#433 Diabetes TrialNet
Carla Greenbaum, M.D. Returns
Carla Greenbaum, M.D., chair of TrialNet returns to the podcast to discuss research and type 1 diabetes risk screening. Get your FREE screening kit here.
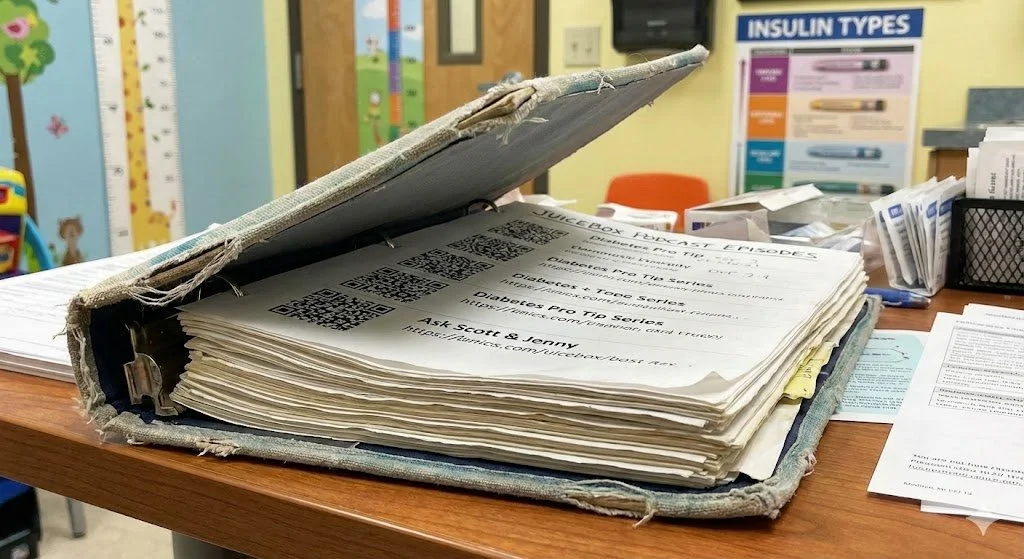
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome to Episode 433 of the Juicebox Podcast. Today's show is sponsored by Omni pod makers of the Omni pod tubeless insulin pump, and they'd be happy to send you a free no obligation demo, all you have to do to get it is go to my Omni pod.com Ford slash juice box. And if you are looking for the most amazing continuous glucose monitor that I've ever seen, you're looking for the Dexcom g six continuous glucose monitor. And you can learn more about it@dexcom.com forward slash juice box.
Today we're going to be hearing from a returning guest, Dr. Karla Greenbaum, who happens to be running things over there at diabetes trial net. I really enjoy talking to Carl, I didn't realize how much I'd missed her until she got back on she's a real easy way about her. And I find it enjoyable to speak with her. So she'll be on in a moment to tell you all about trial net. But let me just tell you what it says right on their webpage trial net.org. Imagine a future without Type One Diabetes trial net is an international network of leading academic institutions, endocrinologist physicians, scientists and healthcare teams at the forefront of Type One Diabetes Research. We offer Risk Screening for relatives of people with type one, and innovative clinical studies, testing ways to slow down and prevent disease progression. Our goal is a future without type one diabetes. All right now let Carl explain to you what all that means. But trust me, this is not just some dry like oh research, you're gonna want to hear this. Please remember, while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making any changes to your health care plan.
Dr. Carla Greenbaum 2:06
I do want to say that, you know, me personally, I'm in the wrong generation. I don't really do a lot of social media. I don't do any stuff, really. But I get reports from the team all the time. And they're always highlighting, like who do people listen to? And you guys are there all the time? It's really, it's pretty cool. What you've created. I think it's pretty amazing. Actually,
Scott Benner 2:26
no, I I still I mentioned trial net all the time. When I'm talking. You know, especially when you're talking to parents who have you know, or prospective parents who have type one, but don't have kids yet. I always ask them I'm like, you know, would you look, you know, what would you think? I've gotten very, very thoughtful answers on both sides back from people. Yeah. But anyway, I guess like, let's just start with, just, you know, obviously, I'll do a lead up to it at some point. But sure, just tell me who you are. Give us your credentials and tell us about trauma.
Dr. Carla Greenbaum 2:58
So Carla Greenbaum, I direct the center for interventional immunology, and the diabetes program at benaroya. Research Institute here in Seattle. And I also am the Chair of diabetes trial net.
Scott Benner 3:15
And you've had this job for quite some time now. Right?
Dr. Carla Greenbaum 3:18
I have good. I've been involved in trial net. And actually, it's preceding study that diabetes prevention trial since the early 90s. And trauma, it started in 2002. And I was Vice Chair for a number of years, and then I've been chair, I guess I should remember about six or seven years now. Wow. That's terrific.
Scott Benner 3:37
So tell us tell me, I guess the the overarching goal of trial net is like, what's the Yeah, what's the thing? Yeah,
Dr. Carla Greenbaum 3:46
that's a good way to start that So first, maybe just say that, you know, what is trial debt? Right. It's, it's NIH funded your tax dollars, international clinical trial network, whose job is to save beta cells. And we do that both before diagnosis to the idea about prevention. And we also do studies, you know, after diagnosis to save whatever beta cells they're left. And, you know, I always think about that that's really the mission. But the secret to what we really do, or the hint to that is in our name of trial net. We're all about doing trials, that's our essence. That's what we're all expert in. And that's what we really, you know, aim to achieve.
Scott Benner 4:29
So if, you know, so I guess on some levels, you need people's samples who already have diabetes. And you also like, I know you tested my son. Long time ago now about eight years ago, my son got tested and did not have any, any bodies that that indicated that he might have Type One Diabetes one day. And we had to go into his my daughter's endocrinologist office to get trialnet drawls, is that still how it all works?
Dr. Carla Greenbaum 4:59
No, it's complete. difference was a great question. So maybe I should step back for a minute and just put the frame around this. So trialnet screens people for the risk of diabetes through our pathway to prevention study. And you can think about that as the funnel, it's the way to test an awful lot of people to find the few people who are unfortunately likely to develop diabetes, because that's really the people that we want to try to see if we can stop or delay the disease. So the first step is this pathway to prevention, which is screening. But as you're talking about, you know, in the old days, you have to go in and get your blood drawn, and you had to go into only a selected number of places. But now, you actually can get tested by going online and doing a consent online and you'll get a kit sent to you. You could test your with a kid at home, you could do that at home, and you put it in a kit, and FedEx comes and picks it up, and it's all free. So that is really a huge difference from sounds like when your child was screened A number of years ago.
Scott Benner 6:04
No kidding? How long? Have you been able to do it that way?
Dr. Carla Greenbaum 6:07
We've been doing that now for a couple of years. I would say of course, during this year of COVID, it markedly increased. So certainly during this past year, I'm guessing don't quote me exactly, but at least 60. But up to 70% of all people being screened are being screened by doing this online, simple home delivery system.
Scott Benner 6:26
Does it cost anything? On my own?
Dr. Carla Greenbaum 6:28
No. Well, it costs your tax dollars, but it doesn't cost you to participate.
Scott Benner 6:33
I just think that's really important piece, I just ignore what I pay in taxes every year trial net is free.
Unknown Speaker 6:38
Exactly, exactly.
Dr. Carla Greenbaum 6:39
But that's that that's really an important thing, right? We are NIH supported. And all the work that we do is free to any participant, not just the screening, but the follow up, you know, consultation with people who are experts about diabetes and diabetes risk. And all the monitoring, we do to look to make sure whether people are progressing in their disease or not, and participating in all the trials all that?
Scott Benner 7:05
Well. So if I'm making up things now, but if I, I send my you know, if I have type one diabetes, and my brother's like, well, I want to see if I'm gonna get it, we find out he's got some markers, and how many markers are there?
Dr. Carla Greenbaum 7:17
Yeah, that's a great question. There are up to five antibodies that are associated pretty reliably with Type One Diabetes. And so trial that will test up to all five, we don't test all five right away, we test two and then depending on those results, we will test on others. But that's what we would know, people who have only one antibody, they just come in on an annual basis to see whether or not or they come in to provide another blood sample to see whether they are developing more antibodies. Because everything we know now suggests that it's really having multiple antibodies that really puts the individual at risk for progressing. So that's our, our main group that we're looking for it Atlanta, buddy. So
Scott Benner 8:01
if I have multiples, so my friend yes scenario has multiples is what are some of the ways that you try to slow the progression down?
Dr. Carla Greenbaum 8:11
Well, the first thing when somebody has multiple antibodies is that we asked them to come in to do a test to see where they are on that path, right? whether their blood sugar's are still completely normal, or whether there's anything already abnormal, because that tells us which clinical trial that might be eligible for. So currently, we are running two different clinical trials for people that have multiple antibodies. One is using a drug called a bad acept or redsea. And that trial has been going on for quite a while now. And we're actually anticipating having the results of that trial before the end of 2021. And the second trial, the one that we're still recruiting for is using a drug called hydroxychloroquine, which has nothing to do with COVID. For the purpose
Scott Benner 8:59
of our study, we now all know what it is.
Dr. Carla Greenbaum 9:01
So yeah, we now would, but the good news is it is an oral medication that people can take. And so people who have multiple antibodies, and have normal glucose can be in this study. And the idea is to figure out whether hydroxychloroquine can slow or delay people progressing to getting diabetes. And it's a really interesting drug because it's been around for more than 50 years for totally other purposes. But it is now widespread use for people who live with arthritis, which of course, is another autoimmune disease like diabetes. And that's true in both kids and adults. So there's lots and lots of information about this drug. And all of that suggests that it could slow disease if it's given early on. And so that's why we're doing that study. And that's ongoing right now.
Scott Benner 9:52
Is that medication, what is what it does centered around inflammation.
Dr. Carla Greenbaum 9:56
Yes, yes. So to a certain extent hydroxylase When works about me how to explain this, there's different of course arms of the immune system. And one of the early steps in autoimmunity we believe is what we call turning on the innate i na te immune system, which is like your immediate response. And this is what we think hydroxychloroquine interferes with. And it's why we hope it can slow the disease.
Scott Benner 10:27
If If a person has multiple antibodies, is it? Are they definitely going to get Type One Diabetes at some point? Or is that not
Dr. Carla Greenbaum 10:36
the case? That's a great question. Because, as you know, this whole notion of stages of diabetes, which means that once you have multiple antibodies, and you have normal glucose, you're at will be called stage one diabetes. And if you have multiple antibodies in your glucoses, are not quite normal that stage two, and stage three is what we used to call new onset diabetes. And that whole framework was really based on all the studies that do suggests that unfortunately, once you have multiple antibodies, it's extraordinarily likely that you will get clinical type one diabetes. Now the important piece that people often miss, it doesn't tell us when you're going to progress to getting type one diabetes, some people may live with multiple antibodies for a long time, and other people will get diabetes in a short period of time after the antibodies appear. So it's the antibodies that tell us who to test further to see who's going to be getting diabetes sooner to see about who could be in our trials. Gotcha.
Scott Benner 11:43
And this is just a point where I mentioned we're talking about type one in case,
Unknown Speaker 11:47
yes,
Dr. Carla Greenbaum 11:48
type one diabetes. And, and, you know, I should say that the, the study that tronic conducted, where we showed that one of the drugs that we tested lism ab could slow progression in people that were at risk for getting diabetes. You know, half the people who had received the placebo, got diabetes very, very quickly, within two years. So when I say that just having antibodies doesn't tell us how long it takes you to get diabetes, it's really having antibodies and doing these other tests that we can help give you information.
Scott Benner 12:22
You know, I have to say that I've now interviewed a number of people who have gotten it in their 60s. Yeah, and I feel like, a decade or two ago, someone would have told you that was impossible. Yeah. But yeah, just I've just talked to too many people who who've had it happen. And and I think at this point, now, if I should have made a flowchart at one point in my life, I've probably spoken to somebody who's been diagnosed at every age between one seriously between the newborn and like, in their mid 60s. So yeah, nobody ever. I mean, don't get me wrong, there's, you know, there's sweet spots, it seems like where people like, you know, they're all like, always, like, 28, or just getting ready to go to college, or, you know, like, there's, there seems to be, I mean, this is very unscientific, but there's there seems to be some sweet spots where it happens. But I, I've had somebody say, every age that I can think of, so
Dr. Carla Greenbaum 13:14
you're absolutely correct. So what you talked about the sweet spots is what we what we talk about by modal distribution, that's a fancy science word, which basically says, if we look at when people get diabetes, there's sort of the group of people, they get it really sort of pre puberty, kind of six to 10 year old range. And then there's another blip around puberty, that people get it. But then we do know, people like you found right people get diabetes, it also Type One Diabetes at all stages. What we don't know, for example, is somebody let's say they have just one antibody. Now, people with it, we test to only have one antibody, we know about 20% of them, will develop more than one antibody after about five years. But we don't know if the other 80% will eventually get multiple antibodies, or will develop diabetes with having only one antibody decades later. We you know, because we haven't followed people 60 or 70 years, right? We don't know that for sure. Wow.
Scott Benner 14:22
What about having other autoimmune like if you have a different autoimmune issue and have an antibody? Does it change your your odds?
Dr. Carla Greenbaum 14:30
What changes your odds is your genetics, right? So your genetics is what sets up any autoimmune disease. And if you have another autoimmune disease, that means you have the genetics that puts you at potential increased risk. But once you have multiple antibodies, diabetes related antibodies, the genetics don't seem to matter that much. So it really the genetics tells you, who's going to give you who's going to have antibodies Not who's going to progress once you have antibodies. Milan, go, I'm sorry, I'm sorry.
Scott Benner 15:04
No, I didn't mean to stop you, if you have something else, thank you,
Dr. Carla Greenbaum 15:07
I was just gonna say that's really why trauma focuses on screening relatives, right? Because we know that's a genetic screening test. If you have a relative with diabetes, that means the genes are in your family more concentrated. And if we screen, you know, we will find about one out of every 50 relatives will have multiple antibodies. It is true that people who never had a relative will get diabetes, but we'd have to screen 750 people who do not have a relative to find that one with multiple antibodies. That's interesting.
Scott Benner 15:42
Let me ask you this. If Can I pluck two people off the planet who are married, and we screen them and find out if their children have more or less of a chance of having type one?
Dr. Carla Greenbaum 15:53
Hmm, not really, because the genetics give us I think what we call a fertile field, right? They give a probability. But they're not like genes that cause particular kind of breast cancer or Huntington's chorea. In other words, monogenic diseases, right? They don't, they don't say you're going to get it. So we could give some ideas, but we can't give enough information. We know some genes that are associated with getting diabetes, but there's a lot of people who have those same genes who never will. So genetics alone doesn't help us. On the other hand, as I mentioned before, we do know about what happens in relatives. So if you're an identical twin, the risk is very high. If you're a child of a father with diabetes, the risk is higher than if you have a mother with diabetes. So we do have that kind of subtle information.
Scott Benner 16:48
Are you learning about? How does diabetes skip generations? Or? Or is it just random? You know, Scott,
Dr. Carla Greenbaum 16:56
it's so funny how often people ask me? No, it does not skip. So that is not true. I don't know why people get that idea. I hear it all the time. But
Scott Benner 17:10
it's just anecdotal. Because probably what you just said is you're more likely if your father has than your mother has. So yeah, maybe your father has it. You have a daughter who doesn't have it, who then has a son who then does have it and then it makes it feel like it's skipping agenda.
Dr. Carla Greenbaum 17:23
Yeah, yeah, you're right. I mean, I don't mean to be No, no, I don't mean to be polite about it. But in general, No, unfortunately, that's, again, why we screen first degree, family members that his immediate family will screen people up until age 45. Where second degree, we actually only screen to age 20. Because the rest becomes lower. The further genetically you are from the person with diabetes.
Scott Benner 17:53
After the obvious goal of helping people who use screen and find what are other goals of trialnet, like, what else am I helping?
