. But anyway, when my 21 year old was younger, I don't know, eight years old, and I was, I was kind of working part time at but mostly like staying at home with them, and it was just so hard. And I thought, What could be easier than raising this child? And so I put them in daycare and went to grad school because I school because I actually thought that would
Scott Benner 6:06
be easier. Do they know that about themselves as a little kid?
Emily 6:09
Oh yeah, like, yeah. They were like, yeah. They're just really funny person. And they'll say, Yeah, I was a total asshole.
Scott Benner 6:18
Is there any auto immune with you, your husband or your other two kids.
Emily 6:21
I suspect that my 24 year old has, or I hope that he doesn't have Crohn's or celiac, but I it's possible he's had a lot of GI issues. And you know, you can only tell your 24 year old so many times that they should probably get an official celiac test, but they just took out gluten and that they're like, look, it works. I feel better. So I don't know, I definitely have some arthritis issues, but it, I think it's probably osteoarthritis. My mom has some pretty severe arthritis issues. Also, she's always been told it's osteoarthritis, but it does both of our hers is quite severe now, and both of our issues tend to be kind of autoimmune in nature, likely just called osteoarthritis rather than rheumatoid
Scott Benner 7:13
and Rosie just type one or anything else. If you take insulin or so final ureas, you are at risk for your blood sugar going too low. You need a safety net when it matters most, be ready with G VO, kypo pen. My daughter carries G VO, K hypo pen everywhere she goes, because it's a ready to use rescue pen for treating very low blood sugar in people with diabetes ages two and above that, I trust low blood sugar. Emergencies can happen unexpectedly and they demand quick action. Luckily, GEVO kypo pen can be administered in two simple steps, even by yourself in certain situations. Show those around you where you store GEVO kypo pen and how to use it. They need to know how to use GVO kypo pen before an emergency situation happens. Learn more about why GEVO kypo Pen is in Arden's diabetes toolkit at gvoke, glucagon.com/juicebox, gvoke shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma, or if you have a tumor in your pancreas called an insulin Oma. Visit, gvoke, glucagon, com, slash, risk for safety information, yeah.
Emily 8:29
I mean, she definitely has some kind of GI issues going on as well, but she's always negative for celiac and doesn't seem to have anything it. I mean, she doesn't seem to present with anything like Crohn's or colitis or anything.
Scott Benner 8:45
Are those issues just since the diabetes? No,
Emily 8:48
she's always kind of had kind of chronic constipation, which I know that seems to be kind of a common theme with a lot of folks with type one, but that, I you know, we've addressed it, but it's, it's still there. I mean, even today. So she, she missed school this morning because of a stomach ache. And, you know, I don't, I don't really, I can't really explain it, you know, we've been to the I've been to the GP. We've been to, I've talked to her consultant about it quite a bit.
Scott Benner 9:16
I have an easy thing for you to try.
Emily 9:19
So, yes, okay, I
Scott Benner 9:21
don't know if you've heard the episode called Arden supplements.
Emily 9:26
Oh, yes, yeah. Has
Unknown Speaker 9:28
she tried? I
Emily 9:28
just haven't, yeah, I just haven't done. I mean, we do a probiotic. I'm trying to remember the one that you Yes. I will go back and listen to that.
Scott Benner 9:37
Yeah, it's 767, but the the quick, easy answer is just to try mixing a digestive enzyme with her meals. Oh, yes, and see, and see if that whole thing doesn't kind of work itself out. Yeah,
Emily 9:51
we'll definitely give it a go. I mean, I feel like we've kind of, we've done the whole macro goal route. And,
Scott Benner 9:57
yeah, it's a low cost. Yeah. Thing, it's there's no skin off your ass to pop the little tablet in your mouth before you eat for a week, just to see how it goes. And, you know, I try to remind people as much as I can, like your pancreas doesn't just make insulin. It does other things and has a lot to do with digestion. A lot of people with type one seem to have digestion issues. Yeah,
Emily 10:18
yeah. I think, yeah, that's a good reminder. Thank you. I will give that a go, and like,
Scott Benner 10:23
I have a question before we move forward, there's a rock song. I think it's an AC DC song with Rosie in the title. And my brain can't think of it, and it won't leave me alone about it. Do you know what
Emily 10:35
it is? Oh, you don't know. No, sorry. I mean, I probably knew all the songs in high school. I got it. I feel like my brain doesn't swear that anymore.
Scott Benner 10:45
Whole lot of Rosie, oh, okay, I don't know what it's about. I'm not making any inferences about your kid. I'm just it got you said, Rosie, and I'm like, oh, there's a song. And I could feel the isn't that strange. I could feel the beat of the song, but I couldn't hear the music, and it couldn't and now, just now, when I thought, I think it's a CDC, then I was able to google it real quick. Anyway. Now I was gonna think about the whole goddamn hour if I didn't figure it out. So I apologize. Now
Emily 11:11
I'm gonna look for it for her. Then she kind of likes the songs from my high school, 70s. Yeah, no, wait, that's not 70s, right? Wouldn't that be later?
Scott Benner 11:22
Wait, a CDC is not maybe it would be this song, 77 okay, it was on the, all right, on the, Let There Be Rock Album in 1977 okay, you're older than you think you are. Emily,
Emily 11:33
it's true, yeah. I mean, it was born in 77 so wasn't listening to a CDC then? But, yeah,
Scott Benner 11:40
sure, but we all were, I mean, honestly, no, in my 20s, like classic rock radio was huge, so you're about you're a couple years behind me, maybe not. Well, I don't know, it's not worth talking about, because that's not why you're here. Mostly, why are you here? What made you want to come on? Well, a
Emily 11:58
friend had been on, and she had said, oh, you should do it and and we, I think you, maybe you were looking for guests on the Facebook group. And I've always thought, Well, I'm not quite sure what I what I could talk about, because you do interview a lot of, I don't know, white middle class moms. I sent an email and thought I could talk about unschooling. So Rosie, she now actually goes to school, but she never went. She did not go to school until age 14. And we are Americans living in the UK, and have chosen to stay, partially because of health care here. So I don't know if that's interesting to
Scott Benner 12:36
we're gonna find out. Listen. Also very possible. We call this episode, white, middle class mom, so you said at the beginning, like, I'm gonna be boring. I'll put a boring title with it. That'll be fantastic. It
Emily 12:47
is, isn't it? Yeah.
Scott Benner 12:49
So how do you end up in in England
Emily 12:51
first? Well, we so we were living in Portland, Oregon, and mostly raised our kids there, and we had briefly lived overseas before. So we lived in Japan briefly, and thought it was a great experience for us and a great experience for our kids, and we were open to the idea of going abroad again. And my husband was able to just kind of get a work transfer over here. And so we came over for kind of this two year experiment, and eight years later, here we are,
Scott Benner 13:24
eight years you've been there now, yeah, you have no accent at all,
Unknown Speaker 13:30
no British accent, yeah,
Scott Benner 13:31
but you don't even like a touch of it. Like, I went on vacation in the south once my father came home, like, you know, like he was on he Hall, so like
Emily 13:39
Southern accent, yeah, it does come out every once. Like, I think there's certain words that I say that on even on accident here. Like, if I'm talking with people and I say tomato, I you know, which is just so ridiculous. But you know, you hear, you hear words the British way, all the time. Then you start to say them. But yeah, I don't think I do.
