#1151 Grand Rounds: Jon Oden, M.D.
Jon was diagnosed with type 1 diabetes at 11 years old. Today he is a Pediatric Endocrinologist.
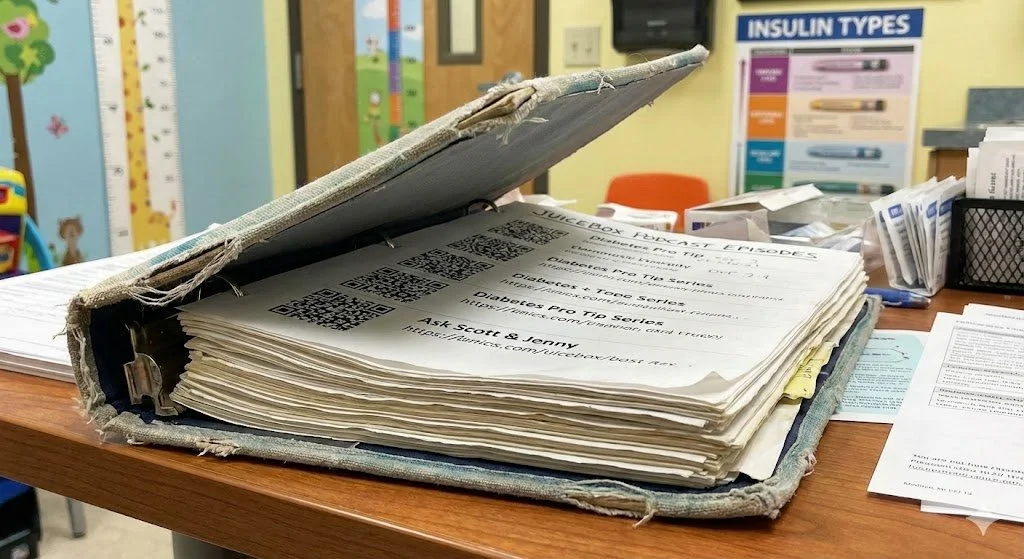
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, welcome to episode 1151 of the Juicebox Podcast
today I'm going to expand the Grand Rounds series. It's not Jenny and I today today, it's Dr. John Oden and myself talking about type one diabetes care. Up until now it's been Jenny and I talking to doctors about what we think people with type one diabetes need. Today we're going to hear from one. Please don't forget that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan or becoming bold with insulin. How would you like to help with type one diabetes research from wherever you are right now? In fewer than 10 minutes? Go to T one D exchange.org/juicebox. and complete the survey. That's it. You need to be a US resident who has type one diabetes, or is the caregiver of someone with type one. And they're very interested in hearing from caregivers of Boys, boys of color, men, men of color, but everyone is welcome. If you're a US resident, you have type one where you're the caregiver of someone who is T one D exchange.org/juicebox. You'll be helping, it won't take much time. Please consider it.
This episode of The Juicebox Podcast is sponsored by the ever since CGM. And sure all CGM systems use Transcutaneous sensors that are inserted into the skin and lasts seven to 14 days. But the Eversense sensor is inserted completely under the skin lasting six months ever since cgm.com/juice box. This episode of The Juicebox Podcast is sponsored by the contour next gen blood glucose meter. Learn more and get started today at contour next one.com/juice box. This show is sponsored today by the glucagon that my daughter carries. G voc hypo Penn. Find out more at G voc glucagon.com. Forward slash juicebox Hello, I'm
Jon Oden, M.D. 2:19
John oden. I am a pediatric endocrinologist in Arkansas. I work mainly at a little rock but go into the Northwest every once in a while. John,
Scott Benner 2:29
why am I talking to you today from where are you at?
Jon Oden, M.D. 2:32
I am currently in a town called Springdale, which is the house of one of our newest pediatric hospitals. For Arkansas Children's. It's our it's Arkansas Children's Northwest. I think our discussion today was born from a couple of my diabetes education people. Roxanna Hutch craft, recommended I reached out to you because, well, I'm an endocrinologist, your podcast is is highlights diabetes quite a bit, which I applaud. I'm an advocate for people with diabetes, and I'm a person who has had diabetes for the past 42 years. And okay, John, how old are you? I am 53 years old. 33.
Scott Benner 3:14
So you diagnosed your 911 11 Oh, damn, you know, I had nine or 11 in my head has a choice. And I don't know why I went with nine. I also don't know why my brain can't figure that out. But that's,
Jon Oden, M.D. 3:23
that's okay. Because I keep thinking I was diagnosed when I was 10. I keep thinking that for some reason. But I was diagnosed in September of, of 81. So I'm sorry, September of 82. So
Scott Benner 3:37
John, you're diagnosed? You're What do you take in regular mph?
Jon Oden, M.D. 3:41
Yeah, two shots a day regular mph? Very strict meals, very strict times exchange diet, if you will. You had to, you know, one slice of bread is a starch. That
Scott Benner 3:53
kind of stuff. Yeah. Now is there in hindsight, other autoimmune in your family? There
Jon Oden, M.D. 3:58
is my mother suffers from thyroid, as does my sister, hypothyroidism. So there is
Scott Benner 4:05
nothing beyond that, though. Celiac? No,
Jon Oden, M.D. 4:09
no. psyllium. But I mean, remember, I mean, my, my, my mother and my sister. You know, they're they're not they weren't born in a time where celiac was a focus. So I can't remember if my doctors ever screened us and I certainly don't know if their endocrinologist screened them. So it's very possible.
Scott Benner 4:26
Can I ask you a strange one that you might not connect? But I asked about because I've been making the podcast for so long. I hear so many people's answers. How about depression, anxiety, or bipolar? Specifically? You mean for me personally, family, like family member even like either side going back anywhere?
Jon Oden, M.D. 4:44
I wouldn't be surprised if there was a touch of depression and anxiety and all of us family members meaning I don't mean to say that in a bad way. They certainly weren't, you know, dark room depressed, you know, they, but you know, every once in a while you could you could probably see the glimmer of some anxiety. My sister and myself. Sure, okay,
Scott Benner 5:02
I just I, over the years and I'm now well over 1100 episodes, the amount of people who will say there's a bipolar I have a bipolar aunt or uncle is kind of overwhelming when you talk about inflammation and, you know, kind of things that we're still learning. Obviously, we're, I think our medical understanding of a lot of things is very young still. So I just like to ask, okay, so you're 11 years old? Just what you do into a day you're eating very specifically, your parents help a lot, or did you get into a rhythm and it was just on you?
Jon Oden, M.D. 5:36
To be honest, it was always on me. And that was not my parents choice. It was mine. From day one. When I was admitted, we were in Houston. So I went to UTMB in Galveston, and from day one nurse walked in, said, Hey, you're gonna start insulin injections. I remember it very clearly, she walked in with this needle that was, you know, six inches long. Not really. They were they were Terumo or BD, you know, big. They were pretty long needles. I took it from her hand. I said, I'm going to do this and ever since then, I can honestly say a nurse has other than vaccinations has never given me a shot.
