#386 Podfather
The Pod Father
John Brooks is the father of a type 1 diabetic and the guy who developed the Omnipod.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:08
Hello friends and welcome to Episode 386 of the Juicebox Podcast. Today, I bring to you a conversation with john Brooks, one of the men who sitting on an airplane over 20 years ago, conceived of and dreamt about, for the very first time, a tubeless insulin pump. Eventually that pump became the Omni pot. And this is the story of how it came to be. John's the father of someone who has type one diabetes, and
Unknown Speaker 0:39
he tried to figure out how to help
Scott Benner 0:40
a long time ago when his son was diagnosed. This is what came of it. It's kind of crazy, right? While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making any changes to your health care plan, or becoming bold with insulin. John's actually been involved in a lot of things around type one diabetes, we'll talk about all of it. But my initial reason for having him on was to learn about the birth of the Omni pod. An interesting idea, isn't it? Just something didn't exist? And then it did.
Hey, if you're looking for a great way to support people living with Type One Diabetes, while you support the podcast, go to T one d exchange.org. forward slash juicebox. And join their registry, you'll answer a few simple questions about you or your child who has type one diabetes. And those answers will help support innovation in the type one world. It's that simple. It's completely HIPAA compliant, absolutely anonymous, you can opt out at any time. And it takes less than 10 minutes to complete right there from your phone, or your computer. T one d exchange.org. forward slash juice box. This episode is also sponsored by touched by type one. Good a touched by type one.org. To learn about an organization that is doing an incredible amount of good for people living with Type One Diabetes. Touch by type one is also putting out there good stuff on Facebook and Instagram. As a matter of fact, I believe the founder of touched by type line just had a beautiful little baby. So if you're interested in seeing cute little babies definitely hit up their social media touch by type one.org. Do you have a great doctor or need one? Check out juice box docs.com. It's a great list of doctors who have been suggested by the listeners of this podcast. The doctors that get it when you want to make adjustments to your insulin, but don't want to just do you know what everybody else does. juicebox docs.com leave a name. Take a name. If you're looking for those diabetes pro tip episodes to share with a friend. It's easy to get them to download an app I guess and say hey, started Episode 210 that's where those diabetes protests begin. Or you can just send them to diabetes pro tip.com. And please help me welcome a brand new sponsor to the weekly shows. g vote glucagon. In the next few episodes, you'll begin hearing about yoke. Arden has already got it at home. We've got the hypo pen, and it's the bomb diggity. The absolute minute I heard there was a new glucagon that did not have to be mixed. I wanted to know more. You can learn more at GE Vogue glucagon.com forward slash juicebox ge vocus GVOK eat glucagon classic way gl ewca. And that might have been wrong. glucagon. Dear God, are we gonna get involved in spelling glucagon right now? All right. GVOKEGL Uc, ag o n.com. forward slash juicebox. Or you could just you know, use your own brain instead of mine and just type it out. g vote glucagon.com forward slash juicebox. Welcome to the show, g Vogue. T one t exchange.org. forward slash juicebox. And of course, touched by type one.org. Check them out when you have the time. I appreciate you doing this very much. I've often wondered about you, not knowing who you are. And I thought this is an interesting time to get your, your thoughts. I mean, if I'm not wrong, right, it's not 20 years since you started the company, right?
John Brooks 4:55
Yeah, it started instantly. In fact, it's funny I was just on the phone like 10 minutes ago with, you know, my co founder and partner at prism, Dwayne Mason's. So we were just literally talking about that 20 years ago, 20 years ago in May 2000.
Unknown Speaker 5:11
Yeah. And now
Scott Benner 5:12
everything is getting ready to. I mean, I don't know how to think of it, they're gonna take the thing you guys made and supercharge it, right. Like, it's, it's getting ready to take a leap, don't you think?
John Brooks 5:22
Yeah, well, you know, I think, you know, if you think of the world that, you know, we started in, it was a device, right, a glucometer. You know, that? Well, a glucometer, you know, was then gonna drive an insulin pump. And now you look at it, you know, it's the whole closed loop, it's the automated insulin delivery capability. But I think what's most important is the fact that it's less about the device, it's really the data, and it's the use of that data to drive better decisions, better clinical outcomes. And I think, you know, with COVID, and the way healthcare has changed, you know, people want to be able to kind of get health care in their terms, you know, they don't want to feel like they have a job to manage your diabetes, but you know, the more of the burden we can take off of them, they want in today's environment, you know, people are more prone, they don't want to go to the doctor's office, they don't want to go to the clinic, they don't want to go to the hospital, you know, that they want to be able to, you know, get help and coaching and support for managing their diabetes, but on their terms, and, you know, I think that's the beauty, whether it's insulin or others, I mean, you know, really leveraging the data, the analytics, the ability to basically determine, you know, trends to be able to look at time and range to be able to look at, you know, where there are any hiccups, or, you know, risks of hypoglycemia. So, you know, it's kind of the evolution of healthcare that, you know, if there was a silver lining to COVID, its accelerated, you know, all this virtual care, remote care, connected care, you know, much faster than, you know, it would have happened on its own, it was pretty, pretty slow. And now it's, you know, changing dramatically.
Scott Benner 7:08
So in the beginning, really, the, it's about, it's a tool, and the tool is the whole, it's the whole story. And now really, the tool is just the way you take the data and and make the decision. And then you don't have to go back to the doctor who would look at whatever data you had, whether they were finger sticks, or log books or CGM graphs, as time goes on, and say, Look, I think you should turn this knob here make this small adjustment. Now the data kind of understands that for you, I guess.
John Brooks 7:34
It's Yeah, I mean, you know, it's pretty much I don't want to say autopilot, because we're not quite there yet. But the idea is that, you know, the algorithms, you know, the systems get to know you, they get to understand, you know, kind of what, you know, what you do, a lot of people tend to do similar things day after day, whether it's their eating or whatever. So at the end of the day, you know, the devices are going to become smarter and smarter and more predictive. And they'll try to determine not only what the right insulin dosing is, but, you know, based on your prior history, you know, based on what they've been able to track, you know, they can almost anticipate, here's what's going to happen, and, you know, kind of get ahead of the curve. So, you know, I think it's the power of AI, it's the power of analytics. And then to your point, you know, you know, in the early days, I remember at jocelynn, you know, you'd have doctors having to look at, you know, printouts from all the different flavors of bgms, there was, you know, a few folks on CGM, you know, you had some ability to download data off of a pump, but none of it was connected, none of was integrated, none of it was aligned, you know, there was no even understanding of the dates on all the devices were the same. And obviously, everything got shifted every twice a year when there was daylight savings time. So, again, I think we've come a long ways and, you know, more to go because, you know, the sad part is, despite a lot of great technology advances, you know, we still do not have enough people with diabetes, especially people on insulin, you know, meeting their objectives, you know, getting their time and range. I mean, you know, and again, I think it's an appreciation that, you know, despite the fact we're making advances, you know, there's more to you know, managing diabetes and just tracking blood sugars, you know, standing now more about stress, understanding more about sleep habits, understanding more about, you know, the food, we eat, nutrition, and even the whole behavioral mental health aspects of diabetes. So, so the good news is, you know, I think we're getting smarter. I think we're getting there. But you know, like anything else, it just doesn't happen overnight. Yeah.
Scott Benner 9:50
Well, let's kind of walk down memory lane for a second. So tell me a little bit how you How did you come to this and like you were saying before, like, I guess that kind of Concept wasn't as much about the pot at first as it was about, just take me to the beginning, like, what were you doing when this happened? Yeah.
John Brooks 10:06
So, um, if I kind of walk back 28 years ago, or then three year old son was diagnosed with Type One Diabetes, okay. And certainly, you know, no real, immediate family history, you know, I didn't quite understand how that came about. And we were living in Colorado at the time, I was working for Pfizer, on their device business. And, you know, I decided that, you know, I need to try to understand, you know, diabetes, both type one and then eventually type two. So, you know, as my career and life advanced, you know, diabetes was always an important component. And, you know, when I, you know, when Pfizer ultimately divested themselves from all the device businesses, they were in, I came back to Boston, I was a co founder of a venture capital firm, called prism, venture partners. And, you know, that's really what I said, in the early days, you know, you know, we were looking at, I was looking at, you know, companies that we're trying to work on, you know, non invasive glucometers, you know, people are trying to work on, you know, how to determine glucose, you know, in a very effective way. And, you know, and then, you know, as I said, you know, a little more than 20 years ago, you know, my partner and I were on a flight coming back from the west coast, and I was describing, you know, the challenges with, you know, trying to figure out insulin insulin delivery, and, you know, the problem with the existing, you know, pumps as they were back then, you know, with the tubing and the priming and the all the issues, and, you know, we kind of brainstorm that entire five hour flight, you know, and thought about, you know, how do we come up with a, you know, small, disposable insulin delivery system and the disposability happened to come out of a nother deal that we had done leveraging technology out of Sarnoff Corporation, which is where the RCA color TV was invented, if you will, and they had an interesting technology for a disposable hearing aid. And, you know, that's another whole story, I won't get down there. But, you know, we had the idea that disposability could be a very disruptive innovation, the idea is that every three days, someone puts on a new pod, you know, we knew we could, you know, hopefully do that in a very cost effective way, eliminate all the problems with the two meeting and the priming. And so you know, that that's kind of where the idea came from. And, you know, we got off the plane, the next day, we called up our patent attorney and said, Hey, we have this idea for a disposable insulin delivery system. And he said, Hey, no one's ever thought of that. And, you know, we got a whole bunch of IP, and then we went to our, you know, fellow partners in prison and said, Hey, we want some seed money, to kind of flesh out this idea of get it off the ground. And, you know, we did that. And, you know, we hired some people that had worked for us beforehand, we set up shop up in Beverly, Massachusetts, had a couple people and pretty much told them, you know, in the early days, just think about all the ways you can do this, think about all the ways to create an IP position, you know, and then little by little, we, you know, had more ideas, we had more IP, we had more prototypes. And then, you know, we went ahead and started to, you know, put together a management team, you know, build on the engineering team, and, you know, little by little, we brought other investors in, and, you know, here it is what, you know, 20 years later, you know, very successful in a multi billion dollar market cap company that, you know, continues to drive innovation, but that, that was kind of the germination of it. And then, you know, as I said, you know, and most of my career since then, you know, continues to be very heavily involved in diabetes. I had the opportunity, I guess, was probably about eight almost nine years ago to run the Joslin Diabetes Center as CEO. So, you know, somewhat unusual to have a fellow that I'm a UMass Amherst, graduate, undergraduate, and accounting, finance and systems. So, you know, you can see I learned enough over the years to be dangerous to be able to run a leading academic and medical research Education Center. But again, you know, it was part of, as I said, 28 years ago, I was bound and determined to try to understand, you know, how did my son get diabetes? And, you know, is there an opportunity to think about a cure and then, you know, as I get further involved, you know, came to appreciate that, you know, certainly type one is a challenge, but, you know, the whole epidemic, you know, I used to call it a pandemic of type two diabetes. with, you know, close to 400 and 60 million people around the world. So, anyhow, I could go on and on. But no,
Unknown Speaker 15:05
it's amazing how it came about.
Scott Benner 15:07
I'm wondering how, how long after you, you you take that plane ride? Are you holding a prototype?
John Brooks 15:14
It's a good question. Um, it was probably, yeah, I want to say probably nine months to a year, I mean, because, again, we spent a lot of time I mean, you know, we probably had some drawings and ideas, but, you know, we wanted to really think about the intellectual property to make sure we had a good patent position, you know, we wanted to make sure that, you know, we had a clear understanding that whatever we did, you know, we needed to have a, you know, kind of a novel way to engineer it, because, you know, most pumps have a motor. And, you know, you're thinking, if we have a disposable device, that, you know, we said, Hey, this thing's gonna have to, you know, cost less than, you know, I think it was, I don't know, maybe 15 $20. You know, and we said, well, you know, if you put a pump in there, you know, that's not going to do it. And then, you know, we thought about how to, you know, basically deliver very precise amounts of insulin. And in fact, kind of interesting enough, you know, we went back to sawn off and said, Hey, here's our problem. And they actually come up with the idea of a heated wire, which basically, is the mechanism that enables when you heat the wire it, you know, stretches and shrinks, and that ended up being kind of the mechanism to deliver the insulin very precisely, and in a very cost effective manner. So lots of, you know, as I said, I'm sure we have prototypes and ideas along the way, but, you know, it was more important to make sure that not only did we have a great design, did we have a design that was really gonna, you know, work, especially for kids and others. You know, we used to call it hassle free. So we didn't want priming, we didn't want to being, you know, we wanted to have a very easy way for the canula to get placed. So you know, it was iteration and it took, you know, it took a while, and then you got to figure out, you know, how to really make sure it works, you figure out what the regulatory requirements are? How do you make sure how we get the insulin in? How do we make sure that, you know, we can communicate, so, you know, lots of lots of steps along the way. So it doesn't happen overnight, and I took a really long process it were
Scott Benner 17:27
there points along the way, where you thought, we'll just get this to a certain point and sell it to somebody else. Did you ever think you were gonna be the company that made the pumps and sold them?
John Brooks 17:37
Well, I, you know, I think we did, you know, you know, we thought, Hey, this is a very, you know, novel idea. And, you know, we felt good about, you know, as we did some early interaction with, you know, customers and focus groups. And we had, I think, from the very beginning, you know, thought about the fact that this was the type of product that would lend itself to high speed automation. I mean, we actually thought, you know, at the time, we had set shop in trying to think where we were Bedford, I think, at the time, and after we left Beverly, where we started, and, you know, we had the idea, hey, we're gonna have a light sound factory, all these pumps are going to put to be put together by robots. Right, you know, and, you know, and then, you know, in some ways you go full circle, I mean, a lot of what takes place today, both in this great new factory that insulin built up in Acton, you know, a lot of automation, you know, lots of ways to produce, you know, massive numbers of pumps that are high quality. But you know, the answer your question, you know, I think we always stopped that, look, you got to build a great company, and maybe along the way, is someone likely to look at it. I mean, you know, what a Medtronic would somebody else say, Hey, this is interesting, but, you know, at the end of the day, I think we said, let's, let's do this, and I remember, you know, some of the greatest moments, you know, when I was a jostling member, we had a lot of Jocelyn had the Joslin camp for boys out in Oxford baths, and it was right next to the camp for for girls, but you know, seeing all the kids, you know, with their pods on swimming in the pond, I mean, that was pretty neat. Because before that is you know, you know, you're gonna disconnect your pump, you're gonna take it off, you know, you can't get it in water if you're using a traditional, you know, to pump and all so, you know, so I think we were always motivated by the fact that hey, this is a better way to help not just kids but families and people that want to get insulin and you know that they want to do it in a way that you know, it's discreet, it works for them. And they don't have to worry about all the hassle that you know, some of the other two pumps, you know, have gotten better but still exists.
Scott Benner 19:57
You know, my daughter has been wearing it on the pod every for 13 years, so, I'm completely aware of the just the benefits of just having your basal insulin while you're in that pond, you know, so amazing as before,
John Brooks 20:10
you know, kids would take the pumps off, and you know, it's a hot summer day, and maybe they even put them under the towel. But you know, the pumps are getting warm, and you know, maybe they're not wearing them for a certain amount of time. I mean, at the end of the day, that's just not good therapy. Right. Right
Scott Benner 20:25
now, it's 100%, I actually, I, I've been through the new manufacturing facility, I've taken that it's amazing, right? It's unbelievable, just astonishing what they accomplished. And, and watching it happen. And like you said, like, you know, things are kind of moving around automatically. And it's, it's not, and I don't think the precision is, is considered like, I want to try to understand without getting too like geeky and technical, you're telling me that inside of that pod, there's not a pump sending the insulin through the kanuma? It's,
John Brooks 20:57
yeah, so it's basically a mechanism that emulates a pump, but it's not a traditional pump with a motor and all. So, you know, so it's a different approach. And, you know, and I'd say, that's really the other, you know, key thing about, you know, being able to produce the number of pods that are needed, you know, where, you know, replacing them every three days. And so, you know, I think the other important thing was to, you know, put a lot of focus on dimensions, tolerances, the tooling, I mean, you know, that this is a product that, you know, that the tolerances are critical, the, making sure you're working with the right vendors, the vendors deliver the right product, and, you know, because we did have, you know, in the early days, you know, there was always a little bit of a concern about, you know, could we, you know, batch the batch consistency, you know, in the early days, we used to joke, we were shipping dollar bills with every pump, you know, because we didn't have the volume, we didn't have the scale, we didn't have the full economic benefits. So, but, you know, that's part of the learning curve. And then when we, you know, that they went to a generation to, you know, which was smaller, more precise, and more, you know, kind of cost effective, you know, that there were some hiccups in the early days, when, you know, you know, things don't quite go the way you expect, then, you know, you just kind of work through them, and hopefully, you know, convince your loyal users that, you know, Hey, sorry, and, yeah, we'll send you some replacements Hang in there. But, you know, the good thing is, I think that's all behind the company now. And I think now they're focused on, you know, kind of what I'd say is there, you know, Gen five product, they've got dash, they've got horizon. I mean, there really, as I said at the beginning, you know, recognizing that it's no longer just about delivering insulin, but it's the context of you know, doing it in a way that understands how that individual was living there live understanding, you know, kind of what their you know, smart CGM and other devices are saying and, you know, optimizing, you know, what their requirements are, so they're staying in range, they're avoiding hypose and hyper Roisin in their care team can continue to kind of fine tune, you know what they're doing. Did you
Scott Benner 23:23
are you still involved or did you eventually sell your share? Or how did how does that
John Brooks 23:27
Yeah, so when I went to the Joslin, you know, I just made a conscious decision. I think it was certainly the right one. You know, maybe not economically, but I i divested all my shares I you know, I just because we were doing some things and, you know, if you're the CEO of a not for profit with the prestige of Jocelyn, I just didn't want to have any perceived conflicts and also, right. So, you know, I'm happy to say today, I'm still an owner, but, you know, I pretty much you know, divested everything for the five years that I was running Joslin, I say, okay,
Scott Benner 24:03
Oh, alright, that's what we wanted the president to do, that he didn't do is that we were saying that that whole, like, you just sort of take yourself not to be political, but you.
John Brooks 24:11
Look, it's the right thing to do. I mean, you know, if we were doing some work, maybe some of the doctors at Joslin, which they were were doing different, you know, studies or, you know, clinical trials. Yeah, you could argue, well, I don't have anything to do with that. But it's appearances and it's really good governance. And frankly, you know, I think it's just having a good moral ethical compass. So, you know, was I going to influence results? No, but you never want to have even the suggestion of impropriety. And I just said, Look, this is the right thing to do. Right? That's excellent.
Scott Benner 24:45
Oh, that's very cool. So you're still you're still involved that and you're so you're an owner at this point still?
John Brooks 24:50
Well, I'm a shareholder share with you know, a small one. Other people yeah, there's
Scott Benner 24:55
you're saying somebody else is listening. This right now going? I have way more than john does.
Unknown Speaker 24:59
Yeah.
John Brooks 25:01
I'm sure every major, you know, you know, public equity fund out there, you know, mutual funds, but now I'm happy to, you know, be involved that in, you know, full disclosure, I have a stock holdings and other you know, diabetes companies because, you know, you know whether it's on the CGM side or it, you know, looking at pumps in and I work with, you know, a lot of young companies that are working on, you know, what I call the next generation solutions, whether it's new new insulins, whether it's a new type of CGM, there's some companies working on, you know, new pumps, the company's working on defeating the auto immune system, companies working on you know, better real time insulin type tration, and people with type two, so, about 80% of what I do, you know, these days is still, you know, helping, especially young companies, and I'm either doing it as the chairman of the board, board member, advisor, consultant, you know, trying to make sure that, you know, what I've learned over the years, and, you know, how can I help them turn themselves into a successful company that is going to further help people, you know, with type one or type two to, you know, live better, healthier, safer lives? That's cool.
