#542 Type 1 and Multiple Myeloma
Susan has had TD1 for 34 years. She also has multiple myeloma, a blood cancer, for 10 years.
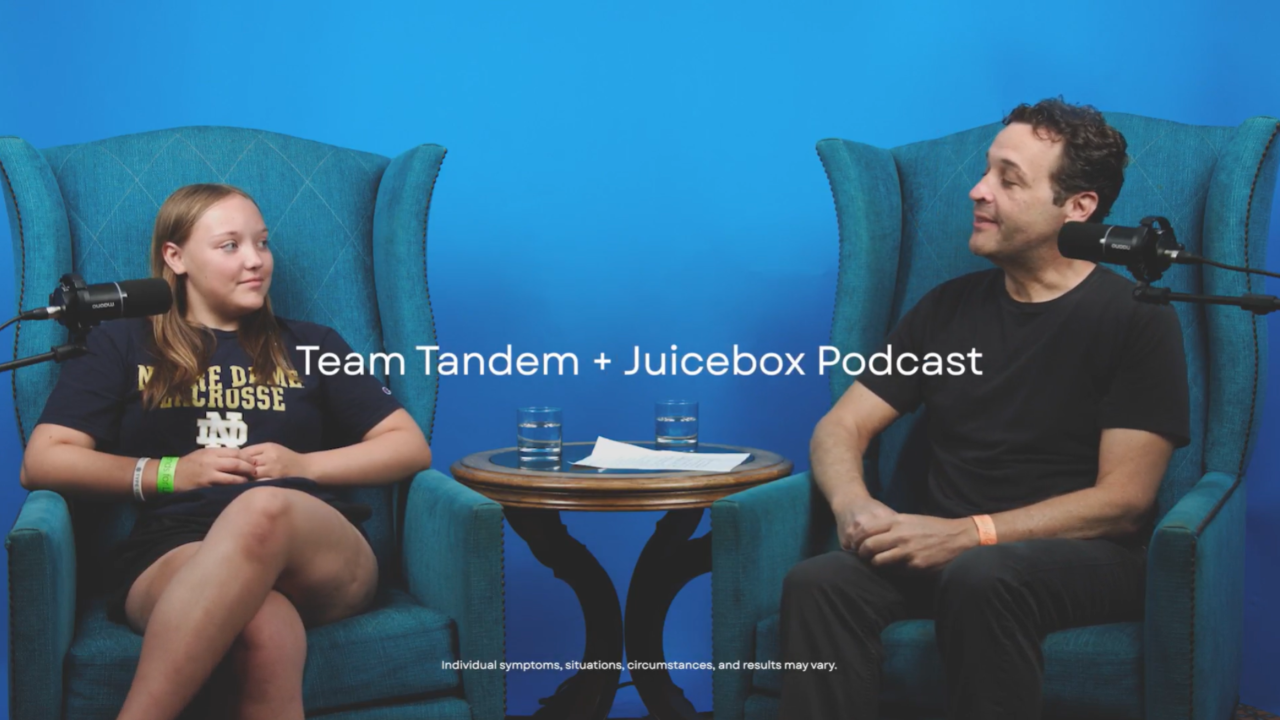
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to Episode 542 of the Juicebox Podcast.
It's often said but worth repeating. People come on this podcast and share very intimate details about their life and their health. And we're all better for it. I just sometimes can't even imagine where they get the strength to do it. And with that in mind today, I bring you Susan, who has type one diabetes and cancer. Susan's story is rather phenomenal, full of Rocky roads, and a lot of hope. Please remember, while you're listening, that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making any changes to your health care plan. We're becoming bold with insulin. If you've heard a lot about the diabetes pro tip episodes from the Juicebox Podcast and you're wondering where they are, they begin at Episode 210 in your podcast player, where you can find an entire list of them at Juicebox Podcast calm or diabetes pro tip.com. Okay, sadolin this is Susan.
Today's episode of The Juicebox Podcast is sponsored by the Omni pod dash. And the Omni pod promise, which I'll tell you about a little bit. But if you want to find out if you're eligible for a free 30 day trial of the Omni pod dash, head now to omnipod.com. forward slash juice box to find out. The podcast is also sponsored by the good people at touched by type one. And you can learn more about them on their Facebook page, their Instagram page, and it touched by type one.org.
Susan Gimilaro 2:05
I'm Susan Gimilaro. I live in New Hampshire. And I've had Type One Diabetes for 34 years. So Susan, I'm gonna ask you
Scott Benner 2:15
to stop because it sounds like someone's getting out a pan to make eggs with behind you that hold on. Okay, did you meet somebody? Did you just go in the other room? And I did. I did. Introduce Okay, so let me try this again. Tell me your name again.
Susan Gimilaro 2:36
Okay, so my name is Susan Gimilaro. And I live in New Hampshire. I've had Type One Diabetes for 34 years, I was first diagnosed as gestational diabetes with a blood sugar of 350. And after birth, my diabetes seemed to disappear for three months. And then came back full force
Scott Benner 3:03
was that. Can I ask Was that your first pregnancy or another? No, that was my first pregnancy. How old were you then? I was 2727. Wow. All right. How many kids do you have total?
Susan Gimilaro 3:16
I have two kids. So I was fully diabetic for my second pregnancy.
Scott Benner 3:23
Fully diabetic. I like that term. So you just you had gestational. And then they tell you Oh to go away after your pregnancy is over. And for three months. You thought they were right. And then they weren't. They weren't hot. We're not calling back with a vengeance. And that's what I want to know about. What What did it look like when it came back?
Susan Gimilaro 3:47
Well, it was funny. I was feeling okay. But then I was out with my sister and I looked up to read a sign in was completely blurry. And I thought that's my, that's diabetes. I'm sure that's diabetes. And sure enough, it was
Scott Benner 4:05
presented that way during pregnancy as well. It did. Yeah. That's a with a three month old baby. Was it heartbreaking?
Susan Gimilaro 4:14
You know, um, I guess I had never had that attitude. Scott. It's been more of these are the cards I'm dealt. So let's play.
Scott Benner 4:24
Yeah. Let's play like that. Okay, so, wow, 34 years ago. I don't even want to try to do the math. I think it'll make me sound silly. But give me a second anyway. Is that the 80s? That was 1987. Look at me. I was gonna say 1980s went with my gut. And that means I'm 62 Ah, there we go. You listen to this podcast.
Susan Gimilaro 4:52
I do. So I had started listening to the podcast I had just come upon it and started listening to it and and that's when I reached out to you to ask if you had ever met someone who had both diabetes and cancer. And because I had not. I had met people with type two diabetes, but but no one with type one.
Scott Benner 5:18
Well, yeah, I was gonna say your, as I was thinking about you getting ready to get this going this morning, I thought, jeez, I'm usually just so like, you're the only person I've ever felt like, I'm sorry that you had to come on the show because it means that you have this, you know, mixture of illnesses that that I don't hear about very often, honestly, not that it doesn't happen. And I'm sure we'll hear from more people that it does, but so let's dig into the diabetes a little bit. And then we'll we'll kind of come full circle at some point. What What did diabetes management look like in 1987?
Susan Gimilaro 5:55
Well, I was on one injection a day and I think it was Lantus. That was it.
Scott Benner 6:05
They just started you with a slow acting. And that's right about the time those things started becoming more popular too. So right. So how and you weren't doing meal insulin injections.
Susan Gimilaro 6:16
I was doing insulin injections. Yes. Just one a day.
Scott Benner 6:21
Right. But not for meals. You were just doing like a background in sauna basil. Just background. Yeah. How long did that last until you had to start shooting for food?
Susan Gimilaro 6:31
Okay, only a couple of years? Only a couple of years. And then I started using regular I think it was back then.
Scott Benner 6:40
No kidding. Isn't it interesting how something can be such a big part of your current life? And with some perspective, standing back 30 some years, you're like, I don't really know, like you don't even like it. I seriously think there's a lesson in that. Not so much. It's not funny that you don't know it's not it's not even expected. I don't I mean, I go back 30 years of my life, you start asking me questions. I don't know the answers to anything either. It's more of an indictment of how maybe unnecessarily? Seriously, we treat everything in the moment. You don't I mean, everything seems so important in the moment. And then you look back on it, you go I don't know, like I took some insulin I don't even remember. But back then it was probably a little more on the president your life. I don't know if that makes sense or not.
Susan Gimilaro 7:31
Yeah, it does make sense. And for me, part of it was that I was determined that diabetes would be part of my life, but would not be my life. And so I i certainly kept track of everything. And initially it was high priority until I became accustomed to giving injections and and back then, of course, it was the three meals a day, two snacks a day. Make sure you have your bedtime snack and make sure you eat right on time. Yeah.
Unknown Speaker 8:08
So that was the regimen I followed. So is it possible then you were using regular and mph and not Lantus? It may have been NPH. Yeah,
Scott Benner 8:18
it's balmy, I think for timing wise. And for the way you're describing using the insulin. I don't think it would have been Lantus. First I think I wonder when lantis was ready. We're going to do the internet during a podcast. People love that.
When was Lantus invented, ah, Lantus was developed by Sanofi in the year 2000. Okay, so I was on NPH then I think this is kind of fascinating. That is fascinating. Yeah. I just think it's like when you said that I thought, well, that can't be right. Because my friend Mike was diagnosed around that time and he was regular on mph for a long time. And you know, a little on him. He didn't switch when faster acting insulins came up, but it's crazy as we're sitting here today, and I'm sure younger people don't understand what I'm saying. It is insane to me that the year 2000 was 21 years ago. I know you know, like it's it's mind boggling really. Like I saw that I thought oh that was recently and it's not myself true. Yeah, that's great. Okay, so you start regular an MPH likely do that for a I guess a while Do you eventually switch to a basil and and mealtime insulin method and was that still injections for you? Or did you ever go to a pump?
Susan Gimilaro 9:49
It was still injections for me for a long time and through my second pregnancy. I which was five years after the first so 1992 I by Ben. Let's see what was I on then? I had to have been on multiple injections then. And I was in very tight control. Okay, during that pregnancy,
Scott Benner 10:14
what did that look like back then? What did they call tight during your second pregnancy?
Susan Gimilaro 10:19
They call tight being right around AD. And, and they were actually not very happy with that and said it was too tight of a control and that, you know, there was a chance that my blood sugar would go low. I wouldn't, I wouldn't feel it. And so they asked me to boost up to like 110.
Scott Benner 10:40
Isn't it funny the other night are doing better blood sugar was 78. I was like, Oh, it's perfect.
Susan Gimilaro 10:46
Yeah, great changes. I know everything changes. And it's interesting, because someone said to me, why are you listening to that podcast? You've had diabetes for 3040 years, you know, what is there to learn? And I just laughed. There's so much still to learn
Scott Benner 11:05
plenty. And it's always changing. And it is, yeah, I, well, I want to whoever told you that, please tell them stop it. I have a life over here too. I'm trying to accomplish things don't don't, you know, heartless for me to find a person to get them to be a listener. Now, like, You're telling me, I got somebody behind the scenes like you don't need to listen. I know, he's cut me a break. Imagine if you were like sitting around watching CSI and someone came up behind you is like, don't watch this. The guy who made CSI would be like, Hey, I totally send my kids to college. What do you do? That's right. So funny. But no, I take your point. There's, it's and I and I love your point, especially man, I say at your age, because it this thing is always going to keep morphing. And I realize there'll be a moment when you don't you don't go with it anymore. Right? And that'll be my expectation is that age, like at some point, you just get to a point where you're like, you know, I don't care what the kids are reading the newspapers on, I get the new york times on paper, like you don't I mean, like at some point, you'll need to hit that spot. But you don't want that to happen when you're in your 40s or your 50s or your you need to keep your 60s. Yeah, you need to keep moving with it. Because I mean, look at what's next algorithm pumps, right? Let me know. Now and I'm imagining you've thought about what that would mean for you. And you're in even your 70s and beyond.
Susan Gimilaro 12:27
Oh, sure. Yeah. Well, I've had two pumps now. And right now I am on the T slim with control IQ. And prior to that I was on the Medtronic pump. Okay, CGM is with both of them.
Scott Benner 12:44
Did you use the 670 G or just were you? It wasn't automated with the Medtronic. How long ago was that? that'll probably answer the question. Oh, that was probably 15 years ago. Yeah. Okay, that's 670 G's so much nowhere, even though it was it's kind of the first algorithm pump. It's it hasn't been that long ago. So you've used one pump. Along with the CGM, with the CGM from Medtronic, did you use the one that people used to refer to as the harpoon? Yes, that was the one. That's how you want your medical devices described to you, right?
Susan Gimilaro 13:23
Oh, that one hurt that really hurt. So I had that for quite some time. And and once we get into the cancer part of the story, I'll tell you what happened. What when I would that CGM Well,
Scott Benner 13:39
okay, let's not happy that was not happy. Yeah. Now, you wouldn't be the only one that's ever said that to me. Um, so. Right. So now you're using control like you right now. You're using an algorithm? I am. Wow. Yeah. With a Dexcom g six. Yes. Yeah. Is it? Is it? What's the question here? You've been? I am not. Just keep in mind as we're talking. I'm not I'm not commenting on your age. It's just you have a different scope and makes it interesting for me to talk about. So yes, that's fine. Yeah. Do you feel like you gotten a rocket ship and went to another planet when you see that? Or?
Susan Gimilaro 14:14
Oh, it's amazing. It's really amazing. It has really changed my diabetes care and my ability to engage more fully in exercising and hiking and just being out and about it's it's been a real blessing for me, it's really been such an improvement in my life. It I have to say, it has taken me a bit to to understand it, to learn about it to get my settings in the correct place. And I have to say I was listening to this podcast that I realized I was having a problem with my basil. And it wasn't my Bolus wasn't my carb ratio, it was my basil. And so thank you for that. And, and since then my, my diabetes has been much better, my control has been much better.
Scott Benner 15:11
That's amazing. Well, so I want you to say a little more about this because earlier, you said, you know, you made a decision early on the diabetes, you know, wasn't going to be your life. But in truth, it sounds like it was limiting some things for you.
Susan Gimilaro 15:28
It was, you know, back in those early days, I'm understanding my blood sugar. And particularly if I was out hiking, it was a real challenge for me. And, you know, I would be like, the the pack meal because I would have so much food in my, my backpack, so much juice in my backpack. And it was, yeah, I had a lot of food and juice with me everywhere I went. And it it did control a part of my life. And, and even in the early days, I didn't tell many people that I have diabetes, you know, it felt like a stigma. And it took me a while to be able to talk openly about it. Without people having pity for me.
Scott Benner 16:24
Do you think they pitted, you ready to just felt like pity do? It felt like pity? Yeah, to me? It really did. I, you try to put yourself in a perspective of now today, where you still meet some if you meet someone who doesn't live around diabetes, they don't understand it in any meaningful way. And this used to come up a lot more on the podcast, I understand that. And I always used to use as the example like, I don't have any perspective on cancer. If you started talking about it, I wouldn't know the first thing about it. I would sound like an idiot if I tried to expound on it. You know, like that kind of thing. But going back 30 some years and saying diabetes, and you're a person your 30s, then right. Right, then that probably be at that probably would have turned you into the lady on the street. We crossed the street when we see her coming, because we don't want to catch diabetes from her, you would think that would be the vibe.