Scott Benner 6:14
Do you think you wanted to do it? Or did you not want someone else to do it? Oh, that's
Jon Oden, M.D. 6:19
a great question. wasn't afraid of it. So I guess, I guess, you know, it just felt it was on me to take care of it. Okay. And in my practice, you know, you see, you see kids like that. And you know, they're very independent predicts pretty good control. Although, you know, in my instance, it was a lot of obsessive compulsive I want to be controlling things, you know, controlling blood sugar that's part of the reason why my control is so quote unquote good partly why I have as many lows as I do, you know, I don't I don't like to be high. And so part of that is, you know, that obsessive compulsive nature of I want my blood sugar to be x and I'm going to fight to make it x and I want to be the only person that puts a needle in my skin and that's, that's what's gonna happen is
Scott Benner 7:07
that focus that attitude prevailed through your whole life or is that just how you treat diabetes? Or can you also not can I not have the remote control for watching television or something like that? If you take insulin or sulfonylureas you are at risk for your blood sugar going too low. You need a safety net when it matters most. Be ready with G voc hypo pen. My daughter carries G voc hypo pen everywhere she goes, because it's a ready to use rescue pen for treating very low blood sugar and people with diabetes ages two and above that I trust. Low blood sugar emergencies can happen unexpectedly and they demand quick action. Luckily, G vo Capo pen can be administered in two simple steps even by yourself in certain situations. Show those around you where you storage evoke hypo pen and how to use it. They need to know how to use G Bo Capo pen before an emergency situation happens. Learn more about why G vo Capo pen is in Ardens diabetes toolkit at G voc glucagon.com/juicebox. G voc shouldn't be used if you have a tumor in the gland on the top of your kidneys called a pheochromocytoma. Or if you have a tumor in your pancreas called an insulinoma. Visit G voc glucagon.com/risk For safety information. That contour next gen blood glucose meter is the meter that we use here. Arden has one with her at all times. I have one downstairs in the kitchen, just in case I want to check my blood sugar. And Arden has them at school. They're everywhere that she is contour next one.com/juicebox test strips. And the meters themselves may be less expensive for you in cash out of your pocket than you're paying currently through your insurance for another meter. You can find out about that and much more at my link contour next one.com/juice box contour makes a number of fantastic inaccurate meters. And their second chance test strips are absolutely my favorite part. What does that mean? If you go to get some blood and maybe you touch it and I don't know stumble with your hand and like slip off and go back. It doesn't impact the quality or accuracy of the test so you can hit the blood not good enough, come back get the rest without impacting the accuracy of the test. That's right, you can touch the blood come back and get the rest and you're gonna get an absolutely accurate test. I think that's important because we all stumble and fumble at times. That's not a good reason to have to waste a test trip and with a contour next gen. You won't have to contour next one.com forward slash juicebox you're gonna get a great reading without having to be perfect. Oh
Jon Oden, M.D. 9:57
yeah, I you know, I am obsessive compulsive about certain things my wife will tell you I have this compulsive nature to buy vintage audio and repair it and she just gets sick and tired of seeing old tape players. And so there are pieces in my life that that Yeah, I think you can see that. But to the most extent, I feel that it's pretty mild. I'm a pretty open person and willing to hear others others thoughts on how things go. Are you using that
Scott Benner 10:27
word clinically? Or just kind of colloquially?
Jon Oden, M.D. 10:31
Obsessive compulsive? Yeah, I would say mostly colloquially, I think it's, it's somewhat clinical. But over the years, I've learned to kind of manage it. So it doesn't really doesn't really frustrate my family. And I here I am the kind of guy that gets up, you know, right before we go to bed and checks the doors three or four times to make sure that they're locked, even though I know I've checked them 100 times.
Scott Benner 10:54
Maybe it is clinical, John, I'm not a doctor.
Jon Oden, M.D. 11:00
Not medically managed, I guess is what I mean.
Scott Benner 11:05
So you grew up this way? How long does the exchange diet idea? Go through your life? Like when did they because if you're an 81, when when did they give you I'm trying to guess what you get? Like Basal insulin and like 88 around then?
Jon Oden, M.D. 11:20
I never started Lantis? No, no, I always was on mph, I started human log in the early 90s. Okay, the honest with you, if my recollection is correct, and I was one of these people that, you know, I kept my diabetes in pretty good control. And we had to drive 45 minutes to an hour, my parents night to UTMB every, I don't remember, I don't think it was every three months. But it could have been up until I graduated high school. And then I started seeing a dolt. And by that time, I had learned how much insulin to give myself based on carbohydrate volume. So I was already doing kind of a meal ratio before doctors or dieticians had talked to me about it.
Scott Benner 12:02
Yeah, that's excellent. So you saw it enough in your own life? You're like, I'm going to make an adjustment here on my own. Yeah. But what was the what was the measurement of success? Like you said, you were in good control. But how did they tell you where you are? Because it was it? I mean, you didn't have a meter right for a while, I would imagine at home.
Jon Oden, M.D. 12:20
Oh, we so we use those old accucheck meters. So we started using those in the mid 80s. And you know, you had to have a big dollop of blood. And you know, it gave you a range of like 80 to 120 or like a roundabout number, you know, so it wasn't, you know, hugely accurate, it took five minutes to get anything, you had to wash it off with sterile saline, that kind of stuff. It was, you know, very technical. But shortly thereafter, we started seeing meters kind of pop up measure of success was always kind of a one see how many low blood sugars did you have? Were you ever in the hospital? And there was a question on the on the questionnaire at UTMB that always struck my parents. And it was does he use he or she use his or her diabetes to get out of, you know, chores or responsibilities?
Scott Benner 13:07
So a one C, amount of lows. Have you been in? DKA? Do you use this as an excuse? Interesting. Okay. And how were your lows? Manageable?
Jon Oden, M.D. 13:19
I think, you know, back then when we were only kind of checking blood sugars with finger poke. And the chemical Kimmy luminescent strips, you know, that gave you a range or the meters that gave you a range or a roundabout number. I think I probably had a couple of lows a week. But in reality, you and I know that was probably not very accurate. You know, we I probably was experiencing lows once or twice a day.
Scott Benner 13:45
So John, tell me what you call low under what? Less than 70? Or 70? Where do you feel it? Like? Where do you feel like you're not yourself?
Jon Oden, M.D. 13:53
Well, with a rapid drop, I can certainly feel it. So when when my CGM shows me with an arrow down or two arrows down, I'm going for like, I'm going to be very conservative, you know, 200 to, you know, to 90 pretty quickly, I'll feel it, you'll feel a little wobbly. You feel a little, you know, shaky, sweaty. But if it if it's a slow decline, I would say I'd probably start feeling less than 6060.
Scott Benner 14:19
Where can you not help yourself anymore? Do you know?
Jon Oden, M.D. 14:23
Oh, goodness, I've been in a teens and still been able to take care of myself. But then I've had some some pretty significant drops overnight that my wife had had to help me and when we measured it was in the 40s. Okay.
Scott Benner 14:35
Does that happen to you now as much that there's the technology's better, like Does that still happen? Oh, no.
No,
Jon Oden, M.D. 14:45
not that it hasn't happened in years. Yeah. You know, we certainly my onesies have been in the lower 60s upper fives for a while. So Right. Yeah. I would say that it's it's very, very rare.
Scott Benner 14:59
Mm hmm. Now it's just that back then. Right there was, I mean, it's just there wasn't as much precision you didn't have any kind of the main the monitoring was, you know, right catches catch can.
Jon Oden, M.D. 15:10
But I've never I never had a severe low I will tell you I'll be honest, I never had a severe low while I was living with my parents never okay, in one time when I did have a low that required glucagon that my wife had to give me. My mom was actually staying with us. And she did not know how to use the glucagon. About that years later. Yeah, years later. And we found that the times that I had severe lows were always associated with like yard work or moving. So if it was hot outside, and I was really active, and got dehydrated, that tend to predict a significant low and so you know, my wife and I are always like, okay, so you chop down a tree today or whatever. You're gonna go, you're getting loads and loads tonight. So tonight, you're going to eat a
Scott Benner 15:57
lot. What's interesting is what age did that that one low? You're talking about where your mom was visiting where you'd like in your early 20s. And you just gotten married or something? Or?
Jon Oden, M.D. 16:07
I was in my fellowship. So I'm guessing I was in my late 20s. Okay.
Scott Benner 16:13
That's interesting. And what was your management like back then? for that?
Jon Oden, M.D. 16:17
I was on a pump. So I started pumps around the same time. If memory serves, I started my pump and my daughter was one. She's 23 now. So it was around the same time.
Scott Benner 16:29
Yeah. Okay. Do you use an algorithm now?
Jon Oden, M.D. 16:32
I'm on the OP five. Okay, so I used to use tandem, but I switched the OP five because I can I can put it in different places on my my torso and my arms. You like
Scott Benner 16:43
the form factor of the Omni pod? I do. Yeah. And up for that use Control IQ or just the tandem Basal
Jon Oden, M.D. 16:51
control IQ? Yeah, okay. I use Basal IQ for a brief period of time, then I switched to control IQ, I find both platforms are just are phenomenal. Yeah,
Scott Benner 16:59
I agree. Also, it's interesting how quickly they went from baseline IQ to control IQ. They, they almost like, released that first thing like, look what we got, like, approved. And then before I feel like they, they didn't expect the next one to come back quickly, because it was really quickly after that. Yeah, it was it was but the tubing and the form factor meant enough to you to move on from something you enjoyed
Jon Oden, M.D. 17:22
the tubing not so much. You get used to the tubing, I just Yeah, I think it was the fact that the pump sites for me, I couldn't put them on my legs, because I'm a runner. And I couldn't discipline myself enough to carefully remove my shirt, so I don't rip my pumps out off of my arm. I tried it a couple of times. So I developed a pretty significant amount of like hypertrophy around my around my, the front of my torso. So I was like, hey, it's time for a change. So you're
Scott Benner 17:51
overusing your only site that you that you were willing to use. Yeah. I also I don't understand when people say I'm a runner, but that's a different podcast. So you go out and run somewhere on purpose. And nothing's chasing you.