Unknown Speaker 26:18
How old's your son now?
John Brooks 26:20
My son is going to actually turn 31. Next month, so just a few weeks away, he works for this company called livongo. I know Yeah, sure. heard of them. He was literally one of the very first people there. In fact, he was with the predecessor company called EOS health. So he's based out in Chicago has been with them, you know, I guess it's been eight years. And, you know, he manages their sales effort in the Midwest. So I guess he's had another, you know, I think, opportunity, he has type one. But, you know, he devotes a lot of his time to, you know, help lavon go get, you know, solutions for self insured employer employees who need help with diabetes, and now they're moving into hypertension, weight management behavior, et cetera, et cetera. And, you know, they went public, and now they're, you know, being acquired by teladoc. So, he's keeping busy, but he's pretty excited that he made a good career choice when he graduated from college, I have
Scott Benner 27:26
to ask you, I'm not sure where you're gonna go with this, but does he wear an army fine.
John Brooks 27:31
So he doesn't, you know, it's interesting,
Unknown Speaker 27:34
all this effort that you put into it.
John Brooks 27:37
But you know, at the end of the day, and I'm sure you might even know, with your daughter, you know, what, you know, it's their live, it's their decision. And, you know, and again, he, he's always been a fan. He's talked about it, but you know, just one of those things where, you know, I don't know why it just didn't fit his schedule, or didn't have the time. So at the end of the day, he may, but you know, today, he's not on it, but it's not a sign that he doesn't believe in, it's just, you
Scott Benner 28:07
know, no, I don't think that hey, listen, on the pod has been a sponsor of this podcast for since the beginning for many, many years. And I always tell people, the same thing, get a demo pod, try it for you, or it's not, it's you know, there are other insulin pumps, you could you could do MDI, you know, get an in pen, there's 1000 things you could do. Yeah,
John Brooks 28:28
the real, the real key is to, you know, use a use technology in a way that works for you. You know, and obviously, you know, whether it's a you know, CGM with a pump, and you know, the idea of this, I think people realize, you know, that, you know, all of a sudden, they're, their lives are better. They're, you know, they're in range. They don't have the glycaemic excursions and, you know, and it fits into their lifestyle. So I think that's really the key, we get up. You know, I do some work with the ADA. And, you know, we had a discussion recently with insolate. Just, you know, kind of getting to know each other up. Bob gubbay is the new chief medical officer, Chief Scientific Officer for the ADA, and he was on the call, I had hired him at Joslin, so he, he's a great person, but the whole idea is essentially just, you know, I think an appreciation that, you know, people that have been on MDI, you know, maybe just thought luck pumps are too complicated. They look like they're, you know, not going to work for me. And, you know, obviously, you know, I think once to your point, they try them. Also, they realize they're pretty straightforward. And, you know, and I think, you know, companies are sensitive to making sure that, you know, they're affordable and, you know, that they work for people. And again, I think the payers, you know, the insurance, I think, you know, understand that they're cost effective. I mean it wasn't too many years ago where, you know, you had to jump through hoops to justify Someone get a CGM or even a pump, you know, but, you know, the good news is the data is there and the values there and, you know, the world's, you know, continuing to evolve.
Scott Benner 30:10
What was the most difficult if there's one difficult part of getting the AMI pod to market? Was it the, the function of it and the mechanics of it? Or was it the FDA? Or is it insurance? Like, I guess?
John Brooks 30:26
It's a good question, you know, part of it, you know, I would say is just, you know, a disposable pump, you know, took a little while for people to get their heads around that I remember, we had some people saying, that's a stupidest idea I've ever heard of, I think the regulatory path, you know, we went through it, but I think, you know, I'm, you know, I spent years you know, kind of, uh, you know, working at Pfizer, you know, really a lot of device companies, you know, I do a lot of biotech and other things, but, you know, still know, the device base. But you know, my partner Duane knew that. So, you know, I think the key is, we weren't all that concerned about the regulatory, a big part of it was reimbursement. I mean, you know, you have to go kind of payer by payer across the country, you know, we kind of started in New England, and, you know, kept going west, to get payers to agree, you know, because it's a different approach. I mean, everybody else, you have this upfront investment for the pump, right. And then you have all the disposables. And in our case, you know, we were kind of turning that upside down, you know, it's really a subscription model effectively, and trying to get, you know, payers to understand that, how did it fit into their reimbursement, you know, even the federal government, you know, would say, you know, if you're on Medicare, you could only get, you know, one pump every four years, well, if you're getting a new pump every three days, and, you know, just things like that, I mean, sometimes the way the reimbursement was set up, but just, it didn't understand that, hey, this was a very different form factor, economic value proposition and, you know, you had to get people comfortable with and, and then they had to understand, you know, at the end of the day, you know, if you looked at it over four years, you know, versus the cost of a traditional pump, you know, they're pretty comparable, but, you know, when you're first starting off, you know, people there will, how does this work? And that's not the way we do it, and, you know, so that there was just a lot of, you know, pioneering and, you know, I think the other part of was just, you know, understanding the manufacturing, you know, despite the idea that we thought it would make sense to have this great lights out factory. You know, we realized that, you know, we needed a different solution, in fact, you know, ended up getting involved with Flextronics, you know, and, you know, leverage their expertise at high speed automation, and, you know, ended up setting up some, the supply chain, you know, generally in China, because, you know, we wanted to, you know, make sure our economics worked. And now, it's ironic, it's kind of coming full circle, back to the US, but so, you know, getting that manufacturing and getting the cost of goods sold was something that we always, you know, spend a lot of time on, because you don't, you know, you don't have a good business, if you're, you know, losing money on every shipment, but you've got to have the volumes, you have to have the, you know, sufficient economics to support, you know, getting the cost per unit down. And so that took some time.
Scott Benner 33:34
Who's gonna say, even understanding, hearing you talk about having to go state by state and explain to payers like, this is how it's going to work. And, yeah, I know, this isn't what you usually do. But this is this. I've had those conversations for my daughter, and back in the day, you'd have to get on the phone. Every time you reordered and say no, no, listen, listen, I know we just got a pump. That's not when then you'd have to re explain it to somebody was fascinating how many times I've done that.
John Brooks 34:00
Yeah, no, and you know, the if you think on the CGM side, I mean, you know, I remember in the early days, you know, payers reluctant to allow someone to have a CGM a reimburse them for it, you know, because if their numbers are in pretty good shape, you know, they say, well, you don't need a CGM. Or maybe you don't need a pump. And then the whole idea was, well, you almost had to have people deliberately, you know, mess up their diabetes management for 30 days to show that while you're not in good control, therefore you should get on I mean, if you think of the absurdity of that, yeah, but you know, that was part of it. And, you know, we used to have a lot of our great doctors that Jocelyn I mean, spending more time on the phone with insurers, you know, and even silly things like you know, why does someone with type one Why do you need to check your blood sugar's whether BGM you know, eight times a day what just do a two dads What are you doing? I mean, just absurdity.
Scott Benner 34:57
Ya know, the lack of understanding it permeate pretty much.
John Brooks 35:02
You know, type one versus type two. I mean, you know, a lot of people just still don't fully understand, you know that. Yeah, it's diabetes. But you know, it's a very different mechanism. It's not like if you have type one, avoid sugar, you're going to be great.
Scott Benner 35:16
It's I just was speaking with a person last night Whose child is more newly diagnosed. And this podcast, john, which you probably don't know anything about, I take great pride in it. It explains to people, among other things, how to use insulin, and my daughter is a one C with the dex comment on the pod is between five two and six, two for over six years. Now, she has a great diet restriction. She's doing terrific. I talked about what we do here, it seems to get to people in a way that they can understand it and replicate it for themselves. So I'm talking to this person, and she's like, I don't understand, why does my endocrinologist not understand? Like, why am I talking to you? And not her? And I said, I don't know. I don't I don't know what to tell you about that. But it just, it's what you it's what it made me think when you were talking through it, that most people would hear this and think, well, how could an insurance company not understand what diabetes is? or How could you know? And the answer is, because people don't, you know,
John Brooks 36:12
I mean, they, you know, and again, nothing against the people there. But, you know, anytime you bring something new or a different business model, different approach, you know, it doesn't kind of fit the traditional, you know, scheme, and you got to educate them, and you got to do the analysis, and, you know, uh, you know, they just tend to be a little bit change resistant, right?
Scott Benner 36:35
Yeah, you fall into something that you're comfortable with. And it works, whether you're a company or a person, and you stop being stop having reasons to wonder about other ways to do things. So exactly, you come along with this little pod, and you're like, Hey, listen, this is the way to go. And
John Brooks 36:49
that's like, what do you mean it after three days and throw it away? Like, why are you throwing it away? Right? That's designed that way. That's what it's for. Exactly.
Scott Benner 36:58
It really is. So if you if you can't say or you shouldn't, I'm not sure. But I've forever want to understand, while you know, you get your pot out, you fill it up it Prime's take off the needle cap, you put it on, and you say Go ahead, insert it, and then there's this clicking that is sometimes four times it clicks, sometimes it's five, sometimes it's six, and then, you know, blink of an eye, the candle is in, in my estimation, it's always been that something fires. A needle that's wrapped in a candle and the needle comes out leaves the candle behind, but is it not functionally firing? Is it tension? How does it do? Are you can you tell me how it does that?
John Brooks 37:40
Yeah, you know, I don't know what it does today, it's probably different than it was. But, uh, but I think your points accurate. And the whole idea was to get rid of needle phobia, to be able to have a very simple way to your point to deploy a Candela, you know, with a needle that would place it properly, and then, you know, disengage itself. So all you had was the candle lit to deliver the insulin. So yeah, I mean, I mean, I don't want to speculate, because I'm not sure how it works today. You know, the idea was to basically, you know, deliver it in a way that, you know, it would get into the skin at the right level, you know, and, you know, not caused any bruising or hypertrophy. I mean, there was a lot of work that went into the, you know, the needle design and the, in the shape and the insertion, pressure force, whatever you want to call it. So, but yeah, I'm probably, you know, it's been a while since I've looked inside one, it prompts me, I probably have an old one around here, I should look into
Scott Benner 38:38
I'm now wondering about the the day in the office where somebody was, like, I put it on me and push the button, and let's see what happens. That's how many how many people do you think in total? Were there in the beginning?
John Brooks 38:52
Well, in the very beginning, you know, there were two of us on an airplane. Right. But then, you know, we ended up as I said, we we had a team, we were up in the Cummings facility in Beverly mass, you know, after we have put our partners that put some seed money in, you know, we hired a guy that, you know, really brilliant in terms of, you know, just looking at the entire intellectual property landscape, you know, were there any other patents? Was anyone else doing anything? You know, and how would we, you know, think about creating the product? How would we think about, you know, what type of plastic what type of, you know, materials, you know, we thought a lot about, as I said, quote, unquote, the pumping mechanism, we thought a lot about the canula and the insertion mechanism, and, you know, what the battery life is and how to make sure that, you know, those accuracies, so in the early days, you know, was a bunch of really bright people, probably more engineering, you know, you know, folks had new devices, folks and new IP folks that understood we had to be able to make this thing very cost effectively and You know, you're kind of designing it and building it on the fly. And, and then, you know, we reached the point where, you know, I think we felt we had a good plan, we had a good business plan, we hired a fellow as our CFO who eventually became the CEO Dwayne to Cisco. And then, you know, we, as the company advanced, you know, we brought more money in, we brought in other venture partners, our our team continued to support it. And then, you know, we ended up getting, you know, new space, we left Beverly in, you know, we started to hire more, you know, a larger team, you know, in terms of, you know, recognizing that, you know, what do you need to have in, in, in addition, engineering, you know, you got to have people that are, you know, working on the supply chain, you got to have people that are working on, you know, understanding the whole regulatory process quality process, you know, starting to think about reimbursement starting to think about, you know, packaging. So, you know, you start building a team, and, you know, that took place over you know, a number of years, we go from kind of a, an idea that we had to you know, starting to think about, you know, what it should look like and again, just simple things, like, you know, what type of plastic and what type of plastic you're going to mold and what's the shape? And how much stuff can you fit into it and still have it work, but not be too big. And, you know, just lots of, you know, iterations that you know, you get a team and then you start getting people thinking about, how do you market it? What are we going to call it all that stuff, right? You know, in the early days, we used to call the op,
Scott Benner 41:42
it must be crazy to be a startup in a space that is, like, you know, pharma and device manufacturers, like bigger companies like Indy, you're sort of just these, your two guys coming off a plane and putting together things, by the way, the company still has a really good vibe, you know, throughout it, you can tell what the, as you're explaining what the roots of it are, it doesn't surprise me. Because I think it's grown in that direction.
John Brooks 42:07
And it's pretty neat. I mean, every now and then, in fact, at the last Ada meeting, not the virtual one, but, you know, My son was with me, and, you know, we were kind of walking the floor and, you know, went by the booths. And, you know, it's kind of one of those funny things where, you know, a couple of people start putting the dots together, wait a minute, you're the father, You're the son, I mean, yeah, you know, all sudden, they realized that, you know, we were kind of the, you know, that the, you know, My son was the inspiration and, you know, I was one of the co founders, every I kind of needed it, and again, you know, still having that, you know, you could call, you know, kind of that entrepreneurial spirit and, you know, really thinking, you know, what, I always like to think of disruptive innovation. And, and again, you know, I spent, especially back in those days, you know, most of my career was in the device world, I, you know, had ran a couple of businesses for Pfizer, and one of them was actually a company that had infusion pumps, and, you know, so, you know, we certainly knew a lot about, you know, delivering, you know, whether it's insulin or other drugs knew a lot about, you know, device manufacturing, regulatory, you know, so, anyhow, you leverage all that. And, you know, at the end of the day, you hire bright, smart, capable people who, frankly, thrive in a small company environment. I mean, you know, in a small company, I mean, you know, forget about your title, everybody's working hard. Everybody's working late, everyone has a passion for, you know, doing what we're doing, because we're going to improve the lives of people with diabetes really have honestly, hey,
Scott Benner 43:42
listen, is this to ham fisted? Or maybe this happens all the time. But do people call you the pod father? I mean, I've never heard anyone call me that. Well, then I'm doing it right now. Because that seems like an obvious pun. I mean, honestly, and, and, and what a, what a, what a, what an absolute parenting story, it is to like, you're like, let me do this thing for you. And you do it and you build this entire thing for it at the end, like, that's nice, but I'm not gonna use
John Brooks 44:12
it. And again, you know, he may very well you know, decide at some point he wants to do it. Yeah. And again, you know, he's a, he's doing great things in the world of, you know, helping employers and payers and all help their patients with diabetes. And now hypertension, weight management, as I said, it's really nice soon, you know, to be, you know, part of Tella Doc, which takes it even to a bigger stage.
Scott Benner 44:37
I'm having. I honestly, the experience that we've had with my daughter, doing telemedicine over the last number of months, I think has been an incredible improvement over what we had been doing prior to that, honestly, yes,
John Brooks 44:50
I agree. I mean, if you think of it, I mean, you know, and I did some piloting a Jocelyn. I mean, this is many years ago, and, you know, it was hard to get Add, you know, great clinicians, but you know, they were just used to, you know, meeting people in their, in their office, if you think of diabetes, I mean, it's the best, you know, way to treat people, because what do you do physically, you don't really need to do anything. There's no procedures, you're, you know, helping people and the diabetes nurse educators and the dietitians. And so but, you know, before we had to do it with COVID, you know, it's just people are convinced that you have to do it that way, right? Now. And in some ways, you know, it was just the, you know, people were resigned to the fact that I'm going to spend an hour to drive in the Boston, I got to spend 4050 bucks to park, I'm going to sit in the waiting room and wait, because this is a, you know, global leader and all the clinicians or bright and busy and, you know, that's the price you get to pay. And, you know, now if you said, hey, let's go back to that, you know, people there Nope, not gonna do it.
Scott Benner 45:57
I don't think that anything's been more gratifying in the last three months and sending an email to somebody and saying, hey, my daughter has hypothyroidism, too. And saying, Hey, I think Arden's a little hyper right now. And she fat and she emails back a script, we get a blood drawn, the next day, they move the tiersen down a level, and it's it's done in 24 hours almost. And before, like you said, get an appointment come in, take a day off from school, like all this other stuff to maybe get an answer in a month, if you're lucky. Really,
John Brooks 46:26
it's a it's a change. And again, I think it says we're saying I mean, I think diabetes lends itself to you know, having smart devices, analytics, AI and the ability to basically let the care team, you know, monitor from afar, how people are doing and make sure they get the right coaching, the right encouragement, you know, but but the idea is essentially, make the lives of people with diabetes easier, and take the burden off of them and, you know, give them an opportunity to basically live a, you know, healthy life and, you know, avoid, you know, the, you know, what, what used to happen, you know, was people developing complications, and, you know, not that they don't exist, but you know, I think we're doing a much better job of, you know, making sure we get ahead of the curve and not waiting for someone to have, you know, eye problems or kidney problems or vascular problems. I mean, the whole idea is, you know, a keep people in range and keep the excursions in, you know, don't let things get to the point where, you know, the the problems start arising.
Scott Benner 47:34
Yeah, you have to be proactive for certain I have two last questions for I thought I was only gonna have one, but now I have to because of your time at Jocelyn, how do you? Or do is it obvious to somebody like you that there's an issue with clinicians not understanding diabetes, as well as the people who have diabetes? And how do you speed up their understanding so that they can help newer people?
John Brooks 47:58
Yeah, no, it's it's a great question. And look, you know, whether it's Jocelyn or other place, Sherman just very talented individuals. But, you know, you know, especially a place like Joslin, you know, part of the Harvard complex, I mean, you know, academic medicine, you know, people are brilliant, but you know, there tends to be a lot of clinical inertia, you know, they want to see data, they want to see papers, they want to see peer reviewed journal articles before they fully get on board. And the other part of it is, you know, I think, you know, they're busy people. And, and, you know, as much as they're going to keep up with all the new developments, all the new information, you know, it just, it takes a little while and, you know, but but I think today, you know, with a lot of, you know, capabilities built into the electronic health records, you know, there's ways for, you know, clinicians to be able to, you know, get a better handle on how this individual is doing, what are the other potential comorbidities or factors that are going on? And then, you know, which is the right approach? And, you know, if you have type one, you know, what type of devices and, you know, do I still think about putting you on some sort of, you know, Sdlt, to inhibitor, I mean, so, but, but, but the issue is, I think it was just, you know, busy people and, you know, just trying to deal with all the stuff they had to deal with, and then after they get done seeing patients, make sure they put all of their information into the, you know, billing systems, so the bills could go out on time. And so, you know, I think it was just easy for people to kind of get into a, you know, I don't have time to think I just got to react. And so, you know, now I think it's easier with, you know, as we said, with kind of the whole virtual care, you know, I think it's just easier to be able to focus on for an individual, you know, what, what is it that we should talk about during this time we haven't, you know, that the doctors don't have to spend time kind of reviewing or trying to make sense on the fly out of CGM plots, and, you know, now that the information is there, it's more a question of helping, you know, determined for that person with diabetes, you know, what's the best way to, you know, help you even further improve? And, you know, to be there, you know, if people are still struggling, you know, because it's, you know, there's still challenges on the board of the college diabetes network Chairman there, and, you know, we spend a lot of time if you think of it, college students, you know, dealing with diabetes in this environment, you know, virtual hybrid classes, and, you know, the whole, you know, sided diabetes around depression, and, you know, behavioral health and also, you know, so in some ways, you know, life is getting easier, but life is getting more complicated, right, right
Scott Benner 50:48
now, it's interesting, I just have, I have such a personal experience over time, where it's gonna sound crazy, but I could sit down with you in an hour and explain diabetes to in a way where you would just understand it. And you'd, you'd be able to put it into practice, I've practiced for a decade or more writing about it and talking about it and, and just when you see someone struggling, who has great care, what really is considered great care. And then they come along, I mean, think about it, really Jimin, they come on and listen to our podcast, and then all of a sudden, they're like, Oh, I understand now. And then they're often there. Okay. It feels like there's a disconnect somewhere in between that, you know, what I mean?