Susan Gimilaro 17:15
Right? And it would be you know, Susan can eat that. So let's not put this in front of her or Susan better not have that. So, so let's not bring that to this party. And and can we even invite her out for dinner because we don't know what she has to eat? And of course, she has to eat at a specific time. And that doesn't seem like a good time for us. was complicated.
Scott Benner 17:37
Yeah, no kidding. It's complicated. And I mean, how long does it take to get to dinner and the Studebaker probably pretty I'm just kidding. That's the 50. That that's, that's really something that I've thought of thought about intellectually, but never heard anybody say out loud before. And I get what you're saying that you might keep it to yourself, but different world now you're saying it's complete? Yes. Yeah. How much of management being different changes how you interact with people like because that's the only real thing. It's changed besides your perspective and having it for a while. But if you were still, if insulin had never progressed, if technology didn't exist, and you were still like regular an MPH right now or or, you know, even you know, shooting, you know, Lantus and guessing at your meals and testing the hope, where you fall in line, you might still feel like that today. Do you think that's a fair statement?
Susan Gimilaro 18:37
I think that's a fair statement. I think that's a fair statement.
Unknown Speaker 18:41
Yeah.
Susan Gimilaro 18:42
Because, you know, it's still be the person who's got the bag of food and the bottles of juice and the glucose tabs and, you know,
Scott Benner 18:51
let's not be the woman without her because it was out. Yeah, that really is the other side of it, isn't it that people it is don't want to feel like they're around sick people. Right? Right. Not everybody but but you're gonna bump into someone that has that feeling.
Susan Gimilaro 19:09
It is and it's not just that feeling. It's also the the sense of, you know, we don't want to be with her because she's just too complicated. You know, there's too much that we have to be aware of, you know, to be with her. And that's that really was what prevented me in the early days.
Scott Benner 19:32
So I have to say much I have two versions around that. What is hiding it look like? Like, how do you pull that off? How do you go to dinner without being the complicated the complication for them?
Susan Gimilaro 19:46
Oh, I ended up with high blood sugar. That's what I was gonna because I'm not going to go to dinner with a low blood sugar.
Scott Benner 19:51
So you ignore your your health to avoid a low right because they can see it. But they can't see a high. Correct. Gotcha. Right? They do anything to avoid alone? Yeah, well, that just made me sad. Susan, early in the morning, don't kill me like this. I just put a tape, I just I swear to you, if sadness felt like something, it just ran from the top of my head to the top of my toes.
Susan Gimilaro 20:21
Yeah, those were hard days. They were hard days. But, you know, I didn't have all the knowledge either. And maybe the diabetes is, you know, community didn't have enough knowledge to share with me as well, because I did not get much guidance. But again, I say, Did I not get enough guidance? Or was that the knowledge that was there? You're going to eat three times a day, you're going to have your snacks and everything's going to stay on time?
Scott Benner 20:53
So yeah, I think the I think the ladder. I mean, I wasn't there for that, aside from having a friend who had type one, but we never talked about it. And you know, I've said before, like he was just the guy like you when he was driving you all like the whoever's in the front seat with him would just pay a little extra attention. It was almost like you were driving to eat because and you never knew why, like, just sometimes Mike didn't make tight turns, you know what I mean? You know, sometimes my guts thoroughly Mike's sometimes he got silly, and, you know, he or he'd get very insistent that he would need to eat. And I look back now. And Gosh, I really wish that I knew then what I know now, because I wonder how much differently his life would have been. But I think it makes the point that you're saying, which is I've been digging into this in a couple of recent episodes. That's all there was. And it means and it was so much better than prior. I do think we forget that. I mean, insulin is, is even discovered in the in the early 20s. I think it's 21. I think this is the 100 year anniversary in 2000. Right? So So prior to 20 or 1921. If I have the net if I have the year right. Prior to that you my daughter, my friend, Mike, pretty much everyone listening to this just just gets diabetes, they look up at the mall one day, their visions blurry and then in a couple of weeks or months, they're gone. Right, right. And so so being able to inject the thing twice a day, and to live back then what were they hoping for 40 or 50 years? Do you remember what they told you?
touched by type one is a great organization. That's just me telling you that from my heart, you can choose to believe me or not. Or you can check it out, touched by type one.org. Well see here an ad where people just say we just want you to check us out. If there's no Have you ever noticed about the touch by type one ad there's no big sell. They're not asking you for anything. They just say come over and check us out. It's worth doing trust me touched by type one.org. We're also on Facebook and Instagram. music as well.
Now let's find out about that on the pod promise, shall we? It's super simple. Okay, super simple. Here it is. The Omni pod promise says this. You do not need to wait for the next big thing from Omni pod. Because with the Omni pod promise, you can upgrade to Omni pods latest technologies for no additional cost as soon as they're available to you and covered by your insurance terms and conditions apply. But you can find out everything you need to know at Omni pod.com forward slash juice box. Let me break that down again. in smaller words. If there's something you're waiting for, like you think, Oh on the pods probably gonna come out with something else one day, I'll wait for that. Because I don't want to get stuck with the thing I have now. Which by the way you wouldn't be getting stuck with because it would be amazing. But that's not the point. That's how you're thinking. You don't need to think like that. The Minami pod promise isn't a thing. It's not a piece of paper you hold you don't have to get them to make you the promise it just exists. So like if you went to alibaba.com forward slash juice box right now. And you found out let's say that you were eligible for a free 30 day supply of the Omni pod dash, then you would get that you would use the dash for 30 days for free. No, nothing to do except use the free insulin pump. And then let's say a number of weeks after that, or months after that, or whenever something else happened. I'll be like oh look, we made a thing. You're like oh, I want the thing. I want the new thing but I just got the dash. You can have the new thing on the pod promise. Am I being clear? I feel like I am on the pod.com forward slash juicebox. Don't wait. Do it now. There are links in the show notes to all of the advertisers and links at Juicebox Podcast comm in case you can't remember the pod comm forward slash juicebox or touched by type one.org. What were they hoping for 40 or 50 years? Do you remember what they told you? Oh, they
Susan Gimilaro 25:27
told me back then they wanted me to last 25 years, they said that was the that was the golden number. And a lot of people were not making it. 25 years. So for you, that would have been right up
Scott Benner 25:41
just around 60 years old. Am I right? You were 34 at the time?
Susan Gimilaro 25:47
Um, let's see. No, I've had her foot. No, I have it for 34 years. I've had it for 34 years. So what would 25 have been 27 and 2552? Well, Susan, someone stood in the doctor's office when you were a young mother in your mid 20s. And told you, if you're lucky, you'll live to 50. Yes. Okay. Yeah. Yeah.
Yeah. And, you know, I kept aiming for that 25 years, 25 years, because the, the diabetes organization that where I received my care, they kept pushing for that 25. And then you would get this medal, and there'd be a ceremony. And so when I got to 25 years, I said, hey, I've made it 25 years. You know, we should have a ceremony, you know, I want to apply for, for my medal. And the doctor said, 25 years is no big deal anymore.
Scott Benner 26:46
Like, wow, I wish someone would have come to me and updated me.
Susan Gimilaro 26:49
Yeah, yeah. Really. And, and I, I felt a little cheated, because I wanted to say, you know, what, 25 years ago, when I was first diagnosed, it was a big deal. And I made it through Yeah, I made it through all those 25 years in good health.
Scott Benner 27:07
I don't have a metal to give you but I give you I'll give you a slap on the wrist and say way to go. That's really something else, you know, virtually, of course, I think a person, we'd have a whole problem. But I'm here. Imagine if I was a diabetes coach. And I went that way. I was like, Hey, good job. But but good job. I mean, honestly, what are some of the things that you did over those 25 years to make it?
Susan Gimilaro 27:34
Well, I really tried to learn as much as I could about diabetes. After you know, when I was first diagnosed, I was pregnant, and I was just determined to do what I could for the health of my baby through both pregnancies, and then, you know, I had this I'm sick to death of having diabetes, I'm going to do what I want. And that lasted for about a week. And and then I pulled myself together just tried to stay on that regimented life as long as I could. And I eventually I'm trying to think whether I went to the pump first, or whether I went to the pen first. I think I went to the gym for us. I took a lot of classes to to understand about diabetes, because I knew the knowledge was changing. I went to a couple of diabetes fairs and talk with different manufacturers. And so just tried to gather as much as I could. Yeah. And stay active, really stay active.
Scott Benner 28:43
I love it. How people have had diabetes for longer save the pump. Like it's a mystical thing that exists off in the distance. I got the pump, pump. It's very common. It's very common phrasing, but I'm always I'm always I'm interested by it like that. It seemed like this, this sort of mystical thing that was out in the future. And if you were lucky, you could ascend to it and maybe put a pump.
Susan Gimilaro 29:09
Yo, yes, yes. Right. And, you know, I remember going to a couple of meetings about about the heat pump and learning so much from other people who were there who were already either wearing a pump or or in we're getting their CGM or or they are to cheerlead us and, you know, back then, the trick was to cut a hole in the pocket in the pockets of your pants, so that you could thread your your pump through your pants, tubing, and they had the tubing through the pants because there was remember there being holsters. I'm sure there were but they may have been gigantic things. And for me, that was the Biggest trick, and I started cutting holes and and all of my pants and my shorts and my skirts and so that I could just thread it right through.
Scott Benner 30:09
Yeah. So you could have the magic of the pump. Right. So the things that you did to make it You said, you know, you tried to learn about diabetes. But earlier you said to that there might not have been a lot of information, I think we've picked through the idea that maybe information just didn't exist, which is why it wasn't there. It was just a lot of people who had been told, hey, if you're lucky, you're going to live 25 more years since your diagnosis. So right, you know, and I want people to hear too that Artem was diagnosed in 2006. And it wasn't, she's gonna live a certain amount of time. The message then was, you shouldn't see any significant long term problems from diabetes for at least 30 years. And I remember thinking, but she's to me, you mean, when she's 32? She's gonna have significant problems. And that was 2006 16. That's only 15 out why am I doing the math, she's gonna have diabetes 15 years this summer. So that was 15 years ago, they were still talking about, like, Oh, you've got 30 good years before your eyes explode. You don't mean like, and it was really the vibe they were giving you they never used the words, right? They never said the words, but they, they would never say like, have vision problems or you know, etc, etc. They just be like, check your feet. You know, there's a lot of check your feet, you know, a lot of check your feet. Yes. And, but that's even just 15 years ago. And so what a great leap is that? I know, this sounds like it's not a great leap. But it's a great leap. If you if you if you step back far enough and take a macro enough view. Susan was told, you're gonna die in 25 years. My daughter was just told, hey, we're just going to probably take a couple of your toes and 30 years like it's, it's, it's a big leap. And now today, no one would say any of that to you when you were diagnosed. Right?
Susan Gimilaro 32:10
Right. And I tell you, when I first started going for treatment, and my appointments, I would walk into the clinic, the where I have treatment is really a well known Diabetes Center. And I'd go and NFB amputees there. And I thought, Oh my God, if I don't get this under control, that's me. Yeah, they're amputees or people who are blind. You know that that can't be my future. No.
Scott Benner 32:42
Did you happen to hear Sophia? Who lives in Russia recently on the show? She's 14? Oh, I started listening to that. Okay. I haven't finished it at some point. She says, because I said to her, like, how did you figure out all this on your own? Like, you're 14? You know, she said that all she could think about when somebody told her she had diabetes, was that she was going to lose a limb. That's what's all she could think about. And that made her dive into the internet to figure out how to manage your diabetes, you didn't have the internet to dive into back then. Limited, it really is. You know, I was I just recorded the 500th episode of the podcast, which is just really me talking for like a half an hour about what the podcast has been so far. And I came to realize while I was while I was talking, basically talking to myself, but I just imagine all of you, which makes it not seem weird while I'm doing it. But the years and years ago, when I first started writing a blog, I used to pitch to companies all the time, that there should be like a depot, a hub, and you should go out and get all the best diabetes bloggers, and collect their writings in one place. Because you're you're making it too difficult for people to find their voices is how I set it. No one ever listened to me. Okay, like Susan. I pitch stuff in meetings, and they're like, Ah, you're not hearing it. And I never mind when I realized why I was saying it the other night recording that that's what I did with the podcast, except it's not bloggers, it's people with diabetes, right? And I'm bringing them all together in one place so that somebody can easily find their stories. I didn't even realize that. I know that sounds weird. You'd think that might be something I realized, but but it's ease of getting to the information. That's always the most important part. You know, people can talk all they want about like, Oh, we have a program to tell you about this or that. It's all boil. It doesn't matter if some company launches a program about the importance of some aspect of diabetes, it doesn't matter because they're not going to actually reach anybody with it. If you can't find it, you don't have time to find it, you need to have everything in a place. So that's, I think what you lacked back then.
Susan Gimilaro 35:08
Yeah, I mean, I think, you know, when I think about your podcast, you you provide us with so much information. But and then on the your Facebook page as well, the bold with insulin it is where we're hearing from real people who have real lives and real experiences with diabetes. So, you know, we feel like we're not an anomaly someone else's, is running high blood sugars for unknown reasons, or someone else who doesn't have their basil set correctly. And, you know, you don't feel alone, when when you're connected with other people who are on the podcast or Facebook,
Scott Benner 35:53
I appreciate that. And I'll tell you the other thing. I said this again, on the in the fight, I don't love that I'm on Facebook, I am not a person. It's like Facebook's amazing. It's just, it does this exact thing. So well. It allows, it allows people to have a private place to talk about things. And the what I what I like about it. People might people from the outside might not see it the way I see it, right, I see it as a tool for all of you to be able to talk to each other. Sometimes you can be there and have this feeling you see it on Facebook all the time. Like somebody just asked that question were searched, the pot is searched the thing like don't be lazy. I'm like, No, no, that's wrong. You want to encourage people to keep saying even if it's the same thing over and over again, wait, what you don't realize is even if you saw somebody say this thing twice or three times, and it starts feeling repetitive to you, there are 1000s of people who don't comment, who are seeing it for the first time. And so diabetes really isn't an unending number of problems to talk about. I mean, there's a lot of variables, right, but there isn't an end to them at some point. And so you need them to keep being turned around. Like you have to turn it up, like if they go down to the bottom and pull it up and bring it back to the topic. And because someone new is there to see it again and again. And someone else has ascended to a spot where they understand it well enough to answer you. So you want to encourage those conversations like So anybody who says, you know, search the forum, don't ask questions that have been asked already, you are missing the exact reason why it's so valuable. That's right. Keep being sad, and it needs to keep happening. Because you might have diabetes now. And you might have gotten over the shock or gotten over this or learned how to Pre-Bolus to whatever you figured out how to do and good for you. But today is somebody else's first day of having it today is somebody else's first day of having the courage to try to find out more about it, to speak up. It's somebody's first day for so many different steps along the journey. And you have to let it keep happening. I'm very happy to be the person or a person who will has a space where that happens. And I think and we all appreciate it. We really do that. That's it to me, it's just, you know, it's me saying like, oh, See, I told you I want it like there is a small part of me that wants to go back in time to all those meetings ago. I told you people to do this. But all right, he didn't do it. I did it instead. But I had to wait for the technology to allow me to do it. Right, because I wrote I wrote a blog and the blog was great, but it still doesn't work the way the podcast works, the podcast ranks better. And so, you know, to be honest, it's a full circle idea of what you talked about about learning about diabetes. I had to wait for the technology to share diabetes the right way. Right. I think this is a sweet spot to I mean, honestly. no judgment. Again. You're a woman in your 60s listening to a podcast that probably shocked you the first time you did that I'd imagine.