Jon Oden, M.D. 18:03
No, nothing's chasing me. No, no, but I can tell you that I am a an amateur runner. I'm not I'm not a person that runs every day. But I am training to do the half marathon this year in Little Rock, which is
Scott Benner 18:16
all five of your toes pointing forwards still.
Jon Oden, M.D. 18:19
Oh, they are lost. Last time I did it. I lost the the big toe nails, which was a little gross for my kids. Yeah,
Scott Benner 18:26
that's gross for me, John, I don't know you and I can't say it. So it's fantastic. When did when in your life do you say I'm going to do you think you would have been a doctor with or without diabetes? This episode of The Juicebox Podcast is sponsored by ever since and ever since is the implantable CGM that last six months ever since cgm.com/juice. Box. Have you ever been running out the door and knocked your CGM off or had somewhere to be and realize that your adhesive was about to fall off? That won't happen with ever since ever since won't get sweaty and slide off, it won't bang into a door jamb and it lasts six months, not just a couple of days or a week. The ever since CGM has a silicone based adhesive forge transmitter, which you change every day. So it's not one of those super sticky things. It's designed to stay on your forever and ever, even though we know they don't work sometimes. But that's not the point. Because it's not that kind of adhesive. You shouldn't see any skin irritations so if you've had skin irritations with other products, maybe you should try ever since unique, implantable and accurate so if you're tired of dealing with things falling off or being too sticky or not sticky enough or not staying on for the life of the sensor, you probably want to check out ever since ever since cgm.com/juicebox Will links in the show notes links at juicebox podcast.com.
Jon Oden, M.D. 20:04
Probably not, I will be honest I, before I was I developed diabetes I am mistake take a step back, my family comes from my mom's side, a lot of people in the Navy and I have a lot of respect for our military. In this country, right? I had planned to become a naval aviator, I wanted to fly a fourteens back in the day, but then after diagnosis, my uncle and I had a conversation about the possibility of a person with diabetes joining the Navy and in any way, shape or form. And he just told me very, very honestly, and frankly, that No, that wouldn't be possible. And that just broke my heart. So thinking back on the days when I was, you know, with Dr. Travis and Dr. Bro hard at UTMB, which is phenomenal group, great doctors. I just liked what they did. And it's it kind of formed an idea in my head to do that. And that's what I, you know, again, with my obsessive compulsive nature, I just kind of went after it.
Scott Benner 21:02
And when you say that they're good doctors, what in your mind, like with the experience you have now in hindsight, what made them good physicians for you.
Jon Oden, M.D. 21:14
They were brilliant. In my eyes, they were brilliant. They knew exactly what they were talking about. So they had this force when they walked into a room, which I don't know anymore, because I'm one of them. So another doctor walking into a room coming in with this knowledge about what's going on. And what's going to be the treatment strategy is just commonplace for me. But back then there was just this, this, you know, this presence in a room and Dr. Travis walked in. I mean, Luther Travis was a big name and diabetes, and they were they were fortunate to have that you haven't met UTMB and Ben, bro hard. Likewise, if memory serves nephrologist, both of those guys went on to write a book about diabetes not too long after I have a copy of it in my office. It's it's in the 80s I think so it's relatively old. But the other thing was that they were just very kind, very direct. They my mom was very anxious at the time, of course, her son was diagnosed with diabetes, but I just remember these guys has been very patient and kind of walking her through the process and walking me through the process. And
Scott Benner 22:18
I'm going to tell you why I'm asking this in a second. But kind honest and smart is what I heard overall, and that they had a there was a lot about them that they knew what they were doing. Yeah. Okay. And then when they walk in, you put yourself in their hands because of these these ideas, and then they know what they're talking about. They're able to lead you. Right. Okay, so are we talking about leadership? You know, yeah, just, yeah, I'll take let me tell you why I'm asking because I know somebody put you on to being on the podcast, so you might not listen to it. I've been doing a series this year, I've been doing two kinds of concurrently. One I'm having health care providers on and other people around medicine. So anywhere from like a human resources professional, up to a I've had CDs, ER nurses, I've got a doctor on the docket coming up, but these people are coming on. And they're speaking anonymously, we're actually even changing their voices. And they, they're dishing about their jobs. I've heard anywhere from I wouldn't go to the ER that I work at, if I had trouble with my diabetes, to I've been directed over the last 23 years to fire so many people because of their medical problems, you wouldn't believe it. Like like that kind of like so that kind of honesty, right. And at the same time, I'm doing another series with a CDE. I know I don't know if you're very particular about the C D. C 's thing now. But her name is Jenny and Jenny works for Integrated diabetes, which is a company where you can go and they'll manage you remotely and help you. She's type one for like 35 years, she a very similar story to yours, like, you know, grew up on regular mph was eaten on a schedule. She's like, we ate at the exact same time every day, like that kind of stuff. And she's just kind of brilliant about how she talks about diabetes. And she and I are doing a series where we're basically we call it grand rounds. And we went out to the audience of the podcast, which is significant. And ask them what do you wish your doctors would have said to you? What do you wish they would understand, you know, what are you looking for in your interactions? Where do they fall short? And so we're kind of kind of doing this series where we're talking directly to doctors and saying, look, look, this is what people need. And I've just been very involved in it in the last like three or four months now. Hearing from physicians hearing from medical people that my doc I work with doctors that overwhelmingly don't know what they're talking about when it comes to diabetes, or the healthcare system isn't even set up to help people with diabetes. Like you'll come into the emergency room and say like I'm having an issue with my heart, but then you look at them and their type two, for example, and they have, you know, significant gaps and how they care for themselves but nobody even explained to them what they're doing wrong. And it's and sort of just trying to parse through the whole thing. So just to hear a person like yourself, who has good control over a lifetime, is an endocrinologist and thinks back on their doctors as being good. I was really interested because I, there's this phenomenon that happens when people come on, and I'll say, What do you think your doctor and like all my doctors, fantastic. And then through the course of the conversation, I learned that they're a one sees in the high sevens, it has been for 10 years, and I'll stop and ask them, Why do you tell me your doctors, fantastic if you're a one, see 7.9. And then they go on to say, Oh, they're lovely, very nice people, you know, and you tend to realize that the personal partner, they liked the person, but the person is not really doing a good job for them. But when they think about it, they think they're doing a good job, because they like them. Does that all make sense? It does.
