#1638 Heavy - Part 1
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
B is the mom of a T1D son who was diagnosed at 16 months. He is currently 2 and they are about 9 months into managing diabetes. Part 1 of 2.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Welcome back friends to another episode of The Juicebox podcast. Hi.
B 0:14
My name is B. I am a mom to a T 1d son who was diagnosed at 18 months. He is currently two, and we're about nine months into this diabetes game.
Scott Benner 0:26
If this is your first time listening to the Juicebox podcast and you'd like to hear more, download Apple podcasts or Spotify, really, any audio app at all, look for the Juicebox podcast and follow or subscribe. We put out new content every day that you'll enjoy. Want to learn more about your diabetes management. Go to Juicebox podcast.com. Up in the menu and look for bold Beginnings The Diabetes Pro Tip series and much more. This podcast is full of collections and series of information that will help you to live better with insulin. Please don't forget that nothing you hear on the Juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. The episode you're about to listen to was sponsored by touched by type one. Go check them out right now on Facebook, Instagram, and, of course, at touched by type one.org check out that Programs tab when you get to the website to see all the great things that they're doing for people living with type one diabetes. Touched by type one.org This episode is sponsored by the tandem mobi system, which is powered by tandems, newest algorithm control iq plus technology. Tandem Moby has a predictive algorithm that helps prevent highs and lows, and is now available for ages two and up. Learn more and get started today at tandem diabetes.com/juicebox I'm having an on body vibe alert. This episode of The Juicebox podcast is sponsored by ever since 365 the only one year where CGM that's one insertion and one CGM a year, one CGM one year, not every 10 or 14 days ever since cgm.com/juicebox Hi.
B 2:19
My name is B. I am a mom to a T 1d son who was diagnosed at 18 months. He is currently two, and we're about nine months into this diabetes
Scott Benner 2:31
game. Wow, currently two, nine months in. Do you have other children? Nope, this is the only
B 2:38
one I say that diabetes is my second kid. We actually were gonna, we were thinking about having another, but he got the diabetes. And I was like, oh, okay, you wanted to be an only child. I understood.
Scott Benner 2:49
Maybe we'll do this instead for a while. Yeah, hold on a second. Arden is asking me why the dog is all wet. Oh, we were outside in the grass. I think he's up in her room. I think she wants to make sure
B 3:02
that you like, always just leave those little, those little parts in the podcast is like, it makes it just like a
Scott Benner 3:09
real thing. Oh, I'm glad. So, okay, let's talk about, how did you figure out? I'm sorry, your son or your daughter, son, son. How did you find out? Figure out your son was what was I gonna say? How did you figure
B 3:21
out? Yeah, so I have a, you know, was in my former life, prior to becoming a mom, was a pharmacist, so I just kind of mom instinct to notice that he was drinking a lot, the standard, peeing all through the diapers, wetting the diapers every night. And you know, when you have a kid, they get older and older, you start using less diapers. But I was noticing, Hey, I've been going back to, like, newborn days, changing diapers all the time. What is going on? Yeah, always wanting to eat, constantly asking for my food, my husband, my mom's food, all the time, always wanting something to drink. And I'm like, What is wrong with this kid? Of course, I didn't immediately correlate it to that. So like everyone else, I go to Dr Google. Hey, why is my kid pink? And then it's like, oh, it might be type one diabetes. And I'm like, Oh no.
Scott Benner 4:14
And so did you take Dr Google seriously when it said that?
B 4:17
I did? Yeah, it doesn't mean it made sense. Like I said, I I have some previous medical background, so once it reminded me of that, I was like, oh, no, yeah, that is
Scott Benner 4:28
what it is. What'd you do? First you go to your was your husband? Did you go to him? Or what'd you do?
B 4:32
Yeah? Yeah. So I went to my husband, told him, Hey, I'm gonna take the kid to somewhere up to we have, like, a little emergency, a children's emergency department just down the street, probably, like, five minutes away. So I'm gonna take him here, but I'm pretty sure this is what it is. And he's like, Well, no, maybe it's a UTI. You know, the same thing that all parents like, like, no, no, it's probably just a UTI or something like that. But sure, take him. I'm like, it's diabetes. Husband, like, that is what it is. And he's like, no, just take him. He. He goes off to work and, you know, he just let me know my mom and I go to the emergency, of course, you know, his glucose is like, 600 and they're like, oh my gosh, you know, like, I think it's, you know, this type one diabetes. I'm like, oh, you know, of course, I already knew that's what it was. But then when you get there and they tell you, that's what it is. You're just like, oh my gosh, yeah, what am I gonna really hit you? And how old is he again? So he's two now, but he was 18 months at the time, and
Scott Benner 5:29
that's even a little, I mean, not big, more or less heartbreaking, but he's so small, right? And sitting there in front of you, yeah, you beat us by like, seven months. Arden was, oh, like, about a month after second birthday. Congratulations. Thanks. Are you in the ER at that point? Yeah.
B 5:47
So we're in the ER there, you know. Okay, well, let's do all of the blood gasses and things and see if he's in DK. You know, he didn't look like he was because he was fine. So we didn't, you know, we didn't get to the DK part. But, like, let's just see if he has the ketones and all that he did. So, you know, they were like, Okay, let's put in an IV so that we can try to flush these things out. Of course, putting in the IV was one of, you know, most traumatizing things that you know a parent can witness. You know, you're having to hold him down while he's staring at you in your eyes, and it's like, Mom, why are these people doing these things to me? You know, he's crying. So traumatizing. So, you know, they give the blues, try to flush them out, and then the ER doc comes back, tells us what is going on. Says, Hey, I called this Endo. That's like, a little bit down the road. We're actually going to send you over there, because she said, if you can get there by noon, she'll be able to see you today. Get you all set up, get you some prescriptions for insulin and all that. I'm like, okay, but great, wonderful. We don't have to go get admit it great. So they pull this IV that took, you know, 30 minutes for them to put in, pull it out. We run over to this in those office and then the lady's like, Wait, why are you here? I'm like, but no, no, they called and then they told you that we were coming. Well, yeah, but I thought that you guys had been admitted on the floor for a couple of days, and then you were coming after a hospital stay, like you just came from the ER, yes, oh no, no, no, no, you got to go back to the emergency like, I can't see you. I don't have enough time to do the education right now. I thought you already had seen the dietitian, seen the, you know, diabetes educator and all that. And I'm like, wait,
Scott Benner 7:32
what? Yeah, oh, my God, did you have to go back and they had to put the IV back in? Yes, yeah, really.
B 7:39
And it was even worse the second the second time, and I think four people had to try to put it in. And the last time, I was like, if you guys could not figure this out, this, I'm not letting you do it. I'm you. You are not putting this in, like, because, again, I'm out there trying to put him in a, you know, the little burrito thing. I'm like, he doesn't, he don't care about that. He's trying to break free. He's never liked to be swaddled as a kid or anything. So, yeah, they're putting it in. Eventually, they got somebody that knew what they were doing, used a little ultrasound machine and was able to find a vein, but I can still see, you know, how he was staring at me and screaming, and I'm trying to hold them down and talk to them and say, like,
it's okay, I'm so sorry. Oh, yeah, still, still have some you're on set
Scott Benner 8:27
by it now, thinking about it, yeah, yeah. And you're never gonna, I mean, I hate to say this, but the truth is the truth, right? Like, you're never gonna know how it impacted him, like you might find out years from now, but in the moment, it's gonna seem like it's okay, but who knows if he'll have an aversion to that, or if he'll just go by and not be a big deal for him. They have to wait, and then you have to worry about that, like you have to wait and worry about whether that's going to be an issue too. You know what? I mean? Yeah, you don't have enough other things to worry about. You're not busy enough be right, yeah. So how long do you end up staying in the hospital?
B 9:01
Okay, so here's another funny thing that's not funny. And we ended up staying six days in the hospital because it happened right when there was a hurricane coming through. We live in Florida, Central Florida, and there was a hurricane Milton, if anybody from Central Florida remembers that, that that's what came through. And so they didn't want to send us home because, oh, you're newly diagnosed, you know, you could lose power, all that kind of stuff. And then also, the the offices, the indos, were closed and right? We didn't have anybody that we could have called if, you know, he had a low or, you know, brand new diagnosis, so they just didn't feel comfortable. And then also, because it was Hurricane short, as the staffing was very short. So, you know, they started him on a sliding scale, and they just really couldn't figure it out, and they're trying to give him mashed potatoes. I'm like, this is not, you know. So, you know, he's 300 and they're no well, we don't feel comfortable sending you home because his numbers aren't well. Well, of course not. You're sliding skeleton in and then you're also trying to give him macaroni and cheese, like, come on, yes.
Scott Benner 10:07
But so instead, they thought, well, you'll, you'll be safer in the hospital, yeah, so you're there for much longer than you would have needed to be otherwise.
B 10:14
Yeah, yeah. We, it was a Monday morning, and that we got initially, took him in, came back, you know, that afternoon, after the whole endo ordeal, and then stayed until Saturday afternoon, I was like, come on, people like, please send me. Please send me home. I'm tired of this, and I'm trying to tell them, like, Hey, I I understand something. You know, I get, of course, I have never, like, poked my kid. And, you know, done. I've done glucose check the blood sugar before plenty of people, but not my kid, but I can do it like, please. Like, I'm okay, like,
Scott Benner 10:45
but maybe better off with the hurricane. And you guys give it a mash potatoes, macaroni and cheese, and tell me you can't figure out his blood sugar. Yeah, yeah. What did they ever get it straight in the hospital? Or did you just kind of wait out your time and then go home
B 10:59
straight where it was like two something, so, sure,
Scott Benner 11:03
not really, but, yeah, okay, whatever. Yeah, better than where it started. How would you describe where you are now? Like, I mean, it hasn't been that long, right? So what's the experience been like so far? How far have you gotten in all this?
B 11:18
I think we're pretty good in. I mean, of course, there's always still something else to learn. And I wish my kid, two year old child, didn't want to eat every five minutes. Because, like, I'm like, I would, I would love to have like, a, you know, six, a, 1c, but the way this kid just eats things every second. And yeah, but anyways, listening to the podcast, doing lots of reading. I, you know, I'm a researcher, and I love reading all of those types of things. So just learning everything I can to be able to dose him appropriately and make different changes to his insulin dosing, like I was Pre-Bolus in within like, the first week, even though the endo was like, no, no, even the hospital, Oh, yeah. Just, just give it to him after he started eating. No, we're not doing that. Yeah. Like, my kid loves to eat. So I trust that if he doesn't eat this, he'll eat this other thing that I know is an equivalent amount of carbs. So, you know, I think we're in a good, enough place. We're currently on Omnipod now, but I transitioned him over to the Moby just for a little bit tighter control, and it's less work from me, because I yeah, I do. I feel
Scott Benner 12:37
like that might help you there. Yeah, I want to go back to you. Said you like I was pre bolusing. Right away you were finding out, you know, you said you like to do research and stuff like, so what gave you the indication that you needed to go look for more information?
B 12:49
Well, just my own curiosity. That's just me as a person. If there's something that I want to learn about or need to learn about, I'm not going to just take the Pink Panther book that they give you and have that be the only thing that gotcha. I learned from or whatever the Indo says, which is the two words that they they tell you, No, I let me find out something else. I even actually remember sitting, I think it was the same, either first or second night in the hospital. I'm like, there has to be a podcast or something that talks about type one diabetes, that I can learn something to help me with this, because I need, I need some additional education, because I just don't feel comfortable here.
Scott Benner 13:36
You started thinking about that stuff right away, like there's got to be other there's content out there something I can figure out. So how old are you? How old am I? I'm 37 Okay, so you're younger. Okay, so podcasts are a thing you think of when you
B 13:48
Oh, yeah, I listen to podcasts every single day about various different topics, podcasts and YouTube. That's how I that's how I learned,
Scott Benner 13:57
yeah, it's where you get people's stories right and figure out what's uh and then you What do? You What do you filter through it and decide what makes sense to you?
B 14:04
Yeah, I went on YouTube first, just because, you know, sometimes visually you can work a little bit, but I just couldn't, I didn't find it there, and then I was okay, well, let's just go to podcast, because we can listen there and still learn it. And found you and a couple others, and they, you know, definitely helped. And what was being said, it made sense. Let's try it out.