Unknown Speaker 18:01
Mm hmm,
Dr. Carla Greenbaum 18:02
great question. So one of the things is that we're helping is that we are providing hope and support for people, right? If you have somebody with diabetes in your family, you know, you are worried about other people in your family. And most the time, you'll get pretty good news, right? Because only about 5% of people will have antibodies. But if somebody is antibody positive, you know, we're kind of there for them. Right? It's like, when a physician has to give bad news to anybody. This is bad news to let people know that, you know, unfortunately, now you have multiple antibodies, but we're there to monitor and follow them carefully. And, and provide opportunity, and to have them prepare if that diagnosis will occur if a trial is not available for them. But on a broader scale, what we provide, and what participants provide to everybody else in the future is, every bit of data we get from any study we're doing is really laying the foundation for the future studies. So trial that was based on some of the studies that were literally started in the 80s, where we studied every family member we could find to measure everything we possibly could. And that's what led to this whole notion about what what predicts risks. So we learn about the Natural History of the disease, we get a better understanding of who's more likely to respond to certain therapies. You know, we really learn a lot from everybody who participates.
Scott Benner 19:33
Yeah, it's, I find it encouraging and whimsical to think about that somebody started something in the 80s that's helping somebody in 2021. Yeah, and I can see how also somebody would think that and go, Oh, great. So they'll figure this all out. 10 years after I'm dead, but but but you really are in. What it reminds me of is that I interviewed somebody who works at NASA recently. I ended up asking what does it feel like to be involved in something that you may never see the fruition of your work? And I guess I feel drawn to ask you the same question.
Dr. Carla Greenbaum 20:11
Well, I'll have to throw in a famous Tom mutek, saying for the Jewish tradition, we're towards the Hasidic story, which basically, somebody goes to this old man who's planting a tree, say, What are you planting the tree? For? You're not going to see it happen? He said, Nope. But my grandchildren will. And that this is all about, you know, thinking beyond myself, and thinking about the future. And that's what we do. I mean, all researches this way, we all have little, little pieces in this puzzle. And you know, the cliche of standing on someone else's shoulders is what we do. So I must say that I'm super excited in my research lifetime, how much has happened, right? We went from not knowing what could predict. And now we can predict. That was like, we couldn't do that before. We went from not having anything to do about it to now we have a therapy that's now been shown to stop diabetes. Now, in fact, there are seven different therapies now that can alter the disease course in diabetes seven. There Were None that long ago. So it's a little piece of the puzzle. We haven't gotten to the destination of curing diabetes yet. But boy, we've made a lot of changes.
Scott Benner 21:29
Yeah, I always imagine that. That the end goal for all these different things like you can use curing diabetes as an example. But the end goal for something, I imagine will never be reached the way the person in the moment now thinks it's going to be reached. Yeah. Do you find that you learn things along the way that reframe your thinking about how to reach that end goal?
Dr. Carla Greenbaum 21:55
I love that. That's a great, that's a fabulous way of thinking about it. I
Scott Benner 21:59
think, Carla, I don't even smoke weed. I just came up with that. I was
Dr. Carla Greenbaum 22:02
just gonna say that's like, totally, you know, 60s thinking now I'm teasing. I would say the answer to that is, whereas much of science progresses in increments, right, where we build on an observation somebody made. And we test that further, we build on another observation. There are certainly times where there are paradigm shifts, right? where somebody came up with a whole new way of either looking at the same data or has a new tool to measure something differently. So you're right. I don't know what the future of this is going to look like. I hope there are clever people in the future, who will, you know, change the paradigms a little bit and advance things even further.
Scott Benner 22:49
Yeah, it just, it makes you feel inside. If you're being whimsical, that one day someone will be able to say, Oh, you have an antibody in your, in your system that you don't want, we'll just take it out. We'll put this thing. Hey, kills it, you know,
Dr. Carla Greenbaum 23:03
you know, like I said, I'm old enough to know, when the whole idea when, when Amazon was first starting to sell books online. You know, I live in Seattle area. And I was telling and there was an opportunity to invest. And I was telling my husband, that's ridiculous. No one's going to give a credit card to somebody online.
Scott Benner 23:22
Well, I yeah, I don't know that people understand. It's funny. We were just talking about this in my kitchen, the other day where I was explaining to Arden, how quickly technology like builds on top of itself. Yeah. And you know, I stand around with my kids who are 16 and 20. And I told them the story I said, you know, when I was 13, I bought the most advanced consumer computer that existed. And I was like, I took it home. And I bought a book, a book at the bookstore that had code in it, I spent an entire day of my life. Looking at the book, typing in this code, he went on forever and ever and I got done. And I pushed Enter, and nothing happened. So I went back and I read the book and looked at the screen, and it took me hours upon hours and I found my typo, and I fixed it. And I pushed enter and a stick figure did one jumping jack on the screen and stopped. And I have to tell you, it was the most amazing thing I'd ever seen in my life. Alright, let's get into these ads and get back out quickly short episode short ads. The Dexcom g six continuous glucose monitor will show you the speed and direction of your blood sugar in real time. It will stop you from having to do finger sticks to know what your blood sugar is. And it will allow you to make decisions about insulin and food in a more precise and targeted way. And those decisions can easily lead to more stable blood sugars. Just imagine knowing how to balance your insulin against your food or seeing a small Lo come up and not over treating it with food because you can kind of watch it happen say, let me just try drinking a half of this juice box instead of the whole thing. This is amazing. On top of that, you can have up to 10 followers so somebody can be wearing the Dexcom g six and share their blood sugar's if they want with up to 10 followers. This is for Android or iPhone. And it's fantastic. I can get my phone out of my pocket right now and tell you what Arden's blood sugar is. And it is 119 and it's stable. I can see it's been stable for quite some time, that quickly if Arden's blood sugar leaves the range that we've set, which interestingly for this is 120 or 70, I'll get a little alarm and a beep beep Arden's blood sugars going above 120. And then we make a small adjustment to her insulin and bring it right back again, there are almost countless ways that you can use the information coming back from the Dexcom gs six, why don't you head over to dexcom.com forward slash juicebox. And take a harder look at it, see if it isn't something you think you might enjoy. And if you're a US military person getting your insurance through the VA, I think you're going to be super happy with the coverage. So you guys should head over to there's a quick little form to fill out and Dexcom we'll get right back to you and a ton of information that you can look at on your own. Speaking of forms to fill out, if you go to my Omni pod.com forward slash juice box, you can fill out a short form that will result in an Omnipod demo coming directly to your house. There you are a loved one can try it on and wear it and see what it would be like to wear a tubeless insulin pump not to be connected to any tubing or controllers and still get the delivery of insulin that you deserve meaning bezels while you're bathing while you're swimming during activity, being able to fine tune that basil insulin right not just inject it once a day and hope for the best. But be able to create basil programs like I don't know I want point five an hour from midnight to 6am. But at 6am I want it to be point seven or whatever you're in control of that. You're also in control of temporary basil increases and decreases extended bonuses and all kinds of ways to help with your insulin delivery to again be more targeted to your needs. Plus, it's tubeless. So you're not going to get wiring, wiring, you're not going to get tubing caught on doorknobs, dresser handles, or have to take it off to babe swim or be active or do adult activities. My omnipod.com forward slash juicebox get that free, no obligation demo sent to you right now let's know what I'm saying free, no cost to you. No Obligation means you don't like it doesn't matter. That's risk free in my opinion. There are links to Omnipod Dexcom and all the sponsors at Juicebox Podcast comm right there in the show notes of your podcast player or you can type them into a browser, my omnipod.com forward slash juice box dexcom.com forward slash juice box. And while we're talking about links, don't forget that they're not a sponsor. But Carl is here today sharing the news. So trialnet.org
a stick figure did one jumping jack on the screen and stopped. And I have to tell you it was the most amazing thing I'd ever seen in my life.
Dr. Carla Greenbaum 28:38
Yeah, well, I would say that, you know, the advances that happened in science are obviously not as touchable for the average person. Like all the technology has changed our world. But But if you look back with a little bit of a broader lens, the difference between what science has brought to healthcare and medicine now versus when I was at med school, which wasn't that many centuries ago. It's night and day. Yeah. And so I really do believe in science.
Scott Benner 29:08
I have to tell you that when when my son was two, so we're about 18 years ago, I'm 49 let me do the math real quick. I think that made me like 36 or 37 ish in there. Maybe 47 Nope, nope. 27 or 21 There we go. My appendix almost burst. When my wife was a child, she had terrible ear infections. And when my daughter was two she got type one diabetes, and you can go back in time not that far and make the case that all three of us would have died. We wouldn't be alive today, you know without just yeah, basic things that have moved forward. Yeah. Yeah. Really fantastic. And yeah, it's just I've always been thrilled to tell people about trial that and I and and then we get into that space right where Yeah. I do believe that people need to understand the benefit of finding out that they have the antibody. Yeah, because I get afraid that when people hear about it, they just think, well, I don't want to just worry, like, wait for the other shoe to drop. And I've also heard people thoughtfully say, guests on the show. Listen, I have type one diabetes, I've had it for 30 years, there's nothing wrong with me, I have a very normal life. And my kids could have a normal life too, if they had it, except the idea that you could maybe take a pill that could exponentially slow the, the onset down or even stop it. I mean, that's, that, to me, is where the exciting part is?
Dr. Carla Greenbaum 30:31
Yeah, I mean, I, I again, look, participating in research is not for everybody. And it's really hard to do it when you're making decisions for your children, for example, as compared for yourself, right. On the other hand, you know, all the money in the world is not going to bring progress if we can't have people participating. So every single person who stepped up to participate, just is accelerating our ability to test new therapies and to find new things. And, and yet, I know it's, it's a challenge. I guess, the only other comment I would make is that research in other areas where families have one child with a chronic disease, for example, has well documented that the other children in the family are wondering about them getting it as well. So sometimes parents say, I don't want to scare my other child, I don't want them to think that they might be at risk, what we know from all sorts of other studies that they're thinking about that anyway, whether they're saying it out loud or not, right. You know, and, and the other thing is that, you know, going back to the 60s, you know, knowledge is power. So I think, when people know that they're antibody positive, there's obviously a sorrow and grieving process around that. But it's such a wonderful opportunity to be able to prepare. And to, to not have to, you know, end up in the hospital with DK or something,
Scott Benner 32:00
no matter how many people I speak to, who are mis diagnosed type two and eventually find out their type one. Yeah, they all, I think I really mean all of them eventually say, it is better to know, than to struggle, or to wonder if they use words very similar. I've never heard anyone say, you know, I would have liked to have gone on thinking I had type two diabetes, when I really like one. And I'm just a big fan of that, like, in my mind, a bill comes whether I think I can pay it or not. I opened it up to find out what it is. Because now at least I know, you know, staring at the envelope closed it, you know, you can't you don't forget it's there. You just putting off the inevitable and maybe, you know, I don't like you know what, maybe I opened it up and realized, Oh, my God, I paid too much last month, this is a freebie I get the whole month of thinking I wonder bills paid already, you know, just yeah, to me. mindset. Yeah,
Dr. Carla Greenbaum 33:00
let me let me throw out a number for you, you know, for you and your your people listeners to think about this, that there's about 40,000 people that are newly diagnosed with Type One Diabetes every year in the United States. If three of each of them had on average, three relatives, that's like 120,000 people, right, which would be 3000 people that would be identified potentially, who have multiple antibodies. If we had that group of people regularly, we would be able to do all the trials much more quickly. And we get the answers much more quickly. That would help everybody
Scott Benner 33:39
people who hopes ever again, I have to say not to mix my apples and oranges here for a second. But I support the T one D exchange. And I sometimes struggle to explain to people why that's important, like, you know, to say to somebody like Oh, they you know, they took data and may and that helped the ADA bring down the a one c guidelines for children. And he hear that and it could it could be very easily you can hear that and go, like, why does that matter? But it but it you know, but it does matter? Because when the ADA says, Look, this should be a target, that every endocrinologist in the country reframes their idea of health. And, and even though it's a slow, you know, it's like, it's like turning, you know, turning a battleship. Eventually that means that everybody gets more targeted information about how to manage their blood sugar's and, you know, everybody can't listen to this podcast. I wish they could but and I know what happens when people listen to their, to their variability in their agency and their overall health, like having good information and good tools is the answer. But, but doctors, they take their marching orders from somewhere else, like largely, and so that's a hard thing to explain in a soundbite. And I think maybe you suffer from that sometimes to trying to say like look, you know, if this many people times this many people, what do you think? 1000 more people, you have no idea how helpful that information would be to help everybody. But now we said it. So now they just have to believe it.
Dr. Carla Greenbaum 35:09
Well, you'll just have to say it three or four more times, because that's exactly the point. I mean, it's, we need people to help us help them. That's really what we need. And, you know, our job is to do the best studies we possibly can. And to do the best we can to support people who are volunteering, you know, for participation. But we need people to participate. That's for sure. Carla,
Scott Benner 35:33
aren't you just gonna take my blood and make a race of lizard people and invade?
Dr. Carla Greenbaum 35:41
Listen, I think there is among the various, the tremendous tragedy that COVID has brought to the world. You know, there have been quite a few silver linings. And I think one is a little bit more insight into science, and what science can help and offer people, you know, was much more in the so called public square than I think it's been in the past. And I hope people see that the number we actually were involved in running one of the we were a site for the Pfizer vaccine trial this past year. We had more people wanting to volunteer for that than anything we've ever done. And I, you know, reflected on that. Why is it? It's because people saw it as an emergency. It's imminent, and people saw it as a public good. They saw how terrible things were and felt that they could contribute to making it better. Yeah. So maybe what we haven't explained clearly enough to people is that contributing is how it's going to make it better. And diabetes.
Scott Benner 36:39
Yeah, it doesn't take that much effort. I mean, honestly, I had to go into an office to do it that day, and it wasn't that big of a deal. And now you're saying I just went to your site. So I go to trial, net.org. And then I want
Dr. Carla Greenbaum 36:52
to participate. Now,
Scott Benner 36:54
I see that. And then oh, it's easy. I hit click Sign up. And there's it says you can get an at home test kit, visit a quest diagnostics, or labcorp. Make and that's it. Okay, so this seems pretty simple. And you put pictures of cute children on there, which is always a smile for a website?
Dr. Carla Greenbaum 37:15
Well, you know, we do have an awful lot of people have participated over the years that are really passionate and eager to tell their story. So we'd like to do that. And we anticipate doing that quite a bit more coming in the next quarter. Yeah, we'll have a whole new campaign where we're telling people's stories and why they participate and what their experience has been in trauma.
Scott Benner 37:35
That's excellent. It really is. I don't know. I don't know how to get through to everybody. Like, you know, I there's times I just think, like, just Just do it. Let's go do it. Like even, like, quick, let me ask you a question. If I wanted to help the, this is gonna sound crazy, because you probably isn't gonna work out the way I'm thinking of, but if I want to help the overall cause, but I don't want my results. Can I do that? No, because it would be medically unethical for you to know something about me and not help me.
Dr. Carla Greenbaum 38:07
Well, it just doesn't help me as much, right? Because we already know, if we got your blood sample, and you had antibodies, we already know what that means. We're not gonna learn anything from that gotcha. What we need is for people to be ready to be in studies to see if we can slow or delay the disease. So I appreciate the sentiment. And I should say, if you lived in Seattle, we would love to have your blood because we do an awful lot of work here, just a better ROI Institute to use blood samples from people living with diabetes, to understand the disease. So we're not running a clinical trial like trial meadows.
Scott Benner 38:43
But if I wanted to just drop off some blood at the institution, that separative trial that I had type one diabetes, I could do that.
Dr. Carla Greenbaum 38:50
Yeah, we have. Well, you don't just drop it off. But yeah.
Scott Benner 38:55
No, Carla, in my mind, I roll up to the curb, and I just toss it out the window. And
Unknown Speaker 38:58
yeah.