Susan Gimilaro 39:09
Well, you know, I really didn't think I would find. Well. You know, what really shocked me is a few minutes ago when you said Oh, when you were diagnosed 34 years ago, there was no internet thinking. You're right. There was no internet. There was no internet. So there was no way to learn. The information that we we have today there there was no Facebook for us to connect and podcast. You're right there. It didn't exist. So so times certainly have changed for me. And listening to a diabetes podcast was not something I would think I would be doing. I didn't think there'd be one out there
Scott Benner 39:55
who would even know what a podcast was probably you know why they call them podcasts. I do not Because the first time they were available to people was through the the apple book was called iPod. That's amazing. I couldn't think of the I, it was the first time you were available. podcasts were available. It was audio that people would record from their homes that was available through an iPod and they became podcasts because you were casting your voice over the iPod. not know that. Yeah, that's great. Now I think iPods don't even exist. Or maybe they do. But I don't even know. Because everyone even now. But in 2007 when I launched my blog, I learned later that I think it was maybe the fourth diabetes blog in the world. Like, you hear a blog now and you think like oh, blog yet everyone has a blog. My dog has a blog. You don't I mean, but right. And there are people whose cats have Instagram, so I'm just saying like it. But back then that was not a real thing. No, no. My link to my my link to my blog. Was http colon forward slash forward slash www died. I want to say it was max something that I forget even I used to use this program iWeb It was iweb.com forward slash and then I swear to you, maybe 60 characters and letters jumbled up afterwards? Oh, my gosh. Times have changed. Yes. Yeah, it was. It that's how long ago it was. And so I get excited thinking about, like, I don't know what comes next. Right. Like, I don't know what, better than podcasting. Right? If blogging was better than you, you know, at the, at the library. And and podcasting is better than blogging, like, I don't know, what comes next. Or this may be is just kind of the pinnacle of of being able to talk right into people's ears. But I'm committed to keeping up with it. Because there's more to learn that we don't even understand exists yet. That's right, you know, that's right. I can't wait to find out what that is. I can't I am. I describe the podcast, in that 500th episode, as it's basically a time capsule, I'm leaving behind for my daughter that other people get to benefit from, you know, so I just hope one day that she listens through it as an adult. And can can accomplish what you did. And even maybe what I did, and what people listening if done without having to go through all of the the harshness that I had to go through to figure it out. Right, he's you know, so me. Alright, Susan. So in this term, tumultuous story, where the hell do you get cancer in this timeline?
Susan Gimilaro 42:56
Well, it was, it was quite a shocker to me, I have to say, and, and, and this is when I was diagnosed, thanks to my diabetes ophthalmologist, which is kind of strange. I had been, I had been writing a grant my first large ish kind of large grant large for me. And once I was to start a new project, once I was finished with it, I was exhausted, I was so tired. And, and then the eyes again, my eyes were really sensitive to light to the point where I would have my sunglasses on my nightstand and put them up, put them on when I got out of bed until my eyes adjusted. So I said, Well, this, I get to see my ophthalmologist. And I walked in to her office, and she said, there's nothing wrong with your eyes. You know, she did all the testing. She said, there's nothing wrong with your eyes, but you look awful. And I said, Ah, it's a makeup free day. And she said, it's not that kind of awful. You need to be seen by your doctor right away. Okay, so the next day, I went to see my doctor and walked in and the nurse said, You look awful. Like, I've heard
Scott Benner 44:31
you everyone. Everyone's saying it.
Susan Gimilaro 44:34
Yeah. And then the doctor said the same thing. And he's like, what's up, I said, I'm tired. I'm a little bit sluggish on the treadmill, just, you know, just tired. And so he sent me off for blood work. And at the end of the day, he called and said your red blood cells are Below, well below normal your white blood cells are well below normal and the emergency room is waiting. You need an immediate transfusion. Like, okay, all right, so off to the emergency room, my husband and I went and my sister joined us. And four days later I was out of the hospital after having five transfusions and a bone marrow biopsy. The following week, I was diagnosed with multiple myeloma, which is, as of now in uncurable blood cancer. So, how long ago was this? 10 years ago? Okay, 10 years ago, and I don't know what I would have done if it hadn't been for going to see my diabetes. ophthalmologist, I don't know what would have happened.
Scott Benner 45:57
Could your have blood values have gotten so far off that it impacted you? Could it have killed you at that point? Like, where do you think you would have just passed out and somebody would have shuffled you off to the hospital?
Susan Gimilaro 46:09
Yeah, I think that's what would have happened. The doctor had said to me, I don't know how you're at the gym, I don't know how you're on the treadmill, you're all of your blood cells are so low. So I, I got the diagnosis. And at that time, they gave me three to five years to live. And I took the I took my diabetes playbook out and said, Well, you know, I have diabetes, that's part of my life. Now I have cancer, that's part of my life, and neither of them will be my life. I'm just going to move forward. And if only it were that simple
Scott Benner 46:57
way, you can say it. It's like, you know what I'm gonna do, I'm gonna cut out some carbs. And I'm gonna drop 10 pounds. And then like, a week later, you're like, I'm eating potato chips. I don't know what just happened. So yeah, I mean, saying it's one thing, right? And then right, but you're you're saying something that you feel like you don't have real control over. Is that right? Yeah. I'm sure attitude.
Susan Gimilaro 47:20
Well, of course. Yeah. I mean, I have a very positive attitude. I mean, they gave me three to five years. And here it is. 10 years, you know. But my first Rude Awakening was when they started me on treatment, which was the following week, and part of the treatment was Dexcom. methadone. that lovely steroid that puts your blood sugar's through the roof. Oh,
Scott Benner 47:46
yeah. So yeah. So now you're fighting? does it become difficult to focus on everything you have to focus on?
Susan Gimilaro 47:57
Again, I really think that's where my, all my years with diabetes really helped me. It's like, this is your life, you get into a routine, you know, what you need to do, and you just got to move forward with it. So but it was always little hurdles that I had to, to overcome. So the dexamethasone was needed. And so we had to adjust my, my insulin at that point, and and I was on a pump, then. I was on a pump. I was on a pump, then.
Scott Benner 48:36
How much do you earn? How much more did you have to go to? Like, what was your percentage increase? Oh, like 50%? Wow. Yeah. That's almost like being pregnant at that. Right? Yeah. Yeah.
Susan Gimilaro 48:50
The dex was only once a week for three weeks, and then off for a week. So it was just a day or two where I really had to adjust my insulin. And then I would settle back down.
Scott Benner 49:05
What was that treatment? Like? Was it hard on you physically?
Susan Gimilaro 49:09
Besides actually it? It was not? And oh, and I have to tell you, so as I said, I had been really tired because I had written this grant. So the morning I was diagnosed with multiple myeloma the afternoon I got the award letter for the grant
Scott Benner 49:28
which I accepted just all anti climatic I would imagine like Oh, great, good. So but but Susan, you don't do that thing. Do you? You from a different generation, like you don't look at the grant coming in and go well, if it wasn't for my bad health news, I'd be able to enjoy this. Like you don't feel that way about things.
Susan Gimilaro 49:51
No, I don't know. it for me. It was kind of the yin and yang that day. I you know, I got this terrible diagnosis and Morning, but then I had this great news in the afternoon. And I wonder how I would have responded if I got the great news in the morning and the bad news in the afternoon?
Scott Benner 50:12
Yeah, I don't know, you would have been a little higher coming into the other thing, but also, look, I don't, I don't have a first hand knowledge of, of cancer. But I have had my, my iron be so low that a doctor said to me, I don't understand how you're standing. Right? You know, so I do get that idea of, I think it's fascinating how your body can just, like almost will itself to keep going. Right? You don't, you don't really realize it's happening. You have this decline in function. And the people around you can see it, but you can't, because your body is just like, stay alive, stay alive, stay alive, right going, which, which should be something that people who who have higher blood sugars and say, Oh, I feel fine. That's what you need. That's one of the things you need to realize is that whether you feel fine or not, you're not fine. That's your body just going stay alive, stay alive, stay alive, like your body when your blood sugar's 250. All the time, your body is basically saying to itself, let's just try to keep going until hopefully this gets fixed, or we fall over one or the other. And it's fascinating how how the human body can do that. It is at no point did you think, Wow, they are really trying to get me off this planet, like the one guy told me 25 years now this one's telling me three to five, like people are like, Did that ever occur to you?
Susan Gimilaro 51:38
Um, you know, I really am a very positive and optimistic person. And
Scott Benner 51:45
not Hi, Susan Are you know,
Susan Gimilaro 51:49
when I was diagnosed, you know, he's, the doctor said to me, the oncologist said, Well, why don't you call them and think about it for a couple of weeks? to think about, you know, I'll start treatment this week. You know, I have nothing to think about. I want to live and I've got a life ahead of me. And so it was, it was quite a journey. You know, I had a couple of infections, one for my CGM. You know, my white blood cells were low. And, and I thought I had cleaned by my sight, very well put the CGM and ended up with a massive infection and in the hospital for eight days and a small surgery because the infection was so bad. You know, I didn't anticipate that. And
Scott Benner 52:40
your body wasn't up for fighting. Even small bikes are the way you put your CGM on a million times that right. Yeah, I see. Okay. No, no, my
Susan Gimilaro 52:49
white blood count was low enough that even when I went in the hospital, I would have an isolated room. Isolated room because the fear of infection was was great. How did
Scott Benner 53:02
you handle COVID?
Susan Gimilaro 53:05
Well, you know, it was, the isolation was hard. But between having diabetes for so long, and having cancer, for then, at nine years, you know, I had already learned that I'm never going to touch a doorknob in winter to begin with, you know, I'd always use my sweater that you know, the sleeve of my sweater, or, you know, so I had some of those habits already in place. Because I knew, you know, with having to, you know, serious illnesses, I really had to manage my infection control, and I always would come right in the house, wash my hands first thing, and so
Scott Benner 53:51
it's okay, so some of those projects are teaches you how to open a doorknob with your butt cheeks, I guess, basically.
Susan Gimilaro 53:56
That's right. Yeah, I will say I did have a moment. I had about a week where I was pretty frightened by COVID. Because I thought, you know, you look around, people are catching COVID people are dying, they're over 60. They have to, they have one or two illnesses. And I thought, if I catch it, then I may die. I'm not going to die because I've diabetes and I'm not going to die because I have cancer. But if I catch COVID I might die. Yeah. And so so that was quite sobering. It took me about a week to pull myself out of that and saying, you know, you know what to do. You know what you need to do keep your blood sugar in good control. Keep away from germs and railings.
Scott Benner 54:48
Yeah, don't look Rawlings, right. And so, before we move on for that, I just want to Did you get vaccinated? I did. You did. Okay. I did, too. Honestly, I didn't think that I wasn't anywhere near the situation you were in, I was still like, I'm doing it. Also, my wife worked on one of the vaccines for, you know, a year and a half in my dining room. So it almost felt like, it would have been rude. Sleeping on our dining room table, I felt like, you know, it would be like, if it took me a year and a half to make dinner and everybody was like, No, I'm okay. So, yeah. But anyway, um, well, I'm glad. Are you moving around more freely now with a vaccine? Like feeling better about that? Yeah,
Susan Gimilaro 55:34
I am, I feel better about that. Occasionally, if I'm going to be in a big crowd, I'll still put a mask on. And I think some of the, the, the habits that I've always had will continue like washing, you know, wiping down a shopping cart. Before I go in a store. I was doing that pre COVID.
Scott Benner 55:56
And I'll continue doing that. Just continue it. I have to say, I know you hear people say it all the time. But I really feel it. I have not been sick. And I think maybe one time in a year and a half, like, Yeah, I thought maybe out maybe I will do the same thing. Like if I'm going to the Home Depot in the middle of flu season, maybe I'll just be like, Huh, pop a little mask on and jump in. You know, I mean, other cultures do it. Without hesitation. Right? Right. You know, if you're sick, you don't go outside without a mask on in Japan or China. That's a, it would be considered to be like unthinkable there. So yeah, no, I mean, something got to come to this understanding of other stuff. Well, well, so. So you've been living with, you've been living with the diabetes that was supposed to kill you. 14 years ago, for 30 years, you've, you've now been living with cancer for 10 years that they told you three to five. And I don't want to ask you some trait like does everyday feel like a gift thing, but I do want to know what it's like to wake up every day, when you've been told these things.
Susan Gimilaro 57:09
You know, I wake up every day saying today is gonna be a good day. I honestly do. I read this book called tiny habits. And that's one of the first habits they've tried to teach is wake up every day saying today is gonna be a good day. And it is,
Scott Benner 57:26
I'm in, you know, a totally optimistic person. I'm very hopeful. But I'm also I'm also not Pollyanna. So I see what's wrong with the world. And I know what and I know where the problems are. And I know where the fights are in the struggles are. But I, I swear to you, I wake up every day like Groundhog Day. I'm just like, let's go get it. By now, has anyone not seen if you've not seen the movie? Groundhog Day, please. When this episode is over, go watch Groundhog Day. But yes, but but I wake up every day like, Okay, here we go. And if something bad happens, then I get in front of it. And if it doesn't, then I just do the things I was meant to do that day or the things that I would like to do or whatever we had a we had like tile replaced in a shower. And the the person we had do it really botched it. And I had my phone in my hand to call them and be like, Hey, get back here and fix this. And I was like, yeah, I'll do it. Yeah, and I just got down on the floor, and I fixed it. And it ate up about the next 18 hours of my life. Hmm. And then I just went back to doing the other stuff I supposed to do, right? Like I just I was like, Alright, well, now the floor in the shower needs to be fixed. And, and. And I just think of it. That's how I think of life. like everything's not going to be perfect. When it's not perfect. You fix it and move forward. And it sounds like you do the same thing except with bigger. I mean, you know, obviously I'd rather fix the shower floor than get bone cancer, but I'm just saying like, you have the same attitude about it. What did you What did you do for a living? You talked about writing a grant? Are you still working? or What did you
Susan Gimilaro 59:09
do? I am still working? I'm an education consultant here in New Hampshire. Okay.
Scott Benner 59:15
What kind of college did you have for that? I have a master's degree from Cornell. Ah, see, you're super smart system. I still have a lot to learn. We all have a lot to learn. But you don't get to Cornell by mistake. No, True. True. I sent the application to the wrong place. And I have a message that you've never heard anybody tell that story before. So how much of I'm trying to figure out where your perspective comes from. So was it how you were raised? Was it like where do you get that kind of thoughtful perspective, from Did something happen in your past, like, I know, for me, I grew up really broke, and then my dad left. And, and, and bad things that usually fell, people keep happening. And I find that that falls under the category of, you know, you know, I don't know how to eat, how do you hardened steel like you beat on it or something like that, like I find that like that falls into there did something like that happened to you in the past?