Scott Benner 13:59
Would you say aluminum, or would you say aluminum? Oh,
Emily 14:04
aluminum. Okay,
Scott Benner 14:05
all right, yeah, yeah. I
Emily 14:06
mean even Rosie. I mean she's been here since she was six, and she doesn't, I don't think she has a British accent at all, although, when we go home to Portland, you know, friends and family will say, Oh, she's got an accent, but she definitely doesn't. I
Scott Benner 14:18
gotcha. Okay, I'm sorry you used the term about school that made it feel like I actually felt like you were making a hemp purse while you were using that term. It sound like such a hippie thing, but what is it?
Emily 14:28
I know it's so hippy dippy. Yeah, yeah, it does, yeah. So unschooling. Unschooling
Scott Benner 14:34
is that like, when what's her name divorced the kid from Coldplay? Did they uncouple?
Unknown Speaker 14:41
Oh, remember that who's,
Scott Benner 14:43
who's the, who's the lady that sells you the egg for your vagina. Oh, okay, and she was married to the Coldplay boy, right? I can't talk about, by the way. I don't want to go down this rabbit hole again, Emily, but I don't like Coldplay, and I. Had that in front of my son. I said they only have two or three good songs. And he's like, my son goes, Look, I'm not a Coldplay fan. He goes, but they have it. They have more good songs than that. And then he made me go through them in the car. And they did have, I'm gonna just say they did have about eight songs that I enjoyed. I just don't like the Coldplay boy. He gives me a weird he gives me a weird, douchey vibe. Just yeah, you know what? I mean, yeah, yeah. Anyway, when they got divorced, they told people they were consciously uncoupling.
Unknown Speaker 15:28
Oh, yeah, that that
Scott Benner 15:30
so with that embarrassment in your mind, tell me again, what it's called, unschooling. Unschooling.
Unknown Speaker 15:36
How does that happen?
Emily 15:37
Yeah, I mean unschooling, it's definitely kind of more of a I guess it is used here in the UK, but it's not necessarily on educating, right, or, or it's not anti school or anti education. I think the term was started by folks that maybe didn't want to necessarily home school. They didn't want say they were, they were going to not send their kids to school, right? But maybe they didn't want to say, Sit at the kitchen table and just, do you know, books in a curriculum the whole time, right? Yeah. I mean, it's again, it's not anti school here, I would say here. People mostly say home educate, I guess, which is kind of, I think of that as homeschooling too. But, yeah, I don't know if I'm explaining, no,
Scott Benner 16:20
I haven't Emily, what? How does it? So first of all, you've got a 2421 and a 14. Does a 24 year old go to regular school, K through 12? So
Emily 16:29
my 24 year old went to so he went to school when he was younger up until about first grade, and then we went to Japan. And so that time I had just the two kids, and I went to his teacher in first grade, and I said, Look, we're going to go to Japan for three months, and it's going to miss all this school. I'm really worried. Could you give me the, you know, the curriculum, and we'll follow along? And I had visions of, you know, we're going to, maybe at the time, you know, Skype, right, zoom, or anything, but maybe we can Skype with the class, and we'll follow along with this curriculum. And you know, this teacher was so nice and printed out, you know, this huge stack of worksheets for us to do. And so, you know, I dragged this all the way to Japan with us, and I remember one of the first week days we were there, I said to my son, you know, it looks like the class is doing they're making this bird habitat out of con balls. So we, you know, we should do that? Well, we can take some pictures, we can send it to your teacher. And my son was like, I don't want to make that. Why? Why would I make that? Why can't we just go to the zoo? Why would we make this bird habitat out of cotton balls? And I thought, actually, you're right. I don't want to make this either. And then I just started taking my kids all over. I mean, you know, how lucky were we? I feel like, very privileged that we got this opportunity. We went to every museum in Tokyo. We traveled all over, you know, as much as we could in those three months around Japan, he was reading everywhere. So he was constantly had a book in his hand on the trains in Tokyo. The train system is color coded and numbered. And he would figure out, you know, if we were at, say, like, you know, the yellow station. I mean, does have a name, but say, like yellow 32 or whatever. And we were going to go to train station, yellow 17. How many stops do we have? So he and he would figure that out. And he so he was constantly doing math, right? And then I could send him to the store at age seven, you know, with Japanese currency, and he would go and buy the milk for us. And he knew that how much changed he should get. So he, you know, he was learning just from living, right? I think my younger one was maybe about four, my kid who's 21 now and then, when we got back to the US, you know, it was summer, and then he was going to start in the next year, or maybe even second grade, whatever it was, anyways, young primary school, right? And so I went to his the next teacher that he was supposed to go into, I think it was third grade. And so I went to it then the third grade teacher, and I said he missed the, you know, these three months of school, and I had this curriculum, but I'm really sorry we didn't do it. So I feel like he's probably going to be behind. I'm really sorry. You know she, of course, you know she gets like, a very serious look on her face and like, oh, okay, did
Scott Benner 19:31
I'm sorry. You can't come back until you give us a cotton ball birdhouse,
Emily 19:36
yeah, yeah. Well, that's right, yeah, where's that cotton ball birdhouse?
Scott Benner 19:39
Diabetes comes with a lot of things to remember, so it's nice when someone takes something off of your plate. US med has done that for us. When it's time for Arden supplies to be refreshed, we get an email rolls up and in your inbox says, Hi, Arden. This is your friendly reorder email from us Med, you open. Up the email. It's a big button that says, Click here to reorder, and you're done. Finally, somebody taking away a responsibility instead of adding one. Us, med has done that for us. An email arrives. We click on a link, and the next thing you know, your products are at the front door. That simple, us, med.com/juice, box, or call 888-721-1514, I never have to wonder if Arden has enough supplies. I click on one link, I open up a box, I put this stuff in the drawer, and we're done. Us. Med carries everything from insulin pumps and diabetes testing supplies to the latest CGM, like the libre three and the Dexcom g7 they accept Medicare nationwide, over 800 private insurers, and all you have to do to get started is call 888-721-1514. Or go to my link, us, med.com/juice, box. Using that number or my link helps to support the production of the juicebox podcast. This episode of The juicebox podcast is sponsored by the only CGM you can take off to get into the shower. The ever sense CGM, ever since cgm.com/juicebox, well, I mean, sure you could take the other ones off, but then you'd waste the sensor and have to start over again, but not with Eversense. Eversense is a six month wear implantable CGM. So if you want to take a shower without anything hanging on, you pop off the transmitter, jump in the shower. When you get back out, put it back on, and you're right back to where you started. Come to think of it, you could do that whenever you wanted to. Maybe it was your prom night or your wedding day. Maybe you just don't want the thing on for a little while, but you don't want to go all through the hassle of taking it off and having to restart it, and, you know, starting back over with, like, wonky numbers, and having, you know, all that that goes with it when you take off a CGM and put it back on. Oh, but you don't have to do that with the Eversense CGM, because ever since is the only long term CGM with six months of real time glucose readings. This gives you more confidence, more convenience and flexibility. The Eversense CGM is there for you when you want discretion, a break, or maybe just a little adult time. Eversense cgm.com/juicebox, cgm.com/juicebox, pop that transmitter off, pop it back on. You're right back where you started, without any wasted devices or time.
