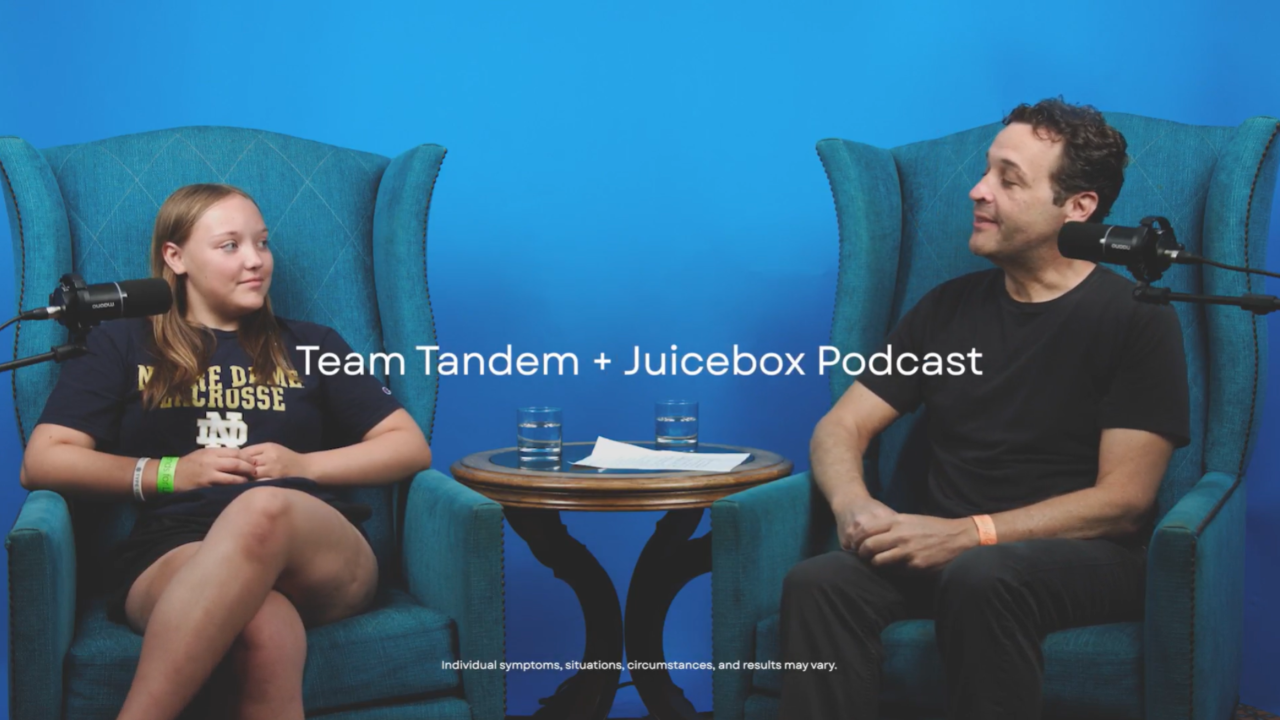
#697 After Dark: Emily
Emily has type 1 diabetes and she is here to talk about her life.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 697 of the Juicebox Podcast.
On today's episode we're going to speak with Emily, she's an adult who has been living with type one diabetes for a large portion of her life. Today is the 26th installment of the afterdark series. And Emily is here today to share her very, very specific rememberings of her upbringing, and to talk about how they've colored her life with diabetes. Please remember, while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan. We're becoming bold with insulin. If you have type one diabetes, and are a US resident, or are the caregiver of a US resident who has type one diabetes, please go to T one D exchange.org. Forward slash juicebox. Join their registry. Take the survey taking the survey takes fewer than 10 minutes. Your answers to simple questions help people living with type one diabetes T one D exchange.org. Forward slash juicebox. I swear it takes no time at all you can do it from your phone. After you get done listening to me head over, I guess maybe you could multitask and do it at the same time. Today's episode of The Juicebox Podcast is sponsored by Dexcom, makers of the Dexcom G six continuous glucose monitor, learn more and get started today@dexcom.com forward slash juice box it is that that very same link where you might find out that you're eligible for a free 10 day trial of the Dexcom G six. The show's also sponsored today by Omni pod makers of the Omni pod dash and the Omni pod five. Find out if you're eligible for a free 30 day trial beyond the pod dash, learn more about the Omni pod Vive or get started with some Omni pod product at Omni pod.com forward slash juice box. If you're in the market for an insulin pump, I highly recommend it.