Susan Gimilaro 1:00:24
I don't think so. I think it really comes partly from maybe partly from prayer, but I think more from mindfulness and meditation, and trying to, to take in the knowledge that, you know, today is here, you know, and whatever, there's this great poem that says, you know, whatever is put on your doorstep, you know, whether it's happy feelings, or bad feelings, accepted as a guest, you know, it's come to, if it's something bad, it's come to clear you out for something good, that's going to, to follow. And so that's, and I have that posted in my, in my home. And in my office, it's just my perspective, it's life is, every minute is passes so quickly, and you just take it head on. And
Scott Benner 1:01:29
so there's an ebb and a flow to life, and you expect both,
Susan Gimilaro 1:01:32
there is an ebb and flow to life, it's not always going to be great. And even though you know, I've talked about diabetes and cancer, it doesn't mean that I go into my doctor's office for my labs feeling like nothing awful is going to happen. I do get nervous. I do get nervous when I go in for my exams, because, and for my labs, you know, I've had both of these illnesses for so long. I'm lucky I have no neuropathy at all. And I really, to be honest, I have very few side effects from either the diabetes or the cancer. And I know I'm very fortunate for that. But you know, the shoe can fall, the other shoe can fall, I just choose not to think about that every minute of every day. Yeah,
Scott Benner 1:02:26
good for you. It feels to me like you're, you're on the beach, at the ocean and you want to look at the surf, and you you walk down to the water and enjoy it. But you know, it's going to come crashing in and you don't stand there defiantly you back up, and you go, Okay, let me let me ride this out, right, the way this is going to go next. And then when goes back out to sea, I'll walk back down to the edge again and stare out there for a while longer. Yeah, yeah,
Susan Gimilaro 1:02:53
that's a good thing. So I mean, I think it's important that we accept whatever feelings we come our way, whether there are happy feelings or, or sad feelings or grieving feelings, we accept them, we acknowledge them. And then you know, let them ride right out as long as they need to, and then let go and move on to the next day.
Scott Benner 1:03:15
So when you listen to me say, get your basil, right, have a strong foundation, understand how insulin works Pre-Bolus understand how food impacts and then stay flexible. That's why all that made a lot of sense to you when you heard it.
Susan Gimilaro 1:03:31
Totally, totally in it. You know that basil? The couple of episodes on basil really changed how I manage my diabetes now. You know, it really changed it. And yeah, you have to be flexible and everything that that I hear on the podcast from your, from you from your guests from Jenny, just brings true to me.
Scott Benner 1:03:57
Jenny's gonna love to listen to this episode. Jenny. Are you listening? Hi. She does. So hi, Jenny. She's gonna be thrilled to hear that. And I am as well. Yeah, I have to tell you, I it was Father's Day recently. And I I wrote this little post on my private facebook page about what I thought being like a good dad was and I looked back at it and I thought I just told people, I just basically said Get your basil right Pre-Bolus understood. What I said was like, lay a strong foundation. You know, try to stay ahead of problems. I said, you know, you know, like that kind of stuff. And when I read it back to myself, I thought I just said basil Pre-Bolus glycemic index, they flex. I just said it about and I was like wow. And I dug through it. I was like that's just how I see life. Like the way I talk about diabetes, it's just the way I see everything. And it's just a plot and and maybe there are like simple truths about Psychologically come existences, I don't know if that's that there's maybe a better word in there for that. But there are, there are simple things that you can do that make a lot of things better and easier and, and and more fulfilling. You just have to have to come at them from the right perspective, I guess.
Susan Gimilaro 1:05:22
I agree. And I think part of it, you know, some people have said to me, Well, you know, haven't you ever said, Why me? Why me? I'm like, No, I've never once said that with either diabetes are cancer, because, you know, it's just happened, these are the cards I have been dealt, I'm going to play the cards and, and, and when it comes, you know, when it comes right down to it, I have a choice. You know, I can choose to live and and do the best I can with both illnesses, or I can stay at home and, and worry, and, you know, choose not to live? Yeah, no, we all have a choice.
Scott Benner 1:06:11
It makes a lot of sense to me. I don't you know, I not that I'm acquainting a person with a bug. But I don't think you know, when a shoe comes down and on, and I don't think the last thing I thinks is why May I think it just lives its life and and some of them get stepped on? And some of them don't. And that no one. I mean, listen, you said prayer earlier. And, and I've been candid throughout the podcast that I don't have any religious holdings at all. And yet, the way you see the world in the way I see the world are exactly the same. Right? I think so. Yeah. Yeah. I just, I just think that there's randomness, and the randomness might smack you in the face? And if it does, I mean, you've got a choice ready to lay there and die or get up and try to keep going? Right? Right. There's no other option, in my opinion, especially for me, because I don't really believe that anything happens after my brain shuts off. So I need to stay here as long as I can. Right? You know, I mean, like, I need to see a I need to watch the bad TV shows that I need to see more of that. I but no, but it truly what I need to see is I want to watch my children, like have a life as far as I can. I want to talk to my wife one more time, like I want to, you know, those are the things that I'm here to do. I want to see things I want to go kind of experience different places that I haven't seen before. But moreover, like, continue to talk to people and hear about like, I mean, all the stuff you said today is, I would have no way of knowing any of this without this podcast. Like you, you all have no idea like what a say, I'm gonna say blessing, because that's the only word that fits here, like what a blessing it is for me to host the podcast. And to get to have all these conversations. It's it's expanded who I am in a in a really meaningful way. And I can't thank everybody enough. Honestly, it's it's really wonderful that we have to share with people so that other people listening know, Susan sends an email and basically says, I'd love it if you'd get somebody on that has type one diabetes and cancer. And I was like, you could be that person. And because that I'm right, right. You weren't looking to be on the show you were looking to, for me to find somebody who had a similar story. That's correct. Do you still feel nervous? You said at the beginning, you
Susan Gimilaro 1:08:37
know? Yeah, yeah. It's been a wonderful conversation. really a wonderful conversation. I'm
Scott Benner 1:08:44
very glad I don't want to sound conceited. But I used to have these phone calls with people who had diabetes. And that's one of the ways that the podcast started. I was like, come on, people would love to hear this phone call. That's what I thought when it was over. That's like, maybe I could record them. Here you go. There you go. Is there anything that we should have talked about that we didn't
Susan Gimilaro 1:09:06
think the only thing I'd like to add is what I have learned from having both of these illnesses is that you need to be your own best advocate. You really need to be your own best advocate you know your body better than anyone else. You know, I had a major procedure with with this cancer and I had been working to keep my eye with my pump keeping myself really under very good control before going in for for this and when I got to the hospital. They said well, you know, we're going to take your pump off and will take over your care. And I really fought them on that. And but they did indeed take my pump away and They, in 24 hours time no one had come in checked my blood sugar. And I thought you don't even know what doses I take, you don't know when I should get them, you haven't checked my blood sugar. And I and I got my pump back. I said I'll take control of, of my, of my insulin, my blood sugar and in this part of my health care, and I had to sign all kinds of papers for it. And and no one ever came back and checked. See how I was doing was
Scott Benner 1:10:37
once you sign the papers? They were out of it? They were out of it and they were answers and they only took your pump so you wouldn't get low. They didn't they're not they weren't going to manage your blood sugar. They just were going to they didn't want you to get low. That's right. Yeah, well, I was 300. I fixed that you weren't low G's. I wasn't low. That's for sure. So it was like it was like you met yourself from back in when you were first diagnosed, like I don't want to pass out I'd rather be high than low. I don't want anybody to see in their case, they were like, this is not a problem we want to create. And I am always fascinated by the fact that a hospital will put you into a procedure where you're going to need your your white blood cells and you're going to need your body to fight infection and to help healing and then they drive up your blood sugar. So that that's not possible. Right? Fascinating.
Susan Gimilaro 1:11:26
Right? So so you know, I always tell tell people, just please be your best advocate. No one knows you better than you know, knows your body better than you. And
Scott Benner 1:11:37
I would add to that no one cares about you more than you. I would agree. Yeah. Even though there are medical professionals and I'm not saying they don't care, they're still there in a business. Right? You know, they got to go from you to the next person to the next person. They're not your personal physician is not a movie. This is not your personal physician. You know, they mean it's a brain who's their mechanic and they're running from car to car.
Susan Gimilaro 1:12:01
That's right, you know, and they don't have it's it's not again that they don't care but they don't have the time to really get into your understanding what your life is like and and what your blood sugar's are like, except tweak it here, tweak it there, and I'll see you in six months.
Scott Benner 1:12:20
That's amazing. I really appreciate you doing this. This was wonderful. Thank you
Susan Gimilaro 1:12:24
so much. I was so nervous about it. But I really this has been really wonderful experience. Thank you so much, Scott,
Scott Benner 1:12:31
my right back at you. I completely agree and and your computer didn't crash the whole time. That's right, your computer crashed three times this morning, but never once while we were talking. So thank goodness and maybe your prayer work.
First of all, a huge thanks to Susan for coming on the show and sharing us her story and sharing her story with us. Thanks also to Omni pod makers of the Omni pod dash and the Omni pod promise Learn more at Omni pod.com forward slash juice box. If you want to check out an organization doing wonderful things for people with type one diabetes, you have to look no farther than touched by type one.org. I want to take a second to thank you all for listening to the show the way you do being so supportive and and sharing the show with others. It's a big deal to me and that really, really helps the podcast. Thanks so much for listening. I'll be back soon with another episode.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#541 Dr. Saleh Adi
Dr. Saleh Adi is a pediatric endocrinologist and the Co-Founder and Chief Medical Advisor at Tidepool.org. Dr. Adi speaks with Scott about insulin delivering algorithms and type 1 diabetes Management ideas.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to Episode 541 of the Juicebox Podcast.
For this episode, I'd like to give credit where credit is due. Steven is a listener who sent me an email. And at the very end of it, it said, Hey, I have a guest suggestion for you. You should have Dr. salia. d on. I did a little research and I found out that the good doctor is a pediatric endocrinologist who is also the co founder of tide pool and their chief medical adviser. So I was like, all right, that sounds like a good idea. But what happened next was nothing short of absolutely inspiring. This conversation is one of my favorites that I've ever had about the management of diabetes, and I hope you enjoy it. Please remember, while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before you make any changes to your health care plan. or become bold with insulin. This conversation is going to break right down the middle almost the first half, we're going to talk a lot about algorithms and the future of them with Type One Diabetes. And in the second half, we're going to talk about Basal insulin, and ideas around management just listen to the whole thing. It's a Master's class.
This show is sponsored today by the glucagon that my daughter carries g vo hypo Penn. Find out more at G Vogue glucagon.com forward slash juice box. The episode is also sponsored by the Dexcom g six continuous glucose monitor, you can get started or Find out more at Dexcom comm forward slash juicebox. There are links to all the advertisers in the show notes of your podcast player. We're at Juicebox podcast.com.
Dr. Saleh Adi 2:02
My name is Saleh Adi and I am a pediatric endocrinologist I spent most of my career taking care of children with diabetes, until very recently, a couple of years ago when I decided that it was time for me to retire. And I left my position at UCSF and I have been just hanging out having fun and volunteer into a number of organizations that I've always done before, mostly related to diabetes in children. And here I am so happy to be involved and continue to be in the community this lovely, wonderful community to be part of.
Scott Benner 2:41
It's excellent. How long did you practice?
Dr. Saleh Adi 2:45
I graduated from UCSF program back in 1997. So that's really when I finished training. And first, I was mostly in the lab doing basic science research until about 2003. That's when I returned to San Francisco and focused my career, refocused my career on clinical work with children with diabetes. And I left the basic science world.
Scott Benner 3:15
What What made you What made you switch.
Dr. Saleh Adi 3:20
I had to make a decision. It's either basic science research or clinical work. And I couldn't do both at the same time, I loved my basic science research area. It was it was wonderful. It was a lot of fun, because I thought that this was something that I wanted to do for a living. But I always miss seeing patients and taking care of patients and interacting with human beings. And I realized after trying for a few years that it's really impossible to do both at the same time, you kind of have to choose either 120% research or 120% clinical, otherwise, you can't really get it done doing 50% here 50% there or a combination. And I had to make a decision and I gave up my lab and decided to be a clinician.
Scott Benner 4:08
Well, there's at least one person who's really glad that you did and it's a person who wrote to me and said you have to have salad on the on the program just to talk about basil insulin and I was like, very specifically was such a specific email. So I said big and I went back and forth with the person they said I'm telling you just have him on and I said okay, I'm gonna believe you. Now you're involved with tide pools still, is that right?
Dr. Saleh Adi 4:39
Correct. Correct. I'm still on the board the tide pool and and Chief Medical advisor. And I know just about everyone who works at tide pool and it's been it's been a lovely and fun journey since we established dipole seven, eight years ago.
Scott Benner 4:55
Well, well, you know, maybe I'll dig into it like this. Maybe. Do you remember The moment when tide pool said, we're going to try to bring an algorithm to market through the FDA.
Dr. Saleh Adi 5:07
Ah, yes, yes, I remember that very vividly. It was a board meeting when we discussed it for the very first time, and everyone was so excited about the idea, such a novel idea, and it was very timely. You know, the loop project has been around as a DIY loop people, you know, download the software and the hardware together and make it work. And it had been for such a long time. So controversial. Is it a good thing? Is it a bad thing? It works clearly works for the patients. But how do we make it official? How do we make it safe? And how do we get the stamp of approval from the authorities? I think there was at that time, it was highly controversial. And the FDA was sort of like, we really like this thing, but we can't allow it to just continue to go on like this. It's so non official, and in the hands of people who don't know what they're doing, it can be not so safe. I don't want to say dangerous, because it's probably okay. But the FDA eventually sort of decided to, well, let's take a different route. And I think in combination between the FDA, and jdrf, and the Helmsley Charitable Trust, they decided that, well, DIY loop is a nonprofit, open source project for the good of the community. title is an nonprofit, open source project for the good of the community. That sounds like maybe we can do something together. And they basically approach tight balls and said, Would you work on this project, to make it more formal and get the official approval, and do all the things that we need to do to make sure that it's safe and efficient and effective, and get it done with an FDA approval? And it was like an aha moment, like, of course, this is what we do. So let's pivot and change direction and make sure that we're going to be able to do this right. And that was a moment when it all started.
Scott Benner 7:20
I have a question. And this will I hope, it doesn't sound like I'm I don't even know the word here. How it I don't mean that if it sounds bit poor, I just don't understand this one aspect of it. How do you take something that's floating around on the internet? And take it and say, we're going to package this up and move it through the FDA? Like? Well, I guess the question is, why is that? Okay? It's just because it's it's open source? Is that the idea?