Scott Benner 14:24
Yeah, and you got it working. That's awesome. So now you're just nine months into this. So yes, where's is a 1c sitting right at the moment. Why would you settle for changing your CGM every few weeks when you can have 365 days of reliable glucose data. Today's episode is sponsored by the Eversense 365 it is the only CGM with a tiny sensor that lasts a full year sitting comfortably under your skin with no more frequent sensor changes and essentially no compression lows. For one year, you'll get your CGM data in. In real time on your phone, smartwatch, Android or iOS, even an Apple Watch, predictive high and low alerts let you know where your glucose is headed before it gets there. So there's no surprises, just confidence, and you can instantly share that data with your healthcare provider or your family. You're going to get one year of reliable data without all those sensor changes, that's the ever sense. 365 gentle on your skin, strong for your life. One sensor a year, that gives you one less thing to worry about. Head now to ever since cgm.com/juicebox to get started, let's talk about the tandem mobi insulin pump from today's sponsor tandem diabetes care, their newest algorithm control iq plus technology and the new tandem mobi pump offer you unique opportunities to have better control. It's the only system with auto Bolus that helps with missed meals and preventing hyperglycemia, the only system with a dedicated sleep setting, and the only system with off or on body wear options. Tandem Moby gives you more discretion, freedom and options for how to manage your diabetes. This is their best algorithm ever, and they'd like you to check it out at tandem diabetes.com/juicebox when you get to my link, you're going to see integrations with Dexcom sensors and a ton of other information that's going to help you learn about tandems, tiny pump that's big on control tandem diabetes.com/juicebox, the tandem mobi system is available for people ages two and up who want an automated delivery system to help them sleep better, wake up in range and address high blood sugars with auto Bolus.
B 16:45
Last time we checked, it was, I think, a 680 that's awesome.
Scott Benner 16:49
Good for you. That's really great. And he's, what, a little over two now, two and a half.
B 16:54
Yeah, he turned two in March, so, and it's what currently July is, for context, for anybody listening, three months in the future.
Scott Benner 17:02
Yeah, that's, well, that's so, how do you think he's so you're doing? Okay, how's he doing?
B 17:07
Oh, he's doing great. Yeah. So, oh, yeah. So we started before we got the pump. I took it, I think about a month for us to get the pump. But before we did that, we were, of course, MDI and again, more trauma, thinking about it took two of us to have to give him the shots. You'd have to, like, hold him down and hold his leg and make sure he doesn't kick to try to shoot it. And then sometimes he'd move, and then he wasn't you weren't sure how much insulin you actually gave him. And, oh yeah, this so getting the pump.
Scott Benner 17:38
This sounds familiar, by the way, I have those memories, because
B 17:41
everything I remember, uh, Arden was four years in di
Scott Benner 17:45
Right, yeah, she, well, she was diagnosed when she was two, and we had a Omnipod on her before she went to kindergarten. So I don't exactly know how old she was then, but going into kindergarten, she was wearing a pump.
B 17:58
So a couple, a couple years now, at least three, I think, oh, gosh, yeah, I can't even, like, it was a couple weeks and I'm like, I, I'm not going to be able to do this. He did fine with the finger pokes. He you know, he'd be like, Oh, you don't poke my finger. You know, thought it was cute, but the spokes for the food, he was not having
Scott Benner 18:18
it. Yeah, I spoke to somebody recently who said that they started off by saying that their kids a 1c was better on MDI, and then the more I spoke to them about it, the more I it became kind of obvious the kid wasn't always eating when they were hungry because they were trying to avoid the shots. So it wasn't so much that and because, but it was interesting as we conversated, because the mother thought, I mean, the way she presented it to me was that pumping is not as good as MDI, because she has her a one CS going up. But what's the truth is, is the kid, the child, is actually eating now, like when they mean to and before, they were skipping meals and skipping certain things to avoid getting an injection, and she didn't realize that it was, it
B 19:02
was happening, wasn't food, wasn't punishment. Basically, it's like, oh, I have to, you know, be injured first before I can eat. So I'm like, I'm gonna make sure I'm really, really hungry. Yeah, and endure
Scott Benner 19:13
this, exactly what was happening. And the mom didn't know, know it until we, I think we spoke, talk through it. So, I mean, yeah, for the people who it's hard for it's really, genuinely hard for them, you know? Yeah, yeah. So it is really rough. So you're pretty new at this, but what's the toll been on you? Like, what's the emotional side of tracking carbs and chasing highs and guarding against lows and overnights? How is it treating you?
B 19:39
Oh, so, like, I haven't slept the full night since, you know, he was born. You know, I thought I was gonna, you know, grow out of that at some point, but then he got the diabetes, and I'm like, oh, okay, well, I guess I won't, you know, sleep it's I have a therapist because, you know, we need those, but I definitely do about 90. 9.8% of all of the diabetes things. So it is very much a a huge toll and mental burden for myself. I'm getting glucose alerts now, and I'm like, Ah, he needs him, and I need to go send him some but I'm in here, so I can't so it's, it's, it's a lot, and it's very, very mentally taxing. And I wish it was a way to be able to explain to others how much of a huge mental burden and physical burden, actually, that it takes on the parent, and then you're also thinking about, like, the long term complications and issues that, like, if I'm not over here, micromanaging This is my kid gonna not have his toes when he's 20, you know? So it's a lot, but I have a therapist, and I really recommend that for for everybody, if you can, because, you know, you need it. You need that unbiased person to talk to you and just be like, let you express yourself in whatever way, if it's frustration or happiness or whatever, and not how you know your mom or your husband might be like, Oh, you're doing great. Like, this is getting people sure, but I like want to shoot myself. You know, when people
Scott Benner 21:22
tell you you're doing great, that's not comforting.
B 21:26
No, no, no. See, here was another thing that I actually wanted to talk about. Is like I mentioned before, previous life was a pharmacist, and one thing that, anytime I tell anybody that my son has type one diabetes, their first thing out of their mouth is, oh, my goodness. Is so great that, like you're his mom. Because, for some reason, because I'm a pharmacist, I just clearly know how to treat a kid with type one diabetes, like, of course, I know the different drugs. I learned all of those things. I know how to take a blood sugar and all of that, but the day to day management, especially in a super young toddler that's running around flipping over here, they're eating every half a second, it is not, it's not the same. And they don't, they don't understand it. And it really bothers me when people say that, like, oh, just because I have this medical background that I'm just automatically supposed to know what to do with my kid.
Scott Benner 22:25
Yeah, it sucks, because you kind of understand where they're coming from. They're trying to be, like, upbeat, and they're like, oh, at least you know about it, and that kind of thing. And you're like, that doesn't help at all. But thank you. Some of the people that I've seen struggle the most have medical backgrounds. I've seen doctors, researchers, nurses, lots of different people with medical backgrounds who are completely flummoxed by diabetes, just like everybody else. You know, yeah,
B 22:50
it all just puts us in the same little basket. Doesn't matter
Scott Benner 22:54
if you have, yeah, good point. We all, we all go back to start when this happens, whether you're a type one, or a parent of somebody like, it resets you, doesn't? It almost doesn't matter what you know sometimes,
B 23:06
like, Sure, I've heard Atlantis before and Humalog, of course, and I know what they do and how they work, but how do they work in my little 18 month old? Yeah, I don't know. Or how am I supposed to
Scott Benner 23:17
think about it at four o'clock in the morning when I haven't slept all night for 567, days in a row. Yeah. What do you do with that when they tell you, do you take it to your therapist later, or do you speak to them about it in the moment when they tell you, like, oh, at least you're a pharmacist.
B 23:32
Took it to my therapist. Actually had one person that I mentioned it to. He was actually a classmate, a pharmacist classmate. And I actually asked him, I'm like, what made you ask me that, or not necessarily ask me that, but what made you say that to me? Because I felt comfortable enough with him to ask, ask that, and he just was just like, you know, I don't even remember what his explanation was. It kind of made sense at the time, but maybe it didn't, because I don't remember what it was, but most of the time, I just take it to my therapist and let
Scott Benner 24:05
her, you know, tell me it's fine. Do you think that's them being insulting, but not direct, not on purpose? Or do you think it's you being like, I don't know, touchy about it, like? Do you mean like? Because I'm trying to figure it out, too? It out too, when it happens to me. Like, is this, is this me overreacting, or is it them, you know, actually being coarse, because I don't think it's them, and I also wouldn't consider myself overreacting. Like, if you told me to sit down right now and really, like, unburden my soul about what it's like, even to this day with a 21 year old who has diabetes, like, I'm gonna sound like, I'm complaining pretty quickly. You know what I mean? Like, like, you're gonna be like, Oh, boohoo, Scott. Is it that bad? But like, you know, in certain moments, for certain things, it's terrible, like it really is, and it doesn't like, it doesn't magically get better because they get. Older, or because they know how to Bolus for themselves, or something like that information. Scott, thank you. No Sure, but you live your whole life knowing this is never gonna get any different, the honesty of it doesn't change, like you get better at maybe living through it, or, you know, like having it not impact you so visibly,
B 25:18
knowing the 17,000 things that you have to pack with you just to go up to the, you know, the library, yeah,
Scott Benner 25:24
yeah, or realizing that, I don't know, you've seen 1000 movies in the last 20 years, and every time you leave for the movie theater, somebody makes sure that there's insulin in a pump, because you don't want to be in the movie if the pump errors or something happens and you have to go home and miss the movie. But the truth is that that's only happened twice the entire time, but you still make sure every time, and the person you're saying it to is like, Why do you say this all the time? Like, why do you keep bringing this up? This never happens, but she doesn't remember the one time it did happen, and how upset she was that we had to leave, and how bad I felt because we had to leave, and how terrible it was to drag my son out of there and like, but she just thinks I'm paying too much attention to it. You know what I mean?
B 26:07
I'm sure they remember, you know, whatever movie that was. We didn't actually get to watch it because of my diabetes, or Arden's, you know, diabetes, yeah, yeah.
Scott Benner 26:16
And it just, and it's sad and it's upsetting and it's not. And if she was 50, and I was 75 and we were going to a movie. I think I'd probably think, Oh, do we have, like, some backup supplies with us, just in case, you know. And she's gonna look at me and go, like, I have five kids of my own here. And like, I don't need your help. But it doesn't stop you from, like, I don't know how to stop thinking about,
B 26:38
I think she'd be grateful if you actually had it, and it did happen. And you just like, yep, nope, here you go, I got it. We can just change it,
Scott Benner 26:44
right? It finally happened, yeah. But like, you know, in the meantime, like, no one's grateful that somebody's worrying about them. They just don't want people worrying about them, and you understand that, but they also don't know what it's like to be the parent and feel like that pressure, if that makes sense or not, but, oh,
B 27:05
trust me, it does. I try to tell my husband all the time about just all the many things that I'm having to think about and remember and juggle just to manage his, you know, his diabetes only for, you know, them to just give them something random. And I'm like, why is he 300 what happened? Oh, I just gave him some of my, you know, frosted flake milk.
Scott Benner 27:31
What? Just gave him milk with sugar melted it. It's awesome. You want to mention that Bolus for anything?
B 27:38
Oh, my gosh. You didn't know how much this, like, how much I do, and then you can ruin it, which is, like, one little thing, Oh, my goodness,
Scott Benner 27:48
yeah, yeah. It all starts over again. And yeah, well, I mean,
B 27:53
sorry you had, you had asked me that one question about whether or not I thought it was them or me. I will say sometimes I could maybe be a little bit sensitive in terms of, you know, I enjoyed being a pharmacist, but I actually chose to stop being a pharmacist prior to even having my son, but in anticipation of having him. So it could just be my own projections of people thinking like, Oh, why are you not doing that anymore or something? And, oh, you're choosing to stay home instead of doing this career that you know you went 1000 years to school for. So it could very much be my own,
Scott Benner 28:34
my own projection. I take your point. I really do. I don't know it's just hard. It doesn't I think it's different, but I don't think it's any less difficult than it was when she was two. Like, there's just different problems today, and now she's older, and I see her side of it, like, I don't want, like, you know what I mean? Like, I you know if it's about, like, you're always talking about this, and I'm like, Well, you need to do the thing. You know what I mean, like, and so I don't want to talk about this. Yes, you do. You love talking about I'm like, I hate talking about this. I was like, this the worst part of my day right now. Like, I don't want this at all. And if she was just 2021, years old, and the stuff was, like, you know, stuff that every kid goes through, that they come out the other side of, normally, I just say, Okay, it's part of the journey. But like when the journey is about health, and you're worried that it could hurt right now, hurt later, create a habit that you know will hurt somebody 20 years from now, whatever it is you're thinking about, I think it's two decisions, like you have two options, right? And neither of them are good. Like, am I going to ignore health right now and maybe all the things that I just said could come with it in the future, or am I going to put more of the value on harmony and be. Harmonious but unhealthy, or would I rather be healthy but less harmonious? Like, there's no good decision in there. And I do really think that at certain points in people's lives, those are the only two decisions, like, which one are we throwing away here? I don't know how to make the decision. I'm still not good at it.