Dr. Carla Greenbaum 39:02
It's a little more than that. But yes, we, the reason why we some of the trials that we conduct, we have decided to do because of what we learned from studying blood samples and people living with diabetes. I gotcha. So, you know, all these different ways that people who have diabetes can contribute again, it's not really what trialnet does, in terms of people living with diabetes. But we do learn from samples all the time. Well,
Scott Benner 39:32
it's an amazing thing, like the work you're doing is it's astonishing. And I do think I do think it'll come to to some or a lot of good one day. I am you know, I have to say that for me being the parent of a child with type one I live, like diabetes won't be cured in my lifetime. I hope it will be like I always have the hope, but I prepare like it won't be because I get super afraid for People who have that feeling like, Oh, don't worry, they're gonna fix it soon. I don't have to take care of myself right as well. I'm always worried about that balance a little bit. But yeah, but that's what kind of struck here. Like, I wouldn't be surprised if I turn the news on one day. And some guys like, yeah, I used that CRISPR. Turns out, you just do this and this and,
Unknown Speaker 40:17
you know.
Scott Benner 40:19
And at the same time, if Yeah, I know, I'll never know. But I tell you right now, if I send somebody to try and get through this podcast 100 years from now, kids don't have Type One Diabetes anymore. I hope I can feel that wherever I am. Because Yeah,
Unknown Speaker 40:32
oh, I love it.
Dr. Carla Greenbaum 40:34
I love it. I love that sentiment. And I, you know, I would say that we do rely on people like yourself who are passionate, not only about helping people with type one diabetes, but sharing information. I think that's, that's really why the type one community is so amazing. do appreciate that kind of work.
Unknown Speaker 40:53
You have to scale it.
Dr. Carla Greenbaum 40:54
Before we leave. I should tell you about our new study, though. Is that okay? Do we have a minute?
Scott Benner 40:58
What are you kidding me? Yeah, I'm busy or something? It's, it's COVID. I'm just gonna stay?
Dr. Carla Greenbaum 41:05
Well, I've got backup calls. But we're okay for a little bit here. Listen, as I spent this whole time, right, we're all about doing prevention, right. But one of the other pieces that Tron that is now doing is looking out at different types of therapies that different companies are starting to think about developing. And we're going to those companies, and we're saying, Look, trialnet can do these studies for you, we can help move it along, we can bring it from the early steps to the next steps to the next steps. And so I'm really excited about this new study. So it's a phase one study. Phase one means first time the drugs ever been to get given to people. And it's just there for testing to make sure it's safe and helps us select what are the kinds of doses we want to use, right for the bigger trial. But this phase one study, if the results are good, is what's going to lead in the future the next step to prevention. So for this study, this is looking just for adults, because phase one means again, only first time and people so we don't give these therapies to children. And we're looking for adults who were within four years of diagnosis. And we're going to be giving them a therapy that I kind of call a designer drug. So it's a designer drug for diabetes that we're testing in this group of adults. So if people particularly people who live near a town, that center, that would be really great. And again, you should be able to read about that on our website as well. New onset studies under new onset studies. Top Bolus this study, spell it to ppl II. Okay.
Scott Benner 42:49
Well, I will make sure I'll put links to everything in here for that. Okay. That's excellent. I'm glad you told me about that. Yeah, I mean, just makes sense. Right? You're doing the work already. And yeah. And they're looking at the same things. You might just Well, I have to say that I had a gentleman on Dr. Millman. Yeah, you don't you know, Jeffrey,
Dr. Carla Greenbaum 43:09
I know of him.
Scott Benner 43:10
Okay, I had him on a couple months ago. And one of the things that it came away from that, that I came away going, Wow, that's crazy. Is it how much more science scientific minded people are now sharing what they learn. And it's, it's become less about, like, we'll just, you know, we'll, if we get it, it's ours. And it's more about, you know, about people being able to dig into other people's research into the labs, helping labs and everything. And I, you know, I really do forget the, the actual, like specifics of what he said, but he left me with a good feeling. You know, if somebody is having a good idea over there, and someone's having a good idea over there, and they're not talking, it seems like a like a waste of time. You know, so
Dr. Carla Greenbaum 43:53
well, you know, there is this, you know, old image of a scientist, you know, locked in their dark laboratory and, you know, never talking to everybody, but certainly clinical research is 100% us network, right, a collaboration I mean, trauma that has hundreds of sites, 1000s of people that are involved in making this work, so it's really all about communicating with others and, and building bridges. So sure, well, isn't Millman isn't no minute wash you He is to get you Yeah,
Scott Benner 44:21
yeah. I I forget why I ended up having him on but something he said something he said on Twitter or somewhere I forget where I saw it. I was like, I'm gonna come on the podcast. And he was just delightful. And, and what he talks about was just very aspirational.
Unknown Speaker 44:36
Yeah, I think that
Scott Benner 44:37
one of the things he said was like, is like the thing we're doing right now was just was just unheard of a short time ago like this just this is something that nobody could have even imagined. And, And that, to me is exciting. The idea that things are exponentially growing and scaling and
Dr. Carla Greenbaum 44:52
right and the cool thing is that a scientist like himself, who's developing new therapies will be able to something like That takes those and Testament people. That's why I'm saying it's, it's like, you know, it's a village, right? It's a whole community of different people using their skills and interests, who then pass that idea along for the next day. That's what it's all about.
Scott Benner 45:17
Hey, huge thanks to Omni pod and Dexcom for sponsoring this episode of the Juicebox Podcast. Find out more about that on the pod tubeless insulin pump at my Omni pod comm forward slash juice box and of course, the Dexcom g six continuous glucose monitor, you can learn about that@dexcom.com Ford slash juicebox. You can get your free T one D Risk Screening from trial net at trial net.org. And you can also find out about those other studies. Just the way Carla told you about. Why don't you check it out at trial net.org. That was pretty good. Right, Don? I did everything I need to do here.
Let me take a minute to thank everybody again for the great ratings and reviews even leaving on Apple podcasts. And wherever you listen to the podcast at thanks so much for sharing the podcast with other people for joining the private Facebook group, which of course is always free. Everything about the podcast is always free to you checking us out on Instagram, or wherever else you follow along. Let me just put this feeler out. If you're an endocrinologist who recommends the show to people, I would love you to come on and talk about that. You could be completely anonymous if you wanted to. I can't offer a voice changer. Although I don't know that I can't figure out how to do that. But you could be anonymous, I would love to hear from an endocrinologist that suggests this podcast to patients. So if you're that person, reach out, find me. I'd like to know more. There's going to be one more episode this week. And then next week, there's going to be an after dark. And what else I have a lot of really cool episodes edited. Which 1am I going to give you next week? So I think this weekend maybe Sarah
Unknown Speaker 47:21
maybe
Scott Benner 47:23
mirdif maybe gallon, maybe gallon this weekend. Next week. And after dark with Josh and Sarah later in the week. I think that's what I'm going to do then there's a how we eat coming up next the two weeks from now. And another after dark coming in the month later. That's what I'm gonna do. Yes, I've just talked myself into it. Now let's see if I can remember what I said the next time I go to put up an episode. Anyway, thanks so much for listening guys. I love making the podcast for you. Thank you for listening means the world to me. I'll talk to you soon.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#432 Bolusing Brothers
Tula and Beans
Katie is the mother of two boys who have type 1 diabetes.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends. Welcome to Episode 432 of the Juicebox Podcast.
Today's show is with Katie and Katie has two sons who have type one diabetes, and they were diagnosed pretty far apart. So she has an interesting perspective about being a young mother with a type one and a more seasoned mom with a type one. I think you're gonna really love this episode, Katie's excellent. And I really enjoyed having her on the show.
Please remember while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan for becoming bold with insulin.
If at some point after this you'd like to find Katie and her boys on Instagram you can their bolusing underscore brothers.
This show is sponsored today by the glucagon that my daughter carries g vo hypo Penn. Find out more at G Vogue glucagon.com forward slash juice box. The juice box podcast is also sponsored by the Contour Next One blood glucose meter. You can find out more at Contour Next one.com forward slash juicebox easily the most accurate and simple to use blood glucose meter that my daughter has ever had.
Katie 2:00
Hi, I'm Katie. I live in Bloomington, Minnesota. I live here with my husband. We have been married for almost 10 years going next month I married my high school sweetheart. We have two kids. Caleb who is 12. He was diagnosed with Type One Diabetes when he was four. And Micah who is three who was diagnosed about two weeks before he turned it.
Scott Benner 2:22
Okay, I'm gonna write this down because there's two things happening and then I'm gonna get messed up. So Caleb and Caleb right.
Katie 2:30
Yep. Caleb.
Scott Benner 2:31
Is 12 diagnosed at four. Yep. And give me the second one again.
Unknown Speaker 2:36
Micah Micah,
Scott Benner 2:38
who was recently diagnosed right?
Katie 2:40
recently. Yep. So it was like his one year anniversary and January.
Scott Benner 2:45
Oh, wow. And how old is he now?
Unknown Speaker 2:47
He is three,
Scott Benner 2:48
three. He's cute, too. Just assuming you know already. But he's adorable. So I know you through Instagram. Is that right?
Unknown Speaker 2:58
Yes. Yep.
Scott Benner 2:59
What's your handle on Instagram?
Katie 3:01
It is bolusing brothers. So b o l u s i n g underscore brothers.
Scott Benner 3:07
What made you start the account.
Katie 3:09
Um, I started that account after Michael was diagnosed. And I was looking to be more connected with the community that I use community, I had my own, I still had my own personal one. But that I would post things there. And a lot of my friends and people just didn't know what I was talking about. So I figured, why not branch off and try to find a community of people who can relate to what I can do.
Scott Benner 3:31
What I know about you initially had an account, and it was it was about you and your family. And all of a sudden you start talking about bolusing and things and they were like, I don't know.
Katie 3:40
I think there was a time where I posted something and I was like at the end of his appointment. I was like no appointment times two. And they're like, what endometriosis? I was like, No.
Scott Benner 3:50
Is that what the jumpsuit? Do you have endometriosis? No.
Unknown Speaker 3:53
That's not what I meant. But okay.
Scott Benner 3:56
So then the other account makes sense. Yeah. What? So you're, you were initially looking for contact with people? Did you find it?
Katie 4:03
I did. I think after starting that, I just put like a post of my family. I was like, This Is Us. And I'm just looking forward to meet people. And everybody was just really welcoming. It's just kind of grown from there. But I've met so many different people from all over the place when it's like I need help. Or if I just need to vent. It's just so much support that I just love. That's cool.
Scott Benner 4:25
That's great. So you got what you wanted out of it. And and you're giving something back probably whether you realize it or not just kind of sharing how things are going. I want to know. I guess you're you're interesting because you have two kids and one's been diagnosed for so long. That the technology that he started with, right that Caleb started with, it's got to be different than what Miko started with.
Katie 4:49
Yes, so it's kind of up Sorry,
Scott Benner 4:51
no, no, I was just gonna say tell me first about how it started with Caleb.
Katie 4:54
So Caleb, Caleb was diagnosed as four so just like preschool. So at that point He was just like really, really sick for a long time where it kept going. I was like undiagnosed, like, every time you want to say was, he's got the flu. He's got this. He's got everything besides diabetes. So he got to the point where that started in, like November. And then by December, he was really sick, to where he was lost all the weight was really skinny. He couldn't see straight, he was like always falling over.
Scott Benner 5:27
So he was in DK,
Katie 5:28
he was in full DK.
Scott Benner 5:30
And it took about a month or five or six weeks to figure that out and coach him. So you kept going back to your general practitioner, and they kept saying it's this it's this and trying different things. And it was the prescription always wait allowed to get better?
Katie 5:43
Yes, yeah. Yep. Oh, and it was kind of like a crazy time because my husband was working three jobs at this point. And I was working too. So there's a lot with my mom, okay. And my mom was like, I'm taking him in. I think he has diabetes. And I was like, I kind of slacked it off that she was just like, crazy. Like, I didn't know anything about type one. So I'm like, diabetes, are you sure. And crazy enough, I got a phone call while I was at work from the doctor sitting with my mom. And she's like, you need to leave right now. Your son's being taken to the hospital, and you need to go right now. Wow.
Scott Benner 6:15
And did she say for? Like,
Katie 6:17
your diabetes? Yes.
Scott Benner 6:18
So I was gonna say were you first more shocked that your kid had to go to the hospital that your mom was right about a little bit? I would love to be in that moment. And in your head, just to hear the like, dammit, she was right. She was right. Was that now Why does my kid Why does my four year old have diabetes? Like what is that? What was your understanding of diabetes at that point?
Katie 6:38
Honestly, I didn't have much of a nice thing besides like, type two, so are just like things associated with like diet and weight. And I'm like, okay, it's fine. It's healthy. What do you mean, he has diabetes? I didn't have any concept of like the pancreas and everything that goes into type one. I didn't know.
Scott Benner 6:54
I don't know. I wouldn't blame you. Any. Now in hindsight, any people in your family with other endocrine issues?
Katie 7:02
Not that we know of my husband doesn't have any. And I only have a relationship on my mom's side. So if there's anything going on my father side would not
Scott Benner 7:09
you wouldn't know, man. Yeah, I'm adopted. So very frequently, when people ask questions like that, I'm like I have, I have no idea. To tell you, I'm as far as I knew, the first person in my family. starts here. So and it hasn't been it's not good roots to the tree so far. years from now, my children's children are gonna look back and go, what was wrong with him? Exactly. All kinds of things. Well, okay, so there's nobody to really lean on. So you're starting fresh. And you and your husband have like you said, you work a lot. So what happens then to Caleb's care? Does it go to your mom, mostly does it fall to you? How do you handle that?
Katie 7:50
Well, when he first started out in this journey, it was my mom. So I took time off. And I stayed with him like he was at a hospital for a week. So I stayed there the entire time. My husband was in and out. But when it was time to go back, he would go and bi moms. Okay,
Scott Benner 8:08
so she had him during the day, where I guess if you're working that many jobs, it's not just nine to five, right? You're,
Katie 8:15
for me, it was a nine like a nine to five, but my husband, it would be a 16 hour days off pretty long. Gotcha.
Scott Benner 8:22
Okay, so he's okay. So even when it wasn't your mom, then it was mostly you?
Unknown Speaker 8:27
Yeah. And
Scott Benner 8:28
did it? Did it eventually grow? Or has your husband sort of stayed? Like, did you guys like, Go look, you go make money? I'll take care of the diabetes are how have you? broken? Yes.
Katie 8:38
Yep. So as time went on, he still kind of works a lot. He slowed down, but I only work one. So I go. Right now I currently work in the same school club goes to so we go to school together, we leave school together or home. That's nice. I
Unknown Speaker 8:51
just nice.
Scott Benner 8:51
I have to tell you, if I could trade 16 hours worth of work every day to not think about diabetes, it might feel like a fair trade to me. Is that all I have to do to get out of this?
Unknown Speaker 9:03
A little up?
Scott Benner 9:05
Probably doesn't think so. But I put it does. You know, that's, it's really interesting. But I listen, I think it's reasonable. For care to be in one person's hands more than the other because of the nature of it. Just it's difficult to pass it back and forth, and back and forth. And we still lose track. Just the other day, I went to the store to go grocery shopping, and I came back and I just walked in the house. I was like, does anybody see origins blood sugar, but me? Am I the only one that sees it? Am I the only one that cares? I'm like, flipping out. Like everyone obviously cares, right? And I hear like, I didn't hear beeping. I didn't hear beeping. I'm like, it's beeping. And you know, and her blood sugar gets to like 180 it's not the worst thing in the world. We get it back down. But my wife goes, Well, you didn't tell me you weren't gonna pay attention to it when you left. And I thought, well, that's reasonable. You know, so she's got this idea in her head. She's working. And she's thinking he's got it. And then all of a sudden I leave and just comment, it felt like comments. Like, I'm not in the house anymore, you know, Could someone else do it, but because of the share, it's not like I'm really disconnected from it. So I was like, Alright, you know, I didn't say anything. You're right. And, uh, so the next time I left, I was like, I'm leaving now. Could anyone pay attention to this besides me, please? And, you know, everybody looked at me really, like kind of snotty sounds like, Alright, I understand what's going on. But no, I think it's a good idea. And that's mainly, so tell me about Caleb's. Like outcomes in those first, you know, I guess, 567 years in there, where they where you wanted them to be, where were the struggles that and wherever the, you know, wherever the, the good parts?