Emily 22:29
So then she stopped me several weeks later, and she said, You know, I don't know what you did, but he's actually way ahead. And that's when I realized that, oh yeah, we could just kind of do our own thing. So that kid went through, so he finished around fifth grade, and then started kind of home educating on schooling with us. And then my, my kid, who's 21 got through about, I don't know, the middle of the year of first grade, and I realized, I don't think this kid is cut out for a classroom. I mean, they weren't the kid that was like running to the window when a bus would drive by or anything, but they would just sit at their desk and take a nap the whole time. And so I felt like we needed something else for my, my middle, now, my middle kid, because at the time, they were coming home after school and saying, Well, you know, I'm a stupid one, and everyone else is smart. And I thought, you know, you have to like yourself that minimum, right? You have to at least believe in yourself, or the learning is not going to happen at all. So we kind of started doing our own thing and taking lots of classes. Support. Linen has a really nice, I say, home ed or unschooling community. So lots of folks that are kids don't go to school, but they take classes in the community or extracurricular activities anyway, that's what we did. And then Rosie came along, and at that point, that's just six we moved over. Yeah, we just kept doing it. And then when we moved to London, I mean, it was amazing. She's been to, probably been to, you know, nearly every Museum in London with peers in some kind of home Ed shop, in a museum or over a historical site.
Scott Benner 24:07
I have a question. So, I mean, you have a 24 year old, right? Did they go to college?
Emily 24:12
Yeah, so what they did is, they're really into music, and so when we moved over here, trying to remember the track, they just they did. They wanted to do music production, and they were already kind of dabbling in it on their own, or, sorry, on his own. And so he, let's see, I think he took the S, A, T or no, sorry, he took the US, G, D early, because I think he was about 16 or 17 at the time, and a lot of home, home schoolers around schoolers, in the US use the US GED as a where they were. I'm not quite sure if they're still using it, but at the time, the US GED was sometimes a good way to access, say, like Community College, yeah, or, you know, adult classes that you want to take. And so he took the US GED, and then you. Used to that to apply here in the UK to a what's called the B tech level three in music production. And then he took that diploma, or the B Tech degree, and applied to university here for music engineering, although he did not finish. But that is because he he's in a band, and the band, well, won. The band was signed to a label at that time, and then also, he was already getting paid to do music engineering, so he was kind of, you know, already getting paid for something that he was learning in university. And felt like, you know, he felt like it wasn't really worth it to keep going at the time, you know, of course, I don't know. I think it was maybe kind of an old school idea of mine, like that. You just finished, get this piece of paper, right? This piece of paper is really important that says you've done this. But I think he was right. He didn't really need it, and he hasn't gone back
Scott Benner 25:57
that makes a living, takes care of himself, is doing well? Like, how would you, like, how would you hold up his current success against other 24 year olds?
Emily 26:06
I mean, probably fairly equivalent. I mean, you know, he's still, like, I mean, it's hard to make it in music, right? So maybe I would still call him a dependent in some ways, but, but yeah, he's doing, he's doing, all right. I mean, he's, we just want them to be happy. And, you know, interesting,
Scott Benner 26:24
yeah, Emily, I'm not, first of all, I'm not. I'm gonna ask a lot of questions. I'm not coming down on your position. I'm really interested, yeah, but, I mean, I think I had a kid when I was 24 or you did, yeah, you were on your way to another one, yeah? And then you take a very traditional route, you and your husband, and I'm guessing you've got two advanced degrees and you're living overseas. You guys are doing okay, yeah, yeah. So if you were broke, do you think you'd be like, hey, go to school, figure out something, because you got to get out there and make money. Do you think that this is partly a thing that they're able to do because you're able to fortify it?
Emily 27:03
Yeah, I do think that there's a whole lot of privilege in what we've been able to do, for sure, okay, but I don't necessarily think that a degree is for everyone. I mean, my 21 year old, you know, they were, they work in a pub right now, almost full time, and they're quite happy working in the pub, and they're not quite sure what they want to do. And I think that's okay. I don't, you know, I don't know if they will end up going to university or maybe doing something in the arts or, you know, I think it just depends on the person.
Scott Benner 27:34
I'm flexed by this I have a 20 My son just turned 24 like, two weeks ago, and my daughter's gonna turn 20, right? So I'm in your boat, minus the hey, let's have one more. I'm always like, like, running through this in my head, because I was incredibly broke growing up. My wife was broke growing up. We're more comfortable now. There's part of you that's like, I can't leave you an amount of money to make sure you're okay. Like, you're going to have to take care of yourself. Like, you know what I mean, like, how and the unknown of like, what does that turn into? Like, what if the system just demands what it demands, and whether it's right or wrong? Because I hear your story, and I think this is fantastic. Like, imagine raising a kid for all those years, taking them out, doing cultural things, letting them learn math and real world experiences like all this stuff sounds amazing. Your kids are probably amazingly, like, rich and, you know, in knowledge and experience and all that stuff. But what happens on that day when, like, so they meet somebody, and that somebody's like, I want a baby in a house, and I want a car, and I want the car to be safe, and I don't want to eat crappy food. And let's go right now. You know what I mean? And like, yeah, and you're like, I don't have a degree, I can't get that job, I don't know how to make that much money. Like, you know? Like, I'm happy. And you know what I mean? Like, when does that? That's my worry for me. Like, when does that worry? When does that I'm happy? Turn into I can't take care of myself that.