B 30:20
Okay, so note to talk to my therapist on Thursday about this. Because, yeah, oh my goodness,
Scott Benner 30:27
yeah. Because I wish someone would have come and found me when Arden was two, and told me that this is, you know, as she gets older, it's going to be the biggest piece of the whole thing, and that no matter what I do, I'm going to be wrong, because if I choose harmony, when her health fails, she's gonna wonder why I didn't help her, and if I choose health, then when she's, you know, having a very real and human, you know, I don't know disengagement as you know how you disengage from your parents as you get older, right? You know, and like, they want to disengage, but they're gonna not know everything to do, so they're going to ignore stuff for a while, and so I let that happen, and then, you know, then we don't have the same relationship. I just honestly, I don't know the answer. I really don't,
B 31:13
yeah, you saying that actually reminds me of, I'm not 100% sure this is the true story, but I'm just going to say it anyway that, you know, Mr. Rogers, you know, how, like everybody, like all the kids, we all watched it when we was where we were little, yeah, and loved him. But then I hear that he didn't actually have a really great relationship with his own children, which is unfortunate. And just the story that you were saying about you being this, you know, diabetes influencer, guy and you know, know that whatever you know based off of raising Arden, that it could be a similar thing. Just you know, you trying to find this balance between the health and the harmony, but wanting to choose help more often can make your relationship with your daughter just not be as close and as strong as you would want it to be, because it's always about diabetes and not just about like,
Scott Benner 32:11
Yeah, her. I also think that I don't know that our relationship is less strong, but I think that in the background, it's always just alive in the background like she thinks I'm too worried about her health, and I think she's not worried quite enough about enough, right? And then somebody's gonna say, well, it's her decision, and that's all well and good. But you know, you're gonna put a 12 year old, a 15 year old, a 20 year old, in charge of that like they you know, that normally doesn't go so well. And I would, in any, almost any other walk of parenting, I would err on the side of like, just let them go make their own mistakes. They'll be okay. Like, this
B 32:55
one thing is like, yeah, you know, could be life or death here, yeah,
Scott Benner 32:59
this one thing feels really different. Also, like, your kid could be like, you know, they have their own personality too, obviously. So you could do one thing with one that works great, and, you know, go to somebody else that doesn't work at all. Like, maybe it's going to work great between you and your son and somebody else listening right now is going to do the same exact thing, and it's not going to go as well. And who knows? Like, I mean, people are still people. They're the variable in the in the whole thing. Like, I don't think I'm doing anything wildly wrong. Like, you know what I mean? Like, I mean, yeah, you're a kid, you know, you people have children. Know, Like, nothing you do ever works out exactly right. But you know nothing objectionable, but you don't know how it's being received on the other side. And even if you think it's going well, sometimes it's not, and you don't realize it, or sometimes it's going great, and you don't realize that either, it's just really difficult to raise children. And then you add this all to it, and it adds about six other levels that are difficult on top of it.
B 33:59
Yeah, the diabetes definitely wasn't part of the plan in my parenting journey, for sure, but yeah, what you were saying about I just really that's another kind of fear that I have about my relationship with my son as he gets older. I really want to remain close with him, and you know, and US him be able to come and tell me things and or at least tell his father, if it's you know, something that you know they need to speak about. But just bring things to us. But I also still want to make sure that he's in good health, and he has all of his limbs, and he can see, and it's just how I mean, is there any way to balance that sounds like what you were saying, that there really isn't a such thing as balance. In this regard,
Scott Benner 34:50
I don't know how to make the decision between, like, how do you ignore something? And I do it sometimes, by the way, right? Like, sometimes there's a blood sugar that really needs attention. And she's not giving it attention, and I don't say anything about it. And, you know, and sometimes, you know, you speak up and you get met with, I don't need your help, or, you know, something like that. And you know, you look and say, Well, I mean, your blood sugar has been elevated for five hours now. Like, I appreciate that. You don't. I appreciate you don't need that. You know what to do, but you're not doing it. So can
B 35:22
you do it, please? Then I'll happily Shut up
Scott Benner 35:25
exactly, yeah, to the point like, if Arden hears this in the future one day, this is the last thing I want to be talking about with you. And I know that when she hears that, she at this moment in her life, she doesn't believe me. But I promise future me and future Arden, like, I don't want to be talking about this. I don't want this. I don't want her to have diabetes. I don't want her to have a thyroid issue. I don't want to be worried about this. I don't want to, I don't want her to worry about it. I wish none of this happened. You know, this isn't something I want to talk
B 35:58
about. Yeah. I mean, if only I could have just, Okay, well, give it to me. I'll, I'll be fine, like, just let me, let me have the diabetes, and let my kid just run off and play and not worried about something stuck to them. Yeah, 24/7 I'll be the robot person.
Scott Benner 36:14
But I would do it just to get rid of the, the psychosocial part of it, like I would, I'd be happy to like, whatever. Like, you know, I know this is not how it works, but I take your point, and I'm right there with you, but I don't even know if that would sound insulting if she heard it like, you know what I mean? Like, I could take, I'd take this if I could. Maybe they're like, Well, I You can't, so it's pretty empty. You know what I mean? Like, there's and by the way, who knows? Like, like, I said, there's going to be plenty of people who make that decision, and their kids are going to just be like, All right, awesome, thanks. And some people rub up against stuff, and some people don't. I don't know why. You know? I mean, if you really listen to me on the podcast, I'm just trying to figure out how all of you think, so that I can hopefully have some answers when I've gotta talk to my own kid, you know, because I don't know, like, I don't know why. I mean, think back on your own life, right? Using a great example, I was 20 years old. I was at work. One day, some guy I worked with, some kid I worked with, came up to me and was like, Yo, I'm gonna be at your birthday party. And I was like, I don't know what you're talking about. So he's like, No, yeah, yeah. And he showed me the invitation, the whole thing, and I was like, Oh, my mom was throwing me a surprise birthday party for my 21st birthday. And it made me really uncomfortable. And to this day, I don't know why, and something about it really made me upset. And I asked my mom. I actually told my mom, like, you have to cancel this party. I am 54 on Saturday just passed. So that is 3141 51 they just 33 years later, I still feel terrible about it, like I don't know why I did that. You know, oh, telling your mom to cancel it, it'll make me cry. Me if I talk about it with you, like, I don't know why I did that, and I wish I could have taken it, but I've wished I could take it back for years and and that's not and there's no diabetes mixed in that, you know, it's just like, it's just the thing between me and my mom. And if you're out there telling your kids, like, hey, I need you to Pre-Bolus, and they have a disjointed reaction, like I had about that birthday, like, what do you do next? You know what I mean? Like, the birthday came and went. My mom was disappointed and she was sad, and eventually she probably got over it. I never got over it. It's been one of the bigger lessons of my adult life. Like, just, I don't know, I don't know why I did it, but I would never do it again. But at least it was a thing we could get past. It didn't come up again three hours later when I was hungry, and then three hours after that, and then the next day, and then at two o'clock in the morning, like, you know I'm saying, because when it's a
B 38:54
diabetes thing, once a year with a birthday, but diabetes, oh boy,
Scott Benner 38:58
I probably forgot about it two years later, she was probably still upset about it, like, and I don't know, I apologize to her as adults. And the truth is, I don't think she really remembered it the same way I did, you know. But my point is, is that when it's diabetes, you don't get, like, you don't get a year off in between talking about it, or get to forget about it, or something like that. It's going to come up again the next time the thing beeps, you know,
B 39:22
so I don't know,
Scott Benner 39:24
yeah, I don't want to bum you out. Am I bumming you out?
B 39:29
Oh, you know. Thank goodness we have therapy on Thursday. Because, um, oh, gosh, yeah. So apparently it just doesn't like, it gets better. Like, somebody asked me that the other day. He's like, Oh, does it get better? And he gets older, and I'm like, yes, and no, from my understanding, yes, you know, he can, I can explain to him what it is that I'm doing and why I'm doing it, and he'll understand. But also, you know, other things happen, other you know, there's hormone attitudes in him, you know, wanting to do it. Own thing. And so yes and no, yeah,
Scott Benner 40:04
it'll change. Sigh, yeah, do you say sigh? I did. That was awesome. So I was like, Oh, she's adding emojis to our conversation. This is awesome. Yeah. I mean, it changes. It continues to change. I'm I think I'm more talking about the parenting part of it. Like the closest, and I'm happy not to have any experience with this, I should probably knock on something, right? But, like, I imagine this sort of, like, if your children are have, like, a serious drug issue, right? Or there, or there's a real significant mental illness, something that, at the end, if not managed correctly, is going to end in a terrible way, but that you really don't have any actual power over I think that's the hardest thing about the diabetes once your kids get older, is the truth is, is you don't have any actual power over it. You can say something and hope that they listen. You can hope that you're right and hope they listen, but you don't. It's not like when they're seven. And you can just go, like, here, you know, take this and they go, okay, and then they do it. Like, that's the part that's like, I've already given away the idea that I have power over it. I know, I don't. I know that she's an autonomous person, like, she's not going to do anything she doesn't want to do, but like the part that doesn't go away is the part that doesn't go away. And for diabetes, it is like all the possible health outcomes and and for me too, just that it impacts how she feels and thinks every day, if it's not managed in a certain way. And other stuff too, like thyroid and stuff like that as well, stuff that you know degrades if you're not managing it, but you don't see it coming. At least with diabetes, you'll end up in DK in a month or a week or whatever, right? Like, but like, you stop taking your, I don't know, your thyroid medication, like, first two months, you'll probably be okay. And then, like, if things are gonna drift on you and drift on you, and you're not even gonna feel it happening when it happens, and then you're going to be burdened with all the problems that come with it, and, you know, etc, and so on. So anyway, like, I don't know if this is going to ring hollow for some people, but like, this feels like this to me. Feels like having like an addicted child, because you don't have any real power over it. People do what they want to do, and if it doesn't go well, the outcomes are dire, like that. To me, feels like diabetes parenting.
This episode was too good to cut anything out of but too long to make just one episode. So this is part one. Make sure you go find part two. Right now. It's going to be the next episode in your feed head now to tandem diabetes.com/juicebox and check out today's sponsor tandem diabetes care. I think you're going to find exactly what you're looking for at that link, including a way to sign up and get started with the tandem Moby system. I'd like to thank the ever since 365 for sponsoring this episode of The Juicebox podcast, and remind you that if you want the only sensor that gets inserted once a year and not every 14 days, you want the ever since CGM, ever since cgm.com/juicebox one year one CGM touched by type one sponsored this episode of The Juicebox podcast. Check them out at touched by type one.org on Instagram and Facebook. Give them a follow. Go check out what they're doing. They are helping people with type one diabetes in ways you just can't imagine. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox podcast. If you're not already subscribed or following the podcast in your favorite audio app, like Spotify or Apple podcasts, please do that now. Seriously, just to hit follow or subscribe will really help the show. If you go a little further in Apple podcasts and set it up so that it downloads all new episodes, I'll be your best friend, and if you leave a five star review, ooh, I'll probably send you a Christmas card. Would you like a Christmas card? When I created the defining diabetes series, I pictured a dictionary in my mind to help you understand key terms that shape type one diabetes management, along with Jenny Smith, who, of course, is an experienced diabetes educator, we break down concepts like basal, time and range, insulin on board and much more. This series must have 70 short episodes in it. We have to take the jargon out of the jargon so that you can focus on what really matters, living confidently and staying healthy. You can't do these things if you don't know what they mean, go get your diabetes to find Juicebox podcast.com, go up in the menu and click on series if you're looking for community around type one diabetes. Check out the Juicebox podcast. Private Facebook group Juicebox podcast, type one diabetes, but everybody is welcome. Type one, type two. Gestational. Loved ones. It doesn't matter to me. If you're impacted by diabetes and you're looking for support, comfort or community, check out Juicebox podcast. Type one diabetes on Facebook. Hey, what's up, everybody? If you've noticed that the podcast sounds better and you're thinking like, how does that happen? What you're hearing is Rob at wrong way recording, doing his magic to these files. So if you want him to do his magic to you, wrong way. Recording.com, you got a podcast? You want somebody to edit it? You want Rob.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1637 Over Producer
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
Alex, 33, diagnosed T1D at 11, shares scoliosis, teen diabulimia, and lactic acidosis. Now a nurse, witnessing NICU outcomes reshaped her care and motherhood plans, rejecting blame.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
COMING SOON
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#1636 Premature to Postponed
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
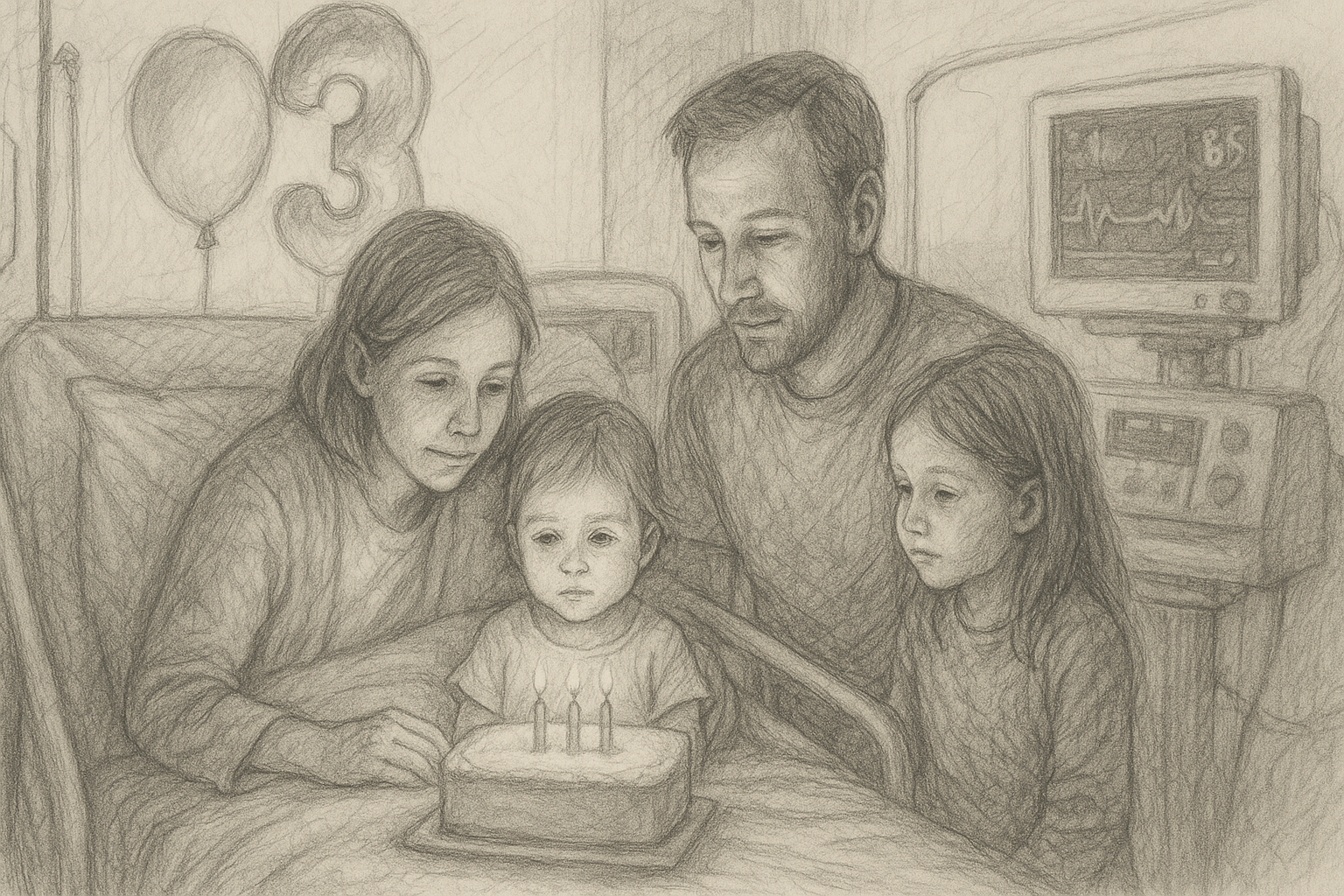
Laura, 45, a social worker and mom of two, shares her oldest daughter’s type 1 diabetes and celiac diagnoses, premature births, and a birthday spent in the hospital.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Friends, we're all back together for the next episode of The Juicebox podcast. Welcome.