Katie 10:40
Well, when we first started out, we were doing okay, I wouldn't say we were doing great. It was I was a lot of overwhelmed with like, all the information and everything. And I didn't really seem to, like figure out everything that worked. But he, we went about like six months before he got on Omnipod. Which was nice, because he really hated the injections. That was really hard. But we went through this like spiral of just like burnout, burnout for years, it was very unhealthy, very stressful for him. And for me, here's a one See, I believe, when he started out was higher, and we were able to get down to like an eight. But for at least like a good three to four years. I couldn't break anything underneath a ton.
Scott Benner 11:26
Okay. So for the first three or four years, you couldn't get under a tent and you were working like you're not. You weren't just like this will be fine and not attention to it. Right. Right. Right. So describe that a little bit like what what did those days look like when, when that was going on? You wake up in the morning, did you test right away like habits like seriously, like start to finish? How did the day go?
Katie 11:48
So when it would be like a weekend or a day he was with me? It would be wake up test for breakfast test before meal. So the directions are doctor's test before meals, or if he's not feeling well. And that's pretty much what I would did. So it'd be before breakfast before lunch before dinner before bed. And then in between if he didn't feel well.
Scott Benner 12:07
Did you have a feeling that this wasn't the right thing to do while it was happening? Or were you just thinking you were bad at it? Like, you know what I mean? Like, what's the feedback that what's the feedback feel like when it doesn't work?
Katie 12:17
I felt like I was bad at it. Like I have the directions from the handle. And I'm doing what they're telling me to do. I'm testing I'm correcting and bolusing when he's getting in, or when he's eating something. But the outcome is always he's not feeling well, and he's high in the ANC is always high.
Scott Benner 12:35
So from your perspective, the only thing you can figure that's wrong is you because you're doing all the things you've been told to do. That's terrible. And I and it does weigh on you right. Like, people call it burnout. But it's the overwhelming feeling, especially as a parent, and you know, maybe I'm taking that back, whether you're an adult with type one or a parent of someone with type one. It's this feeling like you're just a failure, just constantly failing and failing and failing. And and it's got to be you because some guy in a white coat, right? Like who went to school longer than you did. And people call him sir and doctor and stuff like that. He told you what to do, or she I feel badly for you. And I felt the exact same way. I just thought this is me. I'm doing this wrong. You know? It turns out you're not though. So what was the first like light bulb moment for you that led you away from that?
Katie 13:24
It wasn't until his brother was diagnosed. It came to a point like building up so when his brother was diagnosed that last like year was really tough. I had the newborn wasn't a newborn, but I had a new baby him and it came to a point where we weren't on a Dexcom at this point quite yet. We tried like an earlier version of the Dexcom. And he hated it. So getting him on that wasn't gonna work. He wasn't convinced he didn't want to go on whenever again. And then he would eat and not Bolus he would hide it. He was sneaking food, he wouldn't test his fingers. He wouldn't do any of those things. Yeah. And so it was kind of like me trying to control diabetes in the dark. What do
Scott Benner 14:09
you think leads to the sneaking Do you ever does hindsight ever tell you did you see something happening? Or do you think it was just the the unrelenting You know, this isn't working because I don't know about you, but I have a hard time. Back in the day. I had a hard time pretending everything was okay when it obviously wasn't and everybody knew it wasn't you know what I mean? Right? Right. Which which did you go for? Do you go for it's all fine. Don't worry about it or were you more honest.
Katie 14:34
I was more honest. Like it really did frustrate me and I would just tell them I mean if you want eat the snack, eat the snack but we have to do something about it. I don't know if he kind of felt like he didn't want to be bothered with it. Like this is what we're going to be doing every day. We'd go to the end oh you know with that agency and it was always bad news all the time. So you're always getting like beat up I think both of us between all of that just kind of gave up. Did you
Scott Benner 14:58
did you feel like he Where did you begin? Give him any perspective for what it really meant. It's so hard at that age, like you're thinking four to nine, basically, we're talking about in that range, right? Like, how does he like, how do you tell him like, this is really bad for your health? Like, how do kids quantify that? You know what I mean?
Katie 15:13
Free and I don't know, if he fully did. I mean, we would talk about different people are different, like outcomes that could happen or just even comparing it to how he felt. Because they mean days where he'd wake up feeling like crap and would throw up and all that's just related to his blood sugar. So it wasn't because he was sick. And I'm like, if you don't want to feel this way, we have to get on top of it. Wow.
Scott Benner 15:33
It's interesting. Interesting, it's the wrong word. It's overwhelming for me to hear that. Because, you know, I think of you now, like, I don't know, you know, you, but I'm aware of your face. And I know what your children look like, you know what I mean? And, and we, we talk back and forth sometimes and and to feel like your son was so high that he was vomiting is like, his feels crushing to me a little bit that like that happened to you? You know? Yeah. And, and I can't imagine being in the moment, because you're standing there going, this is not okay. And yet, we don't have any real answers. Now. Do you not have answers? Because I don't know what I want to know. Like, when you go back to a doctor and tell them that, how do they respond to you,
Katie 16:19
we would go through is like kind of like re education, but it's like the same pieces of information. But one of his, his nurses, she has her son is like a year older than Caleb and her son is a type one. And she's like, you really have to get this Dexcom. So it was like the newest version. And she kind of just talked him into it. And this was like leading up because at this point, this was what maybe she'll lie. Right before so July 2019. Okay, we were preparing for Caleb to go he was going to go to Kenya for an entire month with my husband and family. So I'm saying here diabetes lady who manages everything is staying in the States. And they're going so his, the nurse was just like, you should really sign up for this. And that was like the stepping point right there was getting that prescription for that.
Scott Benner 17:10
Were you out of your mind that he was going away for a month without you?
Unknown Speaker 17:13
Oh, my gosh, well, yeah, a little bit, I think
Scott Benner 17:17
I would have been like, but he doesn't. He's been working. He didn't know anything about this and not for nothing. I don't appear to know anything about it either.
Katie 17:25
Going away. And it was crazy. Cuz he was my husband and my sister in law both came to like appointments building up to that to get all their questions answered. And everything, tried to be squared away the best as possible for sending him?
Scott Benner 17:37
Yeah. Let me ask you a question that might be a little more unpleasant. And don't answer it if you don't feel like you want to. But have you ever cognitively thought that you're treated differently? For having brown skin in a doctor's office? Do you think there's the the Hey, they those people, quote unquote, don't care as much about their health as other people because I've heard a lot about that lately, that there's there's actually data that says that doctors might subconsciously believe that brown people don't care about their health as much. I don't know where that would come from. But have you ever seen that?
Katie 18:10
I have, not necessarily in Caleb's diabetes experience, or even my cuz i arendal is actually Middle Eastern. And she's a very sweet lady, and she gets us in our stands us. But thinking back to like experiences I've had personally, I have definitely seen that. For example, when I had Caleb, I was 20 1920. And my husband and we're not married yet. And when I went into labor, I feel like we're treated differently in the hospital. Caleb was born with an issue that I can't even name to this point where he has spent a week in the nick you. They kind of were like we were brushed off and people weren't giving us information. I feel like it was treated based on the fact that the way we looked the fact that we were young, unmarried couple and the type of insurance we had, yeah, and I remember like my sister in law was a few years older than us like going in and like yelling at these nurses and yelling at the doctors like about this issue and how they're adjusting and treating us.
Scott Benner 19:07
That's a tough I mean, that is you were like 20 years old. That's it? Yeah. I don't know how to stand up for yourself when you're 20. In that scenario, you don't mean like you need kind people to say, it gets so simple, isn't it right to look and say there's some unmarried young people here having a baby who's come out, and it's having an issue? we could we could lift them up here. You don't I mean, like we could, like common sense voices for them. We could point them in the right direction. But it how much of that feeling of over being treated differently? I wonder is you really being treated differently? And how much of it is you feeling like that imposter syndrome, like you don't feel like you belong there because I've had that feeling in my life to do you know what I mean? Like, my wife and I got married pretty young. And I remember being in a furniture store. And we had an apartment and we wanted a sofa and we had money. For a sofa, and we stood and stood, and salespeople just walked past us and walked past us. And no lie. I've never told this anywhere before. I took out my credit card and held it up over my head and said, I have money and I'd like to buy a sofa. Can someone help me? That's literally how I got somebody to help me buy a sofa. And I don't have any issue with my color that, you know, in that way. And it was really, it was crazy. I was like, Oh, my God, they don't assume I'm serious. Didn't mean like that, or that. I don't know what they didn't think. But they just avoided us. like the plague it was, you know, not the same thing. But I remember feeling then moving forward, that we weren't serious players in like an adult life, if that makes sense. Yeah, and it takes a while to get past that, then, especially if people are gonna keep treating you that way. I just I was really was really interested. And I'm glad to hear it. It doesn't exist with your endo. But your endo also has a different perspective, I guess. Yes. That's that's really something. I wonder if it happens, despite the color of the doctor. Like, I wonder if it is a systemic issue. Do you know what I mean? Like that? That's the feeling. I don't know. That's very strange. That did you ever feel like you weren't interested in your own health?
Katie 21:19
No. Like, if I'm there, and I'm paying business, like No, that's not it.
Scott Benner 21:25
Right? Right. You're not disinterested? Right? So. So the key here, it seems to me is that somebody on the other end, no matter what the scenario is, has to have the compassion to walk you through something no matter who you are on the other side of it. You know, I mean, your interest level like that, because there are people who are just overwhelmed and decide to write off their health because they don't feel like they can do it. But you could reach those people if you worked at it and tried, I think, yes. And so what was it was it seeing the Dexcom is that what brought things into focus for you see and data. g Volk hypo pan has no visible needle, and it's the first premixed auto injector of glucagon for very low blood sugar and adults and kids with diabetes ages two and above. Not only is chivo hypo pen simple to administer, but it's simple to learn more about, all you have to do is go to G Vogue glucagon.com forward slash juicebox Jeeva shouldn't be used in patients with insulinoma or pheochromocytoma. Visit g Vogue glucagon.com slash risk. When you're using a blood glucose meter, you want it to be accurate, you want it to be easy to use, easy to read, and easy to see in the dark. And if you had a Contour Next One blood glucose meter, you would have all of those things. Arden has never used a meter that is so accurate, or so simple to carry with you. It's tiny, but not so small that you can't hold it. It's simple, but yet does everything you needed to do. And if you want it can connect to your phone by Bluetooth. And you can use the contour app to do even more. But you can find out about that at Contour Next one.com forward slash juicebox. While you're there, you'll also be able to find out about their other products, their test trip savings program, and you may even be eligible for a free Contour Next One meter, you'll find out when you get there at Contour Next one.com forward slash juicebox. YouTube can simply and affordably use the best meter that Arden has ever had. And last but not least, to support type one diabetes research and studies that are helpful to people living with type one including you. All you have to do is be a US citizen and have type one or a US citizen who is the caregiver of a person with type one. And in just a few minutes. You can add incredibly important answers to simple and easy questions right there from your sofa right on your phone or your tablet and help Type One Diabetes Research to move forward T one D exchange forward slash juicebox. Alright, let's get back to Katie.
Katie 24:23
Seeing the data for Caleb started putting a focus seeing that what's going on in between those checks are even when he wasn't checking, but it was still problem. Still problem. We had a problem. But it was like a problem from the time where he was at my house the time he left. So problem at home problem my grandma's problem at school school is a big issue. The nurse throughout elementary that was an awful, awful experience. So just like seeing all of that building up. We're already like in a tense mess when his younger brother was diagnosed Wow. So
Scott Benner 24:58
you slap the seat GM on him to go on the trip. I do think I want to find out how the trip went. But but but now you see everything that's happening now it's not just this random mess. It's an actual mess you can look at right? Yes. Yeah. And then your other kid gets diagnosed?
Unknown Speaker 25:14
Yes.
Scott Benner 25:14
Oh my goodness. Did they make it to Kenya?
Katie 25:18
They did. But Kim was not on the Dexcom yet. Okay, you didn't actually get on like a proof to everything and tell. So we started that process in July, I think July and he didn't get that Dexcom till December.
Scott Benner 25:31
Okay, so the trip had happened in between them. So it was really just business as usual while he was born. Wow. Pumping or injections,
Katie 25:40
pumping stuff. So we've been on the Omnipod consistently since six months into his thing, right? And, and,
Scott Benner 25:46
and so and I don't mean this as a judgement, I really am asking, at any point, did it feel to you prior to Dexcom his blood sugar's high, insulin makes you lower. He should have more insulin did that ever? Like
Katie 26:02
it did it did but I had this constant fear of insulin, like I was drilled in my head that if I give him too much, my kid's gonna die. Or he's gonna have a seizure. I'm have to dig out the glucagon and give him a shot. I was really afraid to give him too much. Or even change the settings in that talk.
Scott Benner 26:20
So the fear Got you. That's reasonable happens to a lot of people. And so were you trading so you weren't unaware of what high one season? High blood sugars we're gonna do to him long term? You were aware of that as well?
Unknown Speaker 26:33
Yes. Okay. Yeah. So
Scott Benner 26:34
you were just sort of trading? One for the one for the other. Yeah. Like, I always think of it. I know, this is like more of it. But I always think of people who jump out of windows to avoid fires. Right? You know, like, just just sort of like, well, this is gonna kill me now. And this is gonna kill me later. I'm gonna go with later. And you know, it's just a it's a, I bring it up, because I think that people could see it as an excuse. But it's a coping mechanism, and a survival instinct. Right? You know, it really is. And so fears is good enough reason is any so Okay, so how did the data stop you from being afraid?
Unknown Speaker 27:11
It did it.
Katie 27:14
I would call it out. And I was constantly emailing his team. And it was always correct. Two hours, correct. Two hours. So I'm doing that thinking that I'm making a difference, right,
Unknown Speaker 27:24
but I'm not.
Katie 27:27
But it was just kind of like a whole bunch of series of events that led us to making the change. I think that that was that. But then, Caleb was also right around the same time where Michael was diagnosed, Caleb was scheduled to do a GI stem test, because he hadn't grown in about two years. Okay, so no, wait, no hype, just kind of plateaued at the same.
Scott Benner 27:51
Yeah. And it's funny. So they want to do it. What test then
Katie 27:54
is called a cheap gh stem test growth hormone stimulation test,
Scott Benner 27:59
I would think they would want to give him more insulin so that he could. Okay. Yeah, but I hear you. So that test happens. I'm assuming that led to what? Nothing?
Katie 28:10
legia there was nothing wrong. Yeah. Diabetes.
Scott Benner 28:14
Yeah. What I mean, it's like, I don't know if people don't understand this or not. But, you know, you need that insulin, that's important. And it slows down other functions of your body. And if you look back, I don't know any of the details on this. Somebody not use any of the words, but a long time ago, people who had diabetes would not they would call it not thrive, right. Like they wouldn't grow or gain weight or anything like that. But it really just was they didn't have enough insulin, you know? Wow, that, so how big was he then when you got that test? You remember? Um,
Katie 28:49
I don't it's kind of black. But he's, he was about he's shorter than he is. Now. Let's say that he's, he's put on a good like six pounds since then, since we've kind of made a turn around and he's definitely put on height.
Scott Benner 29:02
Okay. And in how much time?
Katie 29:06
So if we go back to when we actually started, like making big changes, it's about a year.