Emily 29:01
Do you think about that? Well, I would say I've never been anti education. I think, like, I think that my oldest kid is really academic. I think if he wanted to go, and if it was going to be more lucrative for him in the music field to go and do some kind of music to go, like, finish the music engineering degree, then, yeah, he should do that. But I don't know if that is necessarily for his industry what he wants to do. I don't know if a degree is really necessary. If he had said, Look, I want to be a pharmacist or whatever, of course, you know. But I think as long as you know, I mean, he's on the track to supporting
Scott Benner 29:42
himself. I'm talking about, like, when, again, I'm not talking about your kid. I just, you're just a good person to have this conversation with. Like, like, I'm talking about the difference between making enough to get by. You know what? I mean? Like, like, Hey, I got a job. I do. Okay? I make $50,000 a year. I pay my bills. I don't have a. Lot extra, but I have my my house is clean. You know what I mean? Like, I'm okay. I can cover my my nut, etc. The difference between that and when the person looks you in the face one day and says, I want the kids to have a yard to run around in, and it's on and it's on you, and you're like, I don't know how to make that happen. I can't believe I'm saying this, because I don't believe in this, but I do believe in it. I believe in what the world wants, not what might be right for you or another person. Like, what if you have nothing to fall back on? Like, you know, even just that, um, the idea of having a network of other people who went to college, who might be well employed, that you can call up and go, Hey, do you remember me, like, you got anything open there, like that kind of thing, like that. That disappears. You don't build that, that network, right?
Emily 30:48
Maybe you have a different network. I mean, if you Yeah, yeah. I mean, I guess there are plenty of folks that went through high school, like us, High School, for example, are here that, like, the GCSE track, which is somewhat similar, yeah, and then didn't go on to university, and they find their way. I don't know if, like, a bachelor's degree, you know, is right for everyone, and that's fine. I mean, in the US, it's quite expensive.
Scott Benner 31:18
Oh, I don't think it is. I don't think it's I mean, honestly, I don't know that it's necessary for anyone. It's necessary if you want to, if you have the expectation of, I mean, a single family home, or, you know, a car that doesn't break all the time, or $5 aside when you need it, or when you get old, and it costs $3,000 a month to stay alive, like, and you haven't worked in 15 years. Like, that's the kind of stuff. Like, it's just interesting. Like, your mind and my mind just we worry about different things. Like, because I guarantee you, you and I agree about all the fundamentals of what you've just
Emily 31:55
said about people and happiness, etc. Yeah, I don't know. I feel like I do know quite a few folks that have, you know, degrees, or even advanced degrees, that aren't necessarily like doing well. I mean, they have over well, I mean, they're doing okay, but you know that maybe they could, you know, have not done that track and still been this, made out the same, I don't know, or maybe have, you know, if they're in the US had less, yeah, it's
Scott Benner 32:22
the I don't college debt to worry about, right? It's so the part where I'm jealous of you is that it's the it's in the I don't know, like you're willing to say I don't know, and it doesn't matter, keep doing the thing you like. And I wonder if I'm not a person who says I don't know, but you better make sure you're going to be okay as best you can, even if it doesn't work out. These are the steps you should take to ensure as much as possible. This kind of, like,
Emily 32:50
comfort, yeah? Well, I mean, I was definitely there when my kid was like, I, I don't, I don't want to finish this bachelor's program because I'm already getting paid what they're teaching me. And this is kind of, you know, why would I do this, right? And at the time, you know, like I said, I definitely, and my husband as well, both of us were like, dude, just get the piece of paper right. Get this piece of paper. Since you have a master's degree, you're almost done, right? And, but now I understand. I mean, he would have missed out on all these music opportunities. So, you know, yeah, you're right. I don't, I don't know. I mean, I think, I think he's going to be okay. I'm not worried about,
Scott Benner 33:25
I wonder how much of the difference is just that you're, you grew up on the West Coast, right? Like the upper, the upper Northwest check, and I grew up on the east coast, where it's very like, it is quite culturally different. Yeah, it's like, go, go, go, win, kill, like, or die, you know what I mean? And right? And you, you kind of were like, hey, it's cool. We're gonna make like, Yo, we'll probably make heroin legal, like, like that, by the way, I think they took that back. Do you keep or, yeah, did you do you keep up with home? I think Oregon was like, Hey, we shouldn't have done that. And I think they went backwards on it.
Emily 34:01
Oh, did they? I don't know. I mean, I do try to keep up. I mean, I still vote out of Oregon, but not. I don't think I can vote in that. I don't know. In those measures, I can't, not quite sure, Oregon
Scott Benner 34:13
legislators vote to recriminalize low level drug possession.
Unknown Speaker 34:19
Oh, wow, wow. Wow.
Scott Benner 34:20
They were like, that didn't work. Let's try. It's too bad.
Emily 34:23
I feel like that works in Spain and Portugal. I mean, I yeah, I don't know. I mean, don't quote me there, please. I don't know anything. I feel like it works in other parts of the world, and maybe it could work. But, yeah, I
Scott Benner 34:36
just heard, I just heard it on the news the other day. I was like, they were like, they're going backwards on some of that stuff that they did, because it wasn't that long ago, right? They decriminalized, like most drugs, I think.
Emily 34:47
And I think so I didn't realize they backtracked that. But, yeah, I keep up as much as I can interesting stuff,
Scott Benner 34:53
so you have this great experience. Your children are growing up well, you're like, hell, let's just do it again. You're not the kind of. You're not looking to build up whatever, the whatever the British version of a cotton ball house is. So you're like, I'm not doing this. And then your daughter is is going along fine. How old is she when she's diagnosed? Then,
Emily 35:13
uh, yeah, so she was he, we were here when she's diagnosed. She was eight. Eight.