John Brooks 51:26
Sometimes, you know, maybe, maybe the key is, you know, you know, you got to make sure you're connecting with people at their level, maybe some people I mean, you know, especially in type two, I mean, a lot of people are told by their, maybe it's your primary care doctor. And again, I'm not trying to malign anyone, but you have diabetes, and here's what you need to do. And I'm going to put you on Metformin. Well, you know, at the end of the day, I mean, I used to hear from many people, well, I don't really know what it means when I have diabetes. I mean, they don't understand things. And maybe they say, well, I'll avoid sugar. But you know, I can have pasta rice, that's healthy, right? I mean, no understanding, you know, kind of how our bodies work. I mean, when I was a kid, you know, many, many years ago, you know, we actually had something in school called nutrition class, and health classes, you actually had some idea how our bodies work, I don't think we're teaching that to kids anymore. So the idea is a lot of people just, even though if you're in it, it's kind of like, Well, why don't you understand it? Some people just don't fully understand like, Well, you know, what do you mean, my pancreas isn't gonna produce insulin or, you know, it's not producing enough insulin or, you know, I'm watching my blood sugar's but, you know, I'm in competitive sports, or I'm stressed out or, you know, when people start realizing there's all these other factors that affect your your glucose, I mean, you can eat the same meal every day, do the same thing. But if you're stressed out one day, or you didn't sleep well, or something, you know, you're going to have different results. A lot of people don't fully appreciate. Well, why is that?
Scott Benner 52:57
Yeah, I think that when, when I start talking to people, privately, which I do sometimes, just as I don't know, I think it makes me better at being on the podcast to have one on one conversations with people that aren't recorded sometimes. But when I start off by 10, I'm looking at to get your basal insulin, right, because nothing's gonna work. If that's not right. And then you really need to Pre-Bolus to understand how your insulin works. When I get to the third thing and say, You need to understand the glycemic load and the glycemic index foods, I don't think that's what they think they're going to hear next. And when you tell somebody that, you know, 10 carbs of one food in 10 carbs or another food are going to impact you differently. I completely agree with you, it fries their mind. They're like, no, they told me that not the
John Brooks 53:36
cause. And, you know, and again, we were learning a lot about, you know, again, you know, what else is affecting, you know, gastric emptying, you know, which foods tend to get into the bloodstream faster. I mean, again, there's a lot of complexity that, you know, not that we want to make it even more confusing for people. But the hope is that, you know, over time, you know, devices are going to start incorporating in, if you think of all the wearables, people are starting to pick up on heart rate variability, they're starting to pick up on sleep, and at some point in time, maybe those additional inputs, you know, might further cause the algorithms to be even smarter. Yeah. So all of a sudden, you know, we're having a better way to help people with diabetes, you know, understand that, yep. Blood Sugar is fine. But that's not the only ingredient that's kind of driving, you know, what's going on.
Scott Benner 54:26
Yeah, maybe one day the, the pump will know that, hey, I had pizza. So the cheese is slowing down the digestion. But now the cheese is gone. And everything's going through me quicker and not impacting me the same.
John Brooks 54:37
Yeah. And again, a lot of pumps are going to say, you know, hey, I remember the last time you had insulin and here's, here's what happened. And you know, instead of you having to figure out a square wave bolus, whatever, you know, the system is going to basically say, Yeah, I remember that. You know, let me make sure that I'm adjusting your insulin or if you're an athlete, I remember you know, when my son Played high school sports or you know, we've had a lot of kids that Jocelyn, you know, playing competitive sports and you know, the the issue is, you know, your blood sugar's you know, you may be fine during the game and then eight hours after game time you're crashing and you know, understand why why do that's, you know how do you get muscles reload? So anyhow, it's complicated but we're chipping away at, you know, getting it there and maybe in the background we've got people working on, you know, either, you know, beta cell regeneration protecting the immune system, I mean, you know, there's lots of other good things going on that I'm on top of as well. So maybe someday, we'll make all this moot.
Scott Benner 55:39
That's my last question is, what do you see coming that is exciting to you, because I just had a Dr. Jeffrey Millman on the other day from Wash U. And he was talking about stem cells and how they're getting cells. Now the sense glucose make insulin not seen as you're bound by your body as a farm. You know, that's, it's all amazing. Like, yeah, no,
John Brooks 55:59
it is, but you know, and it's happening, you know, in different parts of the world, you know, that there's people working on, you know, defeating the autoimmune process people working on, you know, basically protecting the beta cells, there are people working on regenerating the beta cells or people working on in capitalization, there are people working on, you know, new treatments. I mean, you look at some of the stuff, you know, the nice salsman, you know, at mgh with ECG, and you know, so lots of advancements, people are making headway, you know, you look at, you know, semma, which was a Doug Melton company, now part of vertex and all sudden, you get a very big pharmaceutical company working on, you know, kind of, you know, beta cell and capitalization, you know, you get other kinds of companies that are in that space. And little by little, you know, we're kind of cracking, you know, wider regulatories T cells go awry. And, you know, how do you do that? So, yeah, I mean, we could talk for another couple hours on, on, things that I see. And, you know, I'm usually involved because, you know, I just get motivated by that. And again, companies sometimes seek me out, because they know, I know enough to be dangerous, and maybe I can help them either get financed or advanced, right,
Scott Benner 57:15
understand how to get through the whole process. And that's got to be such a huge part of it. It's just having somebody with you, that can help guide you around the pitfalls, right. That's got to be
John Brooks 57:24
Yeah, I mean, you know, I've been, you know, doing this for a while, and, you know, seeing the good bad, the ugly, but, you know, the hope is that, you know, at the end of the day, you know, a lot of these companies to challenges, you know, getting the financing and having a value proposition that's compelling to investors, and, you know, making sure that they thought through the timelines around, you know, regulatory issues, quality issues, reimbursement issues. And in today's day and age, it's the old Wayne Gretzky line. You know, you don't want to develop something, you know, to solve today's problem. It's, where's that puck gonna be five years from now to
Scott Benner 58:01
skate? Where the puck rolling, right?
John Brooks 58:03
Yeah, where's that competitive landscape gonna be? Who else is out there? And how to make sure that you're, you know, kind of leapfrogging the competition, not just incrementally saying, Hey, I got a better mousetrap. And, you know, if you're already kind of behind the times, so I tell people when they're using their insulin, that everything you do now is for later, and everything that is happening now is from something that you did in the past. And I think that thinking like that, in general is a great idea. Well,
Scott Benner 58:29
john, thank you. I don't want to take up any more your time, but I do want to leave you with something. Because I, I don't know that I fully wrap my head around this sentiment that gets given to me a lot until you were talking about your son. But people thank me, my daughter does not come on this podcast, right. She's 16. She doesn't care about a podcast. And and people tell me all the time, how grateful they are that her situation led to their success. And now I'm realizing as I'm sitting here is that, that this podcast really is born out of my concern for my daughter, and she's wearing an insulin pump that was born out of your concern for your son. So it's very kind of chilling, honestly.
John Brooks 59:09
Well, I would, I'm sure he'd be interested. So at some point in time, you want to do a podcast with my son, I think you're gonna find you know, he's even sharper than I am. So I'm gonna do
Scott Benner 59:19
that. Yeah, No, I haven't. Yeah.
John Brooks 59:22
Yeah. I mean, he, I mean, if you think of it, I mean, you know, he, he's, you know, understands this disease, because he Elizabeth every day, and, you know, working for a company that you know, now is extremely successful. And, you know, what had some interesting experiences along the ways. So, you know, so yeah, you might want to get him on a podcast, I think you'd find it pretty entertaining. Well, it'll be easier for me to find him than it was for me to find you. Because, you know, you just would go around saying to people, like, you
Scott Benner 59:48
know, the guy that made the pot What's his name? And said, finally, somebody one of my friends had on the pods like, it's john. And I was like, Oh, is that him? And she goes, Yeah, I said, I think I know someone at t Wendy exchange. I'll be fine. Cuz like, I'll figure it out, which is another great organization that you you sit on the board of Is that right?
John Brooks 1:00:05
Yeah, yep. T Wendy exchange college diabetes network. You know, so you know, places diabetes related. You know, I'd like to think I can be helpful in some way.
Scott Benner 1:00:16
Well, I'll know I'm doing well, when you want to invest in me. Chad, thanks so very much. I really appreciate it. My pleasure. All right. Take care. Have a good day here.
Unknown Speaker 1:00:24
Yep. Bye. Bye.
Scott Benner 1:00:27
Hey, huge thanks to the pod father, john Brooks. Can you imagine it if people by the way, if you know john, start calling in the pod father, I'd like to see that pick up if you guys can make that happen. Thank you. Anyway, john, thanks so much for coming on the show. And for sharing your amazing and very unique experience dreaming up an insulin pump. Thanks also to the T one D exchange T one d exchange.org. forward slash juice box. Join that registry today support Diabetes Research, support the podcast and touched by type one touched by type one.org. Thank you to those sponsors. And of course, welcome g Vogue glucagon to the family of sponsors here at the Juicebox Podcast. Learn more about that pre mixed prefilled, glucagon or the hypo pen at GE Vogue glucagon.com. forward slash juice box. There are links in your show notes. And at Juicebox podcast.com. To all of the wonderful And may I say delightful sponsors of the Juicebox Podcast. Check them out if you would. Thank you. Hey, last thing, the Facebook page for the podcast is blowing up. I mean, that is what the kids would say. Right? It's it's blown up. Be like you know what they said about their phones and stuff. I'm I'm very old. I don't know what people say. But that's not the point is on Facebook. There's a public group. It's called bold with insulin. And there's a private group Juicebox Podcast, type one diabetes, that private group up to 6000 users just about, huh? Is that bananas, 6000 people and they're just helping each other out. It's amazing. It's the kindest place you'll ever find on Facebook hand to wherever you want to hold your hand up to when you're swearing on things. I mean, it I've never seen a nicer, kinder, more thoughtful, less egotistical, more lovely and delightful group of people helping each other with Type One Diabetes than I have right there in that group. I am as proud of how that group functions, as I am about anything else connected to this podcast. It's really, it's quite something. And the public group has like 10,000 people following it. I'm really stunned. I am not really a Facebook person, but turned out to be quite a little resource and I'm super happy about it. Alright, I hope you have a great day. I hope you've enjoyed this conversation with john learning more about how the Omni pod came to be. I really did and what else feels like I have nothing left to say. So that is that
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
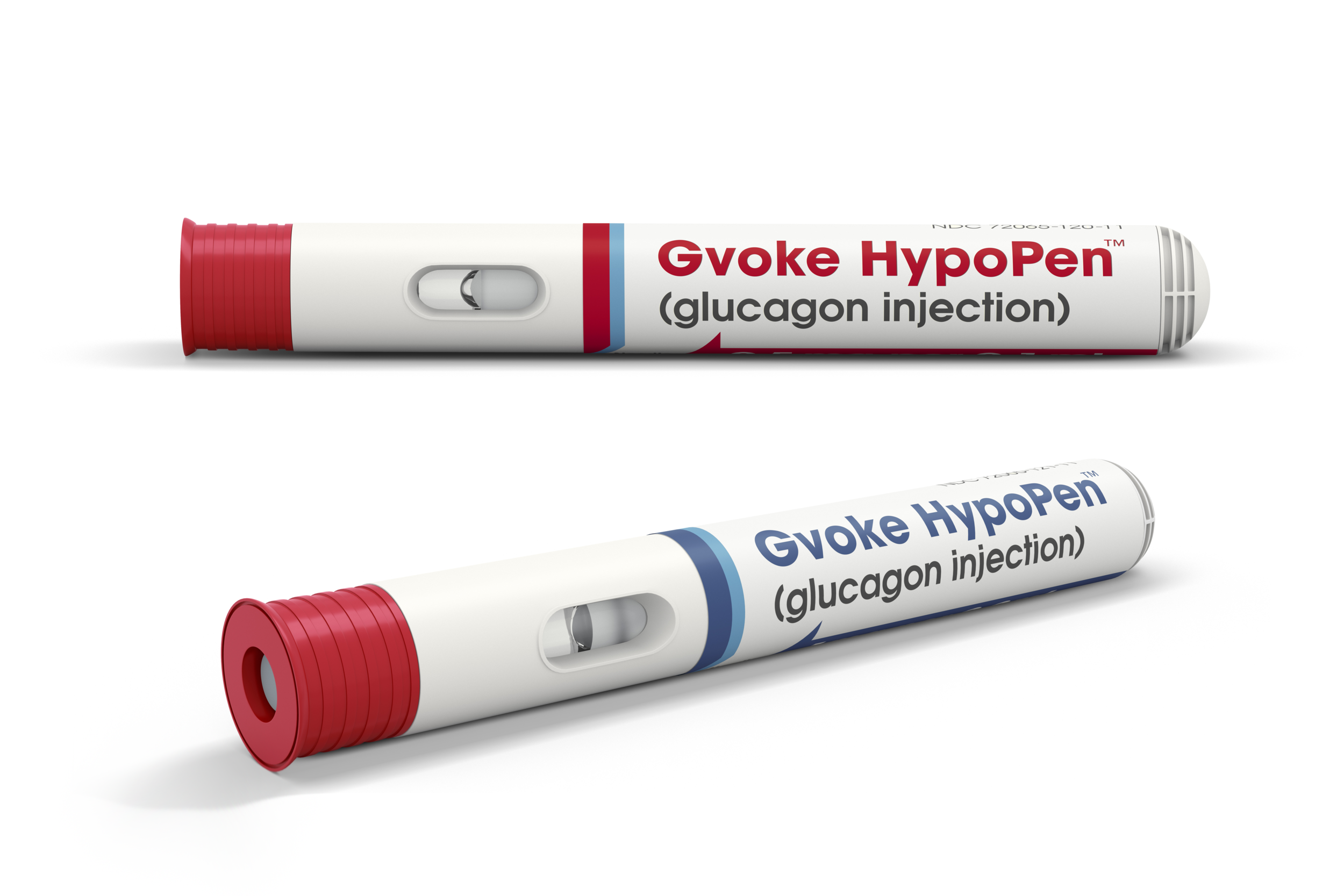
# 385 Gvoke HypoPen
Gvoke is a premixed, prefilled, premeasured liquid glucagon that now comes in a HypoPen!
Ken Johnson is Senior Vice President, Clinical Development, Regulatory, Quality Assurance & Medical Affairs at Xeris. Ken is here to talk about the Gvoke HypoPen. Xeris makes Gvoke. The premixed, prefilled, premeasured liquid glucagon for treatment of very low blood sugar in adults and kids with type 1 diabetes ages two and above.
Jenny Smith is also here to help me answer questions about glucagon.
Learn more about Gvoke here
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott (1s): This episode of the Juicebox podcast is brought to you by GE Voke. The world's only liquid stable Glucagon G Volk is available in our, a prefilled syringe and in an incredibly convenient to carry it an easy to use HypoPen. As a matter of fact, I have a trainer of the HypoPen right here. Let me show you how easy does to use cap comes off. I find some skin press down
1 (28s): And it's done that.
Scott (30s): Yeah. Easy to administer glucagon. It's the easiest thing I've ever seen when it comes to Glucagon hands down. We're going to talk all about it today. How the G vote Glucagon came to be or what it is, and this brand new HypoPen, which is incredibly convenient to carry. And as you just heard, super simple to administer, anybody could do this in my opinion, before I start the show, let me say thank you. Because every question and this episode came directly from listeners to the podcast. So I really appreciate the effort and the thought that you guys put into those questions. And I hope you get your answers. I think you're going to today's episode is going to be a little different than most I'm interviewing to people today about Jeeva Glucagon first.
Scott (1m 16s): I'm not even first. Now here's the surprise. Let me just give you the surprise. Jenny is on this episode. Jenny Smith is here and I'm also speaking with Ken Johnson. Now Ken is a senior vice president of Clinical. Wow. This is quite a title at here. Ken Senior vice president Clinical Development Regulatory Quality Assurance that? Medical Affairs at Xeris pharmaceutical's Xeris makes Gvoke. Ken's got to answer all of your questions and Jenny is going to answer something to me.
1 (1m 45s): You guys,
Scott (1m 46s): You love Jenny. I love Johnny. How can we not love Jenny that's who else are you going to love? Ken Ken who buy the way has the secret talent. The man could play the piano, but not have to wait all the way to the end, to find out about that. Please remember that Nothing you hear on the Juicebox Podcast should be considered advice Medical or otherwise always consult a physician before making any changes to your health care plan or becoming Bold with Insulin
Scott (2m 38s): And there are two ways that you can request it through your doctor, either online or in person. If you have commercial insurance, you can request a prescription for Gvoke HypoPen right from the comfort of your home and have it delivered to your door fulfilled through PillPack by Amazon pharmacy. Just go to
Scott (3m 19s): We're going to start with Jenny Smith and then do a little Ken and then back too, a little Jenn. And Ken you got to get a nice rhythm going a little Jenny a little Ken is going to go just like that. I think you're going to enjoy it at the risk of repeating myself, because I say it in the episode, this is a leap for people who use Insulin making Glucagon liquid stable. It just This. If you don't understand why listen closely Jenny I already talked to Ken Johnson from Xeris pharmaceuticals about the Gvoke Glucagon and he's gonna be on the Show.
Scott (4m 7s): And just a minute, we talked a little bit just about what they were, you know, what they're trying to accomplish. I told him if the end of our conversation, that I'm incredibly excited about that company, like the ability to stabilize Glucagon in a liquid form, I think has other far reaching possibilities that I'm really excited about. But while I was talking to him, I got a it's a it's a, and can you tell if you can see this or not, but it's called their HypoPen and this is just a trainer, so it's not, it's not real, but you just pop off the cap and go like this and that's it. And it's over yet. And I was like, huh, well, that seems simple.
Scott (4m 47s): And I'm going to get one of those for Arden
Jenny Smith, CDE (4m 50s): Beyond simple. It's not scary
Scott (4m 52s): Exactly. Because you know, till this point in my life with type one, diabetes, glucagon has been a little bit of an, a, like a science experiment, but it was going to be an in a pressure situation. It's almost like someone saying to you here, do this while your driving a car, and there's a bear in the backseat, you know, you kind of felt like that to me the whole time. And, and they have their pre, they have their premixed syringes for emergencies to, which is just, you know, it's you just, it's in and push and you're done right yet. But, but still, and I'm, I'm going to ask you first, before I tell you what we do.
Scott (5m 35s): Do you carry Glucagon with you when you leave the house?
Jenny Smith, CDE (5m 40s): I don't carry Glucagon with me. If I'm just leaving the house for like going to the grocery store or going across the street to the park. No, don't I absolutely don't when we leave to go on even like a short weekend, two are in-laws or I go on, you know, to speak somewhere and whatnot. Yes. I, it with me now in that same case, though, if I'm carrying it with me in my pocket at a conference, somebody got to know what's in my pocket.
Scott (6m 9s): There's a lady on the floor. Hey, there's a science kit in your pants. What do you think? That's? What should we do? Where in the same boat, we don't carry it around like that either. If we're going to go too far away, or if it's going to be, if you're going to do at the beach or a trip, it comes with us. So here's my question. Would you carry this with you?