Laura 0:14
So my name is Laura. I'm from upstate New York, and I have two beautiful daughters. My oldest daughter is type one diabetic, and I am a social worker.
Scott Benner 0:25
If this is your first time listening to the Juicebox podcast and you'd like to hear more, download Apple podcast or Spotify, really, any audio app at all, look for the Juicebox podcast and follow or subscribe. We put out new content every day that you'll enjoy. Want to learn more about your diabetes management. Go to Juicebox podcast.com. Up in the menu and look for bold Beginnings The Diabetes Pro Tip series and much more. This podcast is full of collections and series of information that will help you to live better with insulin. Please don't forget that nothing you hear on the Juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. This episode of The Juicebox podcast is sponsored by the Omnipod five and at my link, omnipod.com/juicebox you can get yourself a free, what I just say, a free Omnipod five starter kit, free, get out of here. Go click on that link, omnipod.com/juicebox check it out. Terms and Conditions apply. Eligibility may vary. Full terms and conditions can be found at omnipod.com/juicebox links, in the show notes, links at Juicebox podcast.com today's podcast is sponsored by us med. Us, med.com/juicebox you can get your diabetes supplies from the same place that we do. And I'm talking about Dexcom, libre, Omnipod, tandem, and so much more us. Med.com/juicebox or call 888-721-1514, the episode you're about to enjoy was brought to you by Dexcom, the Dexcom g7 the same CGM that my daughter wears. You can learn more and get started today at my link. Dexcom.com/juicebox dot com, slash Juicebox.
Laura 2:23
So my name is Laura. I'm from upstate New York, and I have two beautiful daughters. My oldest daughter is type one diabetic, and I am a social worker.
Scott Benner 2:33
Nice to meet you. Thank you. Thank you for coming on and doing this. Absolutely. Two kids. How old are they? Two kids.
Laura 2:41
They are seven and nine. Seven and nine.
Scott Benner 2:44
Wow. How old are you? 45 congratulations. That's a lovely little family. Yeah. Thank you very nice. How old was the one who got type one when she was diagnosed?
Laura 2:56
So it would be the nine year old, and she was actually it was her third birthday. She spent her third birthday in the hospital. Oh, gosh, six years ago. Yeah, almost
Scott Benner 3:07
seven. Almost seven. Okay, yeah, yep. What precipitated the hospital visit the typical
Laura 3:14
signs like drinking a lot, using the bathroom a lot, soaking through her diapers and the night before we actually took her in, I was like, telling my husband, because I'm, like, a big Googler, so I was like, Don't Google it, because it says diabetes. And we kind of like, chuckled, because I'm also like, I think of the worst case scenario. So in that case, it was actually right. But so we took her in. The next day, I think I was going to take her to the walk in. Yeah, I was going to take her to the walk in. And she was with grandpa, and grandpa was like, she's complaining her legs hurt. She's not acting right. So we took her to the doctors that day, and they did a urine test, and the doctor came in and was like, What's up with her sugar? It's It's really high. And I was like, what? Oh, my goodness. The rest was kind of history. So next thing we know, we were actually, I think I must have been in denial, because I went back to work, and my husband took her to the emergency room, and they did the blood test there, and her blood sugar was 978, oh my gosh, yeah, crazy. So they ended up going to the nearest Children's Hospital, which was an hour and a half away, and he's trying to contact me, and I'm a social worker, so I was in sessions, and I didn't check my phone knowing all of this was going on. I think I was like, in a state of denial. I was like, No, it's not, she's fine, and then he's like, we're an hour and a half away. What are you doing? So I had to go up to to go join them, and that was kind of the start. And that was like, right before her third birthday. So she was in the hospital for her third birthday.
Scott Benner 4:57
Was your youngest even around at that point?
Laura 4:59
Yes, she. Was Yeah, so I had to make arrangements for her.
Scott Benner 5:03
Yep, she's a baby, right? Yeah, oh yeah, not that the three year old is not a baby, still, but yeah,
Laura 5:08
wow, yep, she was very Yeah, very little, yep.
Scott Benner 5:12
There any sign of other autoimmune issues or type one diabetes in your extended family?
Laura 5:17
Well, my husband side has Hashimotos. My husband's celiac. My daughter's also celiac as well. And on my husband's side, there's also Graves disease.
Scott Benner 5:30
They have graves Hashimotos and celiac.
Laura 5:32
Yes, yeah. I wish I would have known that before I married them.
Scott Benner 5:36
Laura's like there were other boys talking to me,
Laura 5:39
yeah, and I didn't know that until I started listening to your podcast, though all these things, I was like, Oh my goodness. It was like, just waiting to happen.
Scott Benner 5:47
Yeah, I'll tell you right now. If you've got type one and your boyfriend's family is running to the bathroom after they eat, just pick a different guy, right?
Laura 5:54
Yeah, absolutely, yep. Very true.
Scott Benner 5:59
What's your remembrance of the time in the hospital.
Laura 6:02
It's okay. I was trying to sit down last night and think about things, and I think it's kind of a blur, because there's a lot of medical stuff that I can even talk about prior to the to the type one. So we had been at the hospital, like, a year before, when she was almost two, she had to be airlifted, actually, from our local hospital because she had a respiratory virus that sent her like took her to the walk in, and her while we were at the walk in, her lip turned blue, and all of a sudden, we're in an ambulance. They're bringing us to the hospital. It was crazy, and she ended up being intubated when she was almost two years old. Oh, good. And airlifted so that it was the same hospital. So here we were, like, a year later, you know, with a new diagnosis, you know, diabetes. And I was like, Oh my goodness. So it was a little bit traumatizing just being there after, you know, a year prior, we had this, you know, helicopter experience that we were later had to fight a bill of like $65,000 which we got all of that resolved. But, you know, it had just been a long year of trying to fight
Scott Benner 7:12
that it cost $65,000 to fly on a helicopter.
Laura 7:16
Yeah, apparently, yeah. That seems crazy. Yeah, yep. My husband's a very low key kind of guy, but he panicked. He's like, How the heck are we gonna pay me $65,000 for this, you know, Air flight? And I was like, we're not, we're gonna fight it, you know. And we did, and it took a long time, but so it had been a whole year of just getting over that that was very traumatizing, you know, just that whole experience. And then here we are at the same hospital, you know, doing something different. And I was glad that she went because, I mean, she wasn't, thankfully, in DKA, but I think she was in the start of it, because her a 1c was like, 12.4 they told us,
Scott Benner 7:55
so, wow, no kidding. Yes,
Laura 7:56
I know. Yeah.
Scott Benner 7:58
What were her symptoms that day? Like, the day you were like, hey, something's wrong.
Laura 8:03
Well, grandpa was saying her, she was complaining her legs were hurting, okay, but it was just leading up to it, you know, just a lot of the excess thirst, yes, like, and then soaking through her she wasn't potty trained yet, but just soaking through her diapers.
Scott Benner 8:19
Wow, that's something. So, yeah, so they get her straight, right? How long she in the hospital for
Laura 8:24
was only a few days. Yeah, we actually had, my other daughter was getting baptized that Sunday, and I think she was in the hospital that Thursday, so we were there Thursday night, Friday, Saturday, and they, they released us Saturday, you
Scott Benner 8:41
still did the baptism. Oh, yeah, we did. Yep, we sure did. Are you Catholic? My husband is the most Catholic thing I've ever heard in my life. Yeah, we Yeah.
Laura 8:51
Well, you know, the endocrinologist said, Go do it. Just do it. Live a normal life. So there we were, you know, and we went out of the hospital. We were MDI for probably about a year. So we were giving her shots, poking her finger, doing all the things. Like, newly diagnosed was kind of a crazy, yeah,
Scott Benner 9:08
go live a normal life. Like, oh yeah. I don't know if you realize my three year old just got type one, yeah. Not gonna be all that normal. But okay, thanks, yeah.
Laura 9:16
And I remember being at the hospital, being very overwhelmed, like, just throwing all this information. I'm terrible at math, and I remember we were trying to do the numbers, and I kept getting it wrong. And I wasn't too happy with the diabetes educator that we had. She, I thought was a little harsh in the hospital. Yeah, yeah. She wasn't my favorite. But what struck you as harsh, I think because, first of all, I was hungry, so I felt like my blood sugar was dropping myself because I hadn't eaten in a while. And I was like, Can we take a break? And she's like, No, we have this allotted time. You gotta do it, you know? And she just threw a lot of information at us. I felt like in not in a very kind way either, you know, it was more informational. But there. Didn't feel like there was any sensitivity to the fact that, like, we just threw all this, yeah, right, it felt cold, yes, yes, it did definitely.
Scott Benner 10:09
You're like, I need a hard pretzel. And she's like, too bad lady, we got 45 minutes, right, right? Yeah. Tell you a bunch of stuff that you're not going to remember that's not going to end up being that
Laura 10:19
helpful anyway. I know, right? It's very true. Yeah,
Scott Benner 10:23
you said you like to Google. So six years ago, how did you launch into all this? It's not from what she talked to you about, apparently,
Laura 10:29
no, and actually, it took me a while. My husband took on a lot of the care initially, I think because, you know, I had a baby. When my daughter was initially airlifted. I was pregnant with my second daughter, and while we're at the hospital, I was like, Gee, something doesn't feel very right, so, but I was like, I gotta just, you know, be here for my older daughter. And so then I got back after she was, you know, finally getting better, and I went to my OB, and I found out that I had low amniotic fluid, so they ended up sending me to the hospital a few days later, and I was on bed rest at the hospital for two weeks before my second daughter came, who came
Scott Benner 11:14
that like making pasta with not enough water in the pot. Like, how does that work? Like, what happens?
Laura 11:19
Yeah, well, it's just so I had what's called intrauterine growth restriction for both of my girls, both of them were born early. The oldest one, who has diabetes, was was born four weeks early. She was very sick from the very beginning. She was in the NICU for 30 days. How premature was she? Four weeks, four weeks, yeah, so she, yeah, I think she was, like, four pounds and so many ounces, yeah, just little, but not as little, actually, as my second one. But she had a lot of respiratory issues from the very beginning, the first couple days of her life, we couldn't even, like, touch her. She was so fragile that they put signs, you know, in her little incubator, thing that said, please do not touch because she was so fragile.
Scott Benner 12:08
Wow, when you said she was sick from the beginning, what else happened?