Dr. Saleh Adi 7:49
Well, because it's open source, that means it's available for anyone to take it, we don't have to pay for our task, a tight pool was to actually look at it, look at the software itself, and make sure that there are no bugs, make sure that it's rigorously tested, both technically, as well as clinically. Now, doing it clinically is a monumental task, like the traditional route would be? Well, let's take the software. And let's go and design a randomized control trial, where patients can get enrolled in the project and get this DIY loop software or patients and others randomly chosen to not get the software or that they would get another different software, and do the comparisons, you know, do the study, obviously, collecting all of the data, and then do the comparisons looking at the data back and see. Was this safe? Was it as safe as the other projects out there the other closed loop systems? Was it as effective as other closed loop systems? Or was it better or was it worse? And and doing it in a in a randomized control trial in a very efficient in a very official way? That would have taken a long, long time. And the the way we have chosen to do with that title is there are a lot of people who are using it and officially out there on their own. So why don't we end and they've been using it for years. So we have a ton of data collected on them already. It's just not done in a randomized control manner. But there's a lot of data out there that has been generated for years in real people living their real life. So why don't we just go and look at their data if we can, and enroll them in the study and continue to look at the data moving forward for those who are going to start on this system and then see what we get. We know how to look at data We know how to collect data and see whether there's any evidence of that the system is unsafe, or if there's any evidence that it's harmful. Or if there's any evidence that it's actually really good. And we can show the data. And that's kind of where it all started. And we collected the data, the observational study, and we crunched all the numbers. And I shouldn't say we, I think type poll, I really don't take much credit for it, they've done that tremendous job, and submitted it to the FDA and see if the FDA will be happy with all with this sort of non traditional pathway of looking at the safety of a project of a product. And if the if it's acceptable enough to demonstrate safety and efficacy, because at the end of the day, that's what the FDA wants to see. Is that Is it safe, that if we give it to the people to whom it was intended for, that it's going to be safe, if they use it the way it is right now. And is it effective? Does it really do what people claim it does? When we are clearly looking at data and not based on just anecdotal experiences? I see. And we'll wait to see what the FDA thinks about
Scott Benner 11:21
it's an amazing idea to just say to them, Look, I know, this is usually how it goes. But we have all this data, why don't you let us look at it and send it to you and see if you can't be okay with it. And exactly, it really is a fascinatingly simple, you know, you just don't hear too many people approach things in a common sense way, usually. So it's exciting to hear someone look at something and say, here's, here's the common sense of this here. Why don't we do this, I'll have to tell you that my daughter is 17. She's been using loop for maybe a year and a half or two years now. And I mean, she was doing incredibly well, prior, my daughter's a onesies been between five, two and six to for like eight years. But the amount of sleep that we got back exactly. With loop just at all, and we're using an auto Bolus branch. So it's a it's really wonderful. I mean, it's, it's, I haven't seen all of them, obviously. And on the pod fives not out yet. But this is the best one I've seen so far is is is this exact thing that we're using right now. Also, the idea that you that you kind of came to an agreement with on the pod, I mean, the idea that one day on the pod five can either run its algorithm, or yours is brilliant as well, in offering choice to people. I just think there's a lot of open mindedness going on that, that I like saying,
Dr. Saleh Adi 12:50
I like that term, I think the open mindedness, which would be if we were to coin an official term would be interoperability, if you will. So that was something that typos. And I get the credit to Howard and Brandon, the leaders in title of COVID, adopting that concept from the very beginning, from the very early days, it's just like, we have to open up the space of diabetes and, and get rid of all these silos of every company using only their devices and their software. It has to be open so that people can have a choice, which prompted they want to use which CGM do they want to use which software do they want to use, and put an end, put a combinations together, you don't have to buy all of your kitchen equipments from a single manufacturer, with a single brand you like this oven, you like that refrigerator, in that freezer, etc, you can put it together and you can work together. And this is the same concept. And in you know, I'll give the credit to the FDA, who will really was saying, We love the idea as well. And we want to encourage that. So now it's become a very common thing to ask for it just like when you as a manufacturer, when you create a product, how interoperable it is. And it's desirable to be very interoperable and open to other companies and other softwares to work with. And that also was something that jdrf pushed for very, very strongly as well.
Scott Benner 14:26
Yeah, I think that if you're not, if you're not paying attention, you might think of it as I enjoy this pump over this pump. And that's what makes this my choice. But you have to see that moving forward. You're going to want to choose between algorithms like this, the hardware is one thing but the operating system, you're going to want some impact on to so imagine if you really loved Medtronic operating system, but you wanted to wear it on the pot or you know, I mean, I realized it's probably not going to work like that between companies. But this is that idea. Like you get it on the pod because you like it you get on the pod five and you say I really want to try tide pool. And you can like it mean open minus from the FDA from tide pool, I think on the pod to being a privately held company saying, Yeah, well, let's do this like, that's there's a lot of exciting things in here. And I think people with diabetes are going to recognize in the next handful of years and beyond that the algorithms are going to be as valuable as anything else.
Dr. Saleh Adi 15:24
Absolutely. And the algorithm really is the biggest difference, I think that the mechanics of the hardware are more or less for the comfort and the and with what it's like, you know, what I'm comfortable with. And it's the it's the human factor of the hardware that attracts certain populations, certain people, but also the software, I think it's even more important, because software algorithms with all of these closed loop systems are different from each other, they are different enough, that in my opinion, my humble opinion, that that a certain software algorithm isn't going to work for every patient with Type One Diabetes. It depends on how much insulin they take, it depends on how how much beta cell function they have, it depends on how old they are. It depends on their lifestyle, it depends if they are, I think that an algorithm that's going to work really well, for a young adult who eats three times a day very distinct meals, is not may or may not work for a teenager who eats 16 times a day, and eat five grams snack here, and 12 grams snack there, and 128 grams, you know, breakfast, it may or may not work. But and the same thing, if it works for that teenager, who has completely unscheduled bursts of activities and food and behavior may also not be the best algorithm for a two year old infant who has type one diabetes, that's a whole different animal dealing with type one diabetes in a toddler versus an infant versus a young child versus an adolescent versus a young adult, versus even an older person who's like 60 7080 year old with Type One Diabetes, those are very different people. And we really have to approach them differently. And why I think we have to keep that in mind is that not all algorithms for closed loop systems are going to work for every single person with diabetes. Some of them will work better for others, they may work fine and be safe. And I think it may be more, they may be more effective for different populations of people would they be
Scott Benner 17:49
I found that there's a learning curve to I'm going to use the wrong word here. Because I don't mean it to sound like this. But you have to sort of manipulate what the algorithm wants to do sometimes. And sure, and you can make it fit you. If you understand the bigger picture. Surely, no, you definitely have to and for my daughter, you definitely have to Pre-Bolus food. If you miss on the Bolus, you can't lay back and just say, Oh, the algorithm will fix this because maybe six hours later, your blood sugar will come back down again, you have to be willing to go back at it. And then recognize when to let the algorithm start taking basil away again, like there's there's little tricks to do. I think that's where people have to learn on their own how to do it. But I'm saying that away from food, and away from an active Bolus. There's nothing better than an algorithm like this, the ability at a low number is is astonishing the ability to stop a really frightening low, I don't know that my daughter's blood sugar has gone under 50 in two years. Like it, you know, we've had, we've had times where you're like, Oh, I know this happened. But you but you think back to prior to the algorithm, a 50 would have turned into a 30. In a situation like that, then you go back and look at the data and see that for the past 90 minutes, this thing has been trying to stop this low. And I for people who have not lived long with diabetes, you might not know it, you know, for people who weren't born 20 years ago, you might not know it, but everybody needs to understand that in my opinion, this is the way to go. But settings are still King, no matter what like if your settings aren't right. You might as well be doing it blindfolded with a with an old rusty needle like it you have to have your settings right.
Dr. Saleh Adi 19:36
Yeah, good. I agree with you more. And I would add a couple of things. One is you know, Scott, I think you know, I totally agree with what you said is that you need to understand how the algorithm works. And not to the details over over the software engineer can level the you know, understanding but at least know what it's trying to do. The more you know, the more you understand how the software is how the algorithm is thinking, the more effective you can make it by manipulating certain things, not necessarily manipulating the code. Again, that's, you know, let's not go there. But more like, you know, thinking along the same lines that the algorithm is thinking. Just like when you're dealing with a child, you can have just to think, the same way that child is thinking. And you can have a really good relationship if you do that. And the same thing for it for a soccer algorithm, you can make it work much better if you know how it works, and know which buttons you need to turn left to right, to make things better. But also understanding that your manipulations can make can make an algorithm work much better. But it can also, in terms interfere with its function to be 100%. Effective? Yes. So you really need to know what what are you doing to make it better? And what are you doing that can potentially make it worse? And that effectiveness of you know, not getting down to 50 for the last two years, if you don't know what you're doing, you might actually prevent it from being that effective.
Scott Benner 21:22
Yeah, it's 100%. True, as as easily as you can assist it, you can fight against it. And exactly when you start fighting against it, it's making decisions based off of things you've told it, and then you're changing the game, but it's still doing what you told it like you can't, you can't just randomly throw in a couple of units of insulin and not somehow explain to the algorithm that this is because of I mismatched my carbs. It's one of the things that that makes loop, I think really great is the little stuff, like being able to go back to a Bolus from 90 minutes ago and say, You know what, I told that thing, it was 45. But it turns out, this is 52 carbs. Like that kind of stuff is huge. We have got it's brilliant. Yeah, we have a series of episodes in the podcast called Fox in the loop house that I think you might really enjoy. Where we talk about how to, you know how to be Dr. Frankenstein a little bit with with the algorithm I am. I have to say I'm super excited to see on the pod five. I know it's gonna work differently than loop. But I do want to understand it. And I want to try to get to the point where I'm a good tactician with that as well. But can I can I ask you a question before we move forward a little bit and talk about stuff? If you don't? If you don't know, you don't know. But I keep thinking. You said something earlier in the like when you almost came on, like the FDA said they couldn't let this thing go on. Meaning like an algorithm that just lives out in the in the world that's giving people insulin, do you think they're going to come after the DIY DIY loop at some point and try to try to scuttle it somehow?
Dr. Saleh Adi 23:05
I think that, you know, again, I think that if they wanted to do that they would have done that years ago. And the fact that they're working together with jdrf and Helmsley and title and the community to make it safe is like they don't want to go after anybody. They want this to actually work and be safe, so that everyone can have it. That's good, not just not just the, you know, the elite software engineers and mathematicians who want to, you know, grab this and, and put things together. They want everyone to benefit from it. Otherwise, we wouldn't be doing it.
Scott Benner 23:43
Right now. It's it's an interesting topic, because I know a lot of people use it, you know, when you consider that it's just something that exists out in the ether. But, you know, when you pull that up against how many people are using insulin, really, statistically, no one's using loop. You can compare it to how many people need insulin. So if you can get it into hands that way, I mean, I know very little about type two diabetes, but it seems to me if you're insulin dependent type two, an algorithm would be genius for you. And
Dr. Saleh Adi 24:16
yes, yes. But I have to say, Scott. It's it's not a bad thing. That loop is not so widely used currently, as it as it is in its current form. Because I do think that it's not for everyone. Like you hinted at, which is like, you really need to know what you're doing. Yeah. You need to put the pieces together. You need to do it right. And then you need to have an understanding of how the algorithm works. Because because you really you do need to make sure that you're not interfering with You're not going to interfere with its performance because you can, because by design loop was designed to allow for a lot of things that the patients can the user can manipulate. And for a good reason, it was a clever design. But there's so many things you can manipulate that if you don't know what you're doing, you're actually going to make it not effective and even unsafe, if you go far enough. So I think it's a it's a good thing. And that's what I'm excited about his title is trying to make sure that there are some, some guardrails in there, that are put together so that you don't end up manipulating stuff that you shouldn't be manipulating.
Scott Benner 25:43
Now, I agree, I think that if you if you could take a macro view of this, that the idea that this happened, and that there were this kind of small band of people who were so fervently, you know, developing the algorithm, and at the same time supporting people, and they even put up barriers for people to get to it. I mean, it's not easy to figure out how to do this. And so it's sort of that it sounds crazy. But I do the same thing with the podcast, like, I don't make it easy to be a guest on the podcast. And because of that, what if you're there, when I turn on the machine, when you say you're going to be there, I know, you really wanted to be on the podcast, and that, believe it or not, weeds out a lot of good next. So because there are people who flake and bail and, and you know, and I can't wait three months to be on or something like that. And I think the same thing about about loopy has to make it a little hard, you can't just hand it out like candy. because like you said, you could you could really not know what you're doing. But these people then help other people, they saw people brought them into the fold, explained it to him kind of created a little user base of it. And it expanded slowly. It's beautiful, really, like you'll look back on this in 20 years and think
Dr. Saleh Adi 26:58
Oh, absolutely, yeah, that's the revolution. You know, yeah, it really started start a revolution, the way we think about the whole field and about the approach of FDA approval in building software. And, and I think it also drove, you know, pushed the world of ABS into this interoperability concept even further. Because it's it's a product that stands on its own. It's just an algorithm data. Loop doesn't doesn't make a pump doesn't make a CGM. It's just a software. So you know, we don't have to build a pump. We don't have to build our own CGM. It's a software that should be able to be used by by anybody who uses either pump, or either CGM.
Scott Benner 27:46
Is tide pool involved in development, or are they? Are they quite simply just taking this specific algorithm and trying to move it through the process? Or do you think you guys will at some point, say, well, let's get some developers in here, and we'll get an auto Bolus, like version of this and things like that?
Dr. Saleh Adi 28:04
You know, I think absolutely right. It's, it's not just, let's take it, take what we have and get it approved, I think it's, you know, obviously, once it's approved, once that virgin one is approved, we're already working on version two. And it's going to have different features, and it's going to have, but we need to get the approval for the first one need to go out there and actually be used. But no title will eventually continue to be involved in the development and, and optimization of loop as a software.
Scott Benner 28:41
That's really I have to say, That's terrific to hear. Because as much as I enjoyed loop, it didn't really it didn't really live up to its promise for us until the auto Bolus branch came. And that that was a that was a step up. And and I'll tell you to, if for anybody listening, as much as I've learned about diabetes over the years and kind of put it into words that people can understand, I've learned a lot from the algorithm as well like seeing it. Take away basil or or up basil or to see like a bad site. Like you can see a bad site because Luke keeps bolusing you're stuck at 120. And Luke just keeps like the auto Bolus branch just keeps Bolus and Bolus and Bolus and I'm like, Oh, this thing doesn't think it's gonna break this. This this line right now like this 120 is sticking and then you learn to see bad sides because of that. You learn. You know how you could have attacked these things differently without the algorithm. I've learned more about using insulin from loop in the last two years, maybe than I have from using it.
Dr. Saleh Adi 29:50
And yeah, yeah, yeah. Yeah, because this is forcing you to think it's not just take an injection or take a Bolus and go away. There. Because there's not much else you can do, you have to wait for the effect of the insulin. I think because of the intelligence of the software, it's now doing all kinds of things. And if you're really into it, you can start looking at the data. You're looking at that CGM tracing and seeing like, where is it moving from here? Why is it not moving? How can it move too far it was this wasn't the intended action. And it makes you think, and the more you think about it, the more you understand it, and the more you understand it, the better operator you become,
Scott Benner 30:33
it almost becomes second nature. itself. Yes, it takes.
Dr. Saleh Adi 30:38
And it takes a while, it takes a while. And, and there are people who can learn something to themselves. And they can really make it work so well, if they're doing it themselves. But they can't teach it to somebody else. Just like, I don't know how I'm doing this. I just know how to do it. But there are also people who are really good about learning something and also teaching it to someone else. So I think that's where the role of the clinicians come. They have to really understand the algorithms, and figure out how to teach people at different levels of ability to understand these technicalities. And I'm not really good at that. I don't I still don't know how, you know, functions. 100% there's so many things that I don't know about. And I go back to my friends and colleagues and dipole. And I say, Can you tell me why did it do this? Why did it Why didn't do this. And then I learned one more thing about how it thinks and how it operates.