Jenny Smith, CDE (6m 28s): I would, because one, that's really easy to keep in my purse. And I mean, I've also, you know, knowing that I've got a son who'll be in second grade or something like this are easier to carry, I think, and from the standpoint of even teaching him visibly, there's no needle. I can easily say, Hey, pull this cap off, you know, stick it in my thigh, push it until it turns red and it clicks and it's done. I mean, that's it.
Scott (6m 58s): And it has these audio responses. I don't know if you can here the sec. So there's too, there's the push. And then the second one tells you your done. And I was like, huh, this I would put in Arden's bag. Like I really would. It's not going to scare somebody. And not only that, but if somebody opened this up a person who had no idea what they were doing, it's going to, you know, the packaging tells you what to do. And there's nothing about what I said to Ken when I was talking to him was I took this out of the mail, this trainer, and I handed it to my wife. And I said, I don't wanna tell you anything about it. See if you can make it work. And she did it right away, but it didn't take any like thought to do it's easy.
Ken Johnson (7m 39s): Hey Scott, this is Ken Johnson I'm with zeros pharmaceuticals. And I have a number of responsibilities that the company, including how we develop our drugs in the clinic and get them approved by the FDA. We also have medical team that supports ah, people with diabetes. And there are clinicians in the marketplace. And I also have a quality assurance team that makes sure that the drug's as we make them package them and ship them to pharmacy's and ultimately people and their homes meet the higher quality standards required for a prescription product. So all of those combined have been my responsibility at Xeris pharmaceuticals. For the past three years, I've been in this type of role for pharmaceutical development for a better part of 25 years.
Ken Johnson (8m 25s): I started out, I was trained as a pharmacist. I did research at the university of Colorado, whereas also involved in clinical research as a result of that clinical research. And I found my way into the pharmaceutical industry sector and had been there ever since. So that's a little bit about me. I'm I'm in Chicago where our headquarters are based and really happy to be with you today.
Scott (8m 47s): Thank you very much for doing this. I have a question about how you pull a team together for something like this. Does Paul know of you and com for you, or how does that work? Like how do you end up at Xeris?
Ken Johnson (9m 1s): Great question. So Polytech, our CEO, as someone who I met at the early part of my career. So 20 plus years ago, we were at a company based in Chicago called Searle pharmaceuticals. Paul was in charge of a number of commercial activities there and ultimately taking over some of the regional activities around the world, ah, for a number of our products. And I was his medical support. So a, you know, these things start early and have sort of an indelible effect. If these partnerships work and these collaborations work, you sort of maintain these relationships throughout your professional arc. We haven't always worked together, but oftentimes we'd been together out a couple other companies since that time. And most recently is he took the home at Cirrus who wanted to bring it together.
Ken Johnson (9m 44s): A group of folks that you felt could take us to the next level, get Gvoke HypoPen to market. And with that, he found me as well, a few others, we had this collective past together. So it's a little bit analogous to getting the band back together again. And we've, we've done that. And because of our past a familiarity success together, a what I think is an ease of collaboration, we do enjoy working together and I'm sure I'll do it again someday. Yeah.
Scott (10m 13s): How do you feel like The from the starting point to where you guys are right now, do you feel like that was on schedule went quicker than you anticipated? How much of that has to do with the, the, the, the, you know, the G Voke itself and how well it does, what it's, you know, what you're trying to, what you're trying to do.
Ken Johnson (10m 34s): Yeah. I think we encountered a situation where things were a little bit stalled or, or there's a few things that we had to take heat of that had been discovered before we arrived to make sure that we had, you know, a product that could meet all of the standards of the FDA. You could pass all the Clinical assessments. And so it really good foundation Scott, but it needed them and sort of to be rebooted to use that term it, and that meant conducting additional clinical studies further characterizing the product, making sure that we could put it into a prefilled syringe that's RPFs configuration or the HypoPen in the auto injector that was just released earlier this month. Right.
Ken Johnson (11m 15s): So that whole process of building, making testing, and then releasing brought together the team that you see today, you know, in fairness, there were about 12, 15 people at zero S when Paul took over and, you know, it's taken a lot of resources, people energy now in 200 plus employees later, you know, were on market with an approved product.
Scott (11m 40s): And for me to be sitting here holding this, this trainer pen, I guess it's a, it's a long time to get this into, get to this form and make sure it does what it says. So I think I want to understand what does it do because you've obviously come into a space where everyone has that red box and they genuinely think of it as something, you know, that they just have. They don't think much about it. I've been in that situation. My whole life. I get my daughter supplies, my daughter's supplies show up. They're there. I watch it until the expiration date and then I throw it away and I get another one. And I don't know that it's something that many people think about other than I know in the case of an emergency, you know, I've got this liquid in this powder and the syringe, and I'm supposed to mix them together and redraw them and use them.
Scott (12m 28s): And here's how, and ya know, and that kind of thing. And I have to train my school nurse to do it and, you know, My and her, grandma's got to know. So when she comes over, that's, that's, that's the narrative around that my whole life and for, for many, many people. So how do you improve on what's been going on for so long? Like what makes you feel like this is a great business and we should be doing that?
Ken Johnson (12m 52s): Well, I think, you know, just listening to your story and kind of the anxiety and complications that come with administering Glucagon for many, many years now, you know, going on in several decades of having the same configuration, it is a important pancreatic hormone Glucagon has very well known affects in terms of its ability to raise blood sugar. I think, you know, most days we're concerned about lowering blood sugar and insulin is critical, but, you know, think of this as the, the, the break where the accelerator, the, no, that the challenge is always been, it's a powder that requires reconstitution or, or, or put into a solution immediately at a time of use.
Ken Johnson (13m 37s): You can't do it early because it starts to break down very quickly. Most of the potency has lost or within 24 hours after mixing the powder for all these decades, that red box that you describe has been the single and only configuration available to people with diabetes are folks who would experience very low blood sugar. So our chief scientific officer took that on as a mission, you know, had his own personal experience and people in his life who said, you know, is it possible to overcome all those complicating, a multistep requirements of the lateralized Poudre in that vile? And he said, yeah, I think I can fix that. So it was his mission to make it a liquid, ready to use room, temperature, stable product, and to do that, we had to overcome the limitations of water and water is what you would use in the traditional kids to make it as a solution.
Ken Johnson (14m 29s): So we've taken water and replaced it with other a well known a solutions. Ours is called
Ken Johnson (15m 24s): And so you have basically a, a built in system to raise your blood glucose. And as such, we, you know, we wanted to just make the process of administering very approachable, very intuitive and not intimidating. And so we think we've accomplished that, but that was all only facilitated once we had a liquid version.
Scott (15m 44s): All right. After someone uses Gvoke what happens after is, are there side effects or are there things that happen afterwards? Am I going to feel nauseous? Do I have to go to the hospital? That's also, what's your dog's name, Bailey like that?
Ken Johnson (16m 0s): The question is, so I guess, I guess we'll have to give her a credit today. So a couple of things, I mean, you know, the effect that you do want is to raise a blood glucose, and that happens very quickly as we start to see changes in the blood glucose concentration within the first five minutes of administering the product is raised to what we consider a safe level of blood glucose very quickly on average, about 14, 15 minutes. And then the duration of action is probably about 90 minutes or so. So you have this ability to sort of bring yourself back up and then have it come back down, right? So it's a, it's a temporary fix two. What was a scary as hell? What can happen?
Ken Johnson (16m 40s): Glucagon has some other effects has some effects directly on the gastrointestinal tract. And so it at about 30% of the subjects that are trials has some nausea and about 10% handsome vomiting. So those are 10 or 15%, and those are kind of the hallmark features of what Glucagon does not matter what too, to anyone that sensitive to those GI side effects, importantly, they are transient. They are mild 80% of the people in our study and characterize them as mild. They went away and in our case, no one actually stopped being in our study because they had that, that known side effect that you would see that Scott with the old movie got, and you would see it with our Glucagon a you'll see it with future Glucagon so that we haven't mitigated.
Ken Johnson (17m 30s): It's probably dose-related. I think, you know, there will be a Day I hope someday where if we, you know, use different doses for different purposes, that we can mitigate some of that nausea, vomiting, but for the rescue one milligram setting of use your gonna have, in some cases, nausea and vomiting, then those side effects are
Scott (17m 50s): Side effects of Glucagon do not have a specific brand. It's just what happens during the process of bringing that low blood sugar up so quickly through Glucagon.
Ken Johnson (18m 0s): Yeah. And it may not even be read to get your rights. That's, that's the correct way to describe it in event, not even be related to the blood glucose, going back up as much as it is. There is a known, in fact that Glucagon to slow down the action of your GI tract so much. So that is completely different from what we're talking about today, but a radiologist will actually use this drug to stop someone's GI tract from moving, if they need to do procedures and other things. So now this is one of those situations where a bad thing for some person is a good thing for another, but it is important to let people know that there is some mild nausea in about 30% of people who use it for, for rescue.
Scott (18m 41s): Can you help me understand the different ways that I can administer as you vote when, you know, when you guys first came out and I became aware of You, my daughter switched too it, and she has the, the prefilled syringe, but now I'm holding. Like I said, This this dummy pen. That to me feels like I'm like what people would consider an epi pen and to be, I, I, I just push it down on my leg and hold it there for a second and, or a couple of seconds in, and I pulled away. Why do you have different versions? And can you tell me the difference between them?
Ken Johnson (19m 16s): Sure. The Glucagon it's the same for both a Gvoke PFS are people terrains in G Voke, HypoPen in the auto injector, you're holding a, in your hand. And so there's no difference. And that the active ingredient, the solution, the concentration is identical. It was a simpler and more straightforward manufacturing process to come to market with the prefilled syringe. It's less mechanical requirements because you, as a person, are the person helping you is actually going to do the injection much like you would self-inject or Jeff Insulin. Right? So it's a small subcutaneous injection, the necessary requirements to then put that into a device that fires itself, the auto injector, umm, it's more complicated, more engineering.
Ken Johnson (20m 7s): And we wanted to make sure we had sufficient quantity. So we come to market like we did the Smith and not having a sense of shortages or, or, or running out to be able to supply to market adequately. So, umm, there's a really, really high specification for performance of that auto injector because you're no longer responsible for pressing the plunger and the mechanics inside the auto injector. Our and so the FDA has carefully scrutinized the performance of this device and it has to work 99.99, 9% of the time. So that's a manufacturing spec and it came out of the experience that we've all had with epinephrin and HypoPen we want to make darn sure that if someone's going to pull that red cap off and press that yellow plunger, that if a fire's and so that took us a little more time.
Ken Johnson (20m 57s): Both were approved last September and in 2019, we could bring a prefilled syringe to market immediately and then to deal with all the issues that I just laid out. We just need a little more time and happy to release that now in July,
Scott (21m 12s): That's exciting. It really, it really is terrific. As I'm sitting here holding it, I mean the, the leap and leap really is the only word from what I'm accustomed to, to this it's it's like they're not even the same species in a, to B to be honest, it's a, it's a great, a great advancement. So I mean, whoever that guy is, you figured out how to make that, that liquid stable stuff is, is brilliant. Hey, have you ever used the Glucagon Isn't working on everything she's like, so the reason I asked is because while, while we were talking about this, he said, you know, we, we were talking about people administering it at themselves and I'm trying to think, I wish really trying to picture like, where's the tipping point where you're, it's gotta be, you know, it's not going to be one of those like, Oh, I got a little low, I need to eat something.
Scott (22m 10s): Obviously that's that's first, but there's probably a moment where you, I'm guessing, you know, imagine you're on a CGM and you see, you have double arrows down in your 50 a and you think, you know, you do the math real quick and you think, Oh my God, I gave myself too much. Insulin I can't catch this, do this like this. Right. Yeah. That made a lot of sense to me. I I've definitely been in situations where I thought, I don't know if I'm going to stop this with food and you know, and that's for Arden, but I really thinking about adults living by themselves. Okay. Can I have a question that I heard you say a second ago you were talking about self-injection and I think that there are many people who might assume that Glucagon has only for when you are having a seizure or an unconscious, but how would I self inject if I'm having a seizure or unconscious?
Scott (23m 4s): So obviously that's not the only time to use it with when are the times I'm supposed to be using this or, or I'm able to.
Ken Johnson (23m 11s): Yeah, I think that that's a great discussion. Thanks for raising that point. So I think, you know, there are a number of settings. Everybody has their own personal experience with what they deem very low blood sugar. I think you, in some of your colleagues have taught me this phrase, the, I don't know, low. Right? And so when that happens, it could be because you are looking at your numbers, it could be because you start to feel differently. And you know, some of the sort of classic signs and symptoms are, you are shaking. You're dizzy, you confused, maybe you haven't changed your personality or, or more combative, you know, trouble answering questions. Those sorts of things are all kind of hallmark sciences I'm going low.
Ken Johnson (23m 52s): So when that starts to happen, of course, the first rule of thumb is try to correct it with food or drink, right in your favorites. A source of glucose for many, many decades now has been referred to you as the 15, 15 rule, you know, take those 15 grams and the 15 minutes and see if it's work, if you're improving. So that's one situation maybe that isn't working and it's a stubborn lo and you know, you're starting to now wonder what's next. So that would be a time to consider administering Glucagon. And I think most people would not have reached some state of incapacitation where if they were familiar and able to a administered the auto injector where the prefilled syringe, they can, there are other settings where people are unwilling or unable to swallow or to have enough, you know, stuff available.
Ken Johnson (24m 43s): Maybe there a place where they don't even have access to a source of glucose. That would be another situation. If you feel like your passing out and there's somebody with you, obviously you'd want them to be able to administer it so that the community discussion, he should know the other people in your life, be familiar with where, with the gun it is and how to administer it. As you pointed out this HypoPen auto injector, it's a super intuitive and the instructions are printed, write on the pouch. And so I think if somebody found you and you said, you know what to use it, you know, it's going to be very straightforward process. We have tested that and found that in simulation exercises where someone is going through simulation or of an emergency in a very low blood sugar, they were able to administer correctly 99% of the time, follow the directions and do the two step process that you just talked about.
Scott (25m 34s): When the, when the trainer arrived at my house, I took it out of the packaging, took the instructions away from it. I handed it to my wife and said, I told her what it was. And I said, don't even think about it, try to use it. And it didn't take her 10 seconds to figure out what to do with it. And nobody here has ever used, you know, an epi pen or anything like that. So we've never held her or seen anything like this before. And I made me feel like, I hope my insurance company will cover a bunch of them or spread them all over. Arden was a college experience when she leaves for school. For me, I'll just, I'll just put one everywhere. It just really was intuitive. Is the word for it. It's you can't look at it and hold it and like eat.
Scott (26m 16s): There's no other thing to do with it. I don't know if that makes sense or not. You know what I mean? Like it feels like there's just one way to accomplish something and it, and it shows you that while you're holding it, like you said, it's in the instructions, but I'm seeing when you have the physical things in your hand, it's not like there's seven levers and you've got to decide which one it is. It only does one thing. And then, you know, if it does it well then perfect.
Ken Johnson (26m 37s): You know, I think, you know, that was part of the design, the understanding there's a whole area of science, human factors, research the services. How do we approach? So to solve a problem. And, you know, there's very, very intentional features built into that auto injector. The colors are intentional, the little window that you have that shows the liquid Glucagon, you know, in there. And it disappears. It turns red when the dos has been delivered, that's intentional. The clicks that you hear, those are intentional to let you know the sort of audio queue that the cycle it has been completed. We also have safety built in when you finish the injection and withdraw the plunger from the bare skin, it locks out.
Ken Johnson (27m 19s): And so you cannot have a needle stick because there is a needle inside the device, but it's, you know, never appears during the process of the injection. And when you're finished is locked out. So you can't have an accidental needle stick. Can I ask
Scott (27m 32s): Where can, can you just inject it? I mean, anywhere, like where has it, where did you, where were you able to get the FDA approval? And how do I remember that when I'm going low? Like, you know, or is it just anywhere I can get it into me is good.
Ken Johnson (27m 47s): And we, we concentrated on three areas, thigh, abdomen, and your upper arm. So we figured out, in most cases, one of those is going to be readily accessible. If you do have to have bare skin, because we want to make sure, you know, this is a 27 gauge needle. We want to make sure that there's nothing sort of inhibiting its path as it goes into the skin. But you know, we, in our assessment, Scott, most people opted for the abdomen. I think it was probably an easy to just pull your shirt up. And most people have an adequate real estate there. So, you know,
Scott (28m 20s): If I'm going to say I'm okay, I don't, I might all need Glucagon, but I'm a, but I definitely have a place to inject it. So,
Ken Johnson (28m 27s): So, so any, any of those three sites and it didn't matter, you know, the results, the clinical changes that we saw were the same, regardless of psych.
Scott (28m 35s): Well, that's even, that's very exciting because like I said, for people who know about older products, it's a, we were always taught, you know, deepest part of the buttocks, you know, like it's a, it's a big needle, you know, it's a, it's not an exciting, not an exciting endeavor for certain. So even that's a huge leap is my insurance got to pay for this. How do I, I mean, that, that's part of your purview, right? When you were talking earlier about what it is, you're a, you've done in the past. And so you, I'm assuming you have some background on this. You can talk about it a little bit. Yeah, I do.
Ken Johnson (29m 10s): If you know, and you never want to have a drug approved, but then not have any access for people. And so, you know, that's an important contribution that the company had to make in terms of going to insurance companies, going to pharmaceutical benefits management companies, you know, very close to the time of our approval last September and have these discussions about why it would be so critical to be able to offer this new a much easier, much more approachable version of Glucagon and the one they have been covering. So there wasn't any restriction on your Read KIS. And so we ask, can you give us the same treatment? And I'm happy to report as we sit here today for a commercially insured individuals, if you have unrestricted coverage at 87% of plans in the United States.
Ken Johnson (29m 54s): So almost 90%, wow. That, you know, why isn't it a hundred, there's no product that ever has a hundred. So there's always some small portion where there's going to be additional requirements. So that would mean that you would probably still have a copay and everybody's plans are different. These can be very, but you won't get one of these not covered types of messages. And the 87% of covered lives in the United States for commercial insurance. If you look at Medicare, probably the next biggest segment for people with diabetes, who should have Glucagon is about 80%. And then we're still working our way through the Medicaid requirements and were about four to 30% on Medicaid.
Ken Johnson (30m 37s): So if you know, for most folks, your not gonna have any significant access issues in terms of affordability, we are right now, if you go to glucagon.com, you can get all the details on a copay assistance program. And the net effect of that Scott is you would have a $0 out of pocket for the HypoPen for the, for the present time. So we're, we're starting out the launch of the product, offering that additional support, which means if you say had a $30 copay and you qualify it for the program, the company would subsidize at $30. He is essentially received it for free.
Scott (31m 15s): That's excellent. A great what was the,
Ken Johnson (31m 17s): The webinars Gvoke glucagon.com. It's GV. Okay. Now I've had a few people say, gosh, how do you pronounce that? But a GV. Okay, look again on.com.
Scott (31m 29s): Glucagon.com. I got it. And I'll put it in the show notes so people can find it too. So if someone's using a different Glucagon right now, and they've heard you on Thank I'm would like to try this, do they wait to their next appointment, go to their doctor and say, I want to switch my Glucagon are, or what are the pathways to making the change?
Ken Johnson (31m 49s): Yeah, I think any of those might work. I think traditionally, when we need something new, we would contact her in health care provider and se there's a new Glucagon and it's called Gvoke HypoPen. Can you send me a prescription for that? Can I get a film, our experience with clinicians if they are pretty well aware now, but this is a configuration that's on the market. We've been working hard with a professional society's and through their channels to make sure that they know that as a personal Diabetes requested that they would, you know, no of it and not be afraid to read the prescription because have the access issues. Now you have also been cleared that makes it very easy for them. So it's not very cumbersome if you don't want to pursue it that way and just make a call to the doctor's office, usually does not require a visit.