Jon Oden, M.D. 25:53
It brings up a lot of really sensitive topics, right? I mean, you know, who's responsible for diabetes control in the end, right? It's your doctor, or is it you, likewise, the workforce today is much different than it was in the 80s, there's a lot of meat on that bone that I think you you're gonna, you're gonna pull off a lot of it talking to the right people, I applaud you that. The first one that you described as a hacker, you were probably gonna find a lot of interesting information, depending upon which hospitals you get people from. And then the second one is fantastic. I think asking people what they wish, a doctor would say is, is information that is not taught in medical schools. And I learned after I graduated from fellowship years after a basic saying that that really helps families out. And that's just to look at them in the eye and say this, this wasn't your fault. And that's just one little piece of a conversation that probably needs to be a lot longer than it is now. So I That's great. Well,
Scott Benner 26:54
I think that what I'm coming up with is that there's some mixture of humanity communication and knowledge that the doctor has to have. Yeah, sometimes. I'm not trying to be funny, but sometimes what makes you a good doctor does not lead you to be a terrific communicator. And that I'm kind of seeing but but I also at the end of the day, and at the end of it, that's not to blame anybody, right? Like it's a, it's, it would be like saying, you know, I mean, I'm gonna build a building, I want a good engineer, this is not the same guy would ask to put on a community play. Right? Like, like, okay, right, traditionally, like that an engineers mindset and personality might not be, you know, right. For other
Jon Oden, M.D. 27:36
things. You don't have to be a renaissance man to be a good, a good doctor million
Scott Benner 27:40
percent, right? And, but at the same time, when I'm hearing these conversations, I came up with the exact same thing that you said, which is, at what point, if I'm a physician? Can I beat my head against that brick wall? telling somebody? All the good information I have, and feeling like they're going to just ignore me anyway? And there are eight and whose responsibility is it? And I think the answer is it's everyone's responsibility. If I had to push it to one side, I have to push it a little more towards the doctor, because I am making an assumption that they at least have a level of intellect that should allow them to get through this problem. I don't know everybody who has diabetes has that. Yeah, yeah. The the capacity. And that's not their fault, right. So you, and at what point, though, does a doctor burnout and just think, I'm not gonna say to this person, it's not even gonna, it's not gonna matter. Like, what happens when they get to that point in their career when, you know, they mean, they start having lower expectations, I guess, and that stops them that
Jon Oden, M.D. 28:43
unfortunately, that's true. And that's not just the doctors kind of mindset, or it's not always just burnout, but it's the way we kind of Metra size, or measure satisfaction in clinic. I mean, we can't look at a family who is not doing what we asked them to do, what is standard of care, for example, and tell them, hey, if you don't do what we asked you to do, send us blood sugar logs, take your injections every day exercise, etc, etc. We're gonna have to kind of take this to the next level and talk to, you know, CPS or DHS, or whoever it is. Because satisfaction for both parties really goes down. You have to build this ability. And I know very few doctors who can do this. And I wish they would give some sort of masterclass on it because I am not one of these doctors, but there are doctors out there who can have conversations that are very direct, and kind, but forceful. Hmm.
Scott Benner 29:42
So yeah, come in from that. That's the one thing you were describing about your doctors that I didn't want to put a label on it first, but they cast a big they cast a big shadow, like they're smart and bright, and we know that they do a good job so that when they come in the room, you kind of step back a little bit and go Oh, there's the guy Like I heard stories, you know what I mean? The guy,
Jon Oden, M.D. 30:01
there's the guy that's gonna tell me how to take care of myself and I want to be in good control.
Scott Benner 30:05
Yeah. And I believe you healthy. Well, what happens? Here's the thing that happens constantly. So I'm in a weird position John, where I have no medical training at all. I have a daughter who has type one diabetes, she was diagnosed when she was two, I was a stay at home dad, she's 19. Now, I started writing a blog about it the year after she was diagnosed, but in honesty was just trying to raise money for JDRF. Right, and then became, I was bad at diabetes like Jen genuinely. And my daughters, they once he was named to the nines, but I went to a very good or she went to a very, very good what you would consider a very good Children's Hospital for for endocrinology. But it didn't matter, right. Like they tell me what to do, I'd go home and do it, it didn't matter. I just didn't have enough knowledge. I didn't have enough tools. And I build them up along the way, as you know, is a very common story. But because I was writing this blog, I started to like, share what was working for me. And then I started seeing it helping other people, right. And I was like, Oh, wow, my experience transferred to you, you end up having the same outcome I have. That's, that's pretty interesting. And, and then I did that for years, 2007, up to 2015. And it was a really, I'm just saying this, for context was a very popular blog, like it had millions and millions of clicks. And then one day, blogging got passe, I guess, people stopped reading. And I pivoted to a podcast in 2015, January. And it was the, I think, the first diabetes podcast that existed. And I started sharing more like, this is what we do. This is how I feel, blah, blah, blah. And now, John, like, the podcast has a collective total of 16 million downloads, or it's in the top 100 chart of like, 48 different countries. And I have a Facebook, private Facebook group with 46,000 people in it, they're almost all active. And if you go in there, and just if you were to go in there right now and say, Hey, my name is John, I'm an endocrinologist. Tell me what about this podcast helps you, you will probably get responses back for the next five days. And, and so the thing, the things that I figured out about diabetes are transferable, and I'm able to share them without knowing you. So without knowing who you are, or knowing any of your details, because it's a one way communication medium. I'm getting people back like maybe once he came down three points, I'm in the sevens now study, I'm in the sixes, I'm in the fives, I know how to use this. I'm very comfortable. Like, all this stuff happens. When I look back, I keep thinking like, Why can't a doctor do that? For people? Like why they come to me because they have no satisfaction through their health care? Like if they didn't, there'd be no reason to go look for help. Right? They, they'd be okay. Yeah, and the only thing I can come up with, is it's the, it's the frequency, it's so that we can keep connecting that you can have bigger conversations, and you can pick ideas out little bits at a time. Anyway, my thought is, and I say this whenever I can, I think endocrinologist should go to like, group appointments. And so instead of someone coming in for 15 minutes, you should come in and sit in a room for a couple of hours where different physicians will come in and speak to their ideas and, and take questions so that other people can hear other people's concerns, and go back and forth. I think it's the only way for that model to like help people in mass. And I don't know what you think about that. I was wondering, like, I know, they like taking out HIPAA things and you know, billing billing, all the problems that would get in the way that do you think that would work, though?
Jon Oden, M.D. 33:48
I mean, you're talking about kind of mass education on a frequent on a kind of more frequent level. Right. I mean, that's, that's no, I think that would work if you did take away issues with billing issues with productivity productivity measures, for physicians, because hey, we've got you know, X number of physicians in the state and they have to see one in every 600 Chuck kids three times a year that kind of process that you're you're describing although check yes, I think that would that would do a lot for kids would take a kind of Herculean effort to pull off but I will I will add a little bit a little bit of a variable in your in your calculus for please how how things kind of move at least in my in my opinion, and part of that is transference of blame on in some of these patients eyes, I've had families that you know that after years of seeing me and getting to know me and building a pretty good rapport I you know, I have to say I love all the kids that I see Yeah, I look forward to seeing them. I think they're wonderful. I think their families are all wonderful in all ways, shapes and forms all forms of, of control, I feel for them, I empathize with them. But a few of them have come to me and said, You know, when we were first diagnosed, I blamed you for the diagnosis, because you were in the room, but it happened. And I think that that baggage carries a lot of restrictive emotional absorption, if that, if that makes sense. Meaning, you know, I can tell them all I want to tell them, I can have a 50 minute long conversation about pathophysiology and Treatment and prognosis, and hey, kids with diabetes do great. If they have good control, but in that mindset, for however long it, it lasts, because it doesn't last forever. I don't think in any families, I think they they come to terms with it after a while. But I think the absorption of information with that with that mindset of I am in a, in a medical community, with a physician that told me my child had diabetes and X percentage of them hold that physician responsible.
Scott Benner 36:12
Yeah, I had this experience when my son was younger, like very smelly had a blockage in his ear, like like a wax buildup, and I took him to the pediatrician who I happen to know. And he sent a nurse in with like a lavage kit. And then he left the room very specifically. And he came back and I asked him afterwards, like privately as like, Why did you run out? And he goes, I don't want him correlating his experience with me. Yeah. And I was like, Oh, no kidding goes, yeah, let them hate the nurse. And I was like, Okay.