Laura 12:12
Well, it was, it was basically the respiratory stuff. So, right? So I pretty much went to my normal OB appointment, and I was getting an ultrasound, and the lady's like, when are you going to go see your doctor? And I was like, Well, I think I have an appointment in a couple of days. Next thing I know, my doctor comes in and is saying, Nope, you got to go the hospital right away. So it was, Everything happened so fast. It was an emergency C section, you know, they took her, then she ended up being in the NICU for 30 days. So it was a lot of back and forth. You know, 30 days of not being able to bring your baby home, which is heartbreaking, and not even being able to touch her the first few days was also very hard.
Scott Benner 12:53
Yeah, other women in your family have trouble giving birth. There's no thing there. No, yeah, were you older than you would have liked to have been when you got pregnant? I don't like what's the math on that? Is that part
Laura 13:05
of it? I was 35 Yes, yeah, my husband, we'll just throw him under the bus for everything. He'll love it when he listens to it later. No, my husband's a little bit younger than me, like, four years younger than me, so I wanted to get married and start a family, and he was, you know, a little bit younger. So I think we dated probably four years before he proposed, and that probably was a little bit longer than I would have liked.
Scott Benner 13:28
But your good years is that what he does?
Laura 13:32
Yep. So I had my first one at 35
Scott Benner 13:35
see how smart that is of him. He holds you a little I almost said, past your expiration date, but I don't mean that he holds you a little longer, so you're limited in your options now you have to say yes to him when he asked you smart, yeah, yep.
Laura 13:52
Then I should have asked him his family history, because then all this comes out.
Scott Benner 13:56
No, why does your uncle's eyes pop out like that? I need to understand a little better. Oh, well, how about the you know, the six years since, like, since the diagnosis, has she been on a better track, or she's still been suffering with issues? The Dexcom g7 is sponsoring this episode of The Juicebox podcast, and it features a lightning fast 30 minute warm up time that's right from the time you put on the Dexcom g7 till the time you're getting readings, 30 minutes. That's pretty great. It also has a 12 hour grace period so you can swap your sensor when it's convenient for you. All that on top of it being small, accurate, incredibly wearable and light. These things, in my opinion, make the Dexcom g7 a no brainer, the Dexcom g7 comes with way more than just this, up to 10 people can follow you. You can use it with type one, type two, or gestational diabetes. It's covered by all sorts of insurances and, uh, this might be the best part. It might be the best part alerts and alarms that are customized. Possible so that you can be alerted at the levels that make sense to you, dexcom.com/juicebox, links in the show notes, links at Juicebox podcast.com, to Dexcom and all the sponsors. When you use my links, you're supporting the production of the podcast and helping to keep it free and plentiful. Today's episode is brought to you by Omnipod. Did you know that the majority of Omnipod five users pay less than $30 per month at the pharmacy? That's less than $1 a day for tube free automated insulin delivery. And a third of Omnipod five users pay $0 per month. You heard that right? Zero that's less than your daily coffee for all of the benefits of tubeless, waterproof, automated insulin delivery. My daughter has been wearing an Omnipod every day since she was four years old, and she's about to be 21 my family relies on Omnipod, and I think you'll love it, and you can try it for free right now by requesting your free Starter Kit today at my link, omnipod.com/juicebox, omnibus, Omnipod has been an advertiser for a decade, but even if they weren't, I would tell you proudly, my daughter wears an Omnipod. Omnipod.com/juicebox Terms and Conditions apply. Eligibility may vary. Why don't you get yourself that free starter kit, full terms and conditions can be found at omnipod.com/juicebox
Laura 16:22
Oh, yeah. So she had, well, she's very small, so she has some growth issues. Which part of that they say comes from the intrauterine growth restriction that I had. So basically, that's you, your baby just can't grow in the womb. And that was a big part of why they had to take her out, too, because I had low amniotic fluid with her, like, severely low with her as well. So she's very tiny for her age. And we've, you know, talked about maybe doing like, a growth hormone, but you know, for right now, we're just kind of letting her be, and she doesn't mind being so small. So you
Scott Benner 16:58
contextualize that for me, how, like, how tall is she? Well, so she, she'll
Laura 17:02
be in fifth grade. She looks like she's about in second or third grade. I would say,
Scott Benner 17:08
okay, is she thin on top of being short?
Laura 17:11
No. I mean, she's actually at a good weight. It's more her, her growth, that they're just kind of watching. So she has had some growth testing done, okay, you know? And I mean, they said she was at the very lower end, but like, her growth hormone does appear to be working. So that's a positive thing. Also, the celiac can affect growth as well, so
Scott Benner 17:31
hard to take in nutrients. Yes, yeah, yep, any Hashimotos or anything like that,
Laura 17:37
just so far so good. Yeah. And how about your other
Scott Benner 17:41
one? Is she? Is she small too? Yes, she's yep, yep, same thing. Are you
Laura 17:47
I am. Yes, I'm tiny as well. Yep, you're Italian. I'm Italian. So Well, my father was born in Italy, so my dad's side were all very small.
Scott Benner 17:58
No kidding. Oh yeah. You know, it's funny. I remember when, when my son was young, there was this 10 year old boy on his baseball team, and he was a monster, and, like, just so much bigger than the other kids, and stronger and everything taller. I remember saying to his dad one time, wow, man, he might really pop up. And the guy his absolute quickest right off top is that answer, he goes, No, we're Italian. That's as big as he's gonna get. Well, gonna get. And I thought, like, oh, I don't know what that means, like, you know, because I have a lot of context for it. But no kidding, I met that kid eight years later. He did not get much bigger, right? Yeah, right, yeah, yeah. Really something else. He's now the smallest adult I know, yep, but he was the biggest 10 year old I ever seen in my life, right? How do you manage with diabetes? Like, are do they give you a set of instructions and some like, I don't know, they give you a pen. They give you CGM. Like, what do you know about it? What? How do you learn more?
Laura 18:53
Right? So we initially were MDI for about a year, I would say, and a lot of that was our insurance. We were trying to think last night when she got the CGM, I would say, probably about six months, because I can remember doing like, finger checks in the middle of the night for quite a while. And we were actually just looking at my husband had recorded some of her when we had to log it on the little logs, like, some of her numbers. And we're like, Whoa, she was high a lot. We were like, but you didn't know, like, you know, like, in the middle of the night, you know, you were just like, saying, oh, things got better. We didn't know in between what was happening, you know.
Scott Benner 19:31
So you wanted to CGM, but your insurance was stepping in the way even, think we even knew really about it, yeah. Well, what do you think was holding you back then? Like, just the general knowledge, like, so you were like, Hey, I have a meter and I have these pens, and this is what
Laura 19:44
diabetes is. Well, right? Because I'm a rule follower, so if they were telling me to do this, you were gonna do Yeah, and I think they were saying your insurance will let you, like, in six months, get us and then get a pump after so we didn't even, we didn't know, we didn't know anybody with type one. We didn't question anything. Yeah, you know, so we just went with it.
Scott Benner 20:03
How do you figure out the next steps? Is it just that time passes and they offer you a CGM. Diabetes comes with a lot of things to remember, so it's nice when someone takes something off of your plate. US med has done that for us when it's time for Arden supplies to be refreshed, we get an email rolls up and in your inbox says, Hi, Arden. This is your friendly reorder email from us. Med. You open up the email. It's a big button that says, Click here to reorder, and you're done. Finally, somebody taking away a responsibility instead of adding one. Us. Med has done that for us. An email arrives, we click on a link, and the next thing you know, your products are at the front door. That simple us, med.com/juicebox, or call 888-721-1514, I never have to wonder if Arden has enough supplies. I click on one link, I open up a box, I put the stuff in the drawer, and we're done. Us. Med carries everything from insulin pumps and diabetes testing supplies to the latest CGM like the libre three and the Dexcom g7 they accept Medicare nationwide over 800 private insurers, and all you have to do to get started is call 888-721-1514, or go to my link, usmed.com/juicebox, using that number or my link helps to support the production of the Juicebox podcast.
Laura 21:34
Yeah, I can remember being at my daughter's Halloween parade and my husband's like they just said, we can, you know, schedule our pump classes. So I'm gonna do it, you know. And and then, like, shortly after that, we had the pump class, which I didn't even go to. I think he went to that one. And then there we were, is
Scott Benner 21:53
that the setup for the family in general? Like, is he a little more hands on? Like, do you have a busy job? Like, you, I mean, it's weird, yeah, yeah, you know, I'm just wondering, because you've said twice now,
Laura 22:03
yeah, no, I think because I was just in this state of there was so much that had been going on, like, medically, you know. And I had my kids, you know, and then I had, you know, some, probably some postpartum issues, I would say. So I think I was just kind of met with it for, like, several years, you know, it was like I got pregnant, had a baby, and then was nursing and all the hormones with that, and then, like, a year later, get pregnant, and then, like, starting again, you know, and then when I had, when I was pregnant with my second one, I ended up Getting a blood clot in my leg, jeez, I know, yeah, and it was all this was all after the older one had been airlifted, right? So all this happened within like a month. It was just crazy. So I had to deal with that, you know. So I think it was just all of that, you know, we were just kind of surviving all of this other Yeah,
Scott Benner 23:00
if I asked your husband, do you think he'd say, look, I couldn't have given her one more thing. Like, yeah,
Laura 23:06
yeah, yeah. So he was the one a lot of times. Now it's kind of reversed. He was the one staying up in the middle of the night, you know, and just checking your finger a lot of times, you know. And just, he would go to all the all the appointments, you know, and for a while there was covid, so only one of us could go. And so I didn't really get involved as much. I knew the basics with her diabetes, I would say, until probably halfway through, you know, we're moving on to seven years now. And then I started really getting invested into it.
Scott Benner 23:40
Do you think you just kind of lifted from a fog or I
Laura 23:42
think so really, yeah, yeah. My other daughter ended up having hip dysplasia as well. Jesus, because I know it was like all this stuff. She both of my girls were breech, and so we had them just evaluated, like through early intervention, because they were premature. And the physical therapist that was doing the evaluation actually noticed her hip and was like, did they ever have, you do a, you know, a hip X ray? And I was like, No. And they're like, well, they should have, because if she was breech, you know, breech babies are more likely to have this. And I was like, oh, so then we had her x rayed, and then, yep, she had hip dysplasia, so she had to have this big spike of cast for quite a bit of time, and then we had to follow an orthopedic, pediatric orthopedic doctor, and then it didn't stick. So then we had to repeat the spike of cast, like, a year later. So there was just, like, a lot going on, like all the time that I think I just couldn't take on all of it at once, you know.
Scott Benner 24:43
And you're a social worker on top of that. So you're also, yes, you're professional, you're taking on everybody else's problems
Laura 24:48
too. Yeah, it's very true. Yes, yep, yeah.
Scott Benner 24:52
The breech birth brings on the possibility of, like, dislocated hips. So I asked, like, what else does it do? It's interesting. Birth. Injuries, risk of broken bones, dislocated hip, nerve damage during vaginal delivery because of the head comes out last umbilical cord issues, it can become compressed or prolapsed. Head entrapment, some possibility, oxygen deprivation, hip dysplasia, respiratory problems and deliveries. If delivery is prolonged, the baby may inhale fluids or struggle to breathe right away. Wow, crazy. Yeah, why did they come out? I wonder why. I'm asking
Laura 25:27
you, I know, right?
I don't know. I'm like, geez, I guess my that's why I'm like, I'm done with after two. Because I was like, geez, there's no more. Who knows what will be wrong with this if I had a third one ever?
Scott Benner 25:40
We're getting a cat, that's it.
Laura 25:43
Yeah, yeah.
Scott Benner 25:44
Factors related to the baby, I because I asked, like, why to breech birth happen? Prematurities, one rarely issue, although abnormalities rarely issues with babies brain, spine or muscles, can affect movement and positioning. Excessive or limited movement. Some babies just move differently. Too much or too little activity in the uterus can affect the uterus can affect the positioning on the mother side, uterine shape or abnormalities. Placenta previa. If the placenta is low lying or covering the cervix, it can block the baby from moving into the head down position, oh. Amniotic fluid levels. Too much. Fluid gives extra room for the baby to move. Sometimes, leaving them in Bridge too little restricts the movement. Oh, so maybe when it's time to go head down,
Laura 26:26
there's not enough room or something, yeah, yeah. And that's something who
Scott Benner 26:30
would know? Well, I mean, I know. Who would know it's the internet knows.
Laura 26:33
Apparently, yeah, wish I would have, like, done my googling while I was
Scott Benner 26:38
I'll be honest with you, that was AI, that wasn't Google, yeah, yeah, okay. Well, she's doing well, you're alive. That's good news.
Laura 26:46
I know Yes. And so the older one also has one more thing to add to it. I don't even know how to pronounce it, but I'll give you it's e, o, e. So if you look that up, it's like, basically inflammation in her esophagus.
Scott Benner 27:00
Oh, yes. So long has that been? That's been
Laura 27:05
a few years. So she's had five, I can never say if it's an endoscopies. She's had five of those. She now takes, like an oral steroid that we like mix in with some applesauce that like sticks to her esophagus. And right now her like, inflammation levels are pretty much non existent, so it seems to be working, but the oral steroid can also cause some growth issues too.