Ken Johnson (32m 34s): Scott it's just a, you know, a new script is an issue from the electronic system. You can pick it up. That's your favorite pharmacy. You can also go to the website and we've set up some services. They're a little bit more analogous to kind of ordering online and you can enter some personal information or information about your doctor. And we have support services available now through pill pack and Amazon company that will work with your doctor in deliver it to your home at no cost.
Scott (33m 5s): I'm not sure I heard you, right. Is it PillPack?
Ken Johnson (33m 8s): Yeah. So the Jenny that helps assist in sort of the transactional part of this is PillPack. It's an animal Amazon company. A but the easiest thing to do is to go to
Scott (33m 50s): Right? So if someone listening just feels that economically they can't do this, they should be able to and contacting you is the way to go.
Ken Johnson (34m 1s): It is. And I think Listen, there are, there could always be some leg and whether or not the coverage policy has caught up and maybe their getting a strange answer about how much their out-of-pocket would be and things like that. We have a whole assistance program in place to help navigate that. We know how frustrating that is, you know, we wanted to make Glucagon easy to use, and now we want to make getting a prescription filled, easy to do. So, you know, we have very, a nice set of services that are linked to the website. There's also a phone number at the website. And in case it's easier just to call and talk to a real human, but you know, that takes you through a whole tiered process of, you know, is it going to be covered?
Ken Johnson (34m 42s): You know, what pharmacies have it and so on and then write down to even, so the patient assistance programs for folks who can't afford their medication,
Scott (34m 53s): The concept of having to mix Glucagon stopped us from using Glucagon when Arden was legitimately having a seizure. I just don't know that. I mean, you know, technology's better now, obviously, and that's great, but I don't see, I can't imagine going backwards on this one, like this to me seems like the best it's available. Right. I was wondering, do you hear from people about mixing and what did they, what are the responses? Do you think that that having to mix the Glucagon stops people from even considering it as an option? Sometimes
Ken Johnson (35m 33s): I think given that that was all of that, there was all that was available
Jenny Smith, CDE (35m 39s): For such a long time. I mean, you know, again, thankfully my parents never had to deal with that. They never had to mix it. They never had two. It was always there. He always knew where it was in the house, but I, I would say that it's certainly a deterrent to use because it's, there are just the extra steps, again, as you brought up in your situation, it's like having to think through those steps when you got your loved one, either having a seizure or you've discovered them completely like not with it at all out, can't talk to them, whatever your brain is thinking in terms of helping them.
Jenny Smith, CDE (36m 24s): Yes. But all the steps of mixing, making sure it was mixed right now, you've got in the needle on that. I mean, this is scary looking needle, compare it to a syringe needle for Insulin. It is, it's a bigger needle, right? So, you know, imagine putting that into your two year old or even your 12 year old child and knowing that you're doing it the right way. And I can say that it would be a it's a deterrent, although I dunno, in the case of not having anything else as an option, you figure it out, but it's certainly going to be,
Scott (36m 58s): Well, I have a friend who recently had a teenage son, a have a seizure and she got the red box out. She got it mixed. And when she went to draw it back out, like in the, what your describing, running upstairs, people yelling, she broke the needle off in that crazy. So they had to go to a secondary option, but they were getting ready to use it. And she, she was trying to traverse there's and mixed Glucagon at the same time she was running to where it was happening, you know? And I think, I just think that that's the point, is that anything that simplifies that is genius and putting it in, you know, what can be described to people who don't know any different?
Scott (37m 44s): Is it as an epi pen style? Like just this thing in your hand that you just push down and hold this, turns it into something people can carry with them.
Jenny Smith, CDE (37m 52s): Absolutely. I even think two from a school type setting, even the comfort level of, let's say for some reason, you know, technology is down your not able to contact the parent. You don't know exactly what to do. I mean, from the standpoint of safety and feeling okay, and teachers or the Peros or whoever's helping at school, this is a hundred percent easier.
Scott (38m 17s): I think this takes away from that thing that a lot of people who aren't, who know, who have kids know, you go to school and you're like, I need somebody to be a Glucagon advocate from my kid. And everybody's like, no, thank you. You know? Like, like they really do too, like teachers, or like, I don't want to be on the hook for this, but, but this is like, again, I think this takes away the possibility that they can make a misstep in the middle, like drunk when Arden was a little, her, her directions were drawn up half the vile. You should have saw the fear that put on someone's face. Well, how do I measure half of the vile? I'm like, I don't know. I bought it. And they're like, what? I'm like, Oh, here we go. This is fine. After I get either the prefilled syringe or the HypoPen, how long do they last until they need to be replaced?
Ken Johnson (39m 4s): Yeah, that was part of our design criteria. We didn't just want to make a liquid ready to use if you wanted to make sure it could last a long time because you know, hopefully once or twice a year event and most, and even if it's a never event, you know, let's do not have to replace it too often. So right now, from the time of manufacture to the end of life or a potency, a sufficient for a re restarting, the blood glucose it's two years, but it's a very long shelf life. You know, we, again, you know, that was part of the design process and certification process and approval with the FDA that we have a two year from time to a manufacturer expiration.
Ken Johnson (39m 46s): So that'd be printed on that other product. You'll know when it expires a number of pharmacies. Now you can have reminder programs. So, you know, it's time to get at all.
Scott (39m 54s): Can I have to tell you? And I genuinely mean this. I've spoken to a lot of people who work for peop you know, manufacturers of different drugs and devices, and that's the first time anyone's ever said anything to me that almost knocked me off of my chair. I just took two years. Is it's amazing. And not what I expected you to say. That's because what I was going to say is, you know, we got the prefilled syringe, and I had a question about that actually, before I go down my story, we got the prefilled syringe and it comes in sort of a pillow bag is my best description of it. And my first thought was, huh, there's a needle in there. And this is sort of a bag. And then when I reached out to the people who are listening to the podcast, that was actually a question they had was, you know, why does the like, explain to me why the, the needle is safe in this bag?
Scott (40m 41s): And I guess, I guess thinking couldn't it be deployed, but to answer that for me first, obviously you didn't make something and not think, Oh, I wonder, you know, I'm assuming it's been tested, but explain to me how you came to the, the packaging for the prefilled syringe.
Ken Johnson (40m 56s): Yeah. It serves to a number of purposes. The packaging is a sealed foil pouch. Its done a very, a controlled environment. The prefilled syringe that if you describe Scott actually has a noodle shield on it and also has a backstop to keep the plunger from being deployed. So why a pouch? I think you started with that question. So first of all, the instructions are printed on the pouch and we want to make sure because you know, the real estate on a, on a prefilled syringe where the real estate and the auto injector is not sufficient to describe how to use it. It would be six point font and we wouldn't be able to read it. We have these very clear pictures and words printed right on a pouch that could tell anyone how to use it.
Ken Johnson (41m 42s): In fact, we tested that we have people who are untrained in the administration of the prefilled syringe and the auto injector and they successfully administered it. You know, like I said before, 99% of the time. So the second is that foil and the gas that we pack it in inside there. Cause you notice its like a pillow because its actually has a pressurized it's in there helps with and moisture because those are the enemies of any drunk. It doesn't matter if it's Glucagon or anything else sort of protecting it from light and moisture helps contribute to that two year shelf life. So we, we can't stress enough that you should keep it in these pouches until the time you use what people are.
Ken Johnson (42m 25s): You know, people may say, well, it's, here's how I know what to do. What's inside the pouch. So that's why we've provided videos. That's how it could be provided the demonstration units. Like the, when you have, you know, they'll be available in the clinics. Doctors have been requesting those demonstration units. So if there should be no mystery about what's inside the pouch, but we do acid if he started in that until the time of use and it's, you know, so multifold purposes for having that pouch
Scott (42m 52s): Is it all makes sense. It just, and had, I probably thought about it longer, you know, what it really is is that it was just different and so than what I was accustomed to. So when I saw it different felt wrong and now you explain it to me and like, Oh, well different seems like more well thought out in a new and better. So a that's excellent. Can I give you
Ken Johnson (43m 11s): If you want to anecdote as we were testing that power and sort of the size of it and how big the print was and everything else, we've had a number of Diabetes educators as a part of our forum for focus groups. And there was some that wanted it even bigger because they wanted to write all kinds of instructions and the margins and the doctor's phone number and you know, reminders about other things and stuff. That's like at some point we had to say, no, you know, we can't add to it, this giant pouch, it's gotta be small enough and portable enough. So, so, you know, there, there were a few rounds of the things that, you know, let us to the current configuration,
Scott (43m 41s): If they did, they have it up to the size where you could put three holes in it and people get carried around in their binders.
Ken Johnson (43m 47s): They're, you know, so, so know is all intentional and a contributes to the, the long shelf life. It contributes to the successfully administering it and at the time of emergency and it also protects the product
Scott (44m 1s): Going back to the beginning of this thought for me, what I was getting ready to say, when I asked you how long does the product last before it needs to be replaced? What I was gonna say as I think I'm going to get to move on to the HypoPen afterwards, because I can see how, you know, it's just, it would just make, I think this would be easy to show my daughter and say, look, if you really feel like you're in trouble, do this. And it wouldn't feel like, you know, a rigmarole I guess, and, and, and maybe off putting in any way. And so I thought I'll switch, but now I realize I've gotta wait two years. I switched. So a, I M
Ken Johnson (44m 34s): You bet you brought up another issue and that is keep people, staged them at different parts of their daily life. Right? If you keep the prefilled syringe and the nightstand at home, you might have the auto injector at school or with the coaches or wherever. So, I mean, you know, mix and match again. There's no difference that in the Glucagon is contained any of their device for the product.
Scott (44m 55s): No, no, no. I, I, and I, I guess I was half kidding, but I do know that, you know, there are different Podcasts if our kids ever grow back to school, she'll need one for school in, in a couple of other places. And it just, you know, I can't, I can't say it enough, it's the, it's easy to have you on the show and talk about it. Because like I said, this is a leap and this is going to make people's lives. I think easier if they should ever have an emergency and need to use it. And I think the comfort they're going to get from it, just having it around Is is going to be different. I, you know, I really don't mean to pile on somebody, but that, that red box is not comforting. It's off putting, and this, this thing I'm holding this pen here is comforting. So there's a lot to that.
Scott (45m 35s): There's a lot to the psychological, the psychological side of all this. And I appreciate that. That was considered,
Ken Johnson (45m 42s): You know, we've talked with folks sort of who lived through all of this and seeing the changes in technology and new delivery. Insulin certainly advanced and the bringing forward CGM pumps are, you know, all these things have been stepwise improvements. Glucagon just, wasn't tackled. And, and, and now that we have, you know, we want to keep making improvements and exploring other other uses for it and beyond the, the, the currently approved one. And so the companies, you know, vested in making the most of a liquid ready to use Glucagon. And so, you know, stay tuned for more. Now
Scott (46m 20s): That as I was jumping on this call, I got a message from somebody. It was so funny. They don't know the timing of my schedule, but they just were like, if you, if you haven't spoken to the people at chief Oak, yeah. Can you please ask, is there a water and Insulin and if there's water and insulin can, can, Insulin be made more stable with their technology. And I was like, I dunno, I'll find out. So I, maybe my bigger question is, are there other things your stabilizing over there, or, or you just the Glucagon company, or is there more,
Ken Johnson (46m 54s): You know, we are more than a, Glucagon a company. So at our core, we want to take the technology to make liquid ready, to use easily injectable, very stable products and all of the areas where it makes sense. We have talked about it Insulin and it's a, it is a project and it's not anything that's a, you know, advanced in terms of it's Clinical Development. But we do recognize that there are limitations on the storage conditions for Insulin or other things that it can be mixed with cost problems. So maybe we can start to combine it with other effective, low blood glucose agents and make a better combination. So, umm, the, the short answer is yes, we can apply our technology to a broad range of drugs, proteins, monoclonal, antibodies, vaccines.
Ken Johnson (47m 42s): And so, you know, that's, our mission is to take all of the concern and the difficulties of administering and storing and drug out of the equation. And so that's, that's kind of the, the future state of zero S and, and how we'll apply ourselves. But you know, us now as the blue thing, as a company first and foremost, and a, you know, and we'll use that as a starting point and grow from there,
Scott (48m 5s): Your technology applies to a lot of other things. So they're, there are probably many things that we can't talk about that are being considered there. And I'm asking that question as a wink and a nod to all the people who asked me questions that are not covered by your FDA approval. So I can't ask you here, but they'll all understand where they hear this and be excited that you're working on other things I think is that fair?
Ken Johnson (48m 28s): Oh, that's definitely fair. And our company website to a separate from a DeVos glucagon.com describes some of our pipeline and the things that are still in an experimental phase. And you'll see that it's, Glucagon, it's a drug called die as a pan for seizures in other programs. So we're, you know, we're, we're really interested in applying this technology broadly and solving problems for patients and their providers,
Scott (48m 55s): If it's possible that I'll ever be able to get G Voke in a vial for home use to just keep and administer as I need
Ken Johnson (49m 4s): What we would like to pursue that. Yes, I think, you know, there are a number of applications of Glucagon that are different than our are approved used today. It's a one milligram, you deliver the whole dose, a in the setting of restoring very low blood sugar, but there are other settings where maybe the smaller dose would be useful. And, and so there or other settings, whether it's exercise, whether it's hypoglycemia, unawareness, other things were, there are a series of, you know, Clinical Development projects that we've sponsored. We've collaborated with one side as well as a part of a dual hormone delivery with Insulin and Glucagon as part of a closed loop system.
Ken Johnson (49m 45s): So in a, none of these are approved, none of them are a possible with the current configuration. We would need a vile of Glucagon as you describe the Scott. So it'd be very similar to how you would administer Insulin. He would have personalized doses for the situation that your trying to manage. So that's gonna take us some time, but we are investing in those efforts, you know, just ask everybody to stay tuned for more.
Scott (50m 10s): All right, well, I'll say this from my heart and many people may or may not understand this. And I guess if you've been around Diabetes long enough, if it makes sense, but it may not seem super exciting that someone figured out a way to make Glucagon liquid stable, but is super exciting and that it opens many doorways and possibilities for the future. Everyone who has someone that they love with type one diabetes or has type one diabetes, should be incredibly jacked up and excited that you guys figured this out. And I know that it, it's hard to wrap your head around why this is that exciting, but it is. And I'm, I'm very much looking forward to what happens next. So I really appreciate you coming on and explaining all of this.
Scott (50m 52s): And I thank you for your time, unless you want to play some piano. I think we're good.
Ken Johnson (50m 57s): My pleasure. Scott I enjoyed it and hopefully we can do it again sometime. And my best to Bailey you left the room,
Scott (51m 8s): Dammit, cameo bark. So you'll have to cut that part. So I thought I could get a little park at the end and we'd be finished anyway. Thanks so much. Enjoy the rest of your day. Really appreciate your time. All right. Appreciate it by huge. Thanks to G vote for sponsoring this episode and for giving me the opportunity to just speak with Ken and a huge thank you to Jenny Smith for being such a good friend and coming on the show to talk about Gvoke. If you'd like to find out more about you Vogue, there are links right here in the show notes of your podcast player@juiceboxpodcast.com or you can just type the words
Scott (52m 1s): I have a little bonus stuff here at the end for you. If you'd like to keep listening, I actually spoke to Ken the day before we recorded this just for a few minutes, so we could get to know each other. And he told me about his piano playing. So I brought it up at the beginning of this recording while we were getting the audio set up. So it was recorded, but not really a part of the episode, but I left it here. Cause it's interesting. What kind of music do you apply? So,
Ken Johnson (52m 28s): Oh, I'm like what they prefer to, I guess, as a professional journeymen, sidemen I'll play whatever, whatever comes on my way, I read music, you know, I play from classical to jazz, to tribute acts, including pink Floyd and van Morrison and a REIT, the Franklin and two classic wedding bans. You know, the most cliche kind of lounge music. You can imagine it doesn't really matter a musical theater,
Scott (52m 55s): The multiple instruments or not.
Ken Johnson (52m 58s): I'm a piano player, keyboard player.
Scott (52m 59s): That's really, that's an amazing skill to have. That is very cool. And it's great that you get to do it too.
Ken Johnson (53m 5s): Yeah. So Chicago, you know, traditionally has been famous for lots and lots of live music. And of course, many famous bands have come outta here, but we're a complete shutdown now. It's just awful.
Scott (53m 18s): And online really doesn't replicate it. There's been, I think one or two people who have done it well, you know, and it's, you know, you have to, you can see how much money you have to have a, in a crazy example is that, I don't know if you saw, you may not like this kind of music, but maybe you do. You mentioned pink. Floyd Metallica did an old song acoustically remotely. So all four guys were in a different place, but it sounds like it was recorded in a studio. So you have to assume that each one of them has a professional recording studio in their home, you know, but that worked out, but,
Ken Johnson (53m 51s): And that's exactly how they do it. And what we are led to understand as consumers is they record all those tracks independent of each other, and then somebody who mixes them because you can't, you can't use zoom to have simultaneous music because whoever's talking to the loudest takes over the channel. And so there's, there's no mixing up on zoom. It's a, it's a big problem.
Scott (54m 12s): You know, all that equipment and the willingness to spend a couple of million dollars to mix a song together to release it. And they had that money and they did it. And everyone else is just like you said, fumbling through trying to do in a resume for those of you who are not familiar with a podcast and don't know who Jenny Smith Is I thought I'd take a second to let you know Jenny is a frequent guest of the show. She's helped me put together series within the Podcast like defining Diabetes, ask Scott and Jenny. And of course, the very popular Diabetes pro tip episodes and of all of the people I could have had on those episodes with me. Here's why I picked Jenny. Jennifer Smith has had type one diabetes for over 30 years since she was a child.
Scott (54m 53s): She holds a bachelor's degree in human nutrition and biology from the university of Wisconsin. She is a registered and licensed dietician, a certified diabetes educator, and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. I love Jenny. She is a friend. And when I decided to do this episode, I asked her if she could help out a little bit and she was very gracious and said, yes, Jenny works, has integrated Diabetes so you can check her out. If you do, like@integrateddiabetes.com.
Please support the sponsors when you’re able and it makes sense for you. This episode was sponsored by Gvoke.
LEARN MORE about the HypoPen and other Gvoke products HERE
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#384 After Dark: Bipolar Disorder
ADULT TOPIC WARNING
Jonathan offers a raw look into his life with mental illness and Type 1 diabetes during this interview with Scott, which gives a 90-minute glimpse into the complications of living with poor mental and physical health. Jonathan shares his family history, stories of multiple suicide attempts and surviving DKA. He is a thoughtful young adult who calmly discusses his past and the turning point for choosing to live a healthier life with T1D.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:13
Hello friends and welcome to Episode 384 of the Juicebox Podcast. This episode is also the eighth in the after dark series. I call them after dark because they're topics that don't normally see the light of day. we've tackled drinking, weed, smoking, trauma, addiction, sex from both the female and male perspective, depression and self harm, divorce and co parenting. And today's episode is with Jonathan. Jonathan, among other things, has bipolar disorder, ADHD and depression. He also has type one diabetes. He's been in decay a number of times, and has had a couple of failed suicide attempts. Jonathan's life is going in a different direction now, and he was looking for some conversation about it. And that led to this episode. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan. If you're concerned that the topics I've mentioned may bother you, this probably isn't the episode for you. And it very, very likely is not for your child to listen to, at least not alone. I want to thank the sponsors of this episode. dex comm makers of the G six continuous glucose monitor and Omni pod makers of the tubeless insulin pump that my daughter has been using forever and ever and ever. You can get a free no obligation demo of the Omni pod tubeless insulin pump at my Omni pod.com Ford slash juice box Podcast learn more about the Dexcom g six and even to get started. You can go to dexcom.com Ford slash juicebox. There are links in the show notes right there in your podcast player. And at Juicebox podcast.com. When you click the links, you're supporting the show. There are a few little electronic noises in the first number of minutes of the show but we get them worked out.