Emily 2:19
Hi, my name is Emily and I was diagnosed a type one diabetic when I was 10 years old. How old are you now? I'm 41. I mean, sorry, I was 41 years ago. So I'm 52 You're
Scott Benner 2:32
52? Do you know Emily? And by the way, you'd have no way of knowing this, that I interviewed someone yesterday. And today was there 52nd birthday. Oh, that's interesting. And at the same time only interesting to me, really. So now that I've shared it with everybody else. I was amused by it. And it I realized and quickly it has nothing to do with the podcast. So let's just keep moving.
Emily 2:53
Well, all the best people are born in the first quarter of 1970. I have three of my closest friends. were all born in the first quarter. So we get together each year for fun and games, usually in Oakland.
Scott Benner 3:11
What happens in Oakland is it isn't Oh, that's
Emily 3:13
just sort of the meeting point. I have a friend who lives in Oakland proper. And then another who lives in Danville and another who lives in Turlock, which is sort of central California.
Scott Benner 3:26
If anybody listening wants to kidnap your friends, they're a third of the way to it. So
Emily 3:32
I don't think these women will let themselves be taken.
Scott Benner 3:36
Well, oh, you're saying come get us. It isn't gonna work out for you. I gotcha. Exactly. Exactly. That's excellent. So okay, so diagnosed. 10 years old. Is that right? Yes. In the 80s. The early 80s. Yes. And anybody else in your family have diabetes?
Emily 3:54
Nope. I was the first one. Although my sister who was five years older than me, four years older than me, was diagnosed. That 10 years later, when she was in college.
Scott Benner 4:09
Interesting. So you in the early 80s, your sister in the early 90s? Yes, you as a 10 year old her is more like an 1819 20 year old. Yep. Okay, are you guys closer, you're pretty far apart in age. It sounds like, um, well,
Emily 4:24
we were always fighting. There's third oldest sister. And so she and I were more close because she sort of took me under her wing and would recommend, Oh, I like reading this book when I was your age, that kind of thing. Whereas my middle sister and I were too close. Where we actually would end up at that same school like we are at the same high school for two years and that he hated having to give me a ride around town and stuff like that.
Scott Benner 4:59
That sucks. If I would have just said, Look, if you want a car, you drive Emily. And that's that anybody makes a face no more car. That's the end of it.
Emily 5:07
Right? Yes. You met my mother apparently.
Scott Benner 5:11
That's maybe why she didn't enjoy driving you around. So okay, so you're diagnosed me, you're gonna have diabetes for a decade before your sister dies. There's no other diabetes in the family. What was it like having type one as a 10 year old back in the early 80s?
Emily 5:27
Well, it was all a big mystery. And I beginning to suspect it was a mystery to every doctor I ever had. Because we got we took a couple classes and stuff like that. But my parents were never, they never understood sort of what first of all, I was testing my urine with a test tube and, you know, I droppers and little pills that turns certain colors. And so you had a very wide range of what your color might mean, if it was dark blue, then you were really low or had been, you know, five hours ago. It was never explained to me the timeframe between when I tested my urine. And when that low had actually happened. Does that make sense?
Scott Benner 6:20
Yeah, you don't know. There's no context for you between the test and the event.