Scott Benner 31:46
I think that one of the biggest leap that we're all going to have to make is exactly what you just said, which is finding a way for clinicians to simply explain this to someone. I don't know that that's doable. Honestly, like, I think it almost is going to have to be one of those slow matriculation things. We're a generation of doctors lives with it like I did, and stares at it and sees it work, until you can just sort of talk about it in a colloquial way, without it seeming overwhelming.
Dr. Saleh Adi 32:18
Yeah, I think I agree with you, I don't think that it's possible for every clinician to be so immersed in the technology of diabetes, that they're going to understand every single device and every single algorithm, I think there are, you know, a handful of us who really, this is what they do for a living. And it's just best to look at data and look at numbers. And they just love that and they want to understand it. But not everyone's going to have that the ability and the luxury to spend that much time and do all of that. So I think the clinicians have have two different roles in this in this field. One is to know all of the algorithms and the hardware is and what they can and cannot do, and help the patient make the choice. And I stress the word help you cheat, the patient still has to make the choice on their own. Not as a challenge, but more like this, you know, what works for you and what doesn't work for you. But also, but the convention needs to be there for advice. And for sort of direction, I think this one might work better for you. I know you like you know, product B but I think product A might be better for you because of so and so based on experience based on just knowledge from the past and seeing other patients similar to you. So that's one and then the other is, is continuing the education started with simple and then come back, look at the data and say, Okay, how can we make this even better? I really think that closed loop systems should not be accepted to achieve time and range of 70 some percent on the I think they can do a lot more than 75 and 76%. If we if we learn how to operate them, right if we learn how to manipulate them, right. And if we obviously I'm talking like if you Bolus for everything you eat, of course, I mean that's like the essential thing. If you don't do that, then forget it. It's just not gonna achieve 80 90% in time and range. So besides doing that, I think that there's a lot to be done gradually for teaching patients and families and how to use the systems to make it work effectively more effectively. But I also go back to one thing you said earlier, which I think I totally agree with in believing, which is the settings the settings are absolutely key to making any system work effective. If you don't have your setting sites, I mean different systems work differently, obviously. And some will take whatever settings you have and manipulated and increase it and decrease it. And some will just ignore completely what your settings are and just think on their own. But I think for at least for the systems that are based on settings that we put into the pump, then I think that the settings need to be optimized as much as possible. If you don't have settings correct, then the system is just fighting too much, and not being super effective.
Scott Benner 35:35
So I think that leads us pretty well into into the next part of our conversation. I'm very pleased to bring this podcast to people because I think it does the thing. You know, part of what it does is it does the it does the job that manufacturers are not allowed to do because the FDA doesn't allow them to do it. And I say this here so that people understand that a pump company is not allowed to tell you how to Bolus for food. Like they're they're quite literally not allowed to, they can tell you that this is the pump. This is how the pump works. You know, functionally, this is what an extended Bolus is. But I can't tell you when to use an extended Bolus, besides, you know, beyond the example of if you have pizza, they're not allowed to talk about how to use insulin. And that's
Dr. Saleh Adi 36:24
not they're not clinicians, that's the clinicians job 100%. And
Scott Benner 36:27
so a lot of people get frustrated because they get on a pump and they think oh, the thing doesn't work, but they don't know how to use insulin. So at the basis of how I talk about insulin, whether you're using an algorithm or you're not in my mind in this order, it is get your basil correct. Learn how to Pre-Bolus understand the different impacts of different foods and then stay flexible. To me those are the four steps to stability and making decent boluses How do you think about that?
Just briefly before the ad start, let me let you know that that noise you were just hearing in the audio is a person down the street from where I record grinding up the trunk of a tree and that does not last for very long during the episode but I am sorry about it. It was far from here and sounded like it was happening right next to the microphone. Anyway, g vo Kibo pen has no visible needle. And it's the first pre mixed autoinjector of glucagon for very low blood sugar and adults and kids with diabetes ages two and above. Not only is chivo hypo pen simple to administer, but it's simple to learn more about. All you have to do is go to G Vogue glucagon.com forward slash juicebox. g Vogue shouldn't be used in patients with insulin, Noma or pheochromocytoma. Visit g Vogue glucagon.com slash risk. So far, there's been a lot of talk in this episode about algorithms, right an algorithm is a program that will live in the in the case of the Omnipod five, it'll live right in the circuit board of your pod. In the case of tide pool when it comes out. It'll live on your cell phone, if you're using a tandem pump. I think it lives right on the pump. I'm not 100% certain but it no matter which one of those you're using unless it's Medtronic. The one thing that all three of them are going to have in common is that they're getting their data so they can make those decisions that they're going to make from the Dexcom CGM. So maybe now is the perfect time for you to find out about the Dexcom g six continuous glucose monitor. Dexcom is a device that you wear, and it reports your blood sugar back to you in real time. Now for Dexcom users that could mean on the receiver that they'll give you or write back to your Android or iPhone, if that's what you want to do. Users of the Dexcom can have followers up to 10. Actually, people just like me or your mom or dad or brother or sister or school nurse people you trust, who can watch your blood sugar in real time on their phone if you like. or you don't have to share it with anybody. It's up to you. But the option is there. Now what is the Dexcom going to show you it's going to show you the speed and direction of your blood sugar. It's also going to show you what your blood sugar is. You're saying I'm saying the number, say your blood sugar's 124. This speed is it moving at all up or down. And if so how quickly two points per minute, three, four more. It'll tell you that too, with directional hours. So now the arrow is gonna point in the direction if your blood sugar's dropping, let's say and tell you how fast it's dropping so is my 124 dropping it four points per minute to one etc etc. This information is super valuable extremely extremely helpful, and at the core of not only how I make decisions about my daughter, but it's also the way that these algorithms are going to know what to do with your insulin. So just like seeing Arden's blood sugar tells me, I think we need a Temp Basal increase here, we should Bolus a little bit or maybe take away some insulin, whatever it tells us, whatever algorithm you choose, is going to also get that information. Please trust me, if you can afford this stuff, if you have insurance coverage, look into it. dexcom.com, forward slash juicebox, the future is here already. Go find links to the tchibo hypo pen Dexcom. And all the sponsors are available at Juicebox Podcast comm or they're right there in the show notes of your podcast player.
Dr. Saleh Adi 41:05
I love your elements, the four elements. And I think you're absolutely right. First, I would start with a Basal. You know, besides understanding how insulin works, and how long it takes for it to actually start working, and how long does it take to be to peak its action, and how long does it last before it finally gone and has no effect anymore. And different insulins have different dynamics. And understanding how food affects the blood sugar and how the dynamics of digestion and absorption different foods are slower and, and and faster than others. And and and they're different in each person. And they're different in the same person. If you eat something in the morning versus you eat it in the evening, the dynamics of absorption are completely different. So learning all of that all of those individual parameters about that particular patient, then we're we're talking about the algorithms and the software and the hardware, I think, you know, setting the basil correctly is number one, and then figuring out what the right ratios are the incident the current ratio, and the correction ratio, and the insulin duration timing, to factoring all of that into the thought process, not just the mechanics, but also the thought process. And that's really hard. You know, it's it's hard to ask everyone to do this every single time they eat something. So we have to simplify it in the beginning, and then get more sophisticated as time goes by. And it's like you said it's it, it then becomes second nature. It's hard to deal with in the beginning. So I think it's upon us actually the clinicians to make it simple to make it intuitive. And to start with smaller baby steps, and then keep going. And in order to do that, you can't just come to the clinic every three months, and do this lifetime of education about certain things, that the the interactions between the patients, the clinicians and the and the patients needs to be continuous all the time. You grab a teaching moment and you say, Okay, let's talk about this. Let's learn one thing today. And that cannot be again, like every three months, when you come to the clinic, there has to be a channel of communication that's open. And I think this is this is this was one thing that titebond really insisted on from the beginning, from the very early days is just like, we have to make the data visible in an intuitive and simple way, and an actionable way. So that we can collect the data. And we can visualize it very simply that everyone can understand it. Because it's key. You can't you can you can come up with all kinds of ideas and and interventions and trials and say, well, let's do this and see how it works. If you don't collect the CGM data and go back and look at it, you have no idea how your experiment worked or didn't work, or what worked and what didn't work.
Scott Benner 44:15
I've been considering for the future of the podcast. I have a friend of mine comes on the show sometimes Her name is Jenny. She's had Type One Diabetes for over 30 years. She works at integrated diabetes. So she is she spends her day talking people virtually through their blood sugar's and she's just really terrific. And one of my ideas for the future is to do a series for clinicians about how to talk to people about their stuff. And it's cool. Yeah, I think that one of the ideas I've had in the past that I don't know why hospitals don't do instead of seeing people 15 and 20 minutes at a time. What can't you do in a large group setting where you can put together a few hours. So you know, see, see 20 3040 people Time and give their give them a larger instruction, which will, by bringing them all together gives you more time to talk to them.
Dr. Saleh Adi 45:06
Like I think that it means certain things can be done in a group and certain things can only be done in one on one person. Sure. So I agree with you that we can be a lot more efficient if we, if we knew what to teach as a group, and, and the idea of doing classes. But now with the technology that everything can be done remotely via zoom and other platforms, then I think I think we need to take advantage of that. And we're not actually doing that very well. Would it?
Scott Benner 45:39
Would it surprise you to know that literally every day, I get between six and 15 messages from people who are experiencing stability, and a one sees in the fives or sixes who just previously three, four or five months earlier, we're on a roller coaster and had no idea what they're doing just from listening to a podcast?
Dr. Saleh Adi 46:03
Yes, that would that would surprise me. But pleasantly surprised to hear that that within a few months, you can actually get that kind of comfort and stability and feel good about it. It can be as you well know, I don't have to tell you this. But it can be extremely frustrating when you're trying to do something, and it just doesn't work. And I really think that, you know, for a lot of my my own personal experience that I have seen, a lot of people get really frustrated, simply because they've tried everything. And the reason that their experiments are not working is because their settings are not correct. And again, if you don't have your insulin to carb ratio, if you don't have your ISF, if you don't have your Basal rate settings correctly, you can go crazy doing all kinds of things. And this just doesn't make sense, right?
Scott Benner 46:58
You can work as hard as you want to dig a hole. But if you're using a screwdriver, it's not going to go well. And right this is this is what happens over and over. So how do you talk to people about the setting their Basal insulin, because the way I talk about it is so incredibly simplified that I wonder how you would talk about it.
Dr. Saleh Adi 47:19
Basal rate is one of my favorite topics to talk about. Because I believe that the base rate is the key to achieving good results. And it's the most important parameter to look at. Because if you don't get anything else, right, you can get the nighttime when there is no food and no activity, which is the which is the product of nothing else. But basically, there's nothing else going on at night. And if you can figure that out correctly, you get yourself eight to 10 hours of straight line of CGM that is going from left to right. And maybe just maybe changing a little bit or fluctuating, but it's still staying within the target range of 70 to 180, or even 70 to 140. So it's worth studying there. And if you get that right, if you get the base rate right at night, then I think it actually gets you in a very good spot during the day. You don't have to do basil testing during the day, you don't have to go for a whole day without carbs to figure out what your basil rate is. I truly believe that if you get the basil rate correct at night, it gives you a pretty darn good idea what the base rate should be during the day. That's number one. And number two is figuring out the basil rate pattern. There is a pattern of basil of basil insulin requirement throughout the day, but particularly at night. And that pattern is not just a flat one single base rate all night long. What the patient what that is the kids that I dealt with all my career is like when the child with Type One Diabetes requires, you know, point four units of insulin, it doesn't, it's not going to work if you do point four units of insulin the whole night. There's definitely a variability a tremendous variability. And it could be point four in one hour and can be point six or seven in one out and then come back two hours later, and it has dropped down to point two or point three units an hour. And knowing that pattern and following that pattern can really put you in a good spot. And then you can achieve a very good flatline of CGM during the night and it can be extremely satisfying. Not only that you had a very good night but also that when you get up in the morning, you're starting in a good spot to begin with. If you get up in the morning with a blood sugar of 300 it's really hard to get that that fixed For the for the rest of the day, if you start out with a blood sugar around 100, then I think it's going to be a much easier job to actually get it and stay in range for the rest of the day. So Basal rate is the key. Basal rate is the first thing I look at. and nighttime Basal rate is the is where we start. And once we get that, right, we know the basic rate for the day. And then we start working on the incident, the conversation and the eyes.
Scott Benner 50:26
So you have no way of knowing this because you don't listen to the podcast. But when other people listen to this, they're going to be able to feel me smiling while you were speaking. Because you would love this podcast. That's the first thing I can tell you. And you and I are like we are absolutely kindred spirits. You You really did just speak words that I have spoken almost in the exact same order. You used a couple of different ones. But you said exactly the same thing that I've been telling people for years. I'm so glad to know, I'm so thrilled you you said what you did? Because I agree. I mean, everything like I don't think you need to basil tests, like when I tell people when they ask like, Well, how do you figure out what your basil is? I tell them, I think of it as like an old stereo. I turn it up until my mom yells and then I turn it back down just a little bit. And that's good. And you you always do it overnight, right? Like because overnight, all the a lot of the impacts are gone. Unless they're children and they're growing, you know, but overnight, you get overnight, right? And then the daytime is going to be pretty close to the overnight. Some people need a little more overnight, a little less. But for the most part, if you can figure it out overnight, you can figure out during the day and then that just leads into the rest of it, then you can check on your meal insulin is my meal insulin right? Am I Pre-Bolus Singh enough in and then from there, it's just understanding the different impacts of foods and not getting caught up and saying, well, this is 10 carbs. And my ratio is one to 10. I don't know why this one not like what I tell people is I don't care why it goes up. If If meatloaf and green beans mashed potatoes, you know, comes down to 55 carbs, but you always end up correcting later with two more units. We'll then dammit move the two units into the bullet. Because Exactly. It's what that meal needs like just be done. Stop fighting.
Dr. Saleh Adi 52:18
Right, right. It's it's not it's not let's blame the manufacturer who printed the information incorrectly on the box and says if it says 18 grams, but clearly in your experience, it's 24 just counted as 24 next time doesn't matter what the box says. Yeah,
Scott Benner 52:34
no, this has been terrific because you just made me feel like a genius. I really am thrilled. Well, you are you are. No you didn't need to say that. But it just was so free. You know for your edification. Like, I've just been a stay at home dad for decades. My daughter was diagnosed when she was two. I was just like everybody else. I didn't know what I was doing. I didn't understand how the insulin worked. I felt like I was killing her constantly. And honestly, it was before CGM. I probably was. She had a she had had a couple of seizures from low blood sugars. And I just one day I was like, I gotta figure this out, or she's not going to be okay. And back then I had a blog, and I wrote on it a lot. And writing on the blog helped me figure out things. And then one day, I just said to my wife, I'm like, I have a system. I was like, there's a system here and it works. And I don't think it would just work for Arden. I think it would work for everybody. And I just realized that like one of the more damaging things that we say to people with diabetes is like, Oh, that's diabetes. You can't do anything about that. Yeah, yeah. Yeah. Or I'm brittle. You know, you're, you're brittle, because your settings are probably all wrong. Like Like, like, like your jump, I understand your blood sugar flies all over the place. But now I see people all the time. You know, when they come into the podcast, who look quote, unquote brittle from 20 years ago, but their Basal is just wrong, where they let me ask you this. How often do you find that people mistakenly treat Lowe's by taking away basil instead of increasing basil so that they can make better meal boluses does that Oh, it
Dr. Saleh Adi 54:16
it happens. It used to happen more often than it does now. And it all comes back to miss understanding the dynamics of insulin. Cutting off your basil is not going to treat your low, you're gonna be low for the next hour or so you need to do something else. You can prevent the low by cutting up basil, or by stopping the basil or together an hour before or an hour and a half before. But you can't treat a low by doing that.