Jonathan 2:10
I am Jonathan. A lot of people call me john the diabetic kind of grew on that name. I have type one diabetes.
Scott Benner 2:20
JOHN, where do you get john the diabetic from? Is this a girl standing around one day and it comes up? Or how does that happen?
Jonathan 2:28
Um, it was one day with me and my friends were at the bowling alley. And I town a little town I use a little bit and I don't remember exactly what went on. But I did something funny. I remember what it was something to do with a pool table. But they sorry life and stuff I said yes. It's me, john the diabetic and ever since then. It's just been john the diabetic
Scott Benner 3:05
is listen, there's a little bit of an electrical noise behind you. Are you talking to me with your cell phone or with a computer?
Jonathan 3:14
with myself, your cell phone?
Scott Benner 3:15
Okay. It's no big deal. I was just I was wondering if we could move your cell phone away for theater. But if that's Are you near anything else or no? Like electronic?
Jonathan 3:25
No, cool. Okay.
Scott Benner 3:26
All right. So am I to infer that whatever thing you did was silly. And you were you blaming you're like you're like my blood sugar's low or you know how I get it? Was that kind of the vibe? I'm backing up in the in the bowling alley.
Jonathan 3:46
We're sort of talking about the name or Yeah, yeah, I was
Scott Benner 3:50
just wondering like when you responded, you know, um, you know, it's me. I'm john, the diabetic was that because do you do a lot of were you doing a lot of things that were attributed to your diabetes or you just pulled it out of your ass?
Jonathan 4:03
I just pulled it out of my head.
Okay, gotcha. Gotcha. Okay.
Well, listen, you don't worry. I thought I thought it was funny. I thought it was funny. Like I ever since I became a diabetic, I've always made it a fun thing. So I weigh when it bring me down. Personally, I see. Because I've met other diabetics that are way worse than me. Like, they would let the diabetes bring them down and stuff. So I decided not to do that.
Scott Benner 4:40
Yeah, just not to be sad about it and those sorts of things. I hear you. Okay, so So how old were you when you were diagnosed?
Jonathan 4:51
I was 12 years old. November the 11th of 2012. I got diagnosed 2012 Okay. November, which is kind of a big deal for me on that day because November the 11th of 2011. My grandma had passed away from type one diabetes. So and how old is your toll on me is
Scott Benner 5:21
doing now I was just gonna ask you How old was your? Did your grandmother have type one her entire life?
Jonathan 5:28
Yes, she did. Okay. And I believe she was 62 when she passed. Okay.
Scott Benner 5:34
All right. So she passed from like, I mean, you were young back then. Do you even know? Is it complicated? Do they call it complications of type one? Or did she have something specific, like a heart attack? Or what do you remember happened?
Jonathan 5:47
My My mom told me that it was complications of heart of her heart. She said her heart gave out. I don't exactly know what happened. But my mom's mom says is because her heart gave out now. I don't know. If I believe you know, yeah, sure. I don't know if it was because of that. We're the type one diabetes, but it's very possible that my mom told me it was just because her heart.
Scott Benner 6:24
Yeah. To keep me like, not upset about it, I guess. Oh, I see. Not the thing that maybe the diabetes is what what would help her under life early? And I say maybe your mom was protecting you. But no, I mean, now you know, you're older, the type one. If it's, you know, it could affect your, you know, her heart. And you could end up having a heart attack. But the heart attack might be facilitated by, you know, her blood sugar's being maybe out of whack or high throughout her life. But I'm so sorry. I'm sorry to hear I know, it's a long time ago, but I'm sorry to know that I am even more kind of amazed, as I'm sure you probably were on that day. That one one exact years later, you're diagnosed. You know,
Jonathan 7:08
it took a big toll on me. I was depressed from that day. On to, I want to say, three months ago, two months ago, I think I finally made out of depression. And no, it was a big toll on me really was Tell me
Scott Benner 7:29
tell me how old you are now.
Jonathan 7:32
I am 20. You're 2020 and a half.
Scott Benner 7:35
So through your entire sort of adolescence. You just you you were were you clinically depressed? Were they giving you retaking medication for it?
Jonathan 7:43
No, I was not taking medication for it. I I never did like to go to a therapist or anything or doctors or anything. I was just kind of I don't know what you call people like this. But I guess you'd say I'm one of those people that just deals with stuff by themselves. I guess. Yeah, you
Scott Benner 8:10
kind of just internalized it all and tried to work through it. And how did you? I mean, what were some of the things you did to try to work? It's interesting, right? Like it from 12 years old till till 20 What were some of the things you tried to do to help yourself?
Jonathan 8:24
One was smoking marijuana. I was one that, uh, that kind of helped. Actually. I smoked since this last May though. I kind of gave up on it. But smoking? Well, when I was a kid from like 12 to 16 I was taking this medication called Depakote because I was originally put on it for my anger issues when I was a little kid. Okay, that kind of like, helped a little bit because it's a mood stabilizer and
Scott Benner 9:01
around that around the Depakote was that prior to the diabetes diagnosis.
Jonathan 9:08
That was actually that was actually before I got put on that in 2009. Okay. And I was taking it from 2009 to, I want to say 2016 because 2015 I started having seizures really bad. And the doctor that put me on it told me that TEPCO helps with seizures too. But I found out that Depakote actually causes seizures as well. It depends on I guess he said, or I looked up on a documentary and stuff about it is depending on how much milligrams of it you take, depends on the outcome pretty much. Then we take in 1500 milligrams of Depakote a day What? Because I used to have seizures, right? And when 2016 hit, I was having seizures like every once a month, every two months, something like that, you know? And I finally just quit taking it. And I switched over to marijuana.
Scott Benner 10:18
Well, so I'm looking here because you're talking about things i don't i don't know about and it is it's very interesting. Depakote is an you know, an anticonvulsant. So it's prescribed for seizures. It's also prescribed for bipolar disorder, but doesn't an end can also help prevent migraines, it says, seems like it has a couple of different uses. And you were given it specifically for the seizures
Jonathan 10:44
specific. I was actually given it for the bipolar and ADHD. And then like a year later, we found out I helpless seizures. And so I stayed on it because I had seizures growing up. Gotcha. Like, are you are having lost five oh my god, I had one when I was 10 had one when I was 15. And then as soon as I turned 16 I just had them like every month, every two months. And all that became more frequent. Okay.
Scott Benner 11:15
Have you been diagnosed with bipolar disorder?
Jonathan 11:18
Yes, I have. Okay. I've been diagnosed with bipolar, ADHD, a DD and ADHD I, which I don't know if you know what that is not too many people do. I don't
Scott Benner 11:31
jump out when to do for me, can you tell me about it?
Jonathan 11:34
What it is, is you do stuff on impulse. You do stuff without thinking. And that does not make I could tell you right now that does not mix well with bipolar ADHD at all. I don't think it's a thing. But the doctor told me that it was. I don't know.
Scott Benner 11:57
Okay. All right. So I'm gonna ask you a question in a second. But before I do, I want to real quick disconnect the zoom and reconnect it just to see if I can get the noise out of it. Okay, and so I'm literally gonna hang up on and and reopen it right away. So you can click back into the link in like, 20 seconds. All right. Cool. So hopefully, this will do something. If it doesn't, I'm gonna live with it. I just wanted to it was worth a shot. You know what I mean? Right, right. Okay. So all right. I, I'd like if you can you explain to me how bipolar affects your life? Like, what is it? How does it kind of ebbs and flows? Am I right, you have different kind of segments of experiences.
Jonathan 12:37
So for example, when I was five years old, is I was in kindergarten, it was pajama day. My mom doesn't believe in wear pajamas to school, I wore my pajamas, and she told me Get ready for school. I told her I was ready. She said I wasn't gonna go to school in pajamas. So I went to the bus stop anyway, as she picked me up, took me home and said, You're not going to school and unless you get real closer. So I went to my room, and I had a metal bed frame. And I just bang my head on it, like bang my head on it. And because the bipolar that at that time, the bipolar took over, um, and my head was bleeding, and pretty bad. Because of it. She ran in there, it was like, What the heck, john, what the heck. And she took me to the ER, so cuz it was bleeding back. But that's the worst incident I've had because of that. I've had my moments where I would just flip out for no reason, or something. But, uh, over the years, I started to learn how to control it. I had a anger breakthrough, I guess you would say, in the last year and a half, two years, maybe. Okay. Which I'm really surprised. I mean, I still have my moments where I want to just hit on a wall or something or destroy something, you know, but I keep I keep calm about it. And I learned how to control it.
Scott Benner 14:34
Do you experience sort of the classic signs of like, you know, kind of high energy make like the mania where you don't really need to sleep and you kind of lose touch with reality. And then is there a depressive side of it? Where you're kind of more low energy. Does that sound familiar to you? Or does it not?
Jonathan 14:51
Yes. I have that a lot. Actually. I didn't even know that was a thing actually. But um, Yes, um, so like, some days I'll wake up, and I just, I just have those mornings where like, I don't want to do anything. I don't have the energy for anything. All I do asleep.
Scott Benner 15:23
Can those times go on for like long periods like weeks and months?
Jonathan 15:27
Yes, yes. Okay. I think last month, last month was pretty bad about that. I mean, I went to work and stuff, but I would go to work from three to 10, because I closed but I would go to work for like, five days a week. And then after, as soon as I will get off, I would go straight to bed and asleep to one or two. Get up, stay in my bed. And then 30 minutes before I had work, I would go to work. And then repeat. You just you just
Scott Benner 16:06
having to do it out of necessity. You need the money, you need the job. So you're forcing yourself to
Jonathan 16:11
do it. Yeah. Okay.
Scott Benner 16:12
And so, do you see a doctor for the bipolar?
Jonathan 16:17
No, um, I, the last time I seen a doctor for any of that was, I think I was eight. Or no, I was nine. Yeah, I was nine. I'm always seeing him for a year and a half. After that. I told my mom, I never wanted to go see another one. Um, I don't know why I'm like that. I just don't like talking to the therapists or doctors about that stuff. Like to figure it out on my own, which I probably should go see a doctor for it. I probably should. Well,
Scott Benner 16:56
yeah, I mean, I know someone who, who has bipolar. And it took them a fair amount of time, like, I'm not gonna lie to you, they didn't walk into a doctor's office didn't just come out with the answer, but they found a good doctor and have had like real, like real breakthroughs with with medication. It's funny, as you're saying, if they have ADHD, as well, this person I'm talking about, I don't see them getting angry, or, or they don't hurt themselves, like banging their head on things or anything like that. But they do get really kind of internal sometimes, you know, and you don't see them for long periods. When they come back, they kind of look like they haven't kept themselves up for a while, like just, you know, like, visually hair, nails, like things like that, you know, like, learn little things. Yeah, I mean, do you have healthcare?
Jonathan 17:50
loans? Yes. I had a Medicaid for when I was a kid. I had that too. I was a teen or just turned 19. And they finally dropped it. And then I got put on in home health care, home health care. And I was only on that for about six months, and then they dropped that. Why they never told me. Um, I was 19 and a half. And I had no insurance, no way to get my insulin and no way to get my diabetic supplies. I was bouncing from job to job at the time. Okay. And because I was I was so depressed. I didn't want to work. But same time, I just, I just worked for like a week just to get a check so that I can go get the stuff I need. Yeah. And that was a hard time in my life.
One of the hard times anyway, but
I started going to Walmart because they have this insulin called 7030. And I don't know if you know what that is.
Scott Benner 19:10
I know Walmart has a cheaper insulin, that it's very it's for
Jonathan 19:13
a rehash it costs $23 and stuff. Yeah. But I was buying that and using that what it is, is the long lysine short lysine insulin mixed. And that insulin I didn't know how to use properly because I could I didn't see no doctors because I had no insurance and I didn't want to see a doctor and not have insurance
Scott Benner 19:42
because then build up adds up. Yeah, no kidding.
Jonathan 19:48
So I didn't see a doctor for almost two years.
I was just doing the stuff on my own everything. I kept up pretty with it. Pretty good. I did do that. And then I moved to another town, which is where my mom lives now. It was just like two hours from where I was living. But I went, I came up here and I set up a doctor and stuff because I figured it's time to start taking action because I started feeling really crappy every day. I'm just not enough energy film week, all the time. All that you know, so I set up a doctor, and they got me a Medicaid and all that. Now I'm getting insolate and stuff. I'll have to pay for it now, um, which is a relief. I have a doctor now. I'm taking care of myself better now. Good for you. I just started seeing the doctor. I want to say June this recent June. Oh, that's it. It's recently Yeah,
Scott Benner 21:09
I for people listening it. That's just two months ago, when we're talking now.
Jonathan 21:14
Back in January, I think at the end of January, I went into DK diabetic ketoacidosis. Um, it was the worst feeling I've ever felt in my life. It felt like the devils inside of me just tears ripping me apart. My chest was burning. It felt like my chest was getting torn apart. I couldn't breathe. My shoulders and arms. I couldn't lift them because they hurt so bad. And my buddy Mikey, we're going to the store and I felt like that and one of the workers at Walmart. He was a diabetic. And he said, he seen a job down to the ground. He asked me if I was okay. I see my diabetic tattoo on my arm. And he said, What are you feeling? I told him, and he said, You need to go to the hospital now. And I was like, What do you mean, what's going on? And he's like, I'm a diabetic, too. And you need to go now. And so he picks me up over shoulders. And him on my body got in my buddy's car and put me in there. And this worker just walked off his shift to save me as I thought that was the most
crazy thing ever.
Scott Benner 22:49
Jonathan, I gotta tell you, it's made me cry a little bit. So yeah, yeah, that's really something.
Jonathan 22:55
So as we went to the ER, and when we got there, they're like, what's going on? I told him, I need to see a doctor now. I feel like I'm dying. And they they got me back there. There was 10 people in the waiting room. I felt so bad for two. There's 10 people before me, but they put me before them. 10 people, I felt so bad for it. But they said you're you're about to die. You were number one at that moment in time. And I thank them for it. But I still feel bad points.
Scott Benner 23:32
That's just how that works. Man. That's, that's there's nothing wrong with that.
Jonathan 23:35
I was in the hospital for two days for that. And they had me stuck up to IVs or all that, you know, procedures.
And then they finally let me out.
Scott Benner 23:50
Is that sort of the moment that brought you to like, I'm gonna, like pay closer attention to my type one or like you're even talking about kind of feeling like you snapped out of some depression at that point, too. What do you think happened?
Jonathan 24:03
I was I mean, I've been close to death more than once. But that right there. That that got to me. It made me open my eyes and made me more alive than what I was. I guess you would say, Okay, I'm
I'm tearing up right now. I am just Geez.
But it It made me open my eyes to reality. And I was like I need I need to start doing this. I need to start taking care of myself because I had a cousin. His name was he had type one diabetes and he has seizures too. And he died at age 26. I believe because he didn't Take care of himself properly, like I wasn't.
And
I started to check my blood sugars and stuff because I never really checked my blood sugar since I want to say since I was 16
I think a lot of that had to do with marijuana.
Scott Benner 25:20
But how so you just kind of you just felt so chilled. You didn't care?
Jonathan 25:26
Or Yep, yep. And that's why I kind of gave up on it back in this last night because I, I I finally realized that when I'm high on marijuana, I don't care about anything, not even myself. I just chill and, and do whatever. And I realize I can't do that. I cannot do that. Yeah. It takes a level of you have to be interested in your diabetes, that's for sure. Yes, yes. And I've learned a lot this year. This year was the most I've learned about my self and my diabetes and anytime in my life.
Scott Benner 26:11
We had a lockout you have a lot going on, man. I'm Are you you're back closer to your mom now. Is that right? Yes.
Jonathan 26:18
actually moved up to so I was living in a town name. And last year, when my son's mother broke it off, which was August 26. Was x today's officially used it's me and her husband split. Which That's ironic, too. I moved up here, the 27th of august of 2019.
Which is close to
and march 12. Yeah, March 12. I went back down to for my son's birth. And I got stuck down there for a couple months. And in this last May, I came back up to to my mom's and
I've been living up here since
Scott Benner 27:16
then. Your boy is five months old. Now. This coming? 12th he will be six months six. He'll be six months really soon. Well, congratulations. Thank you. Yeah, he's healthy. Everything's good.
Jonathan 27:27
Yes, he's very healthy. Um, he he looks a lot like me. I can't I cannot believe how much he looked like me.
Strange, isn't it? Right?
Scott Benner 27:38
Yeah. Wait, it'll 20 years from now. And he's saying to you that you're just like, Ah, that's something I would have said to my mom. Right. But we want to get we want to get you to 20 years from now, Jonathan. Right. Right. Sounds like you want to be there too. So, you know, listen, I, it's hard for me not to think while we're talking that you are discussing health and life issues with me. And, and when you're talking about them, I feel like you have the problems of you know, somebody in their mid 30s. And at the same time, you're the same age as my son who, you know, we almost don't let be in charge of anything. So, yeah, he's got very limited, um, you know, he goes to school, and he, and he takes care of his, you know, his physical self on his own, he has friends and but we're not putting he's not in charge of understanding bipolar disorder. All the ABS and ages and all that you have, and, you know, hasn't tried to manage a serious health condition with marijuana. And, and, you know, have type one diabetes, you have a lot going on man, like you need. I think you found some grounded points, which is, is great, but I think you really need some support from people who can kind of help guide you a little bit. So let's start with is your mom that person? Or is she not the kind of person we put in charge of something like this?
Jonathan 29:02
Um, she could be somebody that we could put in charge for that. Good, but Me, me and my mom have a lot of issues that we don't talk about. So I, I involve her? Not as much as I probably should. But I pretty much just do it on my own. Yeah.
Scott Benner 29:28
Well, I think that I listen involving your mom creates different problems. You know, we can't just trade one issue for the other. That's not gonna. It's not really gonna help you at all. How did you find me? Like, why are we talking right now? How
Jonathan 29:42
did that happen? I'm actually, uh, I got on Pandora. And I was sorry. I was looking at podcasts. And I came across juice box. I didn't know what it was at all. So I listened to one of them. I don't remember what episode it was. I think is in the three hundreds. But it was the self hormone. But where that chick was talking about self harm and stuff, yeah. I listened to that. And that made me cry that that that made me cry. Um, and at the end of the podcast, well, I listened to a couple of them. I don't remember which one it was, but at the end of one of them said, If you said, if you have type one diabetes or know of somebody with Type One Diabetes, I would like to have an interview or talk to them or something you just reached out. I went on to, I found and I actually typed in your name on Facebook, because I found out your name was Scott Benner. And I went to see if you're on Facebook, and he was, and that's when I swung you that first time.
Scott Benner 30:56
That's right. You messaged me on Facebook. That's right. Well, so did listening to her talk about her issues. Did you feel like some commonality with it? Did you have similar feelings? Or no?
Jonathan 31:09
I felt what she was going through. I mean, I never I never.
I'm not trying to put her business out there.
Scott Benner 31:17
They she, she already did it. It's okay. It's enough as such, she knows. But
Jonathan 31:22
I mean, I have a, I've never cut myself. I never, I couldn't say self harm myself. But I never did those things. Okay. Because I have tried to sell for myself, just not in those type of way. But I understood what she was going through. Me and her go through different things, as I can tell, but I can relate to what she's going to they're going through. And that that hit me really hard. And
Scott Benner 32:03
I think it hit everybody pretty hard. Jonathan, to be honest with you. I think that everybody that heard it felt that way too. But you have more of a maybe you have a little more of a connection to the, to the feeling then than some others do.