Jon Oden, M.D. 36:45
I mean, that's, yeah, we have we have families that, you know, they'll come in with our kids. And you know, they'll say, just trying to be funny, mom and dad will say something like, if you don't behave, Doctor is gonna give you a shot. And I'm like, No, I'm not going to give them a shot. Please don't tell him well make me
Scott Benner 36:57
the bad guy. Right. Right. Yeah, like but, but that is what so, you know, here's the little like, not so dirty secret about the Grand Rounds series that I'm making is, as much as we are talking at doctors. I'm also that's not the only people who are going to be listening. So I am, I'm trying to simultaneously say to a physician, here's what people expect from you. But I'm trying to say to the patients, you know, here's who people are like, they're doctors, they're just people. And you know, here's some of the problems that they have. And you know, some of their hurdles, you have to understand that everybody's got to meet halfway. And you maybe you're the problem, and you think it's the doctor or sometimes, you know, John, I will have people listened to I have a series called diabetes pro tip. It's like 25 episodes, I guarantee you, if you listen to it, you're able to see you'll be in the low sixes. If you if you even reasonably understand what you listen to, if you really understand it, you'll get a high fives I handled whatever you're up to. So but but I'll have people tell me, I listen to the Pro Tip series. I got my a one C down, my variability is better, fewer lows, this whole thing. I go to the doctor, and the doctor says, There's no way you got this a one C without a bunch of lows. And then they Yeah, and then people like No, I didn't but but listen to the chain of events, then John, then they go. No, I listen to a podcast. And then the doctors probably like Oh, okay. And you mean, right? So it gets this missive. And they will tell them bring your A one C up. This is dangerous because they believe so specifically that they must be having a low. So there are physicians out there in maths, who don't even think that a low six is achievable. And if you have one, you're offsetting high blood sugars with very low blood sugars. Yeah,
Jon Oden, M.D. 38:47
yeah. No, I've met those guys. And we had it Dallas. I think we had one of our fellows had a conversation with a doctor out in the boonies somewhere who didn't believe the DCCT. And so his goal for the patients he was seeing was not improvement in a onesie. So I absolutely believe you that there are people out there that say you can safely achieve those kinds of numbers Despite improvements in technology
Scott Benner 39:15
significant. Yeah. Here's some other things that happen all the time. I had a low it. I don't know, two in the morning, or one in the morning, right? And the doctor will tell you, Oh, well then turn your Basal down at like, you know, midnight. They never asked them what they had for dinner, what they ate what the Bolus was three or four hours before, then they make this deficit and in Basal, which then of course creates a high later in the morning. And then then then the next time you come back like hey, I'm getting high at 5am and they they keep messing with it but they don't seem to understand how insulin works. Yeah, you know what I mean? Like that thing you figured out when you were a kid like you You looked and said this amount of carbs needs more insulin I can tell And but it happens so frequently, that I'm going to tell you that the whole basis of the Pro Tip series is just, it's timing and amount. It's understanding how insulin works. And under. That's it. Like, that's the whole thing. Like if if you made me stand up in front of a world full of people using insulin, and said, Scott, you have 30 seconds to fix these people's lives, I'd say it's timing and amount. It's using the right amount of insulin at the right time. I, you know, I don't I don't have time to give you the rest of the details. But that's the entirety of it right there. Go figure that out. Yeah, yeah. But then you're absolutely right. Listen, it's also not brain surgery. John, I was just the first one willing to say it out loud and have my voice recorded that was in, you know, in this kind of medium. If you listen to other diabetes content, they will always artfully speak around giving what they think might be medical advice, I'm don't think I'm not giving medical advice on telling people what I do, they can do whatever they want. And I have a good disclaimer, it's rock solid, John. So don't worry about I just think it's wrong to know this stuff about managing diabetes and not share it with people. But I'm fascinated and dumbfounded by a physician who can't figure out how to adjust a situation for a low blood sugar like, how would you not that my first question would be, what did you eat for dinner? Does it have fat in it? Was it? Did it have protein in it? Did you, you know, what would you eat today? How was your activity? Like just turn your Basal down randomly at midnight, for one low? You saw at 1am? Like, you know, it's just that stuff? That's baffling.
Jon Oden, M.D. 41:32
I think what you'll find, as partly an answer is that the medical community now is struggling. You have primary care physicians who really aren't trained in diabetes, but are in some ways forced to see patients with diabetes, because the volume of endocrinologist is dwindling. Well, there's not that many of us left in this world. And there's many reasons for that, that will take hours to discuss, but I understand your argument. And I think you're right, it's It's baffling to think about, but realize that some of these guys and gals are are having to see, you know, 30 kids in an afternoon and one of them happens to be a person with diabetes. And you know, hey, I have a low in the middle of the night, and they're going to be first thing off the top of their head, the easiest answer is going to be exactly what you described. Yeah. And the answer to make all of that better, apart from improving education, which I wholeheartedly support and work towards, in fact, we're wanting to do kind of a endocrinology for pediatrics conference in Arkansas, which we're kind of crossing our fingers we get funding for but the other other issue would be to explore a way to make sure that either primary care physicians are trained in diabetes, or keep bolster the number of endocrinologist that are being trained, which both of which are going to are, are massive undertakings, would it
Scott Benner 42:57
maybe not be pertinent to to create a new specialty? Like, what why do we ask endocrinologist to know about like, this wide range and diabetes, like there's enough people with diabetes in the world now, like, couldn't a, you know, a specific diabetes endocrinologist be like a lucrative like career for someone? Well, there
Jon Oden, M.D. 43:19
has been discussions about changing the fellowship from a three year to a two year program. And that would be kind of a motion towards that. But think about it this way. We graduated maybe 50 or 60 fellows, every year for the past couple of years, there are hundreds and hundreds of open positions, and more and more opening every month, around the country around the world. Yeah, trying to, you know, kind of find that needle in a haystack person like me, or some of my colleagues that want to do specifically diabetes, which is a chronic disease that is difficult to manage and has social barriers to it, financial barriers to it. It would be hard. Without, you know, I don't I don't mean to say financially incentivizing, but some sort of,
Scott Benner 44:13
kind of It's a hard job. Yeah, you know, I guess John, where I get tripped up is some like 30 years ago, I graduated from high school at the bottom of my class and went to a job at a sheetmetal shop the next morning. And if you ask the right person, you want to come to me to learn about diabetes. So I always feel like if I can do it, like anybody could, like I just I know my communicate. Listen, I understand that my communication style works for a lot of people. I'm sure there are plenty of people who doesn't work for too. That's not the, you know, not up for debate. As far as I'm concerned. I'm sure there are plenty of people that hate me. But like, I know how to talk to people about diabetes. I know how to explain it in a very kind of easily digestible way. And I think that if I can do it, like Jesus, a doctor could do it and been doing it For 16 years, I'm also have a ton of practice. And that is the thing that Yeah, see, I appreciate you saying that because that's even something that I would lose sight of, because I wrote that blog with no, like, it didn't make money. I wasn't trying to make money with it. I, my, my entire focus was to be to share a personal thing with you, John, as I wrote that blog thinking, if I educate enough people about what this is, then one day, if my daughter's out in the world, and she falls over in public, maybe somebody will understand what's happening to her. Like, I really that's what I used to think when she was two years old. And it stemmed from just a newspaper article about a guy that got kicked off the train on the Northeast Corridor, I think, between New York and Washington somewhere, he was on a train, he was strong, they kicked him off at a at a stop. Six o'clock in the morning, when the commuters were coming in, he's laying literally in a stone driveway, and everybody's walking past him and mocking him for being drunk. But this one person who grew up with a sibling with type one diabetes, recognized what was happening with them and stopped and save the guy. Right, because he really had a low blood sugar. And I used to think, maybe odd that crazily, I used to think if I could reach enough people and tell them about diabetes. If my daughter falls over like that somebody might help her one day. And that's a really Pollyanna idea that I had in the beginning, obviously, but I also wasn't trying to make money at it. And I and I was able to have experiences and build on them. And I had feedback coming in from people who were reading so I knew what worked and what didn't work. I could write something and see like, Oh, it doesn't work to speak to people in this tone. It doesn't work to be too specific, too technical. You need to be more you know, it needs to be easier to digest. I had a lot of time to develop this. You should
Jon Oden, M.D. 46:46
well I don't know if masterclass is anything that you should do a masterclass on educating people with diabetes.