Scott Benner 54:47
Yeah, let me let me dig deeper and tell you what I've seen from talking to people. So just let's be accepting of an idea that there's a person in front of you who needs a unit of insulin per hour as basil bye For some reason, they're using point seven. And then they end up having to make super aggressive boluses. At meals, they don't Pre-Bolus usually they fly up, then they crash down. And then they go back to their doctor and say, Look what's happening. And the doctor says, oh, you're having a lot of lows, we should take away your Basal insulin. Now they're point seven ends up point five. And all that does is make them be even more aggressive at meals next time creating more lows. Do you see that? Have you ever seen that?
Dr. Saleh Adi 55:28
Oh, more often than I would like to. And I think that even a lot of people also on their own start adjusting their basil incorrectly. I, I encourage people to look at their data and make small changes. But the first thing that they always think about is it's the base rate that needs to be changed. And sometimes it's it because I think it's really hard to figure out whether the insulin to carb ratio is working or not working. I think it's harder to look at it, I don't think it's really hard. I think it's just harder to assess it. Versus it's the Basal that's too much, or it's the Basal is too little this increase that and all of a sudden there's this imbalance between the basil and the Bolus is. And I think that's also an important thing is to understand for each age group, what should the basil present be compared to the total daily dose of insulin? And that can be an extremely helpful guidance towards where should I be looking? First, there's a big discrepancy. I know that, for example, a 14 year old with Type One Diabetes should have about 40 to 45% base rate. And all of a sudden, I see someone who is 14 year old and only getting getting like 65%, in Basal were clear and 35% in bonuses. And the carb ratio is only, you know, one year for 20 grams, then clearly, there's an imbalance there and I can direct I can straight go to that Basal retinas sake, that's too high, 65% Basal for a 14 year old or for anyone age, that's just too much. I think we need to cut back your Basal. And let's either wait and see what happens to your blood sugars, or we can blindly increase your insulin to carb ratio, because it clearly too low and adequate need to read. We rebalance things a little bit. So it's a very helpful first look to say, where are we in the ballpark of Basal rate? Is it the right percent? Is this something that we need to just generally increase or decrease? Or is it more like it's in the right ballpark? I just need to fine tune it a little.
Scott Benner 57:47
I sometimes believe that that's a holdover from old MDI, clinicians who just pushed up basil to Yes, yes. To ask other problems. Yes, yes. Oh, what was I just gonna say do basil. Oh, I, I have this theory. If this is anecdotal, completely, but I do end up talking to a lot of people, I think a good place to start with children who are pre pubescent, like, you know, no, but nobody's into, you know, any other. Any other real growth yet? point one per hour per 10 pounds. That's where I start in my head. It's not all of it for basil, basil. So if you're 50 pounds, you're around point five. If you're 40 pounds, you're around point four. It's a starting point. It's not always 100%. Correct. But yeah, but when you're, but I find myself frequently put in a position where I'm talking to a person privately, who I don't really know. And I don't know how to like, I mean, they want to they're, they're lost. They're, I mean, try to imagine so that you've, you're, you're a parent of a child, or you're a grown up with diabetes, and you're reaching out to a person on the internet for help, like, imagine how lost you are in that moment, because that's not a good idea. And so then I get a message from somebody. And I say, Well, look, let's just get your basil straight first, then I think everything else will start making sense. Well, where do I start? And then you look, and they have 7000 basil rates, all because they've been chasing ghosts for weeks, you know, trying to, you know, things around. And I'm like, like, let's just start here. And I usually say, if it's a 50 pound kid, and I see for instance, they're at point two, five, they're at point three, five, but they're always in 200. So I'm always like, well, I would maybe move that 2.4, let it sit for a number of hours, see what happens. And then we can move it from there. That's just a jumping in point for me. But
Dr. Saleh Adi 59:39
I never thought of it that way. But it, it may be perfectly reasonable to then I will have to do the math. And if I were to approach it from the way I think about it, I would say you know, a pre pubescent child, let's say an eight year old For example, or a seven year old, would require a total daily insulin of somewhere around point five units per hour. For everything total daily, so a seven year old, let's say if it's a I'm sorry, what did they say? point point five unit per kilo per day? Sorry. I misspoke. point five units per kilo per day. So how many kilogram is that child, let's just say if it's a 20 kilos, that means the total daily insulin should be about 10 units, 10 units for that child who was a seven or eight year old, about 40% of that, or less 35 to 40% of their GDP base rate. So that's about three and a half to four units a day of base rate. Does this jive with your calculation? You don't have to do the math? No, no,
Scott Benner 1:00:55
it's pretty close. It's and like I said, it's not a perfect thing. It's not like you just say to somebody, what's your way? This is it? It's a starting point. It's an exactly, you know, exactly. And that's what they lack. That's what I've learned when you're speaking to people's what they lack is, they're like, I don't know, up, down left, right. I've got seven basil programs. My doctor keeps you know, every time I say, Look, he's, you know, no one says my kid's blood sugar's high at 11 o'clock every night. No doctor says, Do you eat a high fat meal in evenings? Like no one ever says that? They say, oh, we'll turn your basil up an hour before it goes up usually.
Dr. Saleh Adi 1:01:29
Right. Right, right. And the other thing I see a lot is, you know, it's in, you know, if you're, you get up in the morning, your blood sugar is 200. And then immediately jumped was like, well, your base rate is not enough. We need to increase your Basal at night. And I think that that happens a lot. And sometimes it's correct. But oftentimes, it's not. Because what was your blood sugar at bedtime? And what was it at two in the morning, if you went to bed at 202, in the morning, it was 200. When you woke up in the morning at 200. That means your Basal rate is actually pretty darn good. It kept your blood sugar exactly where it was the beginning. And for the whole night, you're a 200, ss flatline. 200 that means your base rate is perfect. You don't need to increase your base out what you need to do is to increase your insulin to carb ratio for dinner, or increase your base or before midnight. So that way, you actually hit the night, hit the bed and hit the night with a good blood sugar and it stays that way. And you wake up.
Scott Benner 1:02:29
Yes, yes, yes. That's the way I think about insulin gwit. When I tell people, I say look, insulin you use now is for later. But more importantly, more importantly, the way to think of it. If you're if you're in the middle of managing in the moment, you have to think of it this way. Insulin from before, is for now. That's it right? Right. Right, right. Same thing, but it's a different way of considering what's happening to me now is from before, like that, that helps you in the moment make a decision. Not you know, if you say well, what I'm doing now is for later, people chase they just keep chasing the insulin. It's it's just it's like a time travel movie. And they're in the wrong timeline. You know, II mean, like they're fighting the dragon, the dragon. The dragon was here three hours ago. You don't find it now, you know, get and I always tell people get low, get steady start over. Like don't because they'll chase for days and weeks. And in it. Yeah. And that's the thing that gets. I think that's where the psychological impact comes in that feeling of I'm working so hard and nothing's going right like and and I want to trace back to something you said earlier, I do completely understand that when people are newly diagnosed, that you want to spoon feed them a little bit and bring them along slowly. But I think the one sentence that never gets spoken to people that they need is this is what we're doing now. But this is going to keep changing. Because exactly they get stuck, especially when a honeymoon ends. I don't understand. I don't understand what's happening. Well, there's not enough insulin here has to be this has always worked hasn't and then I think has no one told you that this was going to increase or how is it he didn't think that you gained 10 pounds. And now you need more insulin, or you know, like little things that just you get you get so you get so micro and you're so close to it. You just kind of can't see the forest for the trees after a while. And if someone doesn't tell you that you have to step back every once in a while. You'll never think to do it.
Dr. Saleh Adi 1:04:29
It's Yeah, no, I agree. Scott, I think this is you know, in pediatrics training, this is drilled in our head, which is the anticipatory guidance, which is to tell the parents what to expect next year, what to expect six months from now, so that they're not all of a sudden, oh my god, what's happening to my child. So it's that anticipatory guidance and then telling them what's going to happen from now. And don't be surprised, and I've always taught people and I can't believe that I get the same response every time just like when they hit puberty, they're going to be on 1.2 units an hour, they're going to be on a current ratio of one to five grams of carbohydrates. Don't be surprised when that happens. And all of a sudden, they just their eyes wide open, just like what they're going to require that much insulin, it's gonna come in just like, no, that's what they need. And we just have to keep increasing it with time. And then the other thing is, no matter what we do, we get the settings right, we get we work really hard at that base rate to get to be just perfect for the whole night. And guess what? It works great for about two weeks, and then two weeks later, just have to start over again.
Scott Benner 1:05:41
Well, I think something you just said really, really sticks with me because I have a number of episodes on how much is enough. And I preach to people that the amount of insulin you need is the right amount of insulin. Not because they ascribe a number to it, or a percentage jump freaks them out. That's another thing that happens to people I get dumped. They love to say it double That can't be right. Well, it appears to be right. And but people get stuck. And when that drags into adulthood. Suddenly, I've interviewed a lot of adults with type one diabetes, they start getting psychological impairments that are difficult to shake. And one of them one of them is a shame about how much insulin they use. Yeah, that's fascinating, isn't it? Yeah, no. So I I've done my best to, to make sure people understand you know, that you just need what you need. Oh, so my daughter 17. She weighs maybe 130 pounds. She is as fit and healthy as you know, a person could be and her her ratios. Her her carb ratio is like one to four and a half. Wow. And that's just how we have our that's what works for her. Now Could I dump a bunch of basil on her and just make sure she eats you know, three times a day and has a snack before she goes to bed? I could. But my daughter also got up this morning. went to high school has not eaten yet. It's 130. Here. I just got a text from her. When are you done? I want to have lunch. Okay, so that okay, and I'm going back on her CGM. I'm going to go back 12 hours, turn my phone landscape and tell you that at 145 in the morning, she was 118 down to 109. I'm now at three o'clock. She's 90 480-893-8591. It's six o'clock. She said school. She's 92. That's it. She's been between 90 and 85. For the last 12 hours. She has not eaten a morsel in that time. Yeah, and that's good. Basil. Right.
Dr. Saleh Adi 1:07:51
That's what but that's that's both the basil way as well as loop and the algorithm. Right. So so but I think it's, I think you also described something which is very key, it's not looking at what her blood sugar is right now is also what it had been over the last hour or two. Because it's a different it. It's when I tell people is with CGM. It's not a blood sugar of 92 anymore. There are five different 90 two's, there's 92 and two arrows up, there's 92 and one arrow up, there's 92 and straight to the right, and two down. So there are five different 90 twos. And each one of them you think about it very differently. And your decision making is going to be different if you have a 92 up versus down.
Scott Benner 1:08:40
Yeah, no, it's just great. Listen, you're allowed to come back on the podcast whenever you Thank you. It every February if you ever like find yourself sitting around the house, you haven't worked in a while and you're like, people need to know about this, you send me an email, get your right on here. Because right, because I really, I can't tell you how much I appreciate your input and your knowledge, especially over all this time. And and for the people listening to I have to imagine it brings them some sort of solace to have you come on with you know, you got quite a quite a long list of bone a few days in front of you. And you really did just say what I say on this podcast for a while and I hope that helps people feel comfortable because I think that you have to dispense with your fear of insulin first. You know, and there are about 1000 other things to understand. And to your point, you can't get them in a doctor's visit. You know you can't bring people together. I think this delivery system for information is great for people because it's at their pace and on their time. And I honestly think if you if you were diagnosed today, and I've seen it a million times already, and you just listened to this podcast. I think you have an A one C in the sixes ease And I, I swear I don't want to do it on here because it'll seem self serving. But I could show you just endless, endless messages about the same thing, people who are diagnosed and find the podcast in the hospital on day one, and will report to me six months later that they don't even understand what. Like when they hear people having all this trouble. They're like, I don't I don't even understand how they could have this trouble. And I was like, Well, yeah, but you you started listening on day one.
Dr. Saleh Adi 1:10:29
Yeah, it's not easy. It takes it takes knowledge, managing type one diabetes, it takes a lot of knowledge. And, and it's acquired the gradually and slowly over time, because it's biochemistry, its biology, its physiology, its food, science, its activity and exercise, physiology and all of those things. And then and then pharmacology when it comes to insulin. And then now we're throwing, you know, software, stuff over, you know, on top of things. So it takes a lot. And it can be overwhelming if you think of it that way. But just take it one step at a time. And look at the data. You have the data, you have tons of data, everyone has CGM data, everyone has pumped you and Bolus isn't insulin, just download those devices take half an hour to just take a look at it and see what makes sense. And if something makes sense. And if it's something doesn't make sense, ask your child, they actually didn't have significant input and insights into it as well.
Scott Benner 1:11:33
I just realized just looking at my at my daughter's data and talking to you. I saw by what the algorithm was doing that her basil could have been a little stronger today because it was taking it away and then Bolus thing and taking it away and Bolus thing for those 12 hours. So if the basil was maybe a tiny bit higher, it might have been able to get away with takeaway and not Bolus, but in the end, it's working exactly the way I want it to. So Right, right. I can't thank you enough. I I invite you if you're interested. Beyond the hundreds of conversations that are in here with people with type one diabetes of all ages, I have a series called defining diabetes that goes through all the tools and in a short way explains what they are. There's a pro tip series that walks you through how to manage yourself. We just launched a variable series. You know, I think the last episode of the variable series was video games. Because, you know, the adrenaline from playing video games for some kids makes your blood sugar go up. I have a great afterdark series with people who have all different kinds of like real world life problems that people who are bipolar, you know, have serious complications there. You know, all this stuff, people that type one talk about it, I swear to you, you listen to this podcast, you're gonna think I ripped you off. So I can't thank you enough for doing this. I mean, this is really wonderful of you to
Dr. Saleh Adi 1:12:58
know I very much enjoyed and Scott, thank you for having me.
Scott Benner 1:13:01
Yeah, and I'm gonna thank the person who sent me your name, even though I don't remember who that was. So if you're listening, you did this. And thank you very much.