Scott Benner 29:13
Okay. Let me share this with you. It's gonna come up in an episode eventually, but I don't think I've ever said it anywhere. When we found out Arden had hypothyroidism, so she wasn't getting enough, you know, of the hormone that she needed from her thyroid. Arden was five feet. Was she five, one or two, and weighed 75 or 80 pounds. And now I think we're three years later. Arden is 571 30.
Unknown Speaker 29:47
Wow.
Scott Benner 29:48
And I think if we don't figure out that she has hypothyroidism, she doesn't get a chance to grow. Right and I just I listened. I'm obviously not a doctor, but it seems to me that when your body is struggling like that, Other systems close down? Yeah. And and that's it, but I can't even tell you. She's one of the tallest girls in her school. Wow. You know, and she was one of the smallest people you'd ever met in your life like, no lie. She was out recently, well, before all this, she was out with my wife in a store that my wife said she bumped into somebody who used to coach Arden and softball, and they're chatting. And while they're talking, Arden realizes what's happening and walks up behind my wife sort of stands over her shoulder, but doesn't interject. She just stands behind her. And Kelly said that the conversation went on for minutes after that, until the guy went, Oh, my God, is that Arden. And she was taller than the guy. And like this grown man, and he had, he's like, I had no, he said, I just kept thinking, I wonder why this person is standing behind her while we're talking. didn't even ask her. So I'm excited to see you know, where your son gets to? It's Yeah, it's exciting. Are you bigger people? Like, are you tall? or,
Katie 30:59
um, I'm about five, four. And I think my husband's like five, eight, so we're not the tallest. But right, it'd be nice to see if he gets somewhere closer, even taller.
Scott Benner 31:08
I think the goal actually at that range, like the goal ends up being right like 5758. And then if they're going to be tall for your family to get to 510, something like that. That would be nice. I know, my son's pissed that he's not taller and blames me. I know, he's, I know, he looks at me, he thinks it's his fault. Yes, my wife is tall and all the men in her side of the family are very tall. So he's probably right. But again, I'm adopted. So I can just say it's not me. It's somebody else that we don't know. Okay, so I want to try to get the idea straight here a little bit. Okay. As you're trying to figure out Dexcom and you're starting to get the information back with Caleb. Yeah, mica comes online as a type one as well.
Unknown Speaker 31:53
Yes.
Scott Benner 31:54
Is it the I can't do this, the two of them feeling like what really, like, propelled you forward? Do you think do you think you just took a little while to figure out the Dexcom? Is it a weird coincidence that they happen at the same time or no?
Katie 32:06
No. Well, with mica, we had him tested through trial net.
Unknown Speaker 32:10
Okay, so,
Katie 32:12
so I knew so we were playing the waiting game for almost almost a year it didn't even even reach the airplane. We were testing him on a weekly basis. So building up with all these background things with Caleb happening, we're just playing waiting with Micah. So when Micah I noticed his blood sugar took one like fasting one, it was like 200 I immediately knew something was Sun was up. So we got into Caleb's endo and he pretty much told me you know, you have a year you have about a year with the with all those antibodies you have about a year before he gets it. So the waiting game goes on that 200 they diagnosed him that day, which is really weird because we were seeing an endo that Caleb used to see when he was diagnosed the same and always seen them and seen in the hospital. Okay, and that endo was the one we were squeezed into super mica. And they ran the agency I think Mike his agency was a like a nine. So like, I didn't need the doctor to come in and tell me anything at that point. We could have went home, but
Unknown Speaker 33:19
we're good. We're good. Let's go for a little bit and then we'll get going.
Katie 33:24
Yeah, so but it was January 17. The same doctor not in the hospital but in the clinic telling me that Micah had it which is the same day and doctor that told me that Caleb had it so it's like this little devil moment
Unknown Speaker 33:39
wait the same day?
Katie 33:41
January 17. May 17 2019 versus 2013 Wow, same doctor which we don't even see on a regular basis ever
Scott Benner 33:49
anyway that's weird if I was you I would never go into hospital on that day to get
Unknown Speaker 33:53
no
Scott Benner 33:56
I got shot like I'm waiting till tomorrow nothing good is gonna happen on this date and anywhere near Oh, doctor. Oh my god. Oh, sorry. That's Well, okay. So his is a nine Caleb's is still high
Katie 34:12
kills like a weapon or even like a 12. At this point. He's going up
Scott Benner 34:15
the other way because the food around you thinks you're not even able to keep it where you were keeping it. I got it.
Katie 34:21
Okay, no. And then I remember I had to continue work that day. We were short staffed. I came home after picking up my kids new prescriptions gave him his Lantus and he's screaming and he's crying at this point, which I don't blame him. You know, it's a whole different thing. And then I turn around and go in the kitchen. And there's Caleb, eating dinner without no Bolus, no checking anything and it just sent me off. I remember looking at him, and I kind of lashed out a little bit. I just remember telling him like, this is what you're going to teach your brother. This is what we're going to do. Are we going to do this for the rest of your life for my life, For his life, this is what we're gonna do. And I remember handing mica after my husband. And I was like, I can't do this. And I went down into the bathroom, and I closed the door and I turned on the ceiling fan and I just cried, like I curled up on the bottom had like a good ugly cry. It wasn't even like a, it was like a full breakdown. I think at that point, I just snapped, like, everything I had spent. And I think that went on for like, a good 30 to 40 minutes. And then I that was just like that aha moment, like, I'm not doing this anymore. I'm not gonna start it with mica, and I'm not doing this with Caleb. Okay. And that was a moment when I wanted to take an initiative that if I wasn't going to get help through the doctor, like I was gonna go and look and find it for myself.
Scott Benner 35:41
So I'm wondering, do you think that you just reset an expectation? Like, this is what we're going to do? And I'm wondering to how much of that because if I'm not sure how well I'm doing the math here, but uh, Caleb's 12. How old are you?
Unknown Speaker 35:58
I'm 32.
Scott Benner 36:00
So you had them when you were 20? If you would agree now at 32 you were a kid when you were 20? Right? Yes. Yeah.
Katie 36:06
Only not mature quite yet there? I
Scott Benner 36:08
don't think so. Is it possible that you start being a parent, not as an adult, and then it feels more like a collaboration like you don't mean like, there's this moment when you have to, like, I use my son as an example. He's a nice kid. And he's bright, and but sometimes he's gruff, and short. And I let him do that because too, he is. But every once in a while, I'll be like, Hey, I, what are you doing right now? Like, great, talk nice. And he's not like that all the time. Do you know what I mean? Like, it's every once in a while, it ends up being honestly, if he's exhausted, or tired, or he's just played for hours, you can't walk up to him afterwards and say, Hey, how'd it go today? Because he's gonna be a girl, you know, but and most of the time, I understand that, but but every once in a while, I stopped and I go, No, no, this is not how we talk to each other. And forget me, don't talk to people this way. Like, you're gonna end up with some girl who will put up with us. And that's not going to be good for you. Because nobody should put up with us like talking, you know, speak. And, and I think there's just a moment when you, you feel you feel like your job. I felt like my job was making my kids happy when I first had them. And then as you get older, you realize your job really is to direct them and to and to do the thinking for them that they can't do. And I just wondered if you got trapped in that in the beginning, so you know,
Katie 37:28
I think so. I think cuz I mean, I wasn't just that, like Mike and Caleb have two different life's like two different parenting experiences. Yeah. And I think when Caleb was little, like, I just wanted to make him happy. And I think I didn't put my feet down as much as I should have.
Scott Benner 37:51
Well, it's a Caleb got like the Ooh, wow, you got pregnant parents? Exactly. And Micah got that, hey, this is working out. And we're gonna have another baby parents. And yeah, we're gonna stay married and make a family. Those people right. Yeah. Now, you don't see that about yourself when you're young. And you're and you're, and that's happening to you think oh, or have a family now. But really, everyone else is looking at you going? I wonder how long this will last? You know, and for most people, it doesn't last very long. And you just end up being too, you know, intelligent, reasonable people who want to make a family and keep doing it. That's really interesting. Don't have a third baby.
Unknown Speaker 38:27
Oh, no, we're done. Back
Scott Benner 38:29
kiddo. Get like back it'll get like, old tired. You just like I don't care what happens?
Unknown Speaker 38:36
yourself.
Scott Benner 38:37
Whatever. Yeah. So to you, you basically walked up to Caleb while he was eating and said we can't do this. This isn't what we're gonna show your brother. You went in and did what you did. I know. I've been on the other side of that before those three boys sat in that kitchen. They were like this. Oh, yeah.
Unknown Speaker 38:57
Yes, she
Scott Benner 38:58
seems really upset. Did you come back? More of a? I don't know. Fierce. How did you come back up the steps. I guess.
Katie 39:07
I came back. I was actually calm. And I was like, we're gonna try something new. I don't know what that is. But we're gonna do it. And I think Yeah, we'll just skip. So it's like, Okay.
Scott Benner 39:19
I don't need her getting into this and being upset and yelled at me. So I'll just do whatever she says. But isn't that interesting? Because at any point along the road, I guess you've had to live with that. At any point along the road. You could have gotten that you could have done this. Yeah. But it took this other thing to happen.
Katie 39:34
Yeah, it's kind of like, in a way I know. sounds awful. But I feel like mica things happened for a reason. And maybe it took my gut getting that diabetes to shake, shake me shake me awake to take that control.
Scott Benner 39:48
Well, I mean, at those agencies, if you want to use that analogy, his diagnosis could very well have saved Caleb's life honestly, you know, because you guys weren't, you weren't getting it, and then you got the CGM and you had that That very there's some people talking about getting a glucose monitor then being overwhelmed by the information. Is that how you felt? At first? Okay. Yeah. And that's because you didn't have any tools you didn't know what to do with the data once you had it. Right. Yeah, that's that that really is. That's still a gap. Right? Like you can't you can't just be have all this thrown at you suddenly, cuz you already struggling. Now you're struggling with numbers you don't understand. That's not good. You know? What did you already well, what did you go figure out? It's time to find out.
Katie 40:32
So at this point, what we're in January, January, I started just like looking at things. So in my head, I was like, I can control his blood sugar if I limit the carb intake. Okay, so I was starting to look up like different things about I didn't fully consider doing like, keto or super low carb. But I started challenging Caleb to have less carbs, especially during the day. So when he is not with me, let's put a cap on how much he's eating for lunch, or because my mom would pack his lunch. So I would talk to her about what what's in his lunch today? Can we keep it under 40 grams of carbs? What about breakfast? So we started there, and I started seeing a small difference, but it wasn't slight. So maybe he was hanging around 300. Now he's hanging around 250.
Scott Benner 41:11
Okay, for me, but still a move? Mo Yeah, little cause and effect, you're saying at least.
Katie 41:17
Mm hmm. And then I remember, like going on Pinterest, I think it was Pinterest, and I was looking up different recipes. And they came up with grit, like a different group. I don't quite remember which group it is. But they're very, like intense about being very low carb and finished, intense. And I was like, well, maybe I should try this. But in my head. I was like, if I push Caleb this way, this could have a negative effect. Because he's already at an edge. I don't want to take away food and things and have him have another negative relationship with the day.
Scott Benner 41:48
This was just too far. The other way. This was your eat an egg. Now don't eat anything. Have a sprig of lettuce like it was Yes. Okay.
Katie 41:56
And then when I'm so switching up these recipes, I had an ad or like a picture of someone posted of your podcast.
Scott Benner 42:03
Oh, cool. This is the part I love. These are my favorite parts of the podcast good.
Katie 42:06
Yeah, I just saw. I saved it. I saved that in a little little board thing I had for a diabetes. And I kept it moving for a couple more weeks. But I was I had idle time, which I usually didn't have much, especially while Mike goes like, smaller. And I turned it on and I had Listen, I think it was your most recent episode. At that time. I think it was Katie and the old man. Okay. And listening to this teenage girl talk about how well she was managing her diabetes. While I'm over here struggling as like a 30 year old woman. Thank you, man wait for her. But I was like a light bulb went off. Like people actually can do this. And they're living and finding their story isn't my story, right? Something's up.
Scott Benner 42:52
Yeah. How do I make this match better and make it make sense? Hey, in that episode, I was the old man, right? Yeah. I seriously couldn't remember for a second. I was like, did we do like an interview with her and a father? Is that like, I wouldn't call someone else. Oh, this must have been about me. I really, but it's interesting, that that had so much impact on you. And as you were talking about, I thought, I don't remember that. All I can tell you is that from the title. I must have listened to it and felt like an old person talking to a young person. And that's why I call it that. And but she did a remarkable job of of handling herself. Yeah. And and that made you think like how this kid can do it? Like, what am I doing? Like, I gotta be able to do this right? Don't you think she'll be thrilled to hear that when this comes out one day? Oh, look what I did. So that's very cool. And so did you delve in Then did you start listening from live? Did you go back would you do?
Katie 43:48
I started like my, that process. I was gonna start from the latest and then go backwards. But I remember I messaged you. And I was like, Hey, I just discovered your podcast and I laid out my situation a little bit and then you messaged me back which I was shocked. Because I was like, podcast, people message people back, which is
Scott Benner 44:05
a thing. Like I remember your story making me feel very sad, which is what got me back quickly. And yeah, here's the trick for people if you must know, children with big agencies, or adults that sound like they're about to, you know, close their eyes and fall off a cliff. That gets me pretty right in the heart. Just so you know. So. Okay, so, okay, but then what? And
Katie 44:26
that was me both of those things. Maybe I was like,
Unknown Speaker 44:30
a bit of a mess is what we're saying.
Katie 44:34
And then I remember You shot me a message and you said start with these episodes. So that's where I started. So what's the different pro tips ones that you had at that point? And then like the ones about like insulin and just like resetting? Mm hmm. So I started there and I started taking notes. But the one thing you had said that will just make like a bit of a difference was Pre-Bolus Singh. So as soon as I got that message, that's what we did immediately. That day was starting 20 minutes set a timer, Mike is is 10 because he Flores with turtle. But doing that. And then I just remember having a conversation with him. I was like, Hey, we have nothing to lose. This was about spring break for school at this point, I was like, give me a week. See how you feel? See if it's something we can do. And just trust me, do you trust me? And he said he did. And within that week, we had seen numbers from that 250 inch cluster that 200 to higher 100. And to him that was like a win. Yeah, right. We're making process. So he we were all in at that point. Cool.
Scott Benner 45:39
He must have felt when did he start feeling low at like, 150?
Katie 45:42
Yes. So that was the conversation. So just like, just try to tough it out. I know, it's just your body adjusting, we just have to give it time. If it gets out of control, then we'll worry about getting some carbs in there. But that's really cool. It took a while for him to get that adjustment to be able to sit at like 80 and feel okay,
Scott Benner 46:01
right? Well, I mean, there's so much to it. Like you can say the steps. I think it's why the podcast is is valuable is because it's easy to say like I'll tell you right now, like here it is. Get your basil right, then Pre-Bolus. then learn about glycemic index and glycemic. There you go, you're done. Right. And so the problem is, is that there's a lot around those three ideas. And it's not as easy as just being told you know it, it's not, hey, listen, here's the steps for getting out of this room, stand up, turn the knob pull the door towards you like it is that but you know that you can you can imagine when someone says to you. Okay, so you started Pre-Bolus. And he went from, like, into the higher hundreds. That gets you excited. And you're like, what do we do? So what was the next step, but you keep doing what
Katie 46:44
I do. So then I was listening to like the bezels. And so that was a scary moment for me, right? Because I already had a few of insulin. So I'm gonna change something and said, I've never changed anything in the pump, without the doctors. So I remember listening to that episode, I was like, You know what, I'm just gonna do it. I don't think it's gonna kill him. So I'm just gonna do it. And once I started this, like that, that basil pro tip episode made all of the difference, Miko was a little bit easier. You still had him winning. So his was a little bit easier to get down. But Caleb, I would set the basil, I'd watch it for a couple of days, study it and make changes. And within like, a month, month and a half, we would see such a big difference in like his clarity app. Yeah, I remember there was one day we had like a family get together. I think this was June. So by June where he had hit like, 98% in range. Wow.