Scott Benner 27:32
Oh, that's unbelievable. Yeah, yeah. EOe, yes, yeah, I'm looking at it right here, chronic inflammatory condition of the esophagus, common symptoms, trouble swallowing, especially solid foods, food getting stuck in the throat or chest, chest pain or heartburn, not relieved by typical reflux treatment, abdominal pain, nausea or vomiting in children, feeding difficulties, failure to thrive, picky eating linked to food allergies can also be influenced by environmental allergies, not caused by one single factor. Jesus, I know, right, yeah, yeah, no wonder you're not all right. I know. Hey, being being a social worker, yes. What's it like professionally, understanding the things you're going through personally.
Laura 28:22
It's crazy. I could say that, yeah, well, it it makes me first of all appreciate what people go through, but also recognize how important it is to take care of yourself, you know. So I've had to do a lot of my own work, you know, in order to be like a better social worker for other people. But can
Scott Benner 28:41
you see yourself in the moment? Like, can you not always? Yeah, right, yeah. It's not like you're going through something. You're like, oh, what would I tell another person who's experiencing this right now?
Laura 28:50
Right? Yeah, yep, yeah. Well, that sucks, yeah, yeah.
Scott Benner 28:54
It's like being a mechanic that can't work on their own car, but a waste, right? Oh, wow. And that must be frustrating, because I imagine at some point you have a come to Jesus, and you go, Oh, this is what's been happening to me. I can't believe I didn't see this sooner.
Laura 29:09
Yeah. Oh yeah. Absolutely. They make you
Scott Benner 29:11
feel like a fraud a little bit.
Laura 29:12
Oh yeah, sometimes, yeah. But now, now I feel like I'm taking the steps that I need to to really, you know, get myself together. And I think one of the things I wanted to talk about for me was, I think for me, the grief with the diabetes came later. I think because I was in such a fog initially, with everything that it didn't hit me, probably to, like, three years later, when I really had to come to terms with, like, this diagnosis, interesting.
Scott Benner 29:41
So 36 months, three years into your kids type one diagnosis, you think the weight of it just started to
Laura 29:49
impact you? Yeah, definitely.
Scott Benner 29:52
You said earlier, like, you're like, she got that diagnosis, I think I was in would you say denial, because I went back to work because I was.
Laura 30:00
Worked a whole day. Didn't even, like, think about it, you know. And and my husband's like, calling me, leaving me messages, like, we're going to the Children's Hospital an hour and
Scott Benner 30:08
a half. Okay? You're like, I got work, buddy, it's Wednesday. No, it was very
Laura 30:12
bizarre, you know. But that must have been my coping mechanism at that point. I think
Scott Benner 30:18
so, when it hits you three years in, What's that feel like? What's the experience?
Laura 30:23
It was very overwhelming. Yeah, I think, you know, as she got a little bit older, too, just realizing, you know, if you go to a birthday party, or just sometimes the differences in things, you know, or all that, just all the stuff you have to bring, you know that I'm like, Ah, when I take my other child places, I don't have to, you know, do all of this, it's such a weird feeling. Like, if I take my younger daughter, you know, to go out to breakfast, I'm like, Oh my gosh, we don't have to pre ball list. We don't have to, like, keep an eye on that. Like, it's just, like, a weird feeling, you know, that
Scott Benner 30:57
happens. I try so hard not to live in it. Yeah, you know what I mean. You know, like, I know what you're talking about. Like you head out for something and you don't have a bag with you, or you're not, you're not thinking, like, is there a Juicebox in the door of my car?
Laura 31:11
Weird feeling. It's a very weird feeling, right? Yeah,
Scott Benner 31:14
I, for me personally, like I never wanted to feel like that was better, right, right? You know,
Laura 31:19
it's just different. It's just a different Yeah, right,
Scott Benner 31:23
yeah. So you're having kind of a delayed reaction to the type one absolutely,
Laura 31:29
yeah, yeah. Have you
Scott Benner 31:30
done this with anything else in your life? Don't think so. No, no, yeah. Do you think of yourself as a as a person who's easily knocked down by problems, or do you think yourself is more resilient?
Laura 31:43
I think that's a good question. See, now you're gonna therapy
Scott Benner 31:48
me. I'm a, you know, just a podcaster, but
Laura 31:51
yeah, no, I think I have some patterns that are more like catastrophic in that. So I'm always thinking like the worst case scenario of things and an urgency sometimes with things that aren't always needed at times. But I think in the moment of things, like when all of this was happening, like with my daughter, I don't think I didn't panic, like it wasn't like a panic all the I think in the moment I can handle it. It's like, afterwards, you know, would you
Scott Benner 32:26
call that compartmentalizing? Yes, oh, totally right, yeah. You know, if people, if people are listening closely, like, I am Laura, you said in the very beginning, like, don't google it, because it's going to tell us she has diabetes. Yeah, yeah. That's a very strange way to think of problem solving. Because what you might want to say is, hey, why don't you go do the research I just did, because I think you might come to the same conclusion, and then we need to get her to the hospital. Yeah, right. But you were like, no, don't look. If we don't look, we can live here longer. Yeah. Yeah, right. Yes. Really is something okay. So what would you tell a person who came to you and said what you said to me?
Laura 33:08
First of all, trust your gut, right? So I think another thing that's been an issue for me is when she had her respiratory issue and then she had to be airlifted, I had thought in the middle of the night, something's not right, like, we had been giving her the nebulizer, and I was like, she should be getting better, and she's not, you know. And so we had come to the decision, oh, it's your first baby. You don't always know what to do, but we came to the decision that we would wait till the morning, you know. So I have a lot of guilt about that, because I think what if we would have taken her like right in the middle of the night, instead of waiting so many hours to take her to the walk in when her and then her lip goes blue, you know?
Scott Benner 33:50
Well, what? What do you think going earlier would have garnered accomplished? I don't know, right, just it could have been something. It could have been, right?
Laura 33:59
My brother in law is a doctor, and he said it, you could have still been in the same position, like, we don't know, you know. So try not to be yours. I think it's, you know, being a mom, I have a lot of guilt about that, which I think has transferred sometimes with diabetes. Like, now I'm like, I can't let this happen. So we gotta keep our numbers really in control. You know, it's like more of a control thing suddenly, again, a delayed response, because I wasn't that way initially.
Scott Benner 34:27
Yeah, no, you were trying to, I don't know exactly. And people online have pointed out that I'm not a therapist, and I'm not saying I am. It feels to me like maybe you were just trying to not make it real.
Laura 34:38
Yeah, right? And I also didn't know enough about it, you know? I mean literally at the hospital, they're like, she can eat whatever she wants, you know, you can live a normal life, you know. Just give her insulin, you know. But nobody again, was telling us, like the impact of food and like, you're gonna need a crap load of insulin sometimes, for certain things, like, nobody taught. Us that, you know. So I think I thought we were doing we'd go to the endocrinologist, and they were like, you're doing a good job. I didn't, we just didn't know any better until I started. I think what hit me was like, if something happens to my husband, he's the one doing the majority of this, we're doomed, like, I need to know what I'm doing. So I started reading and, you know, really educating myself, and that's when things really started to kind of shift, I would say, even with her diabetes care, because then I would pass the information along to my husband.
Scott Benner 35:33
Your husband's gonna love this. When he listens, it's like, all right, you just woke up one day and you're like, Oh, what if a safe balls on his head, like in one of those Road Runners, and then I'm gonna be stuck here with this kid I don't know anything about. I I'll go figure it out. Then, did you explain to him? Then he was doing it wrong?
Laura 35:49
No, I don't think so. I think I I just sometimes I talk, I get excited about things, you know. So if I like, listen to the podcast, I'll like, tell him. And sometimes he's just like, stop talking about diabetes. He would definitely say, I talk about diabetes too much. You know? What would you say? I would say, sometimes I do, but sometimes I'm excited, like, if I learn something, or I like, am following the trends, and I'm like, Oh, I think I finally, like, it took us a long time to figure out breakfast. Like she would go high constantly after breakfast, and I finally figured it out. And like, I was so excited, and now that she's doing amazing after breakfast, so I get excited. So I like want to tell people like we did it, we figured it out. Like, you know,
Scott Benner 36:35
I think of that excitement as the one step closer to it being less of a front and center in your mind, less of a burden? Yes, yeah, if we could figure out all these different things, then maybe it would actually feel normal, the way people are. People saying that it could feel normal. Because, right? What they Oh, you can live a normal life. Well, it's a normal life, but you're going to be managing diabetes, so not, uh, not completely normal, right? I get what they're saying, like, there's no reason you can't have a job or, you know, like, something like that, or do something that you wanted to do, and I completely agree with all that, but it's still not normal to have to take a bag with you everywhere, or not normal to have to tell your kid, like, hey, like, you know you're gonna have to take insulin because you're gonna be gone for five hours and you're going to be too far from home, like, that's not normal. It becomes, becomes normal, right? Yeah. So I would think that that excitement, like for me, would mean maybe we're one step closer to this not being as front and center in our head all the time.
Laura 37:37
Yes, yes. That's very much it, yeah. And just like, figuring things out, I think because my brain works much differently than my husband's, you know, so I'm trying to figure this out, like, so I'll take it on as a project, and, like, okay, breakfast was like, my baby, because I was like, we're gonna get it, we're gonna figure it out, you know, my husband would be like, yeah, it's not so bad. And I'm like, Nope, we're gonna get there. We're gonna, you know, and and even with that, you know, it's like, this morning, I'm like, okay, brand new pump site. We have to do a little bit more than normal, but sometimes the pump sites seem to be working really well. And if I do the normal it's almost a little bit too much. So it's almost like, like, my brain wants it to be. Every day we do the same thing over and over again, but it's just, it's certainly not that, right? I've learned so there's so many variables, you know, and it's like, ah, sometimes I'm just like, I don't want these variables. And sometimes I don't even know what these variables
Scott Benner 38:30
are. So how much of it is, like, also, you're a little older too, yes, yeah, right. Like, so you start getting into that. I mean, I feel you on that, like, I'd like this not to be so much work all the time. Yes, yeah. I don't mean the diabetes. I mean being
Laura 38:45
alive, yeah, oh yeah, yes, yes, absolutely, yeah.
Scott Benner 38:49
The part where this is, like, fun or right, or easy once in a while, and I know, for me personally, like, I don't want that to be when I'm 70, right, sure. Like, I'd like to wake up one day and, like, just have, like, a free and easy day. That's, you know, enjoyable by Scott, who's fully mobile and can grasp the world.
Laura 39:08
Yeah, yeah. And that's, I think, one of the things when you have kids a little bit older, like, you know, you're wiser, but like, you're tired. Like, I always tell me how I'm tired. Like, my little eight year almost eight year old wants to be running around. I'm like, I'm tired like
Scott Benner 39:23
that. I find that stuff insane. I was talking to somebody recently who had a baby around my age. I was like, I don't even, I don't even understand, just tired, yeah? Like, Hey kid, here's $50 like, good luck, right? Yeah, don't buy crack with this. And then I Daddy's gonna take a nap. I did the last night thing, I didn't go to bed till late, but I got tired early, even that's weird, like, you know, like, yeah, oh yeah. At 10 o'clock, I was like, I should go to bed, yeah. And then I couldn't do that because I'm an adult and I've got responsibilities. I was still working. Like, you know what I mean? Like, after I got done working, I was cleaning things up. Like, you know, I other. Stuff I needed to be doing. I'm doing that. Yeah, my wife's still working. Like, you know, it's like 1030 my wife's working, and I'm cleaning something up. I should have cleaned up six hours prior. Arden's out with friends saying goodbye, because they're all heading back to college. Yeah, you know, my son's in the basement lifting, you know, everybody's like that. We have a dog. The dog has to go out. And all I could think is, I should go to bed. Yeah. And then by the time I got through all the things I was supposed to be doing, and everybody got back in the house and was kind of settled and everything, I wanted to watch an episode of Mr. Robot. I'm trying to watch Mr. Robot. It's 1230 like, am I gonna sit in my bed under a blanket like I'm 10 watching an episode of Mr. Robot on a right? I guess I am. Yeah, no. I just feel like once you start getting older, like you said, again, like your mind, like your thoughts are clear, Yeah, but you're like, you're like, why couldn't I have been this clear minded when I was, like, had the energy of a 25 year
Laura 40:53
old? Yeah? It's very
Scott Benner 40:54
true. Yeah, sucks. Everything's backwards. I see what you just Yeah,
Laura 40:57
thankfully, my husband has a lot of energy, so that's helpful, yeah? Except he cannot. He does not hear the alarms a lot of times at night. I even bought him the sugar pixel, and I have seen him just hit the button and or unplug it and then just go back to bed, and he doesn't even remember a lot of times that he's done that isn't that interesting, yeah? Whereas me, I'm, like, a very light sleeper, so I am like, up constantly, I hear a little noise, and I'm like, I think it's just a mom thing. I don't know.