A huge thank you to one of today's sponsors, je Vogue glucagon, find out more about chivo hypo pen at G Vogue glucagon.com Ford slash juicebox. you spell that GVOKEGL Uc ag o n.com. forward slash juicebox. I'd also like to thank Dr. Adi for coming on the show. And I mean it sir. If you're listening, come back whenever you like this is fantastic. Lastly, thank you Dexcom for being a generous sponsor of the Juicebox Podcast if you want to learn more about the Dexcom g six continuous glucose monitor. That's at Dexcom comm forward slash juice box. If you enjoy the Juicebox Podcast, please share it by telling a friend that really is the best way to help the show to grow, sustain. And to continue on. Just tell someone, listen to the Juicebox Podcast, show him how to open up a podcast app if you have to show him where the subscribe button is. That kind of stuff is a huge help. Hey, and if you like the show, you might really love the Juicebox Podcast Facebook page. It's a private group with almost 15,000 people in it now, all talking about stuff like we talked about today. Juicebox Podcast Type One Diabetes on Facebook is the least Facebook place on Facebook. I think you know what I mean by that. And if you're still listening, I'm going to assume you're a real big fan of the show and ask you have you gone to T one d exchange.org forward slash juice box yet and filled out the survey. If you haven't, and you're a US resident who lives with type one or a US resident who is the caregiver of someone with type one. Please do that right now. It'll literally take you less than 10 minutes. There'll be a huge help for people living with Type One Diabetes and you'll be supporting the podcast at the same time. T one d exchange.org. forward slash juicebox. That's it for me. Thanks so much for listening. I'll be back very soon with another episode of the Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#540 Diabetes Variables: Stress
Diabetes Variables: Stress
Scott and Jenny Smith, CDE share insights on type 1 diabetes care
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to Episode 540 of the Juicebox Podcast.
Jenny's here today to do another diabetes variable with me. And today's topic is stress. While you're listening today, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making any changes to your health care plan for becoming bold with insulin, know this as well. Jenny does this for a living. If you want to check her out. Go to integrated diabetes comm you can hire her. Hey guys, please don't forget to go to T one d exchange.org. forward slash juice box and fill out the survey you'll be helping people with type one diabetes and supporting the show. If you do that, it really does just take a few minutes. It's HIPAA compliant. Absolutely anonymous, you do need to be a US resident who has type one, or is the caregiver of someone with type one. But otherwise, if you haven't done it already, please go fill out the survey just takes a few moments.
This episode of The Juicebox Podcast is sponsored by the Contour Next One blood glucose meter. Head over to Contour Next one.com Ford slash juicebox. To find out more links to Contour Next One comm forward slash juicebox as well as all the sponsors are right there in the show notes of your podcast player. We're at Juicebox podcast.com. When you support the sponsors, you're supporting the show, so allow me to thank you right now if you've used any of those links, or if you're considering using any of them. Alright, let's get to Jenni. How does stress impact blood sugar's?
Jennifer Smith, CDE 2:12
Do you want to talk or should I?
Scott Benner 2:14
Well, I mean, it seems it seems obvious, but it's not because I've spoken to people who get stressed out and their blood sugar's go down. So I'm wondering what you've seen from people on both sides of this.
Jennifer Smith, CDE 2:30
I've seen more people who have an impact of stress with a rise in blood sugar or an increase in their insulin need. It isn't to say though, and a good friend of mine, her level of stress, just like her level of like adrenaline rush causes her to need less insulin. Okay, like race morning, she is cutting her insulin down while the rest of us are like rage bolusing
Unknown Speaker 3:02
blood sugar.
Jennifer Smith, CDE 3:03
She's like, what do you guys all doing? Like you're sitting at like 82 like going down? down this high. Right? But yeah, I mean stress the same thing. For the most part stress will cause a rise in blood sugar relative to that like mental strain. It's kind of putting I mean, and then you have to determine the type of stress right? Is it a mental stress? Is it something that you're really working through? Is it a lengthy stress like several days worth of something happening? I mean, one stress I can say personally really increased my insulin needs was when my dad passed away, okay. I mean that week with going to family helping my mom out with a week and a funeral and everything in the process. I was using like a 75% temporary increase in my basil. Okay,
Scott Benner 4:00
well, it was a lot I'm looking here and long term stress can increase depression caused headaches heartburn, insomnia, weakened your immune system. Make your breathing rapid puts you at a risk for a heart attack. It can bring up your blood sugar, your blood pressure, pounding heart fertility problems, stomach aches, low sex drive, erectile dysfunction, miss your periods, tense muscles and high blood sugar. Yes. So when you're under stress, it is not healthy for you know, that's obvious, but it actually can impact your blood sugar. And I don't know if people would consider that or not.
Jennifer Smith, CDE 4:37
Yeah, and you know, in terms of that effect, you also then have to look at the length of time that the stress is going to happen for and if it's already impacted these other health pieces. If you've ever been under significant like work related stress in the past year, then you may have caused injury really too many other pieces. Have your body which until they get healed is likely causing inflammation and inflammation in and of itself also increases blood sugar increases your insulin D input increases resistance to insulin. So stress is bad.
Scott Benner 5:18
And well, I guess what I'm thinking is, like we talked in other variable episodes about, like, you know, I said, My daughter gets into the shower and her blood sugar goes down where a lot of people, you know, would say that might be heat, I kind of think that she's relaxing. Sometimes I think of it that way, like, and can you just chill out? And is that possible in our society, the way the way our days are set up, right? Like this is way more about, you know, your general health than it is about maybe blood sugar health, like sure. stressful moments can make your blood sugar rise, you should be aware of that. I've seen notes from people who have car accidents fender benders, right? And boom, you know, their blood sugar goes up, you think, well, that might be adrenaline, but then it stays like that for hours and hours. And if that's
Jennifer Smith, CDE 6:03
more that fight or flight, that's, that's
Scott Benner 6:05
okay. But yeah, I mean, I realized that this is somebody telling you be generally healthier, and you'll be generally healthier, which is obvious. But it's, um, stress can cause your liver to release extra sugar into your bloodstream, which over time puts you at risk for type two by diabetes. This is telling me here, meaning that if you're a long term stress, you're hurting yourself long term. Right? Wow. So is I have to say I use a breathing app on my phone. It's really helpful. I mean, just got one on my watch. Yeah, yeah, a couple times a day, it, it pings me, and I spend 60 or 90 seconds doing some sort of in and out breathing. It's kind of nice. I mean, I'm sure it would be better if I moved to Wyoming and lived on a hill and a cabin, I'm sure I'd be less stressed. Although I gotta be honest with you. I'd the entire time I'd be like a bear is about to kill me. I'd be incredibly stressed out by that. But you have to find a way to overall lower your stress. But in the moment, so in the moment when it happens. Do we Bolus weren't
Jennifer Smith, CDE 7:13
in the moment for stress is kind of like the adrenaline Bolus consideration, right? Do I Bolus for the stress in terms of like the car accident example. And my blood sugar's now shooting through the moon, you could Bolus at least minor amount. Because obviously, the incident as well as the skyrocketing blood sugar is not going to create anything that's more even flow. It's just gonna keep increasing your anxiety.
Scott Benner 7:45
Let me ask you a question. A personal question before we wrap this one up?
Jennifer Smith, CDE 7:49
Yeah. Do you?
Scott Benner 7:51
Are you so in tuned with yourself? That you always know because it's unfair, like you're here, like this front facing image of you is Jenny, who knows about diabetes, but you're a person to like I actually want to do and I want to interview completely about burnout just one day, like, like, away from all this, like the baby stuff. And but if you're stressed out, if your kids are struggling with something, and your husband's being a jerk, and somebody else is doing a thing, like Do you notice that? And how quickly Are you able to say to yourself, my life is more stressful right? Now I need more basil? Like does that in a real world situation? Does it work?
Jennifer Smith, CDE 8:34
in a real world situation, if you have enough awareness of everything that's happening, it can work to use a temporary increase to basil. I mean, many people I know who are using a pump, you know of whatever kind of pump you're using, have either a basil profile that may be termed stress, or they have a temporary basil kind of setting that's specific to stress increased need. I've got an override that's already programmed for stress. Thankfully, I don't use it very often right now. It has happened. I mean, in terms of like life, things happen, you know, somebody might need some additional help in the family. And beyond that you don't have time to take off of work. So now you're juggling and juggling and sleep, you might get three hours a night instead of your eight hours a night and that can definitely increase you know, but personally, yes, I've, I feel like at this point, I know myself well enough to be able to say my kids spilled the milk all over the table. That's not going to cause my blood sugar to go to 250 I'm just gonna tell him to get a cloth and clean it.
Scott Benner 9:49
I asked because I've become much more in tune with the idea that people have anxiety since I've been doing the podcast because I am a person I get up in the morning. You know what I'm thinking about nothing. I go do the thing I'm supposed to do, I do it as well as I can, if it works out great. If it doesn't, whatever, you know, and I move on, right? But I see my wife get out of bed. And she, you can like, look her in the face. And she's going through a checklist already. She knows what's happening today. And if what's happening today is something she feels like she can't keep up with. It stresses her out. And I've just talked to too many people at this point, who live in that reality. And I just wonder. I mean, it's, it's too simplifying to say to them lower your stress, because they're like, yeah, da, thanks. I can't, you know, so. I don't know. Just
Jennifer Smith, CDE 10:41
I know myself, you know, in terms of like, as you asked me, personally, I know myself enough to also say that I'm kind of like your wife in terms of like the morning time. I'm German. I'm a little bit like, like strategy, figure it out, apply it kind of you know, so in the morning, especially on the weekdays, I know my checklist of things, I have to do this, I've got this many people to talk to, I've got to attack emails, I've got a project, I've got a podcast with you. I've got, I've got this checklist of things. And I keep moving through it through the course of the day. But a stress to me, that would increase like my need for insulin overall would be something major happened to like a family member, and it's blowing all those things on my checklist, like they're now off the list. And like this is an immediate and I'm like, okay, must assess and redo and plan differently. And I
Scott Benner 11:43
only worry about my kids and my wife like that. I don't worry about anybody else. Like when I get in bed at night, I can see Kelly going through that like wind down thing she does. Like I feel terrible. Because all I'm really concerned about what is like are the blankets where I wanted to be and do I have my pillow flip the right way and is my phone on its charger. And once it is on like goodbye. And then I'm just asleep. where she's, you know, trying to decompress and trying not to think about tomorrow. And I feel terrible for anyone who's caught in that because it really is, it really seems like a place he can't get out of
Jennifer Smith, CDE 12:20
you. In terms of like overall stress that's I use that that breathing app like you talked about, I use that because especially in the evening time I really tried to stay away from like, technology itself, right within about 30 minutes of actually like getting in bed and trying to like fall asleep. Because that I found is a big impact for me. I have like one of those mindful adult coloring books.
Unknown Speaker 12:50
adult coloring book, it's just kids,
Scott Benner 12:56
let me clarify for Jenny. They're there. Because my wife actually has these two. They're very intricate, pretty pictures, not naked people having sex. I got your
Jennifer Smith, CDE 13:05
intricate pretty flowers and deer and fish. And yes, there was funny to watch you catch yourself. Anyway, but things like that to kind of do that decompress. And while my brain has an idea of what's coming in the next day, I'm really not too like focused on it until the next day, because I've found that I don't sleep.
Scott Benner 13:27
Here's an interesting question. And I will let this go after that. But say I'm pre diabetic, right? I'm like, type two diabetes is coming for me. And I'm also an incredibly anxious, stressful person. Is there a world where and I'm not pushing medication. But if a doctor prescribed like, like an SSRI or something like that, to take care of the anxiety that as the anxiety went away, and the stress went away, the blood sugar impact would go away as well, to some degree, I mean, could you get some win out of that?
Jennifer Smith, CDE 13:58
You could get some win out of that. I mean, we always try to encourage people in terms of like lifestyle change to actually make a lifestyle change rather than a medication addition. But yes, in all, whatever type of stress reduction you put into play, could have enough impact that that person on the path that they're on whatever stress management strategy they're putting into place could make them turn the road down the path that's going to prevent that now they're going to have to continue whether it's now I start taking a mile walk every morning, because it decompresses me, I think through what's coming for the day, and I'm ready, maybe they choose to start eating broccoli now rather than a handful of potato chips at lunchtime. So there might be other little things that they could do along the way that impact the stress that's on their body helps them to feel better or decreases the chance of type two or any other health condition itself, which in and of itself is a decrease for anxiety as well. Right? If you know you're doing something good to prevent something,
Scott Benner 15:05
even if it bolsters you, I have to say it would be criminal Not to mention in a even in a short conversation about stress, that activity, you know, of any kind is, is really good for your mental health, it just really is. So, okay, well, thank you very much. Friends, if you're enjoying the variable series, I'm going to list all of the available variable episodes in just a moment. But first, I need to tell you actually, I want to tell you about the Contour Next One, blood glucose meter, you know, bare bones, simple cell, it's really, really accurate. And that's incredibly important, especially in a world where sometimes we just get the meter that someone gives us, you can actually make a choice, you can choose an accurate, reliable meter. And the Contour Next One, in my opinion is exactly that. Not only is it easy to carry, easy to read, easy to see at night, but it has Second Chance test strips. So you can go in for some blood, get some but not enough and head back for the rest without impacting the accuracy. We're ruining the test trip. I don't know what else you want in a blood glucose meter. I mean, if you want it to be Bluetooth enabled so that you can launch an app on your phone and see your records. It does that. And it works fine if you don't want to use the app. So there's a lot of flexibility in there for you lets you choose. I mean, really, it's just a great meter. So why don't you check it out, it's super simple to look into Contour Next one.com, forward slash juicebox. He may be eligible for a free meter, there's a test trip savings program that you might find eligibility in. And it's possible that all of this could cost you less in cash than you're paying right now for your current meter through your insurance, I think I'm not sure. But it could work out that way. And if not let your insurance pay for Contour Next one.com forward slash juicebox. If you have to have a blood glucose meter, you might as well get a good one.
First, I want to thank Jenny for lending her expertise to the shell. Don't forget, you can find her an integrated diabetes calm. I want to thank you for listening. And I'd like to remind you that there are others in this variable series. trampolines, temperature travel, exercise, hydration, food quality, leaky sites, or tunneling video games and today's stress. There's one coming every week, this variables list is compiled by listeners just like you, we did it over on the Juicebox Podcast Type One Diabetes private Facebook page, if you're not a member, you should go check it out. We do stuff like this all the time over there. Listeners just like you made a list that is so long that there'll be variables episodes coming for ever I feel like but for now, just once a week, I'm gonna let you go in just a second. But if you're not part of that Facebook group, I wish you are. It's private. And it's full of people just like you. It's a matter of fact, I think this month, September 2021, I'll be celebrating 4 million downloads of the Juicebox Podcast. And I think I'm gonna do it with a like a q&a, I'll probably just jump on Facebook Live, or do it through zoom or something like that. And if you want to know about that, I'll be announcing it there. So I hope you'll become a member. There's you know, it's absolutely free, obviously. I mean, I hope that's obvious Juicebox Podcast, Type One Diabetes to private group, you'll have to answer a couple of questions to prove to the algorithm that you're a human being. And then after that you'll be in and talking to other listeners, just like you. Hey, thanks so much for listening, and for supporting the show. I really appreciate it. I'll be back soon with another episode of the Juicebox Podcast. Please continue to share. Subscribe in a podcast app, tell a friend. Leave great reviews wherever you listen, that kind of stuff is all very supportive and super, I mean helped it. Take the T one D exchange survey. Support the sponsors. All right, that was choppy at the end, but you get the point. I appreciate you. Thank you so much for supporting the show. I'll be back soon.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!