Jonathan 32:15
Yes. And
I, I felt the way she was talking to you, and how comfortable she felt talking to you. And so, and I, and you seemed like a pretty understanding guy and stuff, you know. So I was like, maybe, maybe this can help a little bit. Cool.
Scott Benner 32:40
Well, I hope again, I i think i think we're on our way to under I think I understand, you know the the basic overview of your situation. I did want to ask though, just a second ago, you said you you've tried to hurt yourself, but not in that way. What have you done? Alright, let's take a little break. I'll tell you a little bit about the Omni pod tubeless insulin pump. It is just that an insulin pump with no tubing. Be clear about what that means. There's no infusion site on your body that leads to a thing that you have to carry a controller or you know the thing holding the insolent. Sometimes you'll see people's tubing run all through their clothing. And you know, they've got to hang this thing on their belt. None of that happens with the Omni pod. The Omni pod is one device, it is self contained. It goes right on the body, and the insulin is right there with it. So there's no tubing or controller to lead back to. How could that be. Because the controller you'll use for the Omni pod is wireless. It just goes in your pocket or in your bag. But it's not connected to you, you're not gonna have to stuff it in your bra. Wear down your shorts are in your pocket or in your sock. You can just you know, carry it the way you carry things. be normal. I love the Omni pod tubeless insulin pump for my daughter because she can bathe with it, swim with it and be active with it constantly getting the basal insulin that she needs. There's no disconnecting for soccer, softball, working out at the gym, you're always getting the insulin the way you're meant to. It's a huge thing. Too many times we talk ourselves into believing it's okay to disconnect for an hour or two I have to because you know I'm doing something active but that's really not the way to go. And with the Omni pod, you don't have to, you don't even have to take my word for how this works. Because on the pod, we'll send you a free, no obligation demo right in the mail. All you have to do is go to my Omni pod.com forward slash juice box fill in a tiny bit of information about yourself and the pod experience kit will show up right at your door. You can try it on and wear it. Go take that swim. See what you think. And if you don't like it doesn't matter because there's no obligation It didn't cost you a cent. I'm going to tell you about something that just happened here in the house. Arden had to change her pump. So she changed her pump. She's zoom learning right now, you know, she's doing the school online. And she's in a room by herself kind of quietly and I was trying not to bother. And her blood sugar started to go up at the site change. So we weren't able to make an adjustment to it until right around 190 blood sugar. So the new pods on right we're bolusing trying to get it down, but she kind of ends up leveling out at 200. Now she's done school and she's hungry. She wants soup with crackers. She's gonna have a couple of potato chips. She tells me this is like 70 carbs, but her blood sugar's 200. What do I do? She's hungry right now she doesn't eat normally. I'm able to make a bolus for the correction plus the food a full bolus on top of that 200 blood sugar. And then watch as Arden's blood sugar comes down right there on her Dexcom g sex at the exact right time I give her the food. I'm gonna catch the drop of the insulin with the food and level are out. And I can do that because I can see her blood sugar. That's just one way I use the Dexcom g six continuous glucose monitor. There's plenty of other ways. That is just one way I use it. I'm looking right now at her blood sugar's 115. And still diagnol down and it's indicating that it's falling still slightly. But I love that because I gave Arden her food at 150. This is going to level out. It's going to be amazing. Head to dexcom.com Ford slash juice box to find out more about the Dexcom g six you can learn about no finger sticks about direction arrows alarms to tell you when you're leaving ranges that you set. And the share feature which allows people with an Android or iPhone to follow a loved one with Type One Diabetes. And look at this Arden's blood sugar still indicating diagonal down but it's now at 119 which means we are leveling off. Her foods been going in for about the last 20 minutes. But the insulin has been active for over 45 minutes. That is not something I could have done blindly. I needed the Dexcom g six for that. And you know I made that Bolus with an omni pod, right. Alright, let's get back to Jonathan. links in the show notes at Juicebox podcast.com. For these and all of the sponsors. Just a second ago you said you you've tried to hurt yourself, but not in that way. What have you done?
Jonathan 37:29
Um, uh, I, I this is gonna be hard.
I was living in
the town I was living in, I got so depressed that my mom don't even know this. And I don't know if I have the heart to tell her this way. It happened back in 20s, the beginning of 2017 I do believe. But I tried to hang myself. Um, and it obviously didn't work. The knot somehow got untied when I kicked the little milk crate out from underneath me. And while there's a couple milk crates, but that I was hanging there for a minute, and I thought it was gonna hold. And then finally I just dropped down to the ground. I was like, it ain't my time. It's not my time. And it it was another year from that 2018 sometime in 2018. My brother he had a 12 gauge shotgun. And
I loaded a
bullet in it. And
I pulled the trigger. And that was when I was on all all the narcotics and jugs and stuff. But I I pulled the trigger, but it clicked. And it was it was a good show. There was nothing wrong with the gun the gun wasn't dirty, nothing. But all it did was just click and that that that time I officially knew it wasn't my time
because that gun should have went off
and it did it and I think the higher power for not going off. But when as soon as I pulled that trigger. A second later, my brother walked in He, he, he flipped out. He, he did he vow he about dropped to the ground and didn't know what to do or say. But that those are the times I I tried to self harm myself on that the other time was when I got on Tinder kardex and a jobs really bad. The worst drug I did was a meth.
I never did heroin.
But I was on meth really bad. And the only reason was, is because I was so depressed. I was trying to give up on life. And I thought figured that would be a not a good way, but a way to go out, I guess. Um, since the gun thing didn't work. Um
Scott Benner 41:11
Hey, man, take your time. Listen, you're doing great. First. Don't be sorry. You kidding me? You just said more difficult things in three minutes than I've ever admitted to in my entire life. So I'm, you're doing a terrific job. What I wanted to say was, is that so at the time of the of your first your first attempt, I guess is is with the rope. Were you using then?
Jonathan 41:37
No, no, not that was probably.
That was probably six months before I start using.
Scott Benner 41:44
So that was just a depressed moment in.
Jonathan 41:47
Yeah, that was just a depressing moment.
Luckily, it did it. That not came on time. Luckily, yeah, not came on time. Well, no,
Scott Benner 42:00
but let me let me let me say this man, if you if you're bipolar, and you're experiencing waves of depression, and then waves of, you know, they call it mania sometimes, but there's also normal times too. there's times where you're just you're not, you know, you're not like, full of energy and running around. And you're also not depressed, where you just kind of feel like it's what normal would feel like, do you feel like you feel normal right now? Yes, yes. So I'm thinking man, I'm not with you. And I'm never gonna be able to be with you. We obviously don't live anywhere near each other. But in this moment of normalcy for you, like I think you have to get to someone that can help you manage the bipolar piece, because everything else tumbles around that from your description, right? Like when you're when you're feeling depressed, you can feel suicidal, you can stop taking care of your blood sugar's you can, you know, there's all these are the things that are happening, but if you could get on a good, a good plan, and God knows I'm not the right one to tell you about it. But But my my limited experience with this would be that there are medications that can help take the craziness out of the highs, like you know, cut a little bit of the highs and take the Depression of the lows, and allow you to find the the middle more often. And I don't know that you won't struggle still as you're figuring it out. But at the very least you won't, you won't try to hurt yourself, you know, what would be the goal, I think Does your mom have this to
Jonathan 43:39
do what
Scott Benner 43:39
does anyone else in your family have bipolar?
Jonathan 43:42
Um, my mom does, it runs really bad in my family. And my sister, she has bipolar. She just got diagnosed with schizophrenia, too. And personality, or a
split personality, okay, or
Scott Benner 44:03
what? Listen, you're gonna you you need to worry about yourself and you need to be the unit, you need to be the first person in your family to, to address this head on and try to put an end to it. Because Do you could find an answer that could end up helping someone else in your family one day. I mean, I hope your son never suffers like this. But imagine, imagine if he does, and you you already know how to help him. Right? Because that's where you're stuck right now is you have so many people stacked up in front of you, who are supposed to be your support system who are already suffering the way you are, and through no fault of their own. They can't help you either. They've got their own struggle, but but maybe you can find an answer. And maybe you could help yourself first and then and then maybe be maybe you could be the person that helps other people. You know, I think that's a really that's a really decent goal to have, you know, for yourself personally, but then, you know, answers. I know it sounds silly, but, you know, I, I have like, you know, health problems that are, of course, nowhere near the ones you're describing. But I sometimes think that I work at them as hard as I do. As much for my kids in case they get those problems as I do for myself, like, I want to find the answer. So they don't waste their life looking for one if that makes sense. Right? You know, I and in your Listen, you found a good spot here, you had some things happen to you that that kind of shook you and are making you think of things differently. I think while you're thinking of things differently, and you're, you're you're working on things, this is the time to, to try to like take a big swing and figure something out. You know what I mean? Yes, yeah. How are you doing with your blood sugar's and everything like, how's that going?
Jonathan 45:52
Um, so like I said, I haven't really checked my blood sugar's since I was 16. Until
this reset.
is, right. Yeah.
Scott Benner 46:07
But But how's it? I'm just talking about those couple months. Like, how are you doing?
Jonathan 46:13
Um, I'm doing a lot better. I mean, the first month was kind of touchy. My blood sugar's were always high, a lot. run from 250 to 500. And then finally, like, I'm, like, second month, the second month, I, they started running about, I want to say 172.
To two ad 300. And that's
Scott Benner 46:51
way better than Yeah,
Jonathan 46:53
yeah. And then this last month, this last month, it's been, it's been staying in the hundreds every now and then it will be up above 200. But a bit up above 300. Looking at you for this last month.
Scott Benner 47:10
First of all, congratulations. That's really well done. And thank you, you know, you're very welcome. And is it? Is it helping you feel better? I mean, it has to be helping you feel better, right?
Jonathan 47:22
Yes, yes. I'm not feeling drowsy all the time. Not feeling weak anymore. I've I've actually been going out at night, and after work or something, and walk this trail we got down in the cold, bro. It goes to six, seven different towns and cities here, but oh, I'll just walk through one. That's the town I'm in. I walked out for about three, four hours every night with a friend of mine. And I think that's been helping me a lot of I've been in a lot more healthy to for you. I've been eating a lot of salads, a lot of eggs, protein. And I've been eating a lot of meat. And now I feel really feel healthier. That's excellent. I really do. This all came just from your dk scarin. Walmart.
I'm somewhat
somewhat, I had two more decades after the one in January. I had one in I want to say April. Yeah, it was April. It was two weeks before my birthday. I had one I was down in the town I used to live in at that time. Um, I I was throwing up and my little brother when I say I my brothers, they're not actually my blood brothers. It's just
really good friend boys. Yeah,
yeah. But anyway, one of my little brothers he asked me if I was okay and I said yeah I just don't feel good and stone off that's it. You know, I think I something bad boy. And because I literally thought I ate something bad. And I was just throwing it up. But an hour after I've sewn up, I my chest start hurting my arms and like what happened the first time started happening again.
Scott Benner 49:46
Yeah. So you knew when it was done.
Jonathan 49:49
I couldn't move. I could not move. It was much worse this time than it was the first time and I couldn't say anything. I couldn't even catch my breath. And my brother came in there an hour later stuff. When all that stuff happened, we're starting to happen. And he said, john, you're not okay. And he put me and his mom's car and carried me to his mom's car drugged me. But, uh, and he, he's only 16. He didn't have a driver's license often, but he drove me to the hospital. And the hospital took care of me. I was in there for a couple days, you know, procedures. And then this last time, the third time was, it was actually three weeks, I want to say two or three weeks before I texted you, that first message. I woke up, or I had to work the day before, but I woke up at 12 at night. I remember I threw up and I veggie burger. I never had a veggie burger. But I ate one. So I thought I'd angry my stomach. Gotcha. So I threw up, I felt Okay, after that went back to bed. Six o'clock rolled around. I was supposed to be at work by a a, or no nine. I was supposed to be at work by nine by six o'clock rolled around. And I got up and I went to the bathroom. As soon as I got done using the bathroom, I went to go to my bed to lay down for another hour. And as soon as I laid on my bed, I just threw up everywhere. After that,
excuse me. After that.
I started feeling the chest pain and stuff. And I said this ain't right. This is not right. So I banged on my mom's bedroom door said mom get up now I need to go to the hospital now. And she was like, she didn't know what was going on. And she was half asleep, you know? And I told her call 911 now tell him I need everyone. It's because I already knew what was going on. Yeah, and I was gonna play around this time, I was gonna try play with it. Um, firetruck neighborhood showed up. And I couldn't, I was trying to keep calling about it. I was learning I learned from the first two, to not overreact about it to keep calm and slow breathing. And so that's what I was doing. I was still trying to catch my breath and stuff, you know, but I was keeping calm about it. And that one wasn't as bad as the first or second one. But the second one was the worst one I've went through. Well, let's let's have only I've only had three decades. And they were all this year. Yeah,
Scott Benner 53:12
I was gonna say let's focus on the price. Never having a fourth one. That's that's a neat, that's an end goal like you're after right? So what are you doing now to stop that? I mean, you've got these incredibly you know, improved blood sugars like what is it? You're doing now? You're eating better? You you're checking your blood sugar more frequently taking your insulin?
Jonathan 53:32
Yes, I checked my blood sugar every time I or at least 15 minutes before I eat. Um, I check it an hour and a half to two hours after I eat. And then I check it every pretty much I check it probably every two to three hours because I found out my blood sugar's like to skyrocket in a matter of minutes. Yeah. So I keep on top of it now. I take 50 units of a level
every morning.
And then I take I'm on a sliding scale so whatever my blood sugar is depends on however much insulin I take. Okay,
Scott Benner 54:28
yeah, I and and are you still using the Walmart than overland? No, no, you're using 11 year now and like
Jonathan 54:37
I'm using what the doctor prescribed Great, great. My short term, which is the one I take for the science scale is no vlog. And then my long term is loving here.
Scott Benner 54:48
Gotcha. Yeah, I'm sorry Nova or Nova Lin is a mix of the two I don't know. I you know what? It's funny. The word sliding scale made me think of like an older management styles like regular and mph Your management style. Right? But that's, that's really interesting. I wonder, now are you seeing? Obviously you're seeing a doctor? Are they checking your a one sees for you when you go in? Yes, yes, I see him every three months.
Jonathan 55:14
Actually October I had October 1, I got going for my next appointment. I see him every month or every three months. Do you
Scott Benner 55:23
remember what your lack? anyone see my,
Jonathan 55:25
my last one was 8.9. Okay. The highest spines ever been? was a thing is 14.1 which is really really hot. Yeah.
Scott Benner 55:38
What do you think it might be this time? Are you hoping for something in the sevens?
Jonathan 55:44
Yes, I'm hoping at least 7.302 that's a fascinating number for that.
Scott Benner 55:51
I like that. You're focused on that. That's, that's really cool. I think you're definitely going to get a decrease. Yes. And and are you experiencing a lot of
Jonathan 55:59
like lows? I'm not really go.
My butcher doesn't like to go well. I'm a always likes to go high for some reason. I'm the lowest I have ever been. No. I was in sixth grade. I was walking and talking just just like I always do you know, huh? And, uh, it was down to 15. Wow, that's low. You didn't have a season the nurse. The nurse told me she was like, you shouldn't even be walking right now, let alone talking. I was like, when you mean stone water was also shocked. Yeah.
Scott Benner 56:42
So look, I'm a little kid, stop talking to me and help me. Right? Well, listen, if you're, you know, if you come in next time, with a seven point, you know, whatever, that's amazing. If you're not getting low, you just haven't used too much insulin. But there's more space in there for you, you know, to be slightly more aggressive and to get to where you're trying to be because listen, getting your blood sugar's lower and stable, it really is going to make you feel a ton better. And when you already have other issues that kind of mess with the way your your heads working, you don't need another thing making you feel cloudy, or, you know, confused or anything like that, like, you know, you got enough going on, you don't need another thing. So so I think managing your blood sugars is a great way of feeling better. And then, you know, I can't I mean, listen, I'm not your dad, right? But I would, if you've got insurance right now, man, I would find a psychiatrist to help you with the bipolar. You don't want to just go to a general doctor. And I'm not saying psychiatrists, like, you know, you're crazy. Like I'm not saying it like that. These are just people who really understand these drugs and specific brain issues, right? Because if you could find a course of treatment, that would keep your like I said, keep your bipolar, the highs from being too high and the lows from being too low and keep you more in the middle. That plus your blood sugar's being better, man. That's a it's a 300,000% improvement your life. You know, it sounds like you want like, I'm not wrong, right? You. You don't want to die. You're not looking at how you're trying to keep yourself going. Right? Yes, yeah. That's the way man like, like getting those those two things. More. I don't want to say under control, but but having a good understanding of them so that you can manage them better. I think those are the pathways to you doing better, being alive for a long time and finding answers for yourself and being around for your son and everything else, you know?
Jonathan 58:56
Yes. Yeah. After my son was born, I held him and stuff of these point. It that kind of helped me open my eyes more. Um, I didn't want to die anymore, that I didn't want to do crazy stuff anymore. Like jugs or whatever. Yeah. Um, I wanted because him looking me in the eye when I held him. It was a feeling that no one can ever feel until that moment, you know? Yeah, really is something isn't it? I'm sure you know what I'm talking
Unknown Speaker 59:39
about. Right? Oh.
Jonathan 59:43
I cried. I really did. And, but seeing him in my arms and stuff and smiling at me. It changed my perspective on life. Yeah, I guess I did one die anymore. I wanted to To be something I wanted to be there for him. I wanted him to remember me as he went through a lot of stuff. But Parma language, will believe it or he wouldn't have. He went through a lot of stuff. And he's still here. And he's bettered his self. Yeah.
Scott Benner 1:00:22
Imagine you have a real opportunity. He's a druggie or something, you know, no, but you have a real opportunity to set up a life for him. That's just so much better than yours. You know what I mean? And yes, and that is the that's the goal. That it really is, I genuinely think that, you know, I don't think there's much I wouldn't do for my family. And, you know, and I think that right now, the best thing you could do for yours is, is to take care of your health, so that you can start making bigger decisions so you can get, you know, jobs that aren't just like week long jobs with their jobs that you you know, can grow in and make some more money and have more stability, make sure you get health insurance for yourself. You know, stuff like that. I love that you're eating better. I like that you're getting out and exercising that you got a group of guys that that sound like they got your back. You know, you haven't you haven't been How long has it been since you used?
Jonathan 1:01:18
A used? Like heavier narcotics?
Yeah. Um, let's see, um,
it was tomorrow will be a full year since I've used the date the data, or no, actually, tonight, actually, when my son's mother broke it off with me and stuff. I felt like my heart was ripped out. And so
Scott Benner 1:01:48
is that why
Jonathan 1:01:48
wait and
Scott Benner 1:01:50
do what is that why she broke up with you?
Jonathan 1:01:54
Know, uh, because I was actually clean at that time. I was actually almost a year clean. Um, but she, she
just fell out of love with me. So
that's what she said, anyway, but,
Scott Benner 1:02:13
girls? Tough. Yeah.
Jonathan 1:02:18
But that night, I just felt like, my whole life got taken away from me. So I were in USD, that night, which was August 27 26th. of 2019. Before that, it was I think, October 2018. Somewhere in there, I was the last day I used. Now's the time I put it, put the pipe down. I never shut up. I wouldn't ever do that. But I put I put the pipe down. And side. I can't I can't do it. I regretted doing it when she broke it off. And I've never used since that day, and I never will use again. There's a simple fact. I can't I can't let my son know that. I mean, he's gonna find out visually, you know?
Scott Benner 1:03:20
I'm sure you don't want to be the one to show. I
Jonathan 1:03:22
don't want him to Yeah, I don't want him to see me.
Scott Benner 1:03:26
Go through that. You know, did you've been through a lot? Yeah, seriously, let me talk to you for a second from the time you're 12 to now is only eight years, it's half your life almost. You've been through more than most people are going to be through in their entire lives, maybe two lifetimes. And the fact that you're standing here.