Scott Benner 35:19
Okay, like six years ago, out of nowhere, took you by surprise, I imagine,
Emily 35:25
yeah, I mean, I was surprised. I My mom has always shared this story that her her told her this. So this story was her grandmother would tell her when she was a child, was that the grandmother had moved from eastern Canada to California as a young woman with a sister that had diabetes, and the sister would have been very young, like late teens, early 20s, maybe, and that would have been at the turn of the century, and they had moved believing there was a cure for diabetes in California. And obviously the sister, she didn't make it right. And so my mom had always kind of talked about diabetes when I was a kid. I have one sister, neither one of us had type one, but I kind of knew about it, like if we were thirsty, for example. But, you know, just randomly, you know, my mom would be like, Oh, you too. Appetite in the family, right? But it would have been way back there and it didn't pop up again. I think my mom has a first cousin as well, but, you know, I didn't have any cousins with it or anything. So it was quite removed. When we lived in Portland for 10 years, I had a neighbor who her kid had befriended my kids, and her kid, at the time, was five and and this was even before Rosie was born. So her kid just liked being at our house. And I think she she had moved back to the neighborhood to care for her parents, and her kid had been diagnosed at age three. I think I was kind of the first friend that she met that when she said, you know, my kid has type one. Could he come over and play and, you know, here's all these things you need to know. Is that okay? And I was kind of the first person, maybe because I was a healthcare professional and was somewhat familiar with type one and interested, right? I said, Yeah, sure, he can come over and her kid had, I mean, he had sleepovers at our house. She when she went on her honeymoon, I I gave her kid mixed insulin and a syringe, you know, I checked his blood sugar in the middle of the night. I remember when she got Dexcom, and I remember, you know how excited she was, and her showing me Look, I can see, you know, his blood sugar on my phone. And, you know, I didn't quite at the time understand the level of excitement. I mean, obviously, now I get it. Yeah, you get it now. But I had all this experience with type one and then throw Z, obviously, you don't want it to be that, right? I mean, I thought, I thought that she might have it just because she was so thirsty and she was, it looked like her muscles were wasting away, right? And I bought a test kit and it and I went in one night, and I thought, I'm just gonna and I knew, and she wasn't. So she was pretty scared of needles, right? So, and there's no way she would have let me poke her finger. So I tried to go in in the middle of the night to like poker toe. And that didn't that did not work. So then the next morning, told my husband, look, I think, I think she might have type one, and, you know, he said, and he was quite familiar with my older kid's friend that had, you know, kind of grown up in the neighborhood with them, he said. Then he started worrying about it, too. And he's like, you know, I'm really worried about this. I think you might be right. And so I knew she wouldn't again, let me poke her finger. I didn't want to hold her down. I knew if this was type one, I needed to go into this with her 100% trusting me, right? And so I called the GP, and I just said, Look, I, you know, I think this is what's going on. Could we come in? And miraculously, we got a same day appointment, which is fairly rare here in the UK, although it does happen. And so I brought the test kit in, and I, you know, just told the GP, look, I think she might have this, could you please tell her? And it just explained that we have to poke her finger, because I wanted the GP to say it rather than me, yeah. And unfortunately, he, you know, he wasn't the best. And there are some great GPS out there in the UK. So I hope this doesn't, you know, give everybody, anybody a bad impression of the NHS, because it is, it is it is really amazing. I had a really horrible experience with it when she was diagnosed. But it is an amazing, you know, the energy test is incredible, but so the G, the GP, was like, No, we don't, we don't need to do that. And I, you know, I said, Well, are you sure? Because I brought this test kit. Here's all her symptoms. And I think. He probably saw in his practice. I mean, he probably saw a lot of folks with type two. He probably, you know, maybe didn't even ever see a kid with type one. I have no idea, but he just didn't really know about it. And well, first I said, Look, could you just then, could you at least dip her urine for me? Because then I'll know. And so he agreed to dip her urine, but then he did it incorrectly. And he said, Well, it does look like there's sugar in it, but, or glucose in it, but that could be an infection. And then I kind of knew that, you know that, that probably, he probably wasn't right. And so he said, Well, I'll order a blood test, right? How about because I did kind of press them, no, we need to do more. This is not, you know, not. And he said, Well, order a blood test. And then I thought it would be like in the US. I didn't have a lot of experience with the NHS at that time, right? So I just assumed the blood test would be, you know, the same day, maybe next door, maybe in the clinic, but the blood test was like next week sometime, and I think it was a Thursday or Friday, so it was, you know, kind of the end of the week, and blood test was in a totally different location. And so I just walked Rosie home from the GP, and I said, look, the GP wants to do this blood test in your arm here, I just want to poke your finger. You can do mine first. And could we just, you know, would you be willing to do that? And I convinced her, so she poked my finger first, and it was normal. And then we did hers, and it just said, Hi. So then, you know, we washed her hands. We did it again, and I again. I don't know if you want to the rest of my my story. It wasn't, it wasn't great.
Scott Benner 41:46
Well, I want to hear about, I gotta tell you that before you make me sad with this. I've so far been the saddest when you told me that your distant relatives went to California looking for I
Emily 41:58
know. Can you believe it? So sad. I know it's horrifying, isn't it? What it like? What a horrible death, right?
Scott Benner 42:06
Well, it just like, we're gonna try, I'm assuming, like horseback or wagon or something like that. Like you don't need my railroad. Yeah, you're making that trip thinking maybe there's a medical advancement there, that's not here, and you don't even make it to find out. And now you've relocated your whole family, and along the way, your daughter died.
Emily 42:27
Like I don't so the story that I know, and so my mom and my sister and I would like to go back to eastern Canada, where this grandmother had come from, and just maybe do some, I don't know, spend some time, and maybe, I think there might be some graves there that we could check out. I'm not sure. But my mom has, you know, she's really into genealogy, and she so, from her understanding, is it was just the two sisters. So the sisters left the parents, basically, and as young women, and, you know, again, probably went by train to California. Yeah, I think when my mom went back to look for the some kind of death record, it wasn't in California, so she's not quite sure, but that was the story that the grandmother had told her,
Scott Benner 43:17
right? Still, it's just, I don't, the whole i It's, it's the desperation of it that made me sad.
Emily 43:23
I know, yeah, I know, yeah. It's horrifying, isn't it was,
Scott Benner 43:26
yeah, that's what it was. Okay. So when Rosie's diagnosed, do you have a little bit of a collapse personally? What were you about to tell me?
Emily 43:35
Well, I didn't want it. I mean, I knew that it couldn't really be anything else. I mean, kids don't really tend to get pancreatic cancer, right, somewhat of a clamp collapse. But also, after all that experience in Portland with my friend and watching her raise her kid, and you know, he's such a lovely person, and I felt like I at least I knew we'd be okay. So I was sad for Rosie, but I felt like, you know, we'll be okay, yeah. So we've gone to the GP, you know, wasn't, wasn't very helpful, but now I've got this finger poke that I know she has type one, but I still didn't know quite what to do, because I hadn't had a lot of experience with the NHS yet. So I called the GP back, and I said, Look, you know, she definitely this has to be type one. I don't know what else it could be. Could you just tell me who in Greater London handles pediatric diabetes? And he's like, Why? Why do you think you need to go to the hospital? Why we can just, How about I'll order a specialist? Was like, I I don't have insulin in my home. What it you know? What if she goes into DKA? What you know? I I'm going to the hospital. I just need you to tell me which one to go to. I'm going. I'm telling so
Scott Benner 44:51
a few minutes ago, you thought we didn't need to check her finger, so I'm not sure. Yeah, yeah. What you know exactly? Yeah.
Emily 44:57
Finally, he gave me a couple. Options. I called a friend. She said, you know, go, go to this one, right? We went to this hospital, and I was just happy that they gave her insulin. But they, they were so weird about about the fact that we home educate, and that became the real focus of our of our visit.
Scott Benner 45:16
How did that even come up? You know? Because they just ask, like, Well, where
Emily 45:19
do you, where do you go to school? And that day, I mean, our plan for that day was, we were going to go to a nature study group in Kew Gardens with a bunch of friends. So it's not like, you know, I'm keeping my home school kid locked, you know, in the basement or something. You know, we're supposed to go to this learning group. And I realized, you know, I got this GP appointment, so we skipped it. We, you know, did that went to the GP that day. Now we've presented at the hospital. And then, you know, of course, they ask all these questions at some point, like when you go to school, and I said, well, she's home educated. And then they said, well, oh, we need to, we need to notify the local authority that you home educate. And I knew why the law? Yeah, well, exactly, they were wrong, so the law is on my side. And I said, Look, actually, you, you don't have my permission to notify the local authority, and could we just focus on the diabetes? So they asked a lot of questions, which was quite frustrating, because I felt like, I've, I've literally just explained ketoacidosis to the GP. I feel like I could probably teach ks two or ks plus School, which is at a school level here,
Scott Benner 46:29
yeah. And now it's like, now the focus went from your kid has diabetes too, at home, what's wrong with you? Yeah, no.