Scott Benner 47:35
And what's your range set out again?
Katie 47:37
for him? We had it set from 70 to 140.
Scott Benner 47:41
Wow, that's really great. That's exciting. Wow, good job. Congratulations. How did Caleb feel once his blood sugar got low and stable?
Katie 47:52
He was fine. And he was so excited. Like he would be so proud that that was it. And then you would see some of the other things that came with those high blood sugar starches. So like, he used to be really aggressive or kind of short. Um, I can't say for school, because that was summertime. But as we went into the fall, like his focus, his grades, his things, everything about him change,
Scott Benner 48:15
okay? Just the end, and for the better in your mind. And
Katie 48:19
the better. Okay, the better way better. All different kids.
Scott Benner 48:22
I know that I once got this some private note from a woman. And in the course of the note, she admitted that I used to just think my daughter was a bitch. Those were her words. And, and she's like, she's not. And you know, it took me, it took me finding a podcast to figure that out. And you know, that, I always think of that, because I feel like, like, you know, just for the same for you, like you could have had a relationship with your son for his whole life, or he's not really being himself, and you feel like this is who he is, you know, and that's just not something fair on it is just every level. Wow. What did the doctor say?
Katie 49:05
So let me see. So he didn't see her. I seen her right before we had to start the journey. And then we seen her in August. So I'm off for the summer. So we work this entire summer portion, working on getting it down. And I remember we went in, and then they ran my guess first I think what Michael was like a six. So he went from like the nine to a six. Yeah. And then Caleb's came in. And I think he was what like seven? Well, it was he was down there. And then like the look, he started, he lit up instantly. When because that's the first part we started. They take the agency, then they take you off to the wait for the doctor.
Scott Benner 49:41
Right, right. Yeah, that's how are supposed to.
Katie 49:43
And so when the doctor came in, like she was smiling, and she was just like, I had to make sure that when I printed this out that I had the right last names on here, because this is not what I see. Right? Especially like I double checked a few times before I came in, to make sure that I had printed out the right All
Scott Benner 50:00
right, right. I have to tell you, um, hold on one second. My wife asked me a question. Sorry. So I get them the mica thing. She might have seen that and just been like, oh, the kids honeymooning. This isn't reasonable. But she sees Caleb's. And is he is he from an 11? To a seven or attend to us? Yeah. Wow.
Unknown Speaker 50:22
Did you
Scott Benner 50:23
get the talk? Like you're making him love a lot talk? Is that the next Oh,
Katie 50:28
she was just like, onboard. She's like, what are you doing? Tell me everything. What? What changed? Wow, what changed? Because the last time I seen you, you were struggling. We were getting ready. Like I was setting up an appointment to see like the diabetic psychologists do everything like you are in a whole different space, what's going on?
Scott Benner 50:48
There, we're gonna send them to a psychiatrist,
Katie 50:51
like our family, like the therapy for like burnout, because we were just not getting anywhere.
Unknown Speaker 50:55
Right. Wow.
Unknown Speaker 50:57
And
Scott Benner 50:58
Geez, you were close. See? It's interesting, because you were close to if you go to therapy, then not that you shouldn't have. But if you do now, that's like now you've said, this is the problem, right? Like we burn out. If we can't do this, that's a problem. This problem needs to be fixed. And you start putting effort into fixing what you think is the problem. But the problem is just a side effect of not understanding how the insulin works. Right. Oh, wow. You were close to falling off a cliff there that you might not have gotten back up from? That's really interesting. Wow, this makes me feel nice. I'm happy for you. Yeah. This is very good. Wow, how long ago was that?
Katie 51:43
So that was so that initial one that was last, I guess. But like this last we had a telehealth one. What was it in March? Okay. Caleb is at oh my gosh, 5.8. Wow. And it comes to a point now where when she comes in, for the thing, she asked me, is it okay, if you want to change this Basal rate? It's okay. Are you okay? If we change these things?
Scott Benner 52:08
Let me just ask you, your thoughts on this. A little bit has to be, I don't want to say embarrassed, right? But there's got to be a part of it. It's gotta be like, Wow.
Katie 52:19
It's funny, cuz she's just like, I wish I could just bottle up what you do and give it to my other patients. And I was like, suggest the podcast.
Scott Benner 52:27
Yeah. Tell her I can talk them up and sit in a corner? I'll tell them for sure. Yeah, seriously, I like that, that makes me feel like I would love to. I would love to be able to do that. I would love there to be a talk at a hospital. And I could just give that first hour, answer some questions and then point people towards the episodes that would support it. I don't think that everybody would get it, get it right away. But I don't think that that many people would not get something from it. You know what I mean? You're always very kind online. Like saying, like tagging me and stuff. And I really appreciate that. But it's because it gets then I get the watch. Like you just talked about. Your son had diabetes, basically for eight years. For seven of them. He's it's just a disaster. Like, it really isn't. Things are going completely wrong. You take the bull by the horns when when Mike is diagnosed, and really you change everything. Like it's easy to sit here and be like the podcast, the podcast, but you decided to do something. And then you found something. It could have been something else, like you could easily be, you know, somewhere else right now saying like, Oh, thank you. I mean, obviously, this is the best place. That's not what I'm saying. But, but as long as you find something that's, that's really wonderful. Do you I want to know how it's changed your life. Like personally,
Katie 53:53
personally, at first, I was a little stressed because I was constantly kind of obsessing over looking at everything, but now I feel like even though diabetes is such a big part of my life with two diabetics and everything that goes into it, I don't think about it as hard. Like when I see a blood sugar rising, it doesn't stress me out as much because I know I can get it back. Right? I know that even if because those days like I'm not a super ninja yet. There's days where Caleb might get to a 200 if I didn't nail something but instead of being that old person that I was where I would wait two hours, like I know I can get it back and I get it back quickly.
Scott Benner 54:31
Yeah. Arden's blood sugar goes up and down. And we deal with it the way we deal with it, you know, as best we can last night. You know, we're all just sort of feels like we're all just laying around the house at this point, you know. So, like, both of my wife and I are able to work from home which is really lucky. And, you know, artists, it's summer vacation now. So last night, I think I said around like seven o'clock, I think our washers going which is just No, I had this conversation with my son where he's like, what's the big deal? I'm like you don't understand. Like, no one wants to buy a washing machine. It's just the saddest thing to do with your money, you know. But I, I felt like I had to go out to a store to look at a couple of them. I tried to do it online as best I could. So I laughed and Kelly's like, would you grab some soup and bring soup back for everybody? And I was like, Yeah, whatever. So I brought the soup back. And Arden's blood sugar was great, like, for a long time, you know, after the meal and everything. But she started to get low later at night, like, I think 1130 she started dipping down, and we thought we stopped it. But we didn't. And so we were kind of trying to just nudge it with some carbs. But we were trying not to give her too much. And then finally, she had to have a few more. So there was a moment in their blood sugar kind of dipped down into the 60s, and we got it back up. And now I'm trying to get it back up without it getting, you know, high. And I did. And I can remember being you and thinking, Oh great. She's low. And now she's going to be high. And I'm going to be up all night. And then that all starts to like build on itself and you get upset and anxious. And then there's no way they don't feel that you know, but last night, I was just like trying, we were joking around, like you know, and and fixing your blood sugar. She asked me for a little ice cream, like little frozen ice cream cones. They're probably not really ice cream. But you know what I mean? They're, they're in the freezer. And we came I came up in the top of the roundness of the cone was offset on the cone itself. So it was way off to the side. And I handed it to her. And she said my ice cream cone appears to have Spina Bifida. And I went wide. And then we like I was like, oh, there's something up with it. Like we're like nudging the top of it back again to the center. And then she ate it and leveled out exactly where I thought, you know, her blood sugar's 103 right now 12 hours later. So it does get easier once you have enough experiences over and over again. So you really feel like you're sort of in the beginning of it, but you're doing Did you ever limit carbs? Like you're talking about a one season a fives?
Katie 57:08
Um, so no, I don't like when we did that plan. I kind of let it go. Because I felt like he was pushing back. So he gets what he wants. See? Wow,
Scott Benner 57:16
that's so cool. And he can maintain this with grandma just as easily as
Katie 57:20
Yes, because well, now at this point, like he doesn't go karma so much in Marcos. He's now in middle school. And I work at the same school. So we go and we live together. So it's a lot of text communication. And mica goes to daycare. So when well, pre COVID he went to daycare, but she'll text me and sometimes he'll kind of a little but for the most part, it's not that you were
Scott Benner 57:43
able to handle the daycare to do text with them is that I handled? Yep. So
Katie 57:47
she'll text me back and forth. her grandma does when she's got him too, because he kind of splits between a couple days a week daycare a couple days a week, grandma
Scott Benner 57:55
got it. Dexcom Dexcom is amazing. All the pods amazing. I love Arden's meter, you know I that's why they're all advertisers. But if I could take text messaging as an advertiser, I would tell you that it's an amazing diabetes tools, just being able to text with somebody and have more immediate interactions so that you can kind of stay fluid with the blood sugar while it's doing what it's doing. It's trying to be variable, and you can stay with it. I'm very happy for you. Anything that we didn't talk about that you wanted to? This was really great. You were nervous, right?
Katie 58:28
I was nervous. I it's kind of funny. I don't do well talking to adults, even though I work with middle schoolers, and they're super judgy. And I'm fine with that.
Scott Benner 58:37
Do you imagine this means that I'm not really an adult? I'm perfectly comfortable. While we're doing this, I realize what you're saying. And I hear you. I'm sort of like a child. No, seriously, did we miss anything?
Katie 58:50
I don't think so. I just want to say that, you know, if you feel like you're in that spot of burnout, just get help. I feel like I should have gotten help a long time ago before all of this. But once again, everything happens for a reason. And guess where we're at now.
Scott Benner 59:06
I have to agree with you, I guess wherever and when you're struggling. I was saying the other day to some By the way, the entire time we've been doing this. I've been looking at Katie and there's a giant trolls that are behind you. And I have not been able to not see it for like an hour. And at first I was just like, what is that? And then I started figuring out I'm like, but it looks huge.
Unknown Speaker 59:26
Is it huge?
Katie 59:27
It is huge. This is our random room down here. And it's an office and a twice storage place.
Unknown Speaker 59:34
It's really big. And the sun's coming through the windows hairs all lit up. And
Katie 59:40
it was funny because it was just storming a little bit before we got on it was like pitch dark and stormy. Yeah,
Scott Benner 59:47
I I'm sorry. It was what I was gonna say is that I really believe. Obviously, nobody's perfect in any walk of life, right. So while you're running around day to day feeling like I'm doing great. There are things you're doing that are not right. Right, like they're or they could be better or, you know, I sometimes think, you know, in interpersonal relationships, you feel like, oh, we're good. But the other person might be thinking something. And there's a better maybe there's better than what good is, and we don't know, we get really comfortable with where we are. It's hard to talk to people, it's hard to ask for help. But this is just it's such a big deal. Like you can't, you really just can't ignore things and, and be and you know, your numbers are bigger. So they sound kind of more crazy 10 and 11, or whatnot. But the truth is, is that if you're a one c sitting at, I don't know, at an eight, or seven and a half like you, there's better. And it's not that it's not it's not any harder to be seven and a half, or eight and a half. It's no no, it's not it's not a ton more work to be six and a half versus seven and a half, like I mean, look at you. You're in the fives from 10. It's, it's insane. I really, I don't even know what to say. Like when you said that. It's crazy. Congratulations, I guess.
Katie 1:01:08
Thank you. Honestly, I would have never thought that we would be here. So it's such a good feeling to know that we can do it. And then as my boys get older, that they'll be able to do it.
Scott Benner 1:01:19
I'm glad. I'm really glad for all of you. I'm I hope we stay in touch over the years because I'd like to know. I'd like to maybe get one of those. Get get one of those kids older and get them on the podcast in a couple of years. And I'd love to know about that. It's really interesting. It really is. Can you hang on for a second? I have a question for you. That has nothing to do with this podcast. Okay, good. Thanks so much for coming on. I really appreciate it.
Unknown Speaker 1:01:40
Thank you for having me course.
Scott Benner 1:01:41
A huge thank you to one of today's sponsors, g Vogue glucagon, find out more about chivo hypo Penn at G Vogue glucagon.com Ford slash juicebox. you spell that GVOKEGL Uc, ag o n.com. forward slash juice box. And of course the Contour Next One blood glucose meter. Check them out with the links that are in your show notes of your podcast player, or there's links at Juicebox Podcast comm if you can't remember Contour Next one.com forward slash juice box. And of course that T one D exchange is that T one v exchange.org. forward slash juicebox.
Thank you so much for choosing the Juicebox Podcast. I'll be back soon with more episodes just for you. And a special shout out to all of you that take the time to put up those great reviews and ratings wherever you're listening. And of course, a special special thanks to everyone who shares the show with someone else. You're helping it to grow every day. It's absolutely fantastic of you to do and I could never say thank you enough.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#431 Switching to an Insulin Pump
Community Feedback
The Juicebox Podcast: Type 1 Diabetes social media community sent their tips for switching from MDI to pumping.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends and welcome to Episode 431 of the Juicebox Podcast. Today's show is about switching from multiple daily injections to a pump. And what I've done is gone on to the Facebook page for the podcast and gotten people's feedback about what was most valuable to them when they did the switch from injections to pumping.
Before I jump in and get started, I'd like to remind you to check out T one D exchange at T one d exchange.org. forward slash juicebox. And here's why. You can support T one D research and the Juicebox Podcast by checking out the T one D exchange because they're looking for type one adults and caregivers who are us residents to participate in a quick survey that can be completed in just a few minutes. You can do this survey from your phone or your computer. And you never have to leave your home or visit a doctor's office to make a substantial impact on Type One Diabetes Research. This is 100% anonymous HIPAA compliant. And every time one of you completes the process by using my link, T one d exchange.org. forward slash juicebox. You'll be helping to support people with type one. And the show past participants just like you have helped to bring increased coverage for test strips, Medicare coverage for CGM, and they've helped to change the ADA guidelines for pediatric ANC goals, you can give back in just a few moments. Okay, I've done this a couple of times. And it's incredibly popular. So we're doing it again, and went on to the Facebook page Juicebox Podcast, type one diabetes, it's a private page where listeners can talk about whatever they want. It has well over 8000 members at this point. And it's just a hotbed of discussion around diabetes management. So I put the question up there. For those of you who have transitioned from MDI, to pumping, please share your tips, things to look out for and remembrance. Here's what came back that I thought was very interesting. Right off the bat, Nicole says, start with what the endo suggests, but only give them 24 hours. If you've listened to all the podcast episodes, you know what to do, if you have a Dexcom Be bold. Marianne said that Initially, it was a little difficult to get over having a device attached to her, but that she eventually did. She said, you'll probably need to adjust your dosages with the team, be prepared for that. And nothing's really permanent. So if you don't like it, she's like, just send it back. She also suggested trying to create a time for the transition. That's a less stressful time in your life. Because there is a commitment involved in understanding it. I take Marion's point, but I also think sometimes there's never a perfect time. So I guess, you know, figure out what would be best for you. But I would caution against waiting for the perfect time. And I would also caution against immediately wanting to give up, because it is going to be different. And if you've been doing shots for a while, and succeeding with it, you know, you might just be used to things working. And the truth is you're going to have to start over might not just work perfectly immediately. Jen said that she switched from MDI to pumping over 20 years ago. And all she really remembers was being terrified. She got a quick doctor's office visit tiny bit of training, they sent her home. But she called technical support a number of times the beginning. So she wants to let you know not to be afraid to ask for help when you need it. Katie says not to forget that you're no longer using a slow acting or long acting insulin like levemir, Chrissy but one of those that your pump is giving you all of your insulin, it's doing your basal insulin, as well as your meals and corrections. So if there's a problem with your pump site, you need to be aware that DK a can set in much more quickly than is likely with MDI. So if you get up in the morning, and you're you know, MDI and you shoot your your letelier Lantus, let's say, it's in there, it's doing something, but if you get up in the morning and put a pump on and there's some sort of a problem with the site and you're not getting your basal insulin, you may not know right away. So you know, what I would do in that situation is test more frequently or pay attention to your glucose monitor if you have one. In my opinion, it's not something to be scared of. It's just something to remember. You're getting your basal insulin from your pump now. Ashley said that the first few pumps that she put on just didn't go well. And she didn't realize that she could have them replaced. infusion sets or if you haven't on the pod, the pot itself, and she was just throwing them away. But if you have a failure, especially in the beginning, when you don't know what you're doing, call the company, they very well may replace your items.