Scott Benner 41:27
How's that ego boost getting a younger guy? How was that? It feel good?
Laura 41:31
Or no, no, because he, you know, I wanted to get married. I knew going into it, I'm ready to get married. I want to have kids, you know. And he what? How he was 25 I think when I met him. So, you know, we were in different life stages, but you take advantage of his exuberance. Yeah, now it's, you know, a good thing probably is, you know, maybe he'll live longer than me. I don't know. We'll see
Scott Benner 41:56
Jesus. Laura, you are a bummer. What are you always worrying about the worst thing that's gonna
Laura 42:00
happen? It? I, I'm working on it. How about that? I'm trying to work on that.
Scott Benner 42:05
Is that since, is since the Life Flight, or is your whole life?
Laura 42:08
I would say there's been some patterns in my family that have been that way, you know? So probably some modeling. Yeah, everything's always terrible, yes. But the other thing is, yes, the Life Flight really, like, shook me up, I think, in ways that I didn't even realize.
Scott Benner 42:26
Maybe it took those feelings that you're you grew up with, with your family, and made them feel like, well, yeah, see Yeah, if they were right, bad
Laura 42:32
stuff happened. Right? Yes, yeah. It was like, I think that realization that, like, yes, bad things in my mind before, like they could happen, but now they were, and it was, like, constant, like, every time I turned around, I'm like, now I have a blood clot. Now we have this. Now I'm like, Oh my goodness. You know, it was crazy.
Scott Benner 42:52
Would it not help you if you could think of those things not as bad things happening, but that every day in life isn't perfect, and you just gotta bob and weave a little
Laura 43:02
Yes, yeah, I think I'm trying to again. That was another thing I wanted to talk about. Was like, just some perfectionist tendencies, which I didn't even realize I had until, you know, I suddenly became involved in this diabetes world, and my husband was the one that pointed it out. He's like, you're trying to be perfect with her numbers, and this is driving us crazy,
Scott Benner 43:24
you know, you didn't know that about yourself.
Laura 43:27
I didn't know because I wasn't like the kid in school, like I was fine if I got, you know, an 82 or something. I did terrible on tests. Like, to me, it was more important to be around people, you know, I just wanted to be with my friends, be involved in things I didn't have to have, like straight A's. So I think in my mind, that's what I always thought, like a perfectionism was, you know, and I wasn't that way of my work either. It was just suddenly that
Scott Benner 43:53
person's healthy enough, that's good, we're done, right? Yeah, did you call an 82 a terrible grade?
Laura 43:59
No, I didn't. Yeah, no, that's a great grade. Yes, yeah, other people might think, right? But, you know, my sister was very, you know, book smart. She, you know, very intelligent. Her grades were very important. I was just different, like, to me, it was, you know, I wanted to do well in school, but I also wanted to play sports and have fun, and so it wasn't like top priority for me.
Scott Benner 44:22
Did your perfectionism show up in other ways through your life? Or do you think that you had a touch of it and then the mom guilt, plus the medical stuff equals where you are now?
Laura 44:34
It just plowed through with the diabetes, like my husband was, like, all of a sudden, like she used to be 350 and this was never an issue for you. Why? All of a sudden, you know, she's 180 and you're freaking out, you know, like he's trying to, like, wrap his mind around, like, the change, you know,
Scott Benner 44:51
was 350 not a big deal for him. Or is he trying to say that back before we knew this was a problem, right? Yes. But then the simple. Answer to his question is, well, now we understand it better.
Laura 45:02
Yes, right? And that's what I try to say all the time. Like, now we understand so now, you know, we just didn't know before,
Scott Benner 45:10
and now we know that's a problem, so now we need to stop it. Yes, boys are confusing. Yeah, I don't understand boys. Sometimes I do the same, by the way, I'm lumping myself. I do the same thing. Like, like, the things that like don't occur to me. I'm like, oh, like, when I look backwards, I'm like, how did that not strike a chord quicker? You know? Oh, by the way, I just noticed Laura. My calendar on my whiteboard says 2024 and it's, uh, August of 2020 Oh,
Laura 45:38
my goodness, yeah, right.
Scott Benner 45:41
That's funny. So much writing on the board in other places, but I apparently never changed the date. It's staring right at me. How did I never notice that before? Oh my gosh.
Laura 45:49
Oh my goodness. Oh. And I I thought of one more thing that she has too. So she also has a severe peanut tree nut allergy, right? So we have an epi pen, the oldest one. Yeah, both of them do, actually, so, but that's interesting with celiac, because a lot of celiac items have, like, is made with almond flour, so we have to always, you know, inspect and make sure there's no almond flour in it. Gosh, I now have a nut allergy. I have a tree nut allergy, but I can eat peanuts. Okay.
Scott Benner 46:21
Is anybody impressed that I haven't made a joke about my wife sometimes having a nut allergy? Oh yeah, I'm personally impressed. I just want to say, oh my gosh, I don't know. Jake, what do you guys like? Live in a bubble? What do you do? I know is that how it feels like, like, because with the allergy and the inflammation in the esophagus thing and the diabetes, and now you layered over top of your newfound anxiety about the entire thing, right? Sure, you sound like a person who's trying to put yourself in a controlling situation, like position, like, how do you accomplish that?
Laura 46:52
Well, now I feel like more confident with diabetes, like we've educated ourselves, you know, we've spent time. We worked with Jenny, who's phenomenal, you know. So we're in, like, a much better place, you know. And all the podcast episodes have been very actually, we've I found the podcast when we switched to Omnipod five. I had never heard of it before, so the first episodes I listened to were like the pro tips on the Omnipod five.
Scott Benner 47:20
Oh, awesome. They've been very, very, very popular. Yeah, yeah. As a matter of fact, if everybody downloaded all the episodes the way they downloaded those, I'd probably be in an I don't know, yeah, I don't know. I think there'd be a lot more people listening.
Laura 47:36
Yes, it's very true. And I always want to tell people like that system, I know gets a lot of slack because it's a little more conservative, but I've studied it and get your settings right and, like, it makes a phenomenal difference, you know, we've gone to the endocrinologist, and they're like, You guys are like, killing it with the Omnipod five. Nobody else seems to get it, but you guys are doing it, you know. So it's very manageable. I think
Scott Benner 48:01
you're having good success with it, yeah, yes, yeah, yeah. Overall.
Laura 48:06
I mean, there's still days where I'm like, Ah, you know, if it suspends the the insulin going into a meal, you know, paying attention to that, I think, is a big,
Scott Benner 48:17
big key. Well, let me say this to you at clinical trials.gov if you look up something called Omnipod smart adjust 2.0 system compared to Omnipod five system in individuals with type one or type two diabetes, strive, you will see that this was last updated on June 11, 2025 and the Study overview says the goal of this multi, centered, randomized cross over study is to evaluate the safety and effectiveness of the Omnipod five smart adjust 2.0 system in individuals with type one or type two diabetes. Study participants will complete about five in person visits and be expected to treat their diabetes per their usual routine using the system at the lowest available target settings. Each participant will begin to study using Omnipod five smart, adjust 2.0 or the Omnipod five system for four weeks period one, and then switch to opposite system for the next four weeks. Everyone will use the Omnipod five smart, adjust 2.0 system for at least four to six weeks during period, three participants will have a goal of administering no more than three meal or snack boluses per day. The official title of this here, blah, blah, blah. What I'm seeing here is they're testing a different version of this algorithm. Yeah, that'd be great. So maybe, maybe all that, you know, I wish it was a little more aggressive.
Laura 49:40
I yeah, that's my only complaint. Is that at times, and I look and it's, it's usually when it says suspended the background, I'm like, oh, here we go.
Scott Benner 49:51
I've been corresponding with somebody whose kid is in the trial, uh huh. And I don't know how much about that I'm supposed to say. So I'll hold on to it. I think the target, it's giving you a lower target. I think that's one of the things that would be great. Yeah. I think there's more coming. Yeah, yeah. I don't think that person wants to talk on the podcast yet.
Laura 50:12
Yeah, yeah. That'd be great, though, that's really my only and I'm learning to adjust. Like, now I'm like, Okay, before she eats a meal, let's, let's look and see how much you know has been paused before the meal, because we got to add a little extra, you know.
Scott Benner 50:28
But what did you do? Did you kind of take your knowledge of how the Omnipod five works, and then listen to the podcast about using insulin, and you're combining the two ideas,
Laura 50:37
yes, and then working with Jenny too has been helpful, too, yeah,
Scott Benner 50:41
and yeah, what would you say that overall you've learned that's been most valuable?
Laura 50:47
Well, I think how food impacts your blood sugar, definitely, I think again, especially with celiac, because a lot of the foods, like the celiac stuff, it hits harder and processed foods, I think, like, we've changed a lot of how we have eaten, which has been wonderful, even for myself, because I used to have higher triglycerides, yes, tri cholesterol, all of that. And mine has significantly come down because just of some of the changes that we've made from eating. You know, just watching her numbers, like, I think just watching the Dexcom when she eats certain things. I'm like, Whoa, what's, you know? I know my pancreas is working, but I'm like, wow, that's got to be doing, you know, wreaking havoc on my body too, you know. So, like, maybe I shouldn't be eating all this stuff sometimes, too.
Scott Benner 51:36
Yeah, yeah. I think if you're paying attention, you there's probably benefits for everybody in the lifestyle and the understanding of how to manage your diabetes,
Laura 51:45
yeah, yeah, yeah, it's been definitely incredible.
Scott Benner 51:49
Yeah, good. I'm glad for you. What do you see as next steps, I guess? Like, where? Like, she's nine now, obviously at this point, like, you have a fair amount of control, but like, that's going to change as she gets older, right, right? What are your goals for the next few years?
Laura 52:05
Well, I think to continue to just manage it the best that we can. You know, I think she'll probably be later with puberty, so that probably gives us a few more years, but hopefully, again, there'll be more like some of the systems, because I do worry about, like, puberty with the Omnipod five. But again, it's just trying to manage, you know, when she's sick. You know, we do different things when she's sick, so just trying to manage some of these situations that come up, you know, yeah, and I think for myself, to just try to enjoy life a little bit more, and that, you know, make it all the time about diabetes and keeping I'd like to keep her under control, but sometimes I think it drives other people crazy.
Scott Benner 52:49
So how does it impact her? Like, what's her response?
Laura 52:54
She's like, a rule follower, like me. So she, I mean, she's amazing. She really is, like, such an amazing kid, like she went at the end of the school year. They went to, you know, baseball game, and this was the first time that I wasn't going to be or my husband, or somebody in the family wasn't going with her. They had the nurse go. And of course, it was, you know, the first day of the Dexcom. So all the numbers were a little wonky. And she's like, Don't worry, Mom, I'll make sure before all the other kids eat, that they Pre-Bolus me, you know. And I was like, Oh, that's so amazing. Like, or she'll tell Grandpa, I'm a little bit high. We should probably, you know, give me more insulin, or wait a little bit longer. Of a Pre-Bolus, like, she's picking up on some things, which I think is, you know, great,
Scott Benner 53:40
okay, okay. Where do you see yourself? Then how do you feel like you can pass on more to her, take some off not maybe not even take it off of you, but come to a balance where she's knows what she's doing and you're at the same time not as
Laura 53:54
involved, right? Well, I think also I need to work on my reactions. Sometimes, you know, like if she's going higher or I still get nervous sometimes with some of the lows, so I might get a little panicky. So I I would like to see for myself, because I know she's watching my reaction to be a little bit more neutral with my reaction to things, you know, and also to help her just to keep understanding the knowledge and how food works, and pass some of that on to her without, I think, making it again too much of like a big
Scott Benner 54:27
thing. What are some of the reactions that you have? I do
Laura 54:31
panic sometimes. If I if she's like, dropping really, really fast, I think I get too panicky. I would like to just be a little bit more neutral. Or if she's like, high, I'll be like, like, the heck, you know, like, I just, I'll make noise. Or I'm just like, you're, ah, you know, like, yeah, my husband's very neutral about things. He's just like him, you know, we know now how to bring her down. You know, it used to be she'd be high for hours. We didn't know what we were doing. Now we're like, okay, something went. Wrong, you know, or she just needed more insulin. So we'll just give her more insulin. She'll come down, you know.
Scott Benner 55:06
Why do you think that happens? I've been talking to you for a while now. You seem like a reasonable person. How come you're like, Sure, why are you being dramatic when things are happening? I guess
Laura 55:14
I think it's just anxiety. It's like, Because anxiety gives you that urgency, that feeling, which it's supposed to do in an emergency, right? You're supposed to have adrenaline and cortisol levels shooting up so that you can escape danger. But, like, I have to remind my body that, like, this isn't always dangerous. I mean, you know, low blood sugar could be, but I I know the steps. We know how to handle this. You know, so being confident in the fact that, okay, we can, we can handle this without, like, the panic,
Scott Benner 55:45
yeah. Well, what's stopping that from happening for you?
Laura 55:49
I think it's just the way my brain kind of it just goes into like, emergency mode. So I try to tell myself, like, Okay, this is an emergency. We can figure this out.