Jonathan 1:03:43
Everybody says that. And it blows my mind. Because I I feel like they're there. There should be they're probably there most likely is more people out there. In my situation, you know, not the exact situation, but you know what I mean? And it just blows my mind when people tell me that, um, I, I've been told I have a metallic mindset of a 40 year old. And from many, many people, and a lot of times I don't see it, you know, but it just blows my mind when people say that it really does.
Scott Benner 1:04:25
Well, my my point is that you've got a lot of experience, you've made a lot of decisions about what's right and wrong, like you're building your own structure of, of how to live like so when no one gives it to you when you're young right? When no one tells you this is right. This is wrong. You know, gives you an example of how to work your days how to take care of your your health. You're left to figure that out on your own. And to be perfectly honest with you, a 1213 1415 year old kid is not equipped to figure that out and if that kid happens to be bipolar. They're definitely not equipped to figure that out. So here's the way I would look at you, man, somehow, against the odds, you're still here, you tried to kill yourself a couple of times, you didn't take care of your blood sugar, you decay a bunch, you use hard enough drugs, you know, you've put yourself in situations. And here you are, like you said, You're still standing here. That's, that's enough of a reason to want to keep going. And now you've got some actual experience. And you down can see, you know, these are things I want to do. And these are things I don't want to do. And what I'm saying to you is, get yourself in the care of a physician that can help you with the bipolar thing before the bipolar swings a different way, and knocks you off course, because that could last months. And then you could end up back in DK again, you could get depressed again, you could there's a lot of things that could happen. I'm saying that to me seems like, like, that's the thing to do today. Like, like, forget tomorrow, like, get done with me. Find out what insurance you have. Find a doctor near you that can help you with this and get there. And so that you can tell him the story or her the story that you just told me and and tell him Look, I don't I don't want this. Like I don't want my left to go backwards again. I'm focused. I know what I want. Please help me stay here. That that's that's I think your your next step. I mean, unless you think unless you have a plan that I'm I'm just not aware of.
Jonathan 1:06:24
Oh, no, that sounds really good.
Right? I'm like, cheered up, right? Oh,
Scott Benner 1:06:29
yeah. Like, why why? Like, like, Don't give this away, man. Like, this is a, this is a moment for you. And, you know, and and i think dive in. You know what I mean? Like, I think I think be the person who comes back on this podcast a year from now and it's like, hey, Scott, what's up? You know, I'm, I figured out the bipolar thing that's gone way better. Buy a one season the sixes. I see my son. You know, like, there's there's a lot there for you, man. There's a lot of ceiling. You know what I mean? Like there's a, there's a lot more good in front of you, then, than not like, I don't see why you wouldn't reach for it.
Jonathan 1:07:04
Right? Yeah.
Scott Benner 1:07:06
That's all. I mean, seriously, how many of these things could have taken you down? And none of them did? So. You're only 20? Man. You have no idea? Like, you're like a baby. Yeah, I you wouldn't feel that way. Because you're, you're the oldest you've ever been right now to you. You're the you know, you know, this is this is the end. But this is the beginning. And you just, there's a lot there's a lot of ahead of you that, that it sounds attainable. How? What are you interested in doing for work? Like if you if you had your head about you and you weren't getting, you know, if you weren't feeling depressed and stuff like that? Is there something you'd like to be doing?
Jonathan 1:07:44
Um, I want to, I dropped out of high school, so I never got my high school diploma. Okay, um, I wanted to go get my high school diploma or my GED, and go to college for business, carpentry and welding. And I, I really want like my my main goal is to
not my main one, but my all time goal, I guess,
is to open my own business up for a carpentry work, or welding, or both.
Scott Benner 1:08:21
Yeah. I don't see why you. Have you done those things before you go to them?
Jonathan 1:08:27
Yes, I am very good at them. I used to I, when I was 13. I built a whole house trailer, just from the frame. Well, me and this guy my mom was with. He taught me a lot on carpentry. And me, we just had the frame of old house trailer. Nothing. No walls, nothing. Just a frame. And we built a whole house trailer. on that.
Scott Benner 1:09:02
That's cool. Kind of welding GG. Can you stick and megger? What do you What have you done?
Jonathan 1:09:08
I don't know what kind of welding it is, I think is wire welding or whatever. We got a little gun and it has a wire in it. Yeah, you just pull the trigger. And
Scott Benner 1:09:19
yeah, that's MIG welding. Yeah, that's the end that's incredibly valuable to that that. Yeah. Good for you see, dude. Those are our good, solid, attainable goals. That there's nothing that you haven't said anything that you can't do. You don't I mean, like you I know. It sounds stupid. It really does. Because it doesn't feel apples to apples, though. Hold on a second, but, but I think about it, you're talking to me right now you're gonna be on a podcast that reaches you know, at this point, it's reached millions of people. And, and I just one day said to myself, I'm gonna make this thing. And I know I didn't have to learn to weld to do it. Or, you know, or or get my GED first. But I didn't know what I was doing. I just decided to do it and figured out some steps and started taking them, I started, I did something, I completed it, I moved to the next thing, I completed it, I moved to the next thing, I completed it, and eventually there was a podcast there, and no one was listening to it. And then I just decided this is the right thing to do. I'll keep doing it, it'll grow. And it grew. And it grew. And it grew. Until one day it reached a girl who was hurting herself and depressed, and her life was out of control. And now she's not like that anymore. And her story brought you here, there's no reason why you can't move forward to she just got a job she told me about recently, she's doing really well. And so all she did was go to a doctor, you know, have the balls to go to the doctor walk in there and say What's up, and you've already said it here, you know, you've got the balls to do it, and followed some good advice. And, and things got better for I don't see why you couldn't be you know, have a have an easily have a handyman service that that, you know specializes in welding and, and, and carpentry? I don't I don't see why you couldn't do that.
Jonathan 1:11:15
Um, do you know what? Home advisors? Home advisor?
Scott Benner 1:11:19
Yeah, yeah, yeah, it's like one of those websites you go to, and you're like, I'm looking to have this fixed, and it tells you people in your area, right? Yo, I'm
Jonathan 1:11:29
within the next month, my plan is within the next month, um, to get on with them. So that way I have side work.
Scott Benner 1:11:40
Yes, in Leeds.
Jonathan 1:11:42
I used to work with them.
Back in 2018. where I used to live, I didn't get any jobs because it was a small area. But, uh, and I stopped working with them because I couldn't keep pay on them and stuff. Well, listen, you also, Jonathan,
Scott Benner 1:12:04
you want to be somebody to who when they show up to work, the person who's hiring you looks and goes, I feel good about this. Like, I've had people come into my home a number of times to do things. And sometimes sometimes people show up and you're like, Alright, I feel good about this. And the guy starts working does a good job. You know, like, all right, I've also had people show up, where I'm like, Oh, this guy strung out. You know what I mean? Like, I can tell right away, and then I don't feel good about working with him again. And and so you, you make yourself, you're the face of the company, you know what I mean? Like you be somebody that when you show up people speak to you're a genuine person, you seem very good hearted. And so you show up and you're good hearted and genuine, you work hard, you do a good job. And then somebody else tells someone Hey, and I had Jonathan out, he, you know, he, I don't know, he put he put a new patio on the front of my place. For me. It's great. And he did a good job. He didn't screw around. He didn't overcharge me. And I think you should use them too. That's word of mouth, man that's putting out a good podcast, and having someone listened to it, and someone else goes and checks it out. Because somebody says, Hey, you know, I listen to this thing. And it was good. That's all you're trying to you're trying to build yourself, build your brand. And and and be somebody that people want to be around? And, and, you know, make yourself desirable to them? I don't see how I don't see that that's not possible for you. You do you know, for somebody who's been through as much as you have, you're not an asset. And you're not lost. And your thoughts are clear. And you know, you haven't, you haven't gone too far the other way, man, like, Don't Don't think of yourself as lost. Just I would if I was you, I think of myself as having just popped out of that trail and, you know, into an open field, and you have a lot of possibilities in front of you. Right? Yeah. I appreciate that. No, man, it's my pleasure. Listen, if that's not how you came off today, I wouldn't have said that to you. You know, like, you could have said some other different stuff. And I wouldn't have felt like that. But that's, that's how you appear to me. You think you are that person? Yes. Go be that person. You know, you just you just got a couple of medical things you're going to need help with everybody listening to this podcast has medical things they need help with. And, you know, there's no shame in that. And so to deal with it head on, and, you know, maybe say a lot of weird things, take the bull by the horns, you know, whatever. But, you know, just don't let it happen to you anymore. Just, you know, you do something first, you try to affect it instead of instead of waiting for something crappy to happen, and then you haven't, you know, react to it. You decide what happens next. That makes sense. Yes, john, I think we did good here today. You comfortable with all this?
Jonathan 1:14:53
Yes. Yeah.
Scott Benner 1:14:54
You You want to you want to let people hear this or would you just rather this have been a nice conversation you and I had together Well, we'll put it away.
Jonathan 1:15:02
I don't mind people listening. Cool. That's great. I think you'd hope?
Scott Benner 1:15:07
Well, I definitely think I definitely think it could. I will, I'll tell you what, when I go back, if you want, I'll be back like the names of your town. Would you want me to do that? Do one, like you said, the names of towns you've lived in before? Would you want me to take those out? Or are you okay with them being there?
Jonathan 1:15:24
Uh, you take them out? Yeah,
Scott Benner 1:15:26
I didn't want to stop you while you were doing it. Because I didn't want you to feel really self conscious while you were talking. But I'll do that. I'll be about your towns. And, but other than that, do you? How do you feel right now? Do you feel better? Does this did this make you feel bad?
Jonathan 1:15:42
It helped. It helped a lot. I'm glad I really am getting somebody else's point of view. It helped.
Scott Benner 1:15:52
That's cool. Well, listen, and now you got to find that other person in your life like can't be me, right? But you got to find someone who you look at and go, this person's got their head screwed on superstrate they know what's up. They could be, you know, a guiding figure for me for a little while, because you can't nobody can do it by themselves. You know, like, I listen, my sons had a lot of advantages in his life. And he's 20. If I if I left right now, if my wife and I were just like, he's fine, and we just abandoned him. His life would not go as well as it could. He needs guidance. Still, he's 20. They say By the way, people's brains aren't even fully formed while they're in their mid 20s. So, you know, you just need to help sometimes, and there's nothing wrong with that. You just need a little guidance from somebody who knows. And if you don't, if you're not related to somebody who can do that for you. You know, you might have to end up finding other people like that's and that's not as easy as it sounds probably. But But look for those people look for people who make sense, you know, and, and, and see if they can help you make sense to lean on people a little bit. There's, there's no shame in that whatsoever. there anything we didn't talk about man that you'd like to talk about? Um,
Jonathan 1:17:09
there was one thing Yeah. Um, I want to talk to you about uh, I used to be on a insulin pump. Is the T slim on a few? I know that one.
Scott Benner 1:17:22
I don't have it. My daughter doesn't have it. But I know a fair amount about it.
Jonathan 1:17:27
Um, I got when I first thought I was diabetic. I got put on regular shots with syringes and all that. Yeah. Or the needles.
When I was
the teen
No, yeah, I was 15 or just turning 15 something like that. Somewhere around that time.
I got my doctor.
He suggested insulin pump. Because I didn't like taking the shots every two, three hours. Okay. So he suggested this on pump. And I got put on insulin pump. And it was working pretty good. It was working really good. And then I think it was
2017
the end of 2017
it about killed me.
I was I had just filled us out. I was living out in the middle of nowhere. At my brother's and his mom. Yeah. Um, and everybody had went to work. I was there by myself. I had no phone at the time. So no way to get ahold of anybody is I've just had fill my insulin up the night before. And it took 300 units. I think it was okay. Yeah, and I filled it up and all that. Well, apparently it stopped working in the middle sometime in the middle of the night. It just stopped giving me is my guess is the screen would still turn on and stuff. Right? It just wasn't pumping insulin anymore. Well, I woke up around six or seven sometime in the morning and I felt like crap. So I didn't think any of it
my insulin pump not working.
So I ate something you know, put in my
thing, my insulin pump you know put the carbs in and all that because I used to count cards. I did all that in a calculated for me, you know, like anyway, a three, four hours went by myself and I started throwing out those. There's about
10 3011 I started throwing up.
My brother came home around 3pm and that's when he got off. When he got home the kitchen four was filled with throw up. And I started picking up blood. Yeah, because there is nothing else in my stomach.
Scott Benner 1:20:36
Urine DK because you
Jonathan 1:20:38
weren't acid just.
Yeah, I think that's what that was. No, you are
Scott Benner 1:20:43
that that's exactly what Oscar's
Jonathan 1:20:46
the doctors that told me is DK, but I'm pretty sure it was. I started throwing up blood and stuff and he could add like, I was laying on the couch. I don't remember this part my brother does. He told me what happened. But he he couldn't find me. He didn't know what's going on. So he heard me a gurgling and stuff. Because I was I was choking, choking on my own vomit and stuff. Yeah. Because I couldn't move. And he picks me up. Or turn me on to my side. What the liquid come out, you know, and I could barely breathe still. So here, we only lose like 10 minutes from the hospital. But he drove me to the hospital. He was speeding, he had two cops with red lights on following him because he was speeding. And they didn't know what was going on. Guys, er stuff. Cough charts stopping stuff, but they realized that I wasn't okay. Right. And so that they they were chill about it, you know?
But, uh,
I went in there. And they told me if I showed up an hour to an hour and a half later, I would have most likely been done.
Scott Benner 1:22:12
Yeah. The Jonathan was that simple? You need an answer, right? Yeah. And, and they were you just you need insulin. And without insulin, you've seen it in your life when you're injecting or with a pump. So if something went wrong with the pump, or if you did something wrong with the pump, or whatever, and you're not getting that insulin, this is your body's reaction to not having this insulin. I mean, it's just it's simple. Are you thinking you'd like to try a pump again? But you're worried? Is that what you're asking me?
Jonathan 1:22:40
Um, I mean, somewhat, but I'm really worried because that the pop mound function, the doctors look at it and that it did not function. Okay. It was just one of those mount function ones, you know? I mean, I would love to try another one again. Yeah. But at the same time, I'm kind of fine with the pins. Yeah, the insulin pins I got. Because it was hard for me being on the pump. Because when when I was on the pump, man, I couldn't do things that other people could do, such as playing football, or just messing around and wrestling. You know?
I could, I couldn't do those things. Well, I think
Scott Benner 1:23:36
you should do whatever makes you comfortable. Seriously, right. If I'm good with injections,
Jonathan 1:23:46
or with the pins my bed? No, I'm, I do believe in the future. Like maybe when I'm in my
3540
Scott Benner 1:23:56
I might switch over back to the pump. Right. But I mean, right now, I'd rather just stick with the pins. Cuz What? I'm young, and I still got a lot more stuff I can do. You know, listen, I think you should do whatever makes you comfortable. First of all, but don't think that like you today is not you then you understand that when your pumps stop working, your blood sugar started going up, but you weren't testing your blood sugar. So you'd have no idea you were just like this thing will take care of that is a true, right. But nowadays, you'd be like three hours later, you'd test your blood sugar and go, Hey, my blood sugar is going up and you'd look at the pump and figure out what was going on. It was just you were a different person than than you are now of around your diabetes. So I'm not saying switch to a pump. But I'm also saying don't get it into your head that you'll be more I don't know mature or less done doing active things in your 30s and it'll be easier for you because there are plenty of people who wear pumps and are really active and but I'm also not telling you to switch I'm just saying don't feel limited by that one situation. I think if you were testing back then the way you are now, that would not have happened to you. That's all I'm saying. Right, you know, so.
Jonathan 1:25:08
And I fully agree with that.
Scott Benner 1:25:10
Yeah. Also, I think you have bigger fish to fry, as they say, at the moment. Like, I really think, man, your first step is the is the depression bipolar piece, like that's where you, you want to put your effort right now. And then once you have that in a handleable situation, maybe you'll maybe then you'll start thinking about a pump or a glucose monitor, maybe you don't maybe you'd rather have if you're going to wear something, and your insurance will cover it get index calm, so you can see your blood sugar in real time, like we do you see how that helps you use your insulin? Like, that's really cool.
Jonathan 1:25:44
I've been thinking about asking my doctor about that, too.
Scott Benner 1:25:47
If your insurance covers it, man, go for it. Seriously. But but just you know, first things first, get somebody to help you or you call your insurance company and get numbers and find yourself somebody who can help you with the bipolar piece. Like I can't stress enough that I think that's that should be your next step.
Jonathan 1:26:09
I agree. Yeah.
Scott Benner 1:26:11
That's it, man. I think I think that's, that's, that's a good place to leave off for you and I. But, you know, I, you please send me a message and let me know how it's going. And I will, I would, I'd love to know that you found a doctor and that you're working on just remember to once you find that doctor, I don't know how smooth it's gonna go in the beginning. So try to have patience with it. Okay. Right. Yeah, this medications can be difficult to get dialed in correctly. But if you think you're going to, you know, if you're if you think you're going to have an episode without help, then I don't know. I like who you are right now. I'd like you to be able to stay this person. You know, I'm saying thank you. You're welcome. Hey, I really appreciate you doing this. This is could not have been easy.
Jonathan 1:26:57
I appreciate it. Was it really was it? Yeah, I appreciate you letting me have this opportunity. It's my pleasure. It was
Scott Benner 1:27:05
my pleasure. I'm glad you reached out. Well, I can't thank Jonathan enough for coming on the show and being so incredibly honest with everybody. Thanks also to Dexcom and Omni pod for sponsoring this episode of the Juicebox Podcast You can find those links at Juicebox podcast.com in the show notes of your podcast player, or you can go to my on the pod.com Ford slash juice box to get a free no obligation demo of the Omni pod tubeless insulin pump sent directly to your home. And of course learn all about the dexcom g six, including those alarms. And that follow feature. up to 10 people can follow the Dexcom g six on an Android or Apple phone. It's pretty amazing. dexcom.com forward slash juicebox. The National Suicide Prevention Lifeline is that 1-800-273-8255 the National Suicide Prevention Lifeline is the United States based suicide prevention network of over 160 crisis centers that provide 24 seven service toll free it's available to anyone in suicidal crisis or emotional distress. If that is you call the number right now. 1-800-273-8255. The US Department of Health and Human Services has a helpline for people who are struggling with mental or substance use disorders. It's the essay MH essays national helpline 1-800-662-4357 it's one 806 six to help 4357 the national hotline is confidential, free and available 24 hours a day, 365 days a year. It's in English or Spanish for individuals and family members facing mental and or substance abuse disorders. This service provides referrals to local treatment facilities, support groups, and community based organizations. callers can also order free publications and other information, check them out@samhsa.gov or call 1-800-662-4357. If you're in distress, go find help. Are you enjoying the afterdark series. But think there's more that we could cover something I'm not thinking of send me an email Scott at Juicebox podcast.com always looking for new topics and new people to talk to. Don't forget, you can check the blog out at Juicebox podcast.com. And if you're looking for a wonderful community where you can speak to other people who are not only people living with Type One Diabetes, or somebody who cares for them, but someone who listens to this podcast, if you're really looking for somebody who gets you there is a Facebook page that is private. It has nearly 600 thousand users. 4000 of them are on there every day. It's the Juicebox Podcast, private Facebook group. You can get to it through Juicebox podcast.com. There's a link at the top, you can go to Facebook and search for it. Just answer a couple of entry questions. And just like that you're in and you're having conversations with people who are living the life you are. It's an amazing group. Thanks so much for listening to this episode of the Juicebox Podcast and once again to Jonathan for sharing his story. We'll be back soon with another episode. I appreciate you listening and sharing. I really appreciate when you subscribe in your podcast app.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!