Emily 46:37
So I had to call, I had to call my other one the other kids at home, which they were teens at the time. And I just said, Look, you know, I'm really sorry. She does have type one, and we're going to be in the hospital for a while, and also social services might come to the door. Could you just not, could you not swear at them and just tell them where I'm at? Right? Anyway, social services do not want to see us. And, no,
Scott Benner 47:00
that was a miss. That was a miss, that was a misunderstanding at the hospital side. Well,
Emily 47:04
they messed up. So they did later. They sent me a formal apology, and they apologize. And they were, you know, they were really worried because they had violated our privacy, our information, right? They they should not have shared our information without my permission. That is the law. Like they did
Scott Benner 47:20
it anyway. When you said, Don't do that,
Emily 47:21
yeah, but I mean, at the time, it was pre pandemic, you know, it was pre covid, right? And home homeschooling or home education, it wasn't very common here at the time. And so I think, I think, to their credit, the nurse that saw us had just taken some kind of like, safeguarding, continuing ed, course, where, you know, home educators might be a red flag, right? Obviously, obviously, we weren't. I mean, I'm there to get help, but
Scott Benner 47:51
she thought you got she caught you guys building a bomb in your house or something like, yeah, exactly. She's like, this lady's running a quote. I know it for sure, yeah, for sure. Not crazy, by the way, what, you know, it
Emily 48:04
was a bit weird, and especially because I gone from the GP and again, you know, I logically, I knew there are great healthcare professionals here, but in the moment, because I'm just focusing on get my kids some help Right now, right before she goes into TK, I Google, like I on my phone. I was when we presented to the hospital after dealing with a GP, I literally came in with a UK type one diabetes campaign on my phone, because I thought, what if they think I'm some wacky American? Like there was a moment where I thought, could we, could we make it to New York before she goes into DK, because clearly, no one here knows what I'm talking about, right? And that's fairly irrational, because that, you know, there are, again, are great healthcare professionals. Now she has a fantastic consultant. But in the moment when I hadn't, I didn't have any experience with the NHS, it was pretty stressful, but, but we survived, yeah,
Scott Benner 49:00
but it's a good look into the uncertainty of the situation and how you felt on top of all that. Because, isn't it funny, you had the same thought that your your forefathers had, like, what we there's probably a place that knows better. Let's go there.
Emily 49:13
It's really interesting. Get out of here, yeah, yeah, but
Scott Benner 49:17
a train ride that would have been right, yeah, wow. Okay, so you get this all worked out, she comes home, and what's management like? And, you know, is it needles? Is it pumps? CGM, are available? Like, you get that stuff in any kind of short order
Emily 49:34
when she was diagnosed, the the NHS, or, more specifically, I think it's your called your clinical commissioning group, which is kind of your, where you live in the UK, funds some of the supplies. Okay? So at the time, I think they were funding the Libra, the skin the Libra, that you could scan, right for a lot of kids. And had we pushed to get the Libra, we probably could have gotten that fairly soon, but we left. So we left the hospital MDI, right. And then when we saw our first consultant, they, I think we asked about the Libra, and they were like, Oh well, you know, we'll ask about funding, but we could self fund Dexcom anyway, so we could maybe wait for funding of some sort. But they, they didn't seem very optimistic at the time about funding your our clinical commissioning group funding Dexcom. So I just called Dexcom. The nice thing is, here, Dexcom is just over the counter. We so we paid initially for Dexcom. I want to say it was like 159 pounds a month for all supplies, and at the time, that was cheaper than my friend in the US was paying with her insurance. So, you know, we just wanted to get started on the Dexcom right away. So I think she maybe had the g5 for a little while, and then the g6 came out, I think not too long after she had started on the Dexcom, and then we did MDI for, I think, less than a year, and our first consultant, you'll love this. I I said, you know, we're really interested in the OmniPod. And she said, okay, okay, yeah, we can order that for you. We can, we can do that for you. And I was like, great, amazing. You know, let's, let's get that OmniPod started, right? And so, so months go by between. So here you see the consultant every three months, right? And I went to, so, went to the next appointment. So, how's it? How's it going with the OmniPod? You haven't heard anything? Oh, yeah, yeah, yeah, we're working on that, right? So then, and then emailing the nurse to just saying, you know, how's the consultants promised us the OmniPod. So what do we, you know, what are we doing with that? And then, I think six months later, the I asked about the OmniPod, and or the consultant said, I think when we came to the the into the room, she said, Oh, did you get your port? And I said, Okay, wait, what port are you talking about? Are you talking about the port that you actually put the needle in and inject? She's like, Yeah, we ordered that for you. And I said, Oh no, no, no, no. I've been asking her for the OmniPod a pump for over six months. So are you telling me that that is not what you ordered. And she's like, Oh, and, you know, to her credit, like she could have just been really, she could have been really defensive and denied what she didn't know. But she she was actually really, she was great about it. She's just said, I'm really sorry. I thought I didn't know. I, you know, she didn't know at the time what OmniPod was.
Scott Benner 52:39
What did she order? You an i port? Yeah, yeah. Like that took six months,
Emily 52:45
yeah? Well, I don't even know if it would have to, I mean, we never got the I port. But anyway, so she just said, Look, I'm gonna transfer you to another hospital that actually has, you know, that will, that will do the OmniPod for you. And so then we transferred to a hospital at a different hospital, and yeah, and then we got on omnipot. Shortly after that, it's
Scott Benner 53:08
worth going over that you were standing in front of a healthcare professional telling them that you wanted a tubeless insulin pump called an omnipot, and what they gave you was this thing that sticks on you. It injects once, then you can put a needle inside of it to give yourself insulin, so you don't have to get poked over and over again. I
Emily 53:26
know it's pretty bad, but I think NHS has been underfunded for years and years and years. So you've got healthcare professionals that are, you know, they maybe don't have the time and resources to learn more supplies like this,
Scott Benner 53:41
very, very nice. This is like me calling up, saying I'm buying a car, and I show up and you give me a tricycle, and I go, I mean, it's still transportation, but not nearly what you heard me say, you know, yeah, simply,
Emily 53:53
you get used to a different system here, though. I mean, I have been here eight years, and I think now, you know, waiting for things like, right now Rosie's on the we're waiting for her to come up to get OmniPod five. So we're still using the arrows. Oh, you're on the arrows. No, we're using, yeah, only because I feel like if we switch to dash and loop, because we're looping with arrows, right? If we switch to dash, I'm just a bit worried that we'll get stuck on that and not be able to move to OmniPod five for another four years.