Scott Benner 56:00
Yeah. Can you just, I mean, listen, people's reactions, are the reactions, right? But, but, I mean, it would seem to me, because this happened to me too, like, where something would happen, and I my wife said you'd always be like, like, she's like, You said, so much, like, you know, and it's upsetting to hear, but it's a long time ago, she tells me this, right? Okay, so I stopped trying to think about it. And what is it I'm faced with over and over again, is that you put so much work into this and it didn't work out? Yeah, or, geez, it feels like a failure. Like, it's like, how do I not understand this? I thought I understood this, like, you know, like, that kind of thing. But, I mean, listen, once she pointed out to me, she's like, it's upsetting to other people, like, it always seems like something's going wrong. It could even be making Arden feel like she's doing something wrong. And I was like, okay, and then Laura stopped doing it. Yeah, right. So what's stopping you from just never doing it again?
Laura 56:58
I think again. It's a pattern. It's just something that shows up for me, like, it's like an instinct, but I have to interrupt it. I think that's what I need to do. I need to just be more aware of it. Take a pause. Yeah, you know, one of the best pieces of ice that, you know, somebody told me before, like, her numbers are just, it's data. Like, just look at it as data to try to figure out what you need to do next. Not like, oh, I screwed this up, or it's, this is all my fault, you know,
Scott Benner 57:28
I I'll tell you that I think one of the more difficult things to learn for me was just slowing down. Yes, a little bit like that. You Yeah. I mean, you can tell, like, even just in the podcast, right? Like, if you say something to me, anything like, if you just pivoted right now and said something completely that had nothing to do with what we were talking about, I'd be able to answer you, like, and so it's a strength in parts of my life, right, that I hear something, I form an idea. It's usually pretty cohesive, and I can start sharing it right away. But in that situation, that's not a virtue, right, right? Yeah, situation where you just need to wait a second pause, like, yeah, like, that's not a virtue. I and it's not a thing I was doing on purpose. Like, I think, I think my wife was like, Well, I don't know why you're being so like, defeatist right away. And I was like, I'm not like, I'm just like, I'm already working through the problem again. Like, Oh, we did this. This happened. I didn't want that to happen. And now I'm past this already. Like, I've said it, like, that's me almost pausing and going, Okay, that didn't work. What do I do next? I'm already thinking about it, while I'm thinking about what to do next time they're back there going, like, Oh, this is such a bummer, right, right? So, yeah, once you learn to just shut up.
Laura 58:46
Yes, I need to do that. Yeah, because that's how my brain works. I want to know, what can I do different next time? But I I process things like out loud a lot, right? Which drives people crazy, especially my husband.
Scott Benner 58:57
I gotta be honest with you, I do that. That's not fun for people who don't like that, right? Exactly, you know, yeah, there's people who think out loud, and there are people who don't, and the people who don't don't enjoy it when someone who does
Laura 59:11
right, and you're like, you're saying the same things over and over again, like, that's the way I'm processing that my brain is just like, What can we do differently? Next time, you know, have
Scott Benner 59:19
you ever heard me say that? My wife said that I say no to everything? Yes, yeah. It's because I work backwards from now, yeah. Like, I start with why this won't work, and if I can get to why it will work, then it usually works, right? And if you can't get there, then it might not be possible, right? It feels like, yeah, doing it. Opposite is Pollyanna to me, like, oh, everything's gonna be fine. And then you like, get through it in your head. Not actually gonna be fine. It won't work. Yeah, I prefer to go like, here's what's wrong. Here's all the things trying to stop me from making it right. How do I get around those things? Awesome. I got around them. We won, right? Yeah, I don't see that as negative at all, right? But if. You're a person who's just like, you know, yes, we can then you know, like, you're going to be like, Why are you being so negative all the time? And to me, it's just, it's just the thought process. But doing it out loud, yeah, Laura, doing it out loud. They hate that.
Laura 1:00:12
They do, yeah, people. So I need to write it down. I am big about, like, writing stuff down, so I need, that's why I said might need to next time, maybe write some of this down. Instead of, you know, say it out loud.
Scott Benner 1:00:25
We can pause. You can say it in your head, right? And then think, like, how would, how would these people prefer to hear this and then say that way? Yeah, although you know what I will say this, you notice they don't care about us. Like when they're all quiet and thinking in their heads and then coming up with what they want to say and then saying it. Like, do they know that during that time, I'm sitting there going, like, are you hearing this? Are you part of the conversation? Like, I'm thinking, I'm like, thinking, why don't we talk
Laura 1:00:52
about it? Yes, yeah, that's very true.
Scott Benner 1:00:55
Yeah. No, I don't know how the opposite would go. Like, if you and I were married more, right? And something went wrong. Would it just be, like, this big, like, I don't know symbol loudness of just people talking back and forth till we came up with an idea, right?
Laura 1:01:12
That's true. And would we hate that, right?
Scott Benner 1:01:15
Yeah, would you and I be like, one of us has got to shut the hell up so the other one can talk.
Laura 1:01:20
Probably not a good combination. I
Scott Benner 1:01:23
know, like as much as I look at my wife and our personalities, and they're so different, yeah, yeah, we are pretty successful people, yeah. And I can look at her and say, she has gaps, I fill them. I have I have gaps. She fills them. But you know, what I've noticed is that nobody really sees it that way. Yeah, they just see it as like you're wrong about the way you think about this, right?
Laura 1:01:47
That's true, but you but you're right. If you look at it that way, it is true.
Scott Benner 1:01:51
You know, Laura, I say I'll say it again. Best part of my life, other people, yeah, worst part of my life, other people, yeah. All right, yeah. So what is this? This hour done? You feel good about it? Yeah.
Laura 1:02:08
I just, I hope, you know, people can learn a little bit of something in there. I, I always seem to find something in in the episodes, you know, even if they're random, people are talking randomly, like, I'm like, Oh, that's a good idea about this, you know. And I hope that people realize that, like for them, if, if their grief came later. Because, again, I think people think like, oh, it hits you all at once initially. But I think, you know, grief is so different for people that it can come out later on, or even even, like, I still have moments where I just feel a little sad, you know,
Scott Benner 1:02:42
sure, if you told me to, you know, re encapsulate everything I would have said. I hope people heard you say that, because I think that is something that most people would find crazy, like three years later. You know what I mean, but, yeah, but I don't think it's probably as uncommon as you think.
Laura 1:02:58
No, yeah, right. Just people need to, I think, talk about it, you know, you gotta
Scott Benner 1:03:03
have somebody to talk to about. Listen, my, my mom's been gone for a couple years now, and I texted my brothers the other night, like, we have a little group chat. And I just said, I miss telling mom about, like, how I'm doing and, like, what everybody's up to, you know, right? Yeah. Then I said, I just, I just really needed to tell someone that, like, you don't need to respond. It's just like, I'm sitting here, you know, at 930 on a Tuesday, and I'm like, God, let's call my mom, you know. Yeah, right. And then you just, you're, you're like, why? I can't believe it. This is a feeling I'm having two years after her, yeah, she lived into her 80s. It's not like she was taken prematurely or anything, you know. Yeah, right. So nevertheless, it's very valuable to say that you could be struck by things like that, many, many years past when.
Laura 1:03:56
Yeah, right. That's very true. Well, I
Scott Benner 1:04:00
think you, I think you lended the podcast a lot of interesting conversation
Laura 1:04:04
today. I really appreciate it. Yes, and I did want to say one last thing to you, please, because I, I was born near Philadelphia, so I appreciate how you say water instead. Thank you.
Scott Benner 1:04:17
People don't seem to make fun of me about it as much anymore, although I'll tell you, it's going to be forever. One of those words that just now, like if you said to me, say, you know, if you showed me a glass of it and said, say this correctly, yeah, I don't know which is the right way, yeah, yeah. I think people say water.
Laura 1:04:37
Yes, yep. That's how, now that I'm in upstate New York, we say water, but my my parents still say water, so I get glimpses of that once in a while,
Scott Benner 1:04:46
but I need to tell you, like, when I say water, it rattles through the front of my brain, like something's really wrong, right? Like it sounds wrong to me, and then, and then I say it, and then my kids are go, that's the right way. And I'm like, no. Think it's not, I doesn't sound such a ridiculous thing, you know.
Laura 1:05:04
Yeah, and we're going to see the Phillies in a in another month.
Scott Benner 1:05:08
So well, tell you right now. I said to my son the other day, is there a way we can get into a time machine and start the playoffs right now? Because we'd win this, win the World Series. Yes, they're so good at the moment,
Laura 1:05:20
they are. They're doing a little type one event. So we're gonna meet up with some we don't have much around our area for community, so I think that was another part of my grief, is that we just don't have much around here. So we're connecting with with some people from Philly.
Scott Benner 1:05:36
So wait, Philly's like the Phillies are having a type one event, or there's an
Laura 1:05:40
event, well, there's like, a
section for people, right? Oh, I know they do that every year, right? Yeah, so we're gonna go. I met some moms at a mom's night out last year at Cherry Hill, so some of us might meet up there.
Scott Benner 1:05:56
Look at you. Well, that's awesome. Yeah, good for you, yeah, well, and you'll see a great baseball game. I know absolutely one night when they suck, and you'll be like, how, I know that's very true. You ever did that? Like, if you finally have a moment and you've like, like, we have games on in our house constantly, but like, when I actually sit the watch it, I seem to be able to pick the one they'll win, like, three out of four, and I'll find a way to sit and watch the one game where everybody sucked. I don't know how I do
Laura 1:06:22
that, but we did that last summer. We went last August, and my daughter was so excited, and they lost, and she literally cried, like, yeah, she was crying. And I was actually happy, because it was so hot that day, I just wanted to leave. And I was like, if they start doing extra innings, I'm gonna die. It's so hot. Yeah? Daughter's crying, and I'm like, Yeah, we're done.
Scott Benner 1:06:44
I'm not gonna lie to you, it's hard. It's hard to go into that stadium July and August
Laura 1:06:48
sometimes, yeah, oh, it was so hot. Yeah.
Scott Benner 1:06:51
So weather's turning this, uh, it's getting cooler on the East Coast though, a little earlier this year. So yeah, we all have a great time. I appreciate you. I really do appreciate
Laura 1:07:01
it with me. Absolutely. I appreciate it definitely. Hold on one second for me. Okay, sure. Okay.
Scott Benner 1:07:14
The conversation you just enjoyed was brought to you by us, med, us, med.com/juicebox, or call 888-721-1514, get started today and get your supplies from us. Med, Dexcom sponsored this episode of the juice box podcast. Learn more about the Dexcom g7 at my link. Dexcom.com/juicebox this episode of The Juicebox podcast is sponsored by the Omnipod five. And at my link, omnipod.com/juicebox you can get yourself a free, what I just say, a free Omnipod five starter kit, free. Get out of here. Go click on that link, omnipod.com/juicebox check it out. Terms and Conditions apply. Eligibility may vary. Full terms and conditions can be found at omnipod.com/juicebox links in the show notes. Links at Juicebox podcast.com. Okay, well, here we are at the end of the episode. You're still with me. Thank you. I really do appreciate that. What else could you do for me? Why don't you tell a friend about the show or leave a five star review? Maybe you could make sure you're following or subscribe in your podcast app, go to YouTube and follow me, or Instagram. Tiktok. Oh gosh, here's one. Make sure you're following the podcast in the private Facebook group as well as the public Facebook page you don't want to miss. Please. Do you not know about the private group? You have to join the private group as of this recording, it has 51,000 members in it. They're active, talking about diabetes, whatever you need to know. There's a conversation happening in there right now, and I'm there all the time. Tag me. I'll say hi if you're looking to meet other people. Other people living with type one diabetes, head over to Juicebox podcast.com/juice, cruise, because next June, that's right, 2026, June, 21 the second juice Cruise is happening on the celebrity beyond cruise ship. It's a seven night trip, going to the Caribbean. We're going to be visiting Miami, Coco K st, Thomas and st, Kitts, yeah, the Virgin Islands. You're going to love the Virgin Islands. Sail with Scott the Juicebox community on a week long voyage built for people and families living with type one diabetes. Enjoy tropical luxury, practical education and judgment, free atmosphere. Perfect day at Coco Bay St, Kitts st, Thomas five interactive workshops with me and surprise guests on type one, hacks and tech, mental health, mindfulness, nutrition, exercise, personal growth and professional development, support groups and wellness discussions tailored for life with type one and celebrities, world class amenities, dining and entertainment. This. Is open from every age you know, newborn to 99 I don't care how old you are. Come out. Check us out. You can view state rooms and prices at Juicebox podcast.com/juice, cruise. The last juice cruise just happened a couple weeks ago. 100 of you came. It was awesome. We're looking to make it even bigger this year. I hope you can check it out. Hey, what's up, everybody? If you've noticed that the podcast sounds better and you're thinking like, how does that happen? What you're hearing is Rob at wrong way. Recording, doing his magic to these files. So if you want him to do his magic to you, wrong way. Recording.com, you got a podcast. You want somebody to edit it. You want Rob.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!