Scott Benner 46:51
John, twice a year, a hospital will contact me and ask me to come out and speak to the staff. And then eventually it gets up the ladder far enough at the hospital, somebody puts the kibosh on it never happens. Well, because because I'm not a doctor. Yeah, yeah. But I'll tell you this, John, I did a talk in Austin. This year, or just recently, a couple months ago, it JDRF said, you know, we do these little like, coffee talks, like, would you fly down here and talk to like, there's like, 40 people in our, in our thing, and it's like, if I come down there, it's not gonna be 40 people, like we sold, think every ticket they could for the space, they found, like 350 people showed up. And we had to hold it in the in the Texas State Capitol, which is really cool. She says, so you know, how long do you want this to be an hour and a half? And I was like, No, all day. Oh, well, she goes, people won't sit as like they'll sit. And so we settled finally on 10am to 4am 4pm. So we came in, we did a two hour Jenny came with me. We did this two hour just kind of like chat. It didn't have like, I promised you that Jenny and I talked to each other before we went on stage and said, What do you think we should talk about? And then we went up there started, we talked for two hours, they went to lunch, they came back at one o'clock. We did q&a for three hours. Nobody left. And that evening, I got an email from a woman that said, hey, you know, we did a lot of traveling after we left there. My daughter's blood sugar's normally would have been troublesome in a car, you know, crappy food on the highway, that kind of stuff. And she said, but they weren't they were very stable and and where we wanted them to be. But I don't know why. And I was like, Yeah, you know why? Because we sat around. And we talked about these little like, micro ideas about how to manage and, you know, let's Pre-Bolus And, you know, let's, you know, if you see a high blood sugar, let's knock it back down again, don't look at it. Like, I promise you, there was no slide show. I didn't give any bulleted points. We just had a conversation. And then she left it had a better outcome. And I think that I can I know how to do that. That's the maybe the only thing in the world I'm good at. Chuck, I take your point, that I don't know how a doctor would be expected to accomplish that? Well,
Jon Oden, M.D. 49:06
I think it goes back to my idea that, you know, in some ways, a doctor is kind of looked at in a certain way. And the educators looked at it a different way. And I don't know if there's ever a mix between the two where you can kind of separate it where so Dr. Odin is going to give a lecture on how to manage your blood sugars, and it would it would come off as you know, kind of trite and, and unscientific. Whereas a person like you with a vast amount of experience now and knowledge can give just basic tips and comfortable tips on how to do things in the real world. And that's I think that's a that's a huge bonus for our community. I mean, I think that's great that you do that. The
Scott Benner 49:50
success of the podcast tells me that it works, right because you know, doesn't matter if you have a little kid or a teenager or you're an adult, like I get as many notes from people are like, I've had diabetes for 25 years. Why didn't nobody ever told me this? You know, as I as I do from newly diagnosed people, I think it just works, you know, and this interesting thing that I've been toying with lately, it's nowhere near ready for primetime. But we now have so many conversations, that the way AI works is I've been loading the more management heavy conversations into AI and learning, you can ask it almost anything about diabetes, and it knows the answer. Does
Jon Oden, M.D. 50:32
it really, I mean, so you created that? Or is that just something that's I'm like, I'm
Scott Benner 50:37
using a service, I'm uploading literally the audio from my episodes. And like down to like we have, we have episodes about like how to set your Basal insulin, like the math of your Basal insulin, right. And it's never late. It's just a conversation where we mentioned the math here and there and everything. But you can ask, you can have aI ask that audio, basically, that transcript, I weigh this much. I'm a reasonably active adult, where should I start with my Basal insulin, and they brings back the right range?
Jon Oden, M.D. 51:06
It's, it's, it's creepy and cool. At the same time.
Scott Benner 51:09
Yeah. So I, my my goal is I'm nowhere near done making the podcast but my goal is, the last thing I'd like to leave for people with diabetes is a website where they can just go ask questions about diabetes. Yeah, that's my, that's my end goal for when I'm finished. But for right now, the job is very repetitive. Like, because 150 new people come into my Facebook group every three and a half to four days. And so, you know, you're always kind of saying, you know, you pointed them to the right episodes to get their answers from, and that's also great, too, because they can learn on their own time. They don't have to sit in front of a physician and feel, like judged or like, dumb, which, um, I've, you know, I felt that way, sitting in front of doctors before. So yeah, there's a lot about why it works. Yeah, that's pretty cool. Did I think the truth is, I was talking to somebody about this the other day, they said, every once in awhile, you'll run into somebody who's like, pissed that, like, I don't have diabetes, if that makes sense. I don't know if that would bother you or not, but and I always tell them the same thing. Like, I think I'm able to be like kind of dispassionate about it. Like, I don't have it, right. Like i When my daughter was getting low, I didn't feel low. I just saw a problem that needed to be handled. And so the way I would come up on fixing that problem might be different than the way you would think to if your blood sugar was 50. Yeah. And you know what I mean, and I was motivated, by my, I mean, I want to give my daughter a long life like to be candid. Like I don't I want to die before my kids. Like, that's really like, what most of my focus is. And you know what I mean, I don't want to be a 70 year old guy looking at my daughter, and she's sick. Yeah, yeah, no, I would,
Jon Oden, M.D. 52:45
I would, I would tell you, you do have a form of diabetes. My friend, family members who have you know, my wife has been with me for 34 years. And she has a form of diabetes. Yes, she does. She doesn't have to take insulin. But she does have to worry about blood sugars and exercise and routine and pump site changes. And yeah, she has to do that.
Scott Benner 53:08
It Oh, no, I don't this, I don't discount it. And I appreciate that. I just once in a while online, I'll get some, I'll get from people who are like, I don't know, one person said recently, how much it bothers them that the most popular diabetes podcast in the world is run by a person that doesn't have diabetes?
Jon Oden, M.D. 53:24
Yeah, I don't I don't subscribe to that. I think anybody who has a family member that they love and care for with diabetes has a form of diabetes, it's not path. You know, it's not necessarily affecting their their metabolism, but it's certainly affecting their lives.
Scott Benner 53:40
It's a very thoughtful way to consider it. I appreciate that. So I think I want to make sure I heard right from you that there's a system set up and you said Herculean, at one point, like to sit again, anything really changed is probably unrealistic. So what are we waiting for, for people with diabetes are we waiting for? I mean, eventually is like going to a doctor going to be online? Is it going to be are you going to go to a portal and tell it what's wrong? And it's going to give you like five ideas of what it might be and then put you on a call with a doctor and they'll chat through with you like, do you think it's all going to move in that direction?
Jon Oden, M.D. 54:14
I certainly hope not. I think there is a there is a proximity and physicality to to being a doctor. It's I've done telemedicine before, and I think it has its place, not a huge fan of the experience for my patients or for me, as a physician. I like to see people and kind of have a really good conversation before I make any decisions, or recommendations, I guess I should say. So I think in some in some futuristic view of medicine, there is going to have to be somewhat of a change. I think the pendulum changes though from time to time. So now we're more focused on primary care because there's not enough primary care out there and as our numbers dwindle, there is going to be a more focus on subspecialty He's like endocrinology, pediatric endocrinology, which is what what I do. But in the end, we are going to have to rely a lot on technology and AI, as you mentioned, and you know, all the all the things that we can bring to focus to make sure that our kids are safe and happy, live long lives in our healthy
Scott Benner 55:19
town. Are there? Are there fewer doctors or more people?
Jon Oden, M.D. 55:24
Yeah. Okay. I think I think both is very true. And I can tell you, there are fewer and fewer endocrinologist in my, in the past four or five years or so I know, five or six of my close colleagues that have either retired or quit, or passed away. And I can tell you, the people that mentored me when I was coming up in endocrinology, most of them if not all of them, have retired or passed away. But there were a couple of guys in San Francisco that I just idolized. And there was one in North Carolina that I idolized. And they are two of them are gone. And one of them has retired, and the other one
Scott Benner 56:05
retired, so it's are fewer people becoming doctors. You know, I
Jon Oden, M.D. 56:09
don't know that I can't answer that intelligently. I get a sense that we are struggling to fill seats in medical schools. But I can tell you with almost certainty that we are struggling to fill positions in fellowships. And that is going to affect the way that that diabetes and other sub specialties approach their patient, just
Scott Benner 56:33
applications, the medical school in 2020 to 23, numbered 55,001 88 11.6%, fewer than in 2021 2022. But 4% More than in 2020 to 2021. That can be COVID, though, right? A total of 22,007 12 students enrolled in medical school in 2022 23. Three, about the same as in 2020. Listen, my, my wife wanted to be a physician coming out of college and she had like financial trouble, which just didn't allow her to make a lot of applications. Oh, yeah, border fence is really expensive. She had good MCAT it's like great undergrad like she, she would have been a good doctor. And as she was lamenting that, in the first couple years where she was working in industry, a friend of ours who's a physician said, you know, listen, you're probably going to do better than I do. And you're not going to have to pay all these, like insurance problems. And like all this other stuff, he's like, don't worry about it. Like he actually was telling her like, don't be a doctor. That's doctors telling people don't be doctors. Because of the the headaches that come along with it. Oh, yeah. Yeah. So I mean, I see the slide, the bigger picture is, once you get somebody to be a doctor, they are who they are. And they may or may not be great communicators. I know everybody thinks smart. Right? But not every doctor is brilliant, like, you know, so you're looking for kind on a smart, you know, can be able to communicate, if you're lucky enough to get those things. What if you're then the impediment as the patient? What if you're not, you know, paying attention motivated, etc. There's a lot of a lot of different tripping points through the process.