That would lead me to say that it is not uncommon in the first week or so of using a pump to have user error with the insertion or wearing of the pump, that it's important to, you know, keep trying get information, don't just think that the first experience you have is how this is going to be now because there are a lot of people who use insulin pumps of all different kinds very successfully, all day every day. So when you're starting at the beginning, and it's not working, if it's not working, maybe look inward before you look outward is my best advice. From what I've seen people talking about online all these years. Josh says that his remembrance for the beginning was that he just immediately felt more in control. And he started tweaking his basal insulin and extending his boluses that that made him comfortable. Amy brings something up that I see a lot. They had fairly good control with MDI and then move to a pump and recognize the transition, that it's not just a flick of the wrist, and everything's okay. Again. What I would say that I notice is that sometimes doctors offices can be careful when they set up basal insulin, I guess they think of it as careful when they set up basal insulin for the first time. So say you've been doing MDI forever, and you get 24 units a day. What I would do, there is the quick math and say, Well, maybe I'm about a unit an hour that. But sometimes doctors offices are scared to send you out dollar for dollar from the way you did it to the pump. And they kind of go without better high than low theory, and a lot of them will take back some. But if it was me, if Arden was using 24 units a day of basil, insulin, I'd start by setting her baseline one unit per hour. And I'd see what happens and make my adjustments from there. I guess the problem comes in where the doctors don't want you to touch the basal insulin. So they set it low to show where the highs are. So they can come back in later and add insulin. Being a person, the way we are here that makes those changes on our own. I would start about where I thought because here's what I see happen. Those ratios are kind of lost in the moment for people often. And what happens is, instead of thinking, Oh, I used to use 24 units a day, MDI, and now I'm only using 19, or something like that. I'm probably not using enough basal insulin, they think pumps don't work. So your brain makes this illogical leap that feels logical. And then you get caught in a little bit of a, you know, a shitstorm. And if you don't have a doctor's office that quickly gets back with you and makes adjustments, which a lot of them don't do sometimes, then you start blaming the pump, and you start having these feelings like I was better on shots, you know, and you could lose faith pretty quickly. I've seen that happen a lot. So that is definitely something to look out for. Some arrow warns that once you're on a pump, it's not a free for all of food, just because it's easy to Bolus. So you know, do your best to stay on track with how you eat. She also mentions that it's possible your insulin usage might go up, and that that's okay. I would say it's also possible that people lose track of the fact that they were taking 30 units of basal insulin of one kind. And using, I don't know, let's say they use 20 units are 25 units of, of, you know, novolog fast acting insulin for meals and corrections. So in their head, they're only using like 25 or 30 units of insulin a day because people just generally don't think of basil as insulin. For some reason they think of it when they're MDI, like, I inject this one story of the day. And then my fast acting insulin is from meals and corrections. Somehow the two don't go together. To me, that might be where some of that comes in is then you move over to a pump. And instead of using 30 and 30, you're using 60 of all one insulin. And I guess I'll just say here in case people don't understand that a fast acting insulin like a nova lager, a human blog, Arden uses a pager there's fiasco, those kinds of insolence. Go into the pump, and you get little bits of it, you know, spaced out all day long to act as Basal and then you get more of it to act as a Bolus. So you're used to using to insolence on MDI. Going forward with a pump, you'll only be using one Bob says how backup supplies, things will fail from time to time, and you need some backup supplies. He's
talking about MDI stuff. Don't give away all your needles. I still have syringes from when Arden was four years old, and we still use them once in a while. Bob's 100%. Right? He says, and if you're using it on the pod have a paperclip around. So if anomaly so different pumps have different situations where they're going to all fail, at some point, something will happen to the flow of insulin. The pump will recognize it and shut itself down for safety reasons. They all do it. When on the pod does it it beeps and sometimes the beeping doesn't stop and you have to flip it over. There's a little hole in the back and you stuck a paperclip in there, and it stops the alarm. So a paperclip is definitely something to have around. Bob. You're 100% right? I seem to remember one time and Arden was young and it happened at a baseball game, we use the post of Kelly's earring to stop it. That was a desperate moment. She now says you're not going to learn everything in one day. It's trial and error. Pay attention to your CGM. If you have one adjust accordingly. small bumps and nudges. She says I have anxiety and was freaking out when I didn't have good numbers at first, but I had to just keep adjusting. And now she's in range 80% of the time and she's happy with her pump. Tara says that patience is key. It can take a few days or even weeks to get all the settings correct. She said they started without a Dexcom. So it initially took longer for her son. Since then they've changed pumps twice with the CGM. And with being bold and the transition went much faster and smoother. what she's saying is, is that when you can see the blood sugar, and you feel the reading into what she's saying, but I feel like what she's saying is when you can see the blood sugar in real time, and you have that faith in yourself to make changes, it can it will go much easier. Some of you will use pumps that offer soft candles or steel candles. She said that they had great success with this the old ones, and that you can get your endo to write prescriptions for changes more frequently if you need it to to avoid absorption issues. And that's with any pump. Misty says it may get worse before it gets better. It takes time to dial in your settings. She's saying again, your rates from MDI will change and change again. But it's worth pushing through. And she suggests that Basal testing is definitely necessary. She found pick a timeframe at a time like I think that to start with overnight, then, you know, pick pick segments of the day to get I have to tell you too, and I say in other parts of the podcast. I'm a fan of as few basil programs as possible. Like I don't think you're outsmarting diabetes by having like a different Basal program every hour. You know, it's point three, five at three o'clock and point four or five at four o'clock and point to like, yeah, I think there's a balance in there you find you can find eventually, where maybe you'll have one, two, maybe three standard Basal settings throughout the day. I think if you start having more than that, there are other things you could be looking at. staska says start with the endo settings. But keep in mind they keep it on the safer side. I said this earlier. We give it a week to see they gave it a week to see how the body was adjusting. But she didn't want to keep things high too long. After a week, they started to make slow adjustments after talking to the endo. And once she was confident and she understood how the body was reacting to the insulin, started making the insulin adjustments on her own. She says you can be as bold as necessary as long as you're paying attention. Joanne said what I said earlier, which is don't panic right away and just decide this is a bad idea if it doesn't go exactly right. A lot of people came in to agree with her about that. And Jessica wanted to offer that she loves using the extended Bolus features and Temp Basal that pumping allows a different Jessica says listen to the pro tip episodes. Thank you, Jessica. Don't rely solely on your endo to make adjustments, watch the Dexcom keep track of your trends and make adjustments was necessary. When you leave the house, it's more than 20 minutes away taking insulin pen as a backup because in case you have a bad sight. So I have to say we don't bring extra insulin with Arden. If we're in what I think of driving distance. Like if it's an amount of time I wouldn't care if I had to go back. If I'm going to try to spend the afternoon at someone's house for a picnic and it's a half an hour from my house. We take extra insulin and some pumps with us. I don't bring needles I have to admit. But her point is valid and worth considering having backups is not a bad idea. Brent makes what I think is a great point. He said that it's just the new ballgame when you start over and this is something I find myself telling people privately as well.
Want to see how to put this, you might be doing terrific on MDI. But what what comes with a pump, you know, maybe you just don't want injections or you want more control over basil insulin or something like that. Anyway, it took you a long time to figure out injections. And it's going to take you a little bit of time to figure out pumping, it is a different game. But at the same time, it's really exactly the same. It's the mechanics of the pump, the nuts and bolts, how it works that you have to get accustomed to. And while you're getting accustomed to it, you will feel like where you could feel like I should say that you don't know what you're doing, which might lead you to have that feeling like why did I do this, I knew what I was doing. And now I don't again, but trust me, it's worth the effort. If it's something you're looking for. Amy makes a great point here. She said that after you're up and running and things are working, take a step back and look at the pump data, right look at what it's doing. Especially she says if you're using an algorithm based pump, because you'll be able to see the increases and decreases and basil when corrections go in and stuff like that. And it'll give you an insight into what's happening. Heather says that she felt like every new step was scary for her son, who was just diagnosed recently, and eight years old. They got their demo on the pod and just left it on the table for a few days until he was ready to try it on. She also figured out things about how to remove adhesive and overlay patches that help hold things on. So there's a little bit of a new world in there. Some people use patches, Arden doesn't we never put a patch on ardens Omnipod. It stays on fine for three days. But I like that she didn't rush here, she went out and got the Omnipod demo, and just was like alright, let's just leave it here till we're ready. I think that's a good vibe. Even though this episode doesn't have a sponsor, it's a great place to say, I really do believe when I say during the app in the ads for Omni pod, one of the greatest things about Omni pod is you can get a free no obligation demo, you can actually try it on and where'd the other pumps just don't lend themselves to that. But on the pods tubeless nature makes that accessible to you. My Omni pod.com forward slash juicebox to get that free demo. And you're helping out the podcast if you use the link. Allen's recommending the book pumping insulin which I've never read, but I've heard so many good things about I'm absolutely happy to say it here. He also wants to point out that the information that's available in doctors offices can often be lacking. And that's what led him to pumping insulin. He said back in. Let's see back in 2007. My doctor at the time told me they'd write a prescription for a pump. But if I needed help with it, I'd have to get somewhere else. He said he appreciated the honesty but finds that a little frightening. Lauren says keep in mind that you are probably rounding up your insulin amounts of MDI. So the same ratio on a pump might not work. So this is the exact opposite of what I was talking about earlier. But it's still really valuable to say that you might what she's saying,
Laurie, I'm Lauren, I'm sorry, Lauren, I'm speaking for you here. But what I'm saying is you might have been using a unit or a half a unit because that's what you could measure with a syringe when maybe point four or point six or 1.1 was more like what you need it. Brianna says to do your research to decide what pump is right for you. She spent a long time looking at the pros and cons of all the pumps that were on the market. She says that she eventually found that her body responded differently to insulin going in through MDI and through a pump that there was a big learning curve for she had to Wendy for 19 years and was previously on a pump years ago as a child but didn't use insulin correctly then and eventually transitioned to MDI, having been well controlled with MDI. She just thought the transition to a pump would be seamless. And it wasn't. Kristen says Try not to put too much pressure on yourself when you make the switch. She found it stressful to learn to use a new piece of equipment, and says give yourself or your child some time to adjust. And you may hate it at first, but give it time. She said it can be strange to wear something on your body at first, but one day, you'll probably barely notice it. I must say that I've worn a couple of Dexcom and some Omnipod demos in my time. And I have to agree with that. I've obviously never used them for insulin or for actually taking care of diabetes. But when I've worn the things myself, I have forgotten that they were there eventually they do become pretty seamless. And that's probably hard to imagine, especially for parents who are looking at their kids and thinking oh, they're so small and this thing, but I do think you just get accustomed to it. I know Arden Christian continues on that for her switching to pumping was life changing. It just took time to adjust. She says as far as management goes, you already know how to use insulin pumps to the same this is a great point that I really want to echo. You're just delivering the insulin a different way. That's it. The basil is going in a different way. The boluses are going into Way, instead of pushing in a needle and pushing on a plunger, you're pushing a button, it's going through a tube, she finishes by saying, take your time. And if you need help, come back to this Facebook group will help you Kaylee's saying something that I've heard people say before. A pump is not a cure for diabetes. And while it makes life much easier with type one, or type two, I guess if you need insulin, it still sucks, you still have diabetes, it's going to be work to learn a new method for both you or if you have a child for your child, too. Don't forget to write down your settings, she said. So you're not scampering around trying to remember things. And remember that technology can fail at times. So you're gonna want to not just rely on that programming to remember all your settings forever, write them down somewhere. But what she's saying is valid, that sometimes you can hear people outside of diabetes, say, Oh, do you have one of those pumps, and they say it like, Oh, you must have if you have a pump, it's probably just super simple, right? Probably makes the whole thing go away. If you're feeling that way, like a pump is just going to make diabetes disappear. And it's not going to you're still gonna have diabetes, you're still gonna need to Bolus your meals Pre-Bolus you know, understand your settings, just the delivery of insulin is going to be different, easier, in my opinion, and you're not going to get stuck as much, which is a big deal to me, Arden also being an omni pod user, I really enjoy the fact that she does not have to take her pump off to bave or to swim, which means we can get a nice stable basil setting and use it 24 seven kgs just jumped in and thanked me for doing the episode and said that they've been MDI for three and a half years and the idea of pumping scares everyone in our family. And I'm, I've got to tell you hate. That is unfounded fear, you really don't need to be afraid. You're just delivering the incident a little differently. You get rid of the shots, and you're picking up your ability to manipulate your basal insulin and create extended boluses. It's not scary. I know you're scared, but trust me, it's not actually scary. Christy said she wished that someone would have told her that or on the pod beeps to let you know when it's done. She was in a board meeting the first time it went off and she had no idea what to do. Christy, I would tell you that the on the pod came with a book and it would have explained all that in there. But I get your point, it would be nice if someone would just go over it real quickly with you. That's one of the great things about I don't know about other pumps, but on the pod for certain. let you know when your reservoir is getting low, let you know when it's coming time to change it. It's good stuff. Linda says they got a pump quickly and not had and at that time had not known about the podcast. So they were very reliant on their endo team for help. She said her diabetes educator was awesome and called several times after we placed the pump. In the days and weeks that followed. They were calling to make sure everything was going good to help with adjustments. This is great if you get this kind of no good knock on some wood Good for you.