Scott Benner 54:22
That a consideration of being in the UK.
Emily 54:24
I mean, I just don't know about switching like that. I just, I just don't know, but we're, we're on the list for OmniPod five, and, yes, it's weight, yes, it's, yeah, you, you don't really get things right away, like you can sometimes kid in the US, but I'm okay with that. I mean, we don't pay anything now, so all of our supplies are hotter. I can't wait
Scott Benner 54:46
for them to call you one day and tell you that it's already and you show up and they get you a Roomba. You're like, Wait, this is a robot vacuum cleaner. I wanted the omnipot Five, no, but on a chance for you. Oh, how. Hospital. Who knows what that is?
Emily 55:01
Yeah, no, it's much better. I assure you that it's now her consultant now is fantastic. And I mean, every time we go to our appointments, they're just like, you guys are doing great. What do you want? Right? And so we've said, you know, we're ready for OmniPod five. Well,
Scott Benner 55:19
living in this system and having the ups and downs you've had with it. How are you How did you figure out how to, how to help Rosie like, where did all that information come from? From your friend who has type one kid has type one? No,
Emily 55:32
no. I think my friend and her son had such a different experience. I don't I mean, Facebook wasn't even a thing when she, you know, when her kid was younger. I mean, I listened to the podcast fairly early Facebook groups. I went to a sugar surfing workshop fairly early on. I went to what used to be friends for life here, which is now called, see, I think it's called children with diabetes. There's a it's like friends for life events, the UK version. And the thing is, like, though, those friends for life events evidence based lectures for the parents. And so it was a kind of a combination of different things, but I knew that I wasn't going to get a lot of information from, you know, the consultant that didn't know about OmniPod. And in fact, I remember going to one of the appointments fairly early on, after we got the Dexcom and showing the nurse and the consultant her Dexcom graph. And they were like, Oh, she's doing great. And I said, Yeah, but she's, Look, she's, you know, she's eating, and then she's spiking to 14, and sure she's coming back down, but she's spiking to 14. And I remember the nurse saying, oh, yeah, but you know, we all spike after we eat. And I was like, but I don't think not. I just don't think I yeah, I don't think we spiked to 14. Obviously that wasn't right. Do
Scott Benner 56:58
you think they thought that that happens to everybody, like people with and without diabetes, my
Emily 57:03
guess is they probably be a bit more informed. Now, I think maybe access to information is maybe better than it was. You're
Scott Benner 57:11
so polite about this. Are you afraid you're gonna get deported or something? What's going on? You're so like, anytime you're like, Oh no, it's okay. They're better at it now. Or I don't think they meant it, or like, like,
Emily 57:22
I think, I think I have a lot of compassion for NHS employees that, you know, I just think that a lot of folks are doing the best they can with what they have. Again, it has been underfunded for years and years and years, and, you know, even at that I I'm staying because I feel like my kid will never, ever pay for supplies, right? But it's, it's not without problems, and that, that being one of them, you get folks that I think the other problem is at that time, I don't think that pump rep or reps that are pump companies. I don't think they did a fantastic job of getting into the UK market here. I think, you know, we go to the consultant and she'd say, like, well, here we have this Medtronic and and that was kind of like the only option. There may have been one other one, but you could tell, you know, they probably had done some kind of session with a Medtronic rep. And I'm, you know, I'm not testing on Medtronic or anyone else, but I just think they had a kind of a command of the market, or knew how to to get in with consultants here that maybe, at the time, OmniPod wasn't in yet, maybe they definitely weren't in at that clinic,
Scott Benner 58:41
yeah. So, you know, we never really said, you said you had kids early, went back, got an advanced degree. What did you do professionally after that?
Emily 58:52
Oh, so I was physical therapist in the US. Okay,
Scott Benner 58:55
so you have, you have, like, that knowledge of that side of it, like being on the provider side for sure? Yeah, it's not easy either. I've been doing that cold wind series with providers, and you know, they're they're anonymous, and they talk about their jobs and everything. And by the time I get done every one of those conversations, I think there's problems on every side of this issue. And I don't totally, yeah, and I don't see a way to fix any of them. It's, you know, always, you know, at the core human issues, obviously. But I don't think there's any way around it. I think we should all just be happy that things run as well as they do. You know what? I mean, yeah, absolutely, it's interesting. But anyway, it's just, it's you're on their side. I like, as you're going, I don't know if you know that about like, about how you there's nothing wrong. Yes, no, I
Emily 59:44
was really mad. I mean, I was really upset. It took me a long time to get over the GDP. I mean, I just thought he was an idiot. It took me a long, really long time to get it over my hospital experience, and I think part of, part of it was. That I presented to this hospital expecting to be treated like a peer and expected to be listened to, and I was, to an extent, but I just felt like, you know, we left with we stayed in the hospital. So we stayed in an award for like, five days, which is a bit ridiculous, considering, you know, we had some experience with a kid with type one. I think it had someone just in the beginning, come to me and said, You guys are going to be great. This is, you know, you know you're going to be fine. We're going to get you trained, we're going to send you home. I think I would have been fine, but we but because I thought that social services was looking for me. And here's my kid, who, you know, she's always home educated or unschooled, right? And she had this, you know, idyllic childhood in London, but, yeah, we didn't do the normal route. I didn't send her to kindergarten. Or here, it's called reception in here one. But you know, we were living kind of, you know, atypical, yeah, lives compared to other, most other people. Because here definitely, definitely at the time. I mean, you know, home education was very rare. It was really stressful. It took me a long, long time to get over this idea that social services is looking for me, and they're going to, you know, make me send my kid to school, or, you know, investigate me unnecessarily and and I felt really protective of her education. I felt like, you know, what a horrible time to assess someone's knowledge or your home Ed provision, when they're getting a type one diagnosis, when they probably haven't felt well in months, right? I mean, she would, she would wake up in the morning, and for months she was, I mean, she she was a bit irritable, right? And she was irritable with her best friend, and so she'd get up in the morning, and she'd eat breakfast, and then she'd just kind of like, sit with her head resting on her hand, like she was going to fall asleep, and she was having a really hard time learning how to read. And by that time, you know, she was eight years old, and I thought, you know, does she have dyslexia? You know, it just, or, you know, maybe I thought she had, you know, some kind of learning disability, but it didn't present until then, right?
Scott Benner 1:02:26
And then that possibility comes in that they're going to uproot the rest of her life now that you've got a diagnosis, yeah,
Emily 1:02:31
really stressful. And, you know, actually, I don't think she's dyslexic. I think she just had diabetes this whole time. And, you know, poor thing, her sugar has been sitting at, you know, 20 something for probably a long time.