Jon Oden, M.D. 58:14
To that point, every doctor has a bad day. Every doctor has multiple bad days such a good point. Yeah, you're on call the week before. It's Monday, you're you've got a full clinic and you're just tired. You know, sometimes you don't put your best foot forward. And, you know, with the way that we're measuring satisfaction and the way we're measuring productivity, it weighs on you all the reports that we get all the nudges that we get from people that are above us it, it does it weighs on you. It's a stress, and it does, as you mentioned before it contributes to burnout. Yeah,
Scott Benner 58:52
I use a boutique and Oh, for my daughter. And you know, look, we're lucky our insurance covers that after the fact really well. But I have the ability to text or email a doctor, and she still has trouble keeping up. And she has a limited, you know, practice. She doesn't take everybody actually I don't think she's taken new patients in the years. And still, it's hard. as much of a personal relationship as I feel like we have with her. I still recognize that every time we see or speak to her the first five minutes is you reminding her who you are and what your situation is, because there's no way for her to keep all that in her head like she'll, she'll be like, Oh, I remember all that kind of stuff. But I actually think that's a problem people. Like I see one doctor, the doctor sees hundreds of patients. But when I go to see them, I feel like I'm having such a personal interaction that I just expect that they remember everything that's been said between us. And that's not nearly the case either. In the end, a lot of these conversations, whether they're the cold wind, which is what I'm calling the anonymous conversations or these grand rounds or anything at the end, what I come down to is like this whole process it See human limitation issue on both sides? Yeah, yeah. And that's not a thing you're going to fix or change. No,
Jon Oden, M.D. 1:00:06
yeah. Not not completely and not in the short term now. Right.
Scott Benner 1:00:10
So the answer is what you hear people say all the time, you have to advocate for yourself and take your care into your own hands to some degree. Yeah, yeah, I agree. It's pretty, right. Yeah. Well, I guess we keep saying that out loud. Long enough. People will listen. But you know, I don't know. I can't reach everybody. John, I'm trying. Well, I think
Jon Oden, M.D. 1:00:29
you've done a good job. I think the the podcast my educators, some of my education, educators listen to it, and they really enjoy it, and they get something out of it. So that's, I appreciate that. No, I'm
Scott Benner 1:00:39
glad a printer and thank you for thanks. So I really that is my underlying goal. You know, day to day, I want to help people living with diabetes, but long term, I just want to impact enough people who will end up in medicine, that maybe they'll say, Hey, you got low, one o'clock? What'd you have for dinner? That's all. Yeah, that's yes, that's my hope. A little bit. I'm just looking for little, little, little advancements on that. I'll ask you one last question. I'll let you go. I know we're up on time. Why do we not talk about the impacts of fat, protein and general food quality with type ones?
Jon Oden, M.D. 1:01:13
Oh, good Lord, I have been, well, I'm not going to blow my own horn, because I certainly don't emphasize this in clinic and in any force at all. But I've always been an advocate for a healthy diet, you know, I grew up on the exchange diet, which was in some way, a healthier diet than kind of a meal ratio diet, which allows kids to eat whatever, whenever. But it's because of the kind of westernized diet that we have that kind of brings that down the ratio down because kids don't have access to really good healthy food. I think the other answer is that the metabolism of protein and fat, although defined in some scientific reports, is difficult in pediatrics, because of their their variability in metabolism. So it's hard to build out a structured education component to, you know, say, for example, a 14 year old football player versus an eight year old gymnast versus a 12 year old who likes to play video games. I mean, how do you build that kind of one size fits all education?
Scott Benner 1:02:18
I can tell you how I did it. Say if you see a rise 960 To 90 to 120 minutes after you've eaten, that's another impact that's coming from slower digestion, you should probably Bolus for it.
Jon Oden, M.D. 1:02:31
That's pretty. Yeah. That's one way I was thinking more along the lines of hey, if I'm gonna have a steak and potato, or pizza, or spaghetti and meat sauce, how do I dose for that? Yeah. And that's, that's challenging. You
Scott Benner 1:02:47
don't want to set somebody up with an extended Bolus, for example, if their activity will burn through that. Right, that right push, right.
Jon Oden, M.D. 1:02:55
And then again, to some families are set up to where they can they can process that information relatively simply. And then there are other families that, you know, Mom and Dad worked three jobs and you know, sisters helping out in the evening. And, you know, it's hard to kind of get them on board with that. That kind of math.
Scott Benner 1:03:13
Yeah. Yeah, I do see the bigger problem. I really do. I just Yeah. But once they ask the question, why don't they get the answer, then, like, once they show the propensity for like, Hey, I don't understand what's happening here. Like, you can't just tell them fat slows down digestion, and because of that your insulin might wane while there's still food being you know, carbs being leached into your system is blood sugar. Like, is that not difficult? No,
Jon Oden, M.D. 1:03:39
no, no, no, no, no, that's not when the question does arise, I think at least I mean, I approach it that way. But I'll tell you, the question doesn't arise very often. What I
Scott Benner 1:03:50
tell people all the time is that maybe the phrase I hear the most that I hate the most is, oh, that's just diabetes. works. Yeah. Which gives away the idea that there could be an impact here that we could understand and do something about.
Jon Oden, M.D. 1:04:03
Yeah, yeah. No, I think and then, yeah, it's one of those things. I think, if you had that hour long, two hour long education piece with a very few number of families, and you looked at their downloads, and you could see their, you know, the waves of their blood sugars and insulin boluses. You could probably say, Okay, on Friday at six o'clock, what G and they would say, Oh, we went to you know, Buster Steakhouse. And you would say Oh, so this is probably fat and protein, we need to do it this way. This is how we would do it. But that doesn't happen in real life.
Scott Benner 1:04:36
So do you have a minute for another question? Sure. No, great. So for people who are never going to get it? Do we just want them to be on like an eyelet pump for example? Oh,
Jon Oden, M.D. 1:04:46
wow, good question. I think there was space for an eyelid pump and it's curtain current programming for such statement. Yeah,
Scott Benner 1:04:55
yeah. Just say look, you got an eight a one say there's nothing and by the way, eights being I'm being polite, right? Like the people who don't get it don't get it to the tune of like 910 11. A one sees, right? Sure. Yeah, yeah. So you say to them, Look, you put this on small meal, it's breakfast, you're gonna get a seven a one C, is that a win? And you because they were never gonna get it anyway, that makes you
Jon Oden, M.D. 1:05:16
look at it from the lens of an agency as being your target metric, then yes, check. And the DCCT did show that I was in a conference a couple of years back where one of my colleagues said something that has just stuck with me. And she was commenting on how some algorithms, you know, shut down insulin delivery for X number of hours. Yeah. And she said, Well, we don't know what happens to your body when it doesn't have any insulin at all. And it alluding to the fact that it could kind of be producing in some small way, you know, metabolites that aren't healthy for you. Interesting. And so I think before we answer that question as to whether or not that pump would be, quote, unquote, good in the long run, we need to know exactly what it's doing to their metabolism. And I think that's going to be, that's not going to come out in the near future that's going to come out over the course of the next five to 10 years. It's
Scott Benner 1:06:16
interesting. I've watched a lot of different algorithms work a lot of different ways. My daughter at the moment is wearing Iaps, which is a DIY algorithm. It kind of manages backwards, like it front loads with insulin, and then takes away basil until it needs to come back again. But you're not really without insulin, because you have a pretty large Bolus going. Right? Do you know what I mean? Yeah. Is that person talking about like, when Basal gets cut away for a very long time? To try to try to save a low? And
Jon Oden, M.D. 1:06:46
yeah, and what is a very long time? Is it five minutes? Is it 30 minutes? Is it an hour? Is it two hours? We have we have? It varies, yeah,
Scott Benner 1:06:53
in this situation is going to keep it because if you're everything settings, like in algorithms, like your, it's all about your settings. So it's your settings, and you timing your meal, boluses. That's pretty much where you're gonna get success from. But it's an interesting idea. I just think that if someone's going to have that unhealthy of a lifestyle to begin with, and time has proven that, that for whatever reason, they aren't changing that, if you can at least put this thing on them that would keep them in as at a seven. I mean, that's got to be a net positive. Like, I get that I get that you can't say that, for sure would be but it feels like it would be,
Jon Oden, M.D. 1:07:28
it feels like it would be to me as well. Yeah, I don't disagree with you. And I think in some ways, you have to say that it's a win, because, you know, their agencies are better and their blood sugars are better. And their, you know, their triglycerides are probably better. So, metabolism has probably moved to a space that it's it's better, but it's better good enough,
Scott Benner 1:07:45
right? Oh, no. Yeah, and I don't think it is. But I guess my question is, what if that's a person who was you just weren't going to reach? Do you know what I mean? Like, it almost feels like, I can't believe I'm saying this feels like a clean needle program for diabetes. Like, I'm not gonna get you to stop using heroin, but I can at least give you a clean needle. Yeah, yeah. No, I mean,
Jon Oden, M.D. 1:08:04
I mean, that's, that's an interesting analogy. But um, I think for now, we can say that it would be a good, a good pump, a good platform to recommend. We can have some baseline assumptions on what it's going to do with some, with some kind of joy in our heart that it's going to do better. But again, do we know that it's the best step forward?