She still says she remembers being overwhelmed at first by all the steps that it took to replace the site and being afraid that she'd forget something. That's just the I get that but that's the not knowing right? It's like you don't know what you don't know. So you're worried about everything. She has a tea slump pump. She said it's user friendly, told her exactly what to do. Her biggest advice would be to just know that there will need to be adjustments made. Julia says something I've heard a lot of as well. She remembers feeling like she'd just been diagnosed all over again. We kind of touched on it earlier, but it could give you that feeling. Heather says take your time. Listen to the instructions on how to change your sight. And if you're getting persistent highs, it could be that your candle is bent or something like that happened while you were changing your infusion set. We've only ever had that once where Arden got a bent canula and it took a couple of hours to figure out because we were swimming and she was away from her CGM. Had she been right with her CGM. At the time we would have noticed the rise right away. And he says I remember being in high school when pumps started really being used that her endo was all about it. Her mom really wanted her to get it and she didn't want anything to do with it. She didn't want the tubing, the pumping attached to her all the time, the newness of it. She just didn't want it. She got a two pump and had it less than a year and hated it. She'd get it caught on doorknobs drop it never had a pocket to put it in. She was in private school. She wore skirts sounds like everything was not going well. It wasn't until her sophomore or junior year of college that she got an omni pod and it was a game changer. Oh, well. Thank you my Omni pod comm forward slash juice box. That was nice of you to say any Thank you. Carmen, figuring out how to adjust the basil rates on time of day was a huge advantage. So you know my daughter you guys hear me talk about all the time but Arden needs less insulin from basil overnight than she does during the day. And you have the ability to make those changes you can say from midnight to seven, I want it to be point nine, five, but from seven to, you know, midnight, I want it to be 1.2. Sara says she's the type one she's had it for 29 years she used the pump for about 13 years, got tired of it went back to MDI was never super comfortable with extended bonuses and stuff. But she says, however, I am now trying to regain better control, and I'm about to switch back to a pump. She's got a Dexcom g six now, for about six months. She loves it and she's eager to get going with a pump again. And she's hopeful to lower her one season the sixes Sarah, I definitely think you can do that. Christine's talking about the power of Temp Basal, and extended boluses. There's things that I think a lot of people don't think about. I talked about them pretty extensively with Jenny in the diabetes pro tip episodes. I think these things are amazing tools that pumping offers. And please take a look at those episodes and try to figure it out. Dee says that when they started on on the pod, she had a couple of errors in the beginning. And it all seemed like a pretty big mess. But she stuck with it. Just remember basil is not going to be right right away. And the need to make changes. It's obviously you're hearing a lot of people say the same things because it's just what happens. Megan basil testing and patience is huge, especially if you're moving to an algorithm based pump. Like the Medtronic 670 G, for example. Both of these systems should be started with the algorithm off until basil testing is complete. So if you're thinking about doing that, she's 100%. Right? If you're starting with an algorithm, you start with the algorithm not working so that you can get the basil right before you start expecting the algorithm to do something. She said juicebox listeners know the importance of basil testing however, it seems there's not enough follow up in the transition from MDI. long acting insulin to pumping basil rates. I very much agree Megan it's a we do not talk about basal insulin the right way overall. Tara says if you have a younger child, oh, this is a good point. They're on the pod like ticks as it's getting ready to go in and she said it made her daughter anxious. They gave her headphones and an iPad so she wouldn't hear it. It's click click click. I have to tell you Arden's been working on the pod for 13 maybe years, and she still counts the clicks as they go in. So I hear you. I think everybody within the pod knows about the clicking. But the clicking is it's part of the game. It's how it makes tension to put the insert. It's not important. It's just you know how it works,
but the headphones to eliminate you being able to hear the clicking smart. Courtney's reminding us that the pump is only as smart as the settings that are in it. She had to remind herself that the pump was only going to do its job once she did hers. Here's a fun story from Danielle. She said my daughter was six years old when we told her how she wasn't going to have to get shots anymore because she was getting it on the pod. So she was very excited. The first time they put on the pump. The clicking and insertion scared her but they told her Don't worry, because you're not going to feel it anymore. No more shots. Then it came time to give her her first Bolus. They explained it again no more shots that her daughter ran from the house down the street to avoid the Bolus. She said when they finally got her to calm down and gave her the insulin. Her eyes went very big and she suddenly realized no more shots. She thought she was going to feel the insertion every time she got insulin. That was the one thing they didn't think to explain to her. That's a great little piece of advice and an amusing anecdote. Sara just says please, everyone share your tips so we can get this episode up. I need it. We're making the transition soon. Big smiley face. That's really great. People here we're waiting for insurance approval. A lot of people in the thread are just talking about we're getting a pump. Laura, I would say that the fear of making the move from MDI to pumping at least for her fear of change. Yeah, what's what we already doing something it's working. And then she said we should they were worried about and then she says they were worried about cost. Is this really something everyone would like? So a lot of those concerns? Okay, good. I was hoping this one came up with. Okay, good. I was hoping this one would come up. Martha says that her total basal insulin went down, that the initial formulas for pump therapy starting with about 80% of original basil dose had to be dramatically reduced. She went from injecting 18 units of to Joe to 12 units on the pump. See, everyone's not the same. And I'm not saying this happened to this specific person. But there are many people on MDI who are using way too much basil and find themselves feeding their insulin constantly. So as long as they eat on a certain schedule, they don't notice that they're using too much basal insulin, and it mimics really great control because you're being held low and steady. And as you try to drop you add food. I hope that makes sense. So there's a lot of different scenarios people find themselves in with their Basal. Some people don't have enough some people have too much, you know, etc. You'll find out who you are. When you change to a pump. Jennifer says, if you're using a tube pump, remember that you're going to disconnect it for, you know, bathing, for example, she says, Be aware that your child may take the pump off for a shower and forget to put it back on. Of course, whether you're a child or an adult for getting to hook back up to your
Unknown Speaker 30:29
pump,
Scott Benner 30:30
we know you don't have insulin, and you will be surprised how quickly your blood sugar will rise to a dangerous level without any insulin. Tommy asks for me to talk about transitioning during the honeymoon period. Tommy what I would say there is if someone's honeymooning, and they maybe don't need very much insulin or at times it feels like they don't need any for 15 or 20 minutes at a time. Your ability to shut basil down or to tamp it back is going to be amazing for you. Here I'll bring this up. Never turn your basil insulin off. So you don't suspend your pump. When you want your basil to go away. You always do a Temp Basal decrease, because when they end, you go back to your regular Basal rate. suspending insulin and again, maybe forgetting to turn it back on is another quick way to get into DK always Temp Basal never suspend. Now I hope all of you find the diabetes pro tip episodes that are here in the podcast. They begin at Episode 210 with an episode called diabetes pro tip newly diagnosed or starting over. But if you've been through them, and just want to get back to some things that might be specific to this to 19 is about insulin pumping to 26 about the perfect Bolus setting basil, insulin 237 Pre-Bolus ng 217. These are all things that might have more stuff for you about using a pump like episode 218 Temp Basal. There's also one here about fat and protein rises, which we'll talk a little bit about using extended boluses. And that's Episode 263. You can find them all in your podcast app or at diabetes pro tip.com. All right back to the list. Kyle says Don't forget to rotate your sites, that's a great one. Don't always put your pump in the same exact place. Oh, he also says you can do a Temp Basal like 0% like Temp Basal off when you first start pumping until your old injected basil insulin gets through your system and then boom, pop it right back on again. You can just sort of match them up as close as possible. So you don't have an overlap of your injected basal insulin, and you're pumped basal insulin on your first day. Eva says that for her pumping was the first time she had any concept of insulin onboard, since it was now being displayed right there on her pump and sometimes scared her away from being as bold with insulin as she was with MDI. It was only once she pushed that out of her head that she was able to add insulin when she knew she needed more. So we talked about insulin on board through the pro tip series, I hope you've heard them. There's a lot about how your settings get set up on your pump, your doctor chooses an amount of time that they think the insulin stays in your system. If that number is not accurate, then the pump can imagine that there's insulin, it's still active when there's not. In other words, imagine that the pump thinks that the insulin stays in your system for four hours. But really, you use up the insulin most times in three hours. Then between that third and fourth hour, the pumps gonna still think there's insulin active in there working and say you go to have like three or four carbs. The pump might say no, you don't need any insulin. You still have some active, but he may not. It's a you'll figure it out. But don't just maybe I'll do an episode of insulin on board with Jenny sometime might be a good idea. Alright, let's see what's next. He says I need this episode. Now. very forceful IV is coming. Carrie remembers being excited that she would not wait. I remember being excited that I would not be as lazy of a diabetic since I would not have to get all the paraphernalia out just to give myself a single shot. But I wish I had a provider that once we had all the settings in would have done the little small test with me to really hone in the settings. Also remember that it's a tool, not a savior or a cure. We've gone over that you're still responsible for understanding. Absolutely true have a backup plan for failures with your pump. It is an electronic device and it could fail. Twain describes learning about a pump as an elephant that's charging at you. I think she's mixing her metaphors you're joining I think you're mixing your metaphors but I love it. I'm just starting this week so I'm a super noob But here is what I know it's an elephant a giant elephant that feels like it is charging you the classes and forms the logging pump the represent The logging, the pumper apps, the sailing start actually starting it more logging. It feels like you'll never see the end of the tunnel, but you get there. So an elephant one bite at a time. So worth it. So where she mixed is she said, I love this. You said it's like an elephant charging it. But I think the saying is how do you eat an elephant? One bite at a time, right? I'm not sure what you did there join. But I like the kid who I like what Vicki does here. She says I can wholeheartedly say it was the worst thing I've gone through in 25 years of having diabetes.
Looking back, I wish I really understood all the terms in the defining diabetes series before getting a pump. I went from MDI and basically had no knowledge of carb counting. I was diagnosed in 95. And I really didn't stay up with it. So overnight, I needed to understand basil correction factor, insulin on board, extended Bolus, etc. Also, she says work with your diabetes educator, when you're setting the basil rates, get them to teach you when you should make the changes. I was on 14 units of lantis on MDI, my diabetes educator who I later fired started me on four units. Yeah, that wasn't gonna work out with a pump. And would only let me increase it if she said it was okay, they need to teach you how to use the pump. I agree. And Vicki, I appreciate you bringing up the defining diabetes series. There is a series within the podcast called defining diabetes. And this is going to be a big deal for you. Because new terms are gonna pop up with a pump. If you don't know what they mean, you might as well be reading a different language when someone's explaining it to you. You need to understand the terms that you're going to be using. And I do believe, and I'm just you know, I know I made them. So I might be a little biased. But those defining diabetes series are an amazing way to learn a lot of things very quickly. Hey, Katie, you have a great post here. But we covered everything that you said already. But I want to thank you for it. Oh, I hear Jennifer says I recall being nervous about my son accidentally dosing. When he first got his pump. He had an animus Ping. So I learned how to lock the pump or use the second security feature that helped ease my anxiety and apparently there was a pin number she could use. Also, I recall being thrilled that our world got bigger once parents don't have to worry about the needles, he got invited to a lot more playdates and sleepovers. People were just more comfortable with the electronics. That's an excellent point. And leads me into the idea that I'd like to bring up which is that I know the Omni pod has limits that you can set I'm sure every other pump those as well. Max Bolus max basil rate so that you can't by mistake want to give one unit give 100 units as a Bolus or so you can set it wherever you want. I think ardens max basil is set at like six units are seven units an hour. So I can't mistakenly type in nine or 10 or 77, or something like that. And same with her Bolus. I don't remember where it's at at the moment, but I just took the biggest Bolus I've ever made in my life added a couple of units to it and limited it at that so that somebody doesn't end up doing, you know, 175 if they mean 17, but I'm also not in a situation where if suddenly she eats something more than usual, the pumps not stopping us from giving a couple of more units than we normally do. It's a very important safety feature. Please check it out. Kelsey, you're asking a lot of good questions here in the thread. They're all covered in the diabetes pro tip episodes. Stephen says best tips I got were in my original training from a CDE, who was also a T one D. The first was about changing sites, be sure to prime the kanila and add the appropriate amount of insulin to create the puddle of insulin so it can aid so it can enable the insulin to start the absorption breaking the clumps of insulin into single molecules so the body can use them. Steven, I am not following you because Arden's never used the tube pump, but I trust you as a great person on this site. So I'm going to continue reading. The second great tip was to use skin prep as a skin barrier. And adhesive enhancer been using it for over 20 years. The third was to understand that the basil rates will change and that the insulin to carb ratio will change no matter what you do. Don't take it personally, Steven, I'm gonna say I'm guessing tube pumps get air in them, you have to prime them through. It's not something I understand. Because I've never used the tube pump but I do know it's important. So if you have a two pump, make sure you understand how to prime it. If you have an omni pod, it takes care of that automatically. And what else did I want to say here? I just had a thought in my head Steven, what the hell you made me think of something and now it's gone.
Unknown Speaker 39:35
Oh, Tim, what
Scott Benner 39:38
about basil rates? I got it. Look at me. I lost my mind yet. Basil rates are going to change and that's whether you're MDI or you're pumping, you're gonna gain weight become more or less sedentary. There's all kinds of reasons why the amount of insulin you'll need will change, hormonal changes. It's not ever going to be set it and forget it, you're never just gonna be like, Oh, my basil rate is point seven, five an hour. I'll never think of that again. Don't think that's gonna happen. Jenna, this is brilliant. Start your first few sites around the same place on the body. for consistency. different locations can require different basil rates. Like for instance, Arden's thigh needs a little more insulin than ardens arms, very good, her belly doesn't need as much as her thighs, etc. That could be different from every for everybody. Jenna goes on to say different locations can require different basil rates, Pre-Bolus times and just overall insulin need and action time. Personally, when doing MDI, I recognize that I have poor arm absorption and great belly absorption. Jenna has great belly absorption. If you're ever on the podcast, Jenna, that's gonna be the title of your episode. So I started putting my pods primarily on my belly for the first few months. So I could figure out how to best use my pump. And its features without adding confusion of absorption differences. That's pretty brilliant. Also a great time to re mind you that you can't just put the pump in the same exact spot over and over again, very similar to you just can't inject over and over in the same places, you have to have a few sites and you should rotate them often. And don't forget that please. In the same vein, Arden has times of the month where she's more easy to control and less easy to control. I don't think that was English. But when I know she's going to be harder and need more insulin, I make sure that her pumps are on her sites that work better. And times when she's going to be easier. I put it on the sites that need a little more work. So it's not that drastic, but it is significant enough to mention that you should be paying attention to it. Okay, well, that's it. I appreciate everyone jumping in the thread and leaving their thoughts remembrances and tips of switching from MDI, to pumping. I remember the time personally as not that confusing or different, because I was pretty bad at it with MDI. So I didn't notice that I was bad at it with pumping, just just move one show from this side of the room to that side of the room. You know what I mean? I can say now looking back with hindsight that everything that everyone mentioned here is well worth understanding. But in the end, you're changing insulin delivery systems, you're eliminating using two different insolence, you're using just one fast acting insulin that's being dispersed by the pump, both for basil and Bolus. You need to know the terms of the pump stuff, because otherwise you're like, I don't understand what a Temp Basal is. You learn that kind of stuff, you learn what a kanila is that kind of thing. You start figuring out what spots on the body work better, which spots need a little more insulin, get that basil insulin, right? Don't sit and stare at it, especially, especially just do the math. If you were using 10 units a day, and now all of a sudden you're using five units a day of basil, insulin, and you're like, oh, the blood sugar is always high. Please don't say pumps don't work. Think, why are we not using all the basal insulin we used to? That's just such a big thing. Just I just see it so much with people. And here's one last tip for me. When you're wearing an insulin pump, and you think this site might be bad for whatever reason, and you're, you know, pumping in insulin, you're not seeing anything happening, you're not sure if the site's bad. Or if you just have a high blood sugar and you're not using enough insulin. making it an injection, as a correction will bypass the pump, right? So if you inject in that scenario, and your blood sugar starts to move down pretty quickly, that's a good way to figure out that the site might be bad. You say makes sense, Scott, but what I think of it in the moment, you probably would not, which is why I've mentioned it here. Anyway, I hope you enjoyed this, I really want to thank the people on the private Facebook group for the podcast. It's called Juicebox Podcast, type one diabetes, I hope to see you there. And that's it. They don't forget the T one D exchange. If you can go to T one d exchange.org. forward slash juicebox. And get involved in the registry. You'll be helping people with type one diabetes, a huge amount you'll be helping the show. That by the way is for us residents who have type one diabetes or us residents who are the caregivers for someone who has type one diabetes. And because we talk so much about it. I know there are plenty of other pumps. But of course the Omni pod is a sponsor of the show, and they offer a free, no obligation demo, it'll be sent right to your house, you can actually try it on my omnipod.com forward slash juicebox. There's
still links in the show notes and links at Juicebox Podcast comm I forgot to mention that the defining diabetes episodes are of course available, they're spread throughout the podcast. But if you go to diabetes pro tip comm and scroll to the bottom of the page. There's they're all there. So you can find them that way if you just want to find out what number they are and then Don't listen to the media player or you can listen to them right on the website. I really appreciate you listening. I'll be back soon with more episodes of the Juicebox Podcast.
If you'd think you'd be a great guest for the podcast, reach out to me by emailing me at Scott at Juicebox podcast.com. I'm currently booking for the second half of 2021 I think that's August or later. I'm looking for anyone who thinks they have a good story. Somebody who really wants to share help people or just want to be involved in the podcast. bonus if you think you have a good after dark episode and you email me, I'm Scott@Juiceboxpodcast.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!