Scott Benner 1:02:43
Yeah, she's lucky. She was upright and moving, let alone thinking and trying to learn. Right, right? Okay, well, I want to kind of finish up with, you know, I know people sign up to do this, like so far in advance that you probably don't remember what you wrote, but you know, when it said, what are some of the themes you'd like to cover. You said parenting, modeling the care with joy transitions to teens, giving kids full autonomy in most aspects of their lives. Now, I think your conversations talked about the the autonomy part a lot, actually, but what did you mean about the rest of it? Like, what about modeling care with joy? What did you mean by that? Yeah,
Emily 1:03:20
I mean, well, Rosie's 14 now, which, I think sometimes this, you know, independent, independence with diabetes, or moving towards independence, happens so fast. And probably when I wrote that, I was doing a lot more for her, but now she's so she's going to school. Now she's, she chose to go to school this year, and I totally support that, you know, whatever she wants to do, and she's doing a lot more of the day to day care, and she's doing great. And I think you know where I was going with that was one thing I really have appreciated about the podcast, is I feel like the way that you have cared for Arden is probably fairly similar to how I've cared for Rosie, and I think, have you been a different parent or advocated at a different way of parenting or and parenting with diabetes? I wouldn't have been a listener, right? But I think you know, managing your child's diabetes with a smile on your face and just doing it, even when it's like the smallest task of, you know, poking their finger or bolus, saying right when the phone, the phone could be right next to them. And even if you say, Oh, hey, could you, you know, could you please bolus for this meal? And they're, you know, they don't want to, or they're busy, or they're, you know, they're playing a video game, or whatever they're doing homework. And so you just do it for them and you and again, you do it with a smile on their on your face. I think, I think it's a great way to manage I think probably outcomes are better that way. And my guess is to get more independent, capable individuals, adults with type one that way.
Scott Benner 1:04:59
Okay, okay, that's really interesting. I I mean, I think the same thing. I think you're, you're gonna do these things anyway, if you moan and groan through it, it's just gonna, it's gonna permeate everything, you know, yeah, yeah. And like, I enjoyed this with you. I appreciate it. It's a different perspective on something. I like that. I like that you and I agree. Like, it's interesting because, as you were talking about, like, you know, letting kids learn at home and on their own paces, I guess all makes a lot of sense to me. Like, when you said the kid came back ahead, not behind, I thought that makes sense to me too. Like, all of this makes sense to me. And then the panic I have from growing up broke, like, sets right in like, well, what if you can't pay for yourself? Like, what if you can't get insurance? Like, what if Arden, like, couldn't get health insurance, like, that kind of stuff. Like, yeah,
Emily 1:05:51
for sure. I mean, that's definitely a real concern in the US, for sure. Yeah, I'm definitely not anti degree. It's more of a just, no,
Scott Benner 1:06:02
you don't come across as anti anything. Yeah, you come across as kind of like, thoughtful, wide open, willing to experience things you're not like, you know, you're not, not worried about 50 years from now, but you're not letting it make your decisions for the moment. I thought it was all really interesting. I just, you know, just interesting. Even further, how different people's perspectives can make them pick that information up and what they think about next, like, once they hear it, like you don't even, yeah, this is really, it's wonderful if we haven't missed anything. I'm gonna say thank you, but I'll ask you here, is there anything we didn't talk about that we
Emily 1:06:42
should have? I can't think of anything nice.
Scott Benner 1:06:45
See how easy this was. Were you? You weren't worried, right?
Emily 1:06:48
Much easier? Yeah, I just didn't want to do the gas station. Voice, or cry, those were my goals. You
Scott Benner 1:06:56
didn't. You almost made me cry with that going to California thing, and I didn't hear a gas station? Voice, yeah, no, I feel like I was pretty good about that. Yeah. I think of that as a local news anchor. Voice, too. I love did they do that in England? Did you do that fake excitement about everything on the news?
Emily 1:07:14
Guess so. Yeah. I mean, I don't watch a lot of I don't either, but that kind of news, yeah,
Scott Benner 1:07:21
the local news just cracks me up. I love it. He's like, Hey, Bobby, I have a great story today about a cat that died. Like, why are you sound so excited the poor cat? Yeah,
Emily 1:07:31
that's true. I don't, I don't, I don't think I've ever seen that here. I guess I haven't really seen, like,
Scott Benner 1:07:35
local I love it. When they try to transition from one thing to another in that same voice. They go from like, this upbeat, stupid thing to something horrific, but they never leave that big, dumb voice they have. It's fantastic. Yeah, yeah, there's this bad, yeah. Everyone should find all right, I'm gonna tell everybody how to find this. There's a Casey or Casey case I'm is not a person. Probably anyone knows anymore, but if you he was a radio disc jockey, really like very popular he was on all over the country. So if you Google Casey, Casey Casey case some dog
Unknown Speaker 1:08:11
death
Scott Benner 1:08:12
dedication, go ahead and YouTube Casey Casey dog death dedication, and you will find audio of this guy trying to lay down ads, and they come out of, like, a birthday celebration into a dedication for a dead dog. And he just flips out in the middle of it. He's just like, how do you expect me to come out of a goddamn upbeat thing into this fcking dog dedicated? He's just like, going crazy anyway, that's uh, that just find that you'll, that'll be a nice five minutes. I don't know if that's like, something I can like, include here, or if it's copyrighted, but holy, take a second because you want to hear a person just like, like, in five seconds. Have an existential like, decision to make, like, Am I really gonna do big happy voice out of a birthday dedication into a dead dog like any just,
Emily 1:09:10
he just loses his it's fantastic, and no one can really blame him for losing it
Scott Benner 1:09:18
as he's doing it. I'm like, he's 100% right. I mean, he sounds like a diva because he's, you know, recording ads for like a, like a, I don't know, a radio station. His life is probably fantastic. But, you know, he's like, he just is, like, how do you expect? It's fantastic. Go find it if you haven't heard it. Okay? Emily, thank you very much. Can you hold on one second for me? Sure. Thanks. Oh. A huge thank you to Eversense CGM for sponsoring this episode of the podcast. Are you tired of having to change your sensor every seven to 14 days with the Eversense CGM? You just replace it once every six months via a simple eight. An office visit, learn more and get started today at ever since cgm.com/juice box, US med sponsored this episode of the juice box podcast. Check them out at us, med.com/juice box, or by calling 888-721-1514, get your free benefits check and get started today with us. Med, a huge thank you to one of today's sponsors, G VO, glucagon. Find out more about G vo hypo pen at G VO, glucagon.com, forward slash juicebox. You spell that, G, V, O, k, e, g, l, U, C, A, G, o, n.com, forward slash juice box. If you're newly diagnosed, check out the bold beginnings series. Find it at juicebox podcast.com, up in the menu in the feature tab of the private Facebook group, or go into the audio app you're listening in right now and search for juicebox podcast, bold beginnings. Juicebox is one word. Juicebox podcast, bold beginnings. This series is perfect for newly diagnosed people. Hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast, the episode you just heard was professionally edited by wrong way recording, wrongwayrecording.com. You.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!