Scott Benner 1:08:28
Okay. My last question about algorithms are after seeing people who are paying attention, learned to understand their diabetes go to an algorithm, did they get dumb about diabetes? So they forget things? Or does that not happen?
Jon Oden, M.D. 1:08:41
I don't think so. Yeah, I
Scott Benner 1:08:43
don't think so either. But that was a concern at the beginning that people had, like, if we put we keep slapping these algorithms on people, they won't know how to take care of their diabetes, but I don't think that's the case.
Jon Oden, M.D. 1:08:52
I don't think so. I honestly I have noted the opposite. In fact, you know, many of these families, and they come from all different backgrounds, I don't want to say that, you know, there is a certain socio economic norm to those groups, but there are people out there who absorb this stuff. And when they get on an algorithm, they understand a little bit better. And they they apply it a little bit better, and they understand it and they're able to do things independently, and they come to see me and they're like, Oh, hey, Dr. Owen. We're doing great. We just changed his you know, his sensitivity other day, and he's doing great, we don't really need you, thank you very much. And then they're out the door.
Scott Benner 1:09:28
I learned more about watching the loop work through like Nightscout I was already but when my daughter started looping a number of years ago now I was really good at diabetes like I had array one C and the fives It was no trouble. I was basically an algorithm already we were you know, Temp Basal Ling taking insole away giving extra that kind of stuff. But watching it do it automate idli I think upped my game. And so I agree with you. I know I keep saying one last thing, but I want to share something with you and get your, your top line reaction from it. So my daughter is 19 and uses Basal 1.1 and our her insulin sensitivity one to 42. Her carb ratios like one to four and a half like pretty, pretty strong stuff, right? But she also has what we thought maybe like some PCOS symptoms, okay, so her physician put her on the lowest dose of ozempic. That's allowable point, like point two, five is as low as you can inject, right? She has not moved up. And she's been doing this for two and a half months now. She lost 10 pounds that honestly, I didn't think she had to lose. But after she lost it, you go okay, that's, that's fair. But that's not the point about the weight part. Her Basal went from 1.1 an hour to point seven, and our insulin sensitivity went from one to 42 to one to 63. And her insulin to carb, I think now is like one to seven and a half or eight. And I'm calculating that show us more than 12,000 fewer units of insulin next year. Yeah, that's great. Yeah, that's great. I have an interview coming out real soon with a third of the mother of like a 13 year old girl has had type one diabetes for over three years, I think was using 70 units of insulin a day on average. And she's down to between four and seven units of injected Basal. She took her pump off and doesn't have to Bolus for food anymore. And she's using weak Ovie for weight loss.
Jon Oden, M.D. 1:11:36
Yeah.
Scott Benner 1:11:38
Are you seeing that? Well,
Jon Oden, M.D. 1:11:41
no, because we can't get those medications approved. Yeah,
Scott Benner 1:11:44
they're cash based off for sure. Yeah, well, not for the but not for this one little girl because she got it approved for weight loss. And then she just happened to have type one and got all these other benefits from it.
Jon Oden, M.D. 1:11:55
every state and every insurance company is different is what we're finding, and we fight the good fight for a little bit. And we've just been kind of pushed back for the majority were advocating for the GOP ones to be covered. But we haven't quite made that a success story. Yeah,
Scott Benner 1:12:14
I think we get there in the next couple of years on that. And that would be great. But I mean, how fascinating is that? That my daughter's needs change, by the way that they would call point two, five of ozempic a non therapeutic dose? Oh, yeah, yeah. It's insane what it did for?
Jon Oden, M.D. 1:12:32
Well, I've had, like I said, I was a runner, and you know, you go on kicks, if not running for very long, and my insulin sensitivity goes down, and my requirements go up. And then I start running again. And, you know, I dropped, you know, 1015 pounds and, you know, comes right back. And it speaks volumes for healthy appetite. I mean, healthy meals, and good exercise every day, which is what we try to instill in all of our kids,
Scott Benner 1:13:00
for sure. And I agree with that. But I need to tell you that the my daughter's insulin adjustments came before the weight loss. Like literally within the first four days, we had to start taking her insulin away, she was getting low. Right, right away. It was insane. Yeah, I keep wondering out loud, if we're gonna learn that people have some sort of a GLP deficiency at some point in the future. Because I will tell you that I, I, the only reason I knew about it to talk to the doctor about my daughter is that I used week OB for weight loss. And in a year, less than a year, I've lost 45 pounds, but I haven't really changed anything about my lifestyle. So it's, I lost four pounds in the first five days after shooting it with just the Iso I don't know, like I can't, I'm trying to stay alive long enough to hear the how this ends, John, because I'm very interested.
Jon Oden, M.D. 1:13:52
But these medications are, are going to be critical in the management of type two. And, you know, there may be there may be a space in there. For certain patients with type one, it's
Scott Benner 1:14:04
very, it's possible. It's not going to be for everybody. I know that like, I also see I don't know if you're hearing from people or not, but the Manjaro know, or the step down. Like that seems to have fewer kind of impacts on people's bowel habits, I guess and stuff like that, like, kind of like indigestion stuff, but but it's just very, it's very interest. It's all in its infancy. And it's incredibly interesting. I'm excited for people to start talking about it like oh, that's what famous people do to be thin. I'm like, there's a lot of application here. So now I can go. Alright, man, I can't thank you enough for doing this. Was this what you expected?
Jon Oden, M.D. 1:14:38
I hope? Yeah, yeah, this was this was a lot of fun. Thank you very much for accepting my request. Oh, are you kidding?
Scott Benner 1:14:45
So some pretty cool people said you were good. So I was like, Alright, oh, good, Lord. So I was like, Alright, I definitely would love to do this. Thank you. Hold on one second for me. Oh. A huge thank you to one of today's sponsors, G voc glucagon. Find out more about Chivo Capo pen at G Vogue glucagon.com forward slash juicebox. you spell that GVOKEGL You see a ag o n.com. Forward slash juice box. Having an easy to use and accurate blood glucose meter is just one click away. Contour next one.com/juice box. That's right Today's episode is sponsored by the contour next gen blood glucose meter. I want to thank the ever since CGM for sponsoring this episode of The Juicebox Podcast and invite you to go to ever since cgm.com/juicebox, to learn more about this terrific device, you can head over now and just absorb everything that the website has to offer. And that way you'll know if ever sense feels right for you. Ever since cgm.com/juice box if you were a loved one was just diagnosed with type one diabetes, and you're looking for some fresh perspective. The bowl beginning series from the Juicebox Podcast is a terrific place to start. That series is with myself and Jenny Smith. Jenny is a CDC es a registered dietitian and a type one for over 35 years. And in the bowl beginning series Jenny and I are going to answer the questions that most people have after a type one diabetes diagnosis. The series begins at episode 698. In your podcast player, where you can go to juicebox podcast.com and click on bold beginnings in the menu. If you're looking for community around type one diabetes, check out the Juicebox Podcast private Facebook group Juicebox Podcast type one diabetes, but everybody is welcome type one type two gestational loved ones. It doesn't matter to me. If you're impacted by diabetes, and you're looking for support, comfort or community check out Juicebox Podcast type one diabetes on Facebook. Thank you so much for listening. I'll be back soon with another episode of The Juicebox Podcast. The episode you just heard was professionally edited by wrong way recording. Wrong way recording.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!