Emily 6:25
Right. And they never bothered to explain it to us. And my parents never realized. They don't know how they could have realized that they would be punishing me for something that I had done five hours ago and had no idea I was doing. So I was running high all the time. Simply because, you know, I had never learned any portion management because that was not in the cards in the early 80s for 10 year old. And so I just feel like every single piece of knowledge that we got that then was wrong and just set me up for failure. Yeah.
Scott Benner 7:07
Were you using early 80s? We're using animal insulin or we're using regular mph.
Emily 7:14
Yes, like for the first couple months, it was beef and then we got brand new pork insulin for a while and then I went to Cuba log insulin and mph or human. Insulin, probably starting in college, maybe?
Scott Benner 7:35
Okay. Oh, a lot a decade. Yeah, yeah. All right.
Emily 7:40
Well, I went to college when I was 17. So seven years. Look at
Scott Benner 7:43
you, smarty. So, so basically, you're shooting insulin in the morning, and at dinnertime. And, and you're, I mean, you know, I've never asked anybody this, but you get the pee in the test tube the way I assume right? You just hold it under yourself.
Emily 8:01
You get this hat. I don't know if well, you're if if you're a woman, and you go into the hospital, and they need to collect your pee, they give you this what looks like a plastic hat that you put underneath the seat in the toilet, and then you pee into that. And then you take out
a sample eyedropper and you take out the sample. So then you have this plastic head that's always in your
Scott Benner 8:28
bathroom. I was gonna say it's the plastic cats were usable, right?
Emily 8:32
Yes, but it still got gross. Even when you clean them.
Scott Benner 8:36
Anything up on Emily? I don't know. Yeah, it's a gross factor at some point. So you're basically using this thing, taking out the sample, dumping out the rest of it, rinsing it off putting it I imagine it starts not even getting put away. Right? It's just leaning on the wall in the bathroom or something like that.
Emily 8:51
Oh, yeah. It never had a place to be put away. It was always just stuck in a corner. Yeah. Have you ever
Scott Benner 8:55
noticed when they build houses? They don't think where would we put a plastic cat if somebody needed the bathroom?
Emily 9:01
Yeah. It's they're still not building them in there. i It's not fair.
Scott Benner 9:06
So it's still not out? Yeah, gosh, I mean, even that alone has got to be arduous as a young child, right? Just, yes, I drudgery.
Emily 9:17
Yeah. And the only time I was doing it was in the morning or at night. You know, I was only testing myself. At times when my blood sugar's or, you know, my blood urine. My urine sugars would be high, you know, like after I've eaten dinner.
Scott Benner 9:36
So you have a real chance for this test to come out looking positive anyway, because you're probably not using enough insulin. You don't have any idea about food or nutrition. So you're just basically testing at the highest points of the day. And then exactly right. Your parents see a color and get mad at you. Yes.
Emily 9:53
And so it took me 25 years to start. Seeing a blood test as being just information that I'm being given and not a judgment on what kind of person I am. Yeah. And it's still, I'll still fall back into that. Sometimes I just recently got a Dexcom. And I mean, I just got it. I'm on my second transverse.
Scott Benner 10:26
Second sensor, you're less than 20 days with it. Exactly. Wow. Okay.
Emily 10:31
And so and it's, it's driving me crazy, because I will see, you know, it tells you you're going up, you're at 190. And you're going up, and I'll be like, no, okay, I have to wait. I've taken my insulin I've eaten not do I have to wait for it to calm down and then I can't, then I'll be like, I'll take two, two units of insulin straight to get it down. But of course, that doesn't show up for another hour. And by then, I haven't gotten the hang of it yet. It gets very saddening.
Scott Benner 11:02
Well, so first of all, I know exactly what you're talking about. Because when you're presented with the data in a new way, it feels like starting over. Because even if you weren't doing it, you know, doing it doing diabetes, the way you were hoping to prior to that you were at least probably in a rhythm. Like you did it the way you did it. And it's, you know, what, what's expected happens, etc. And then you get a whole new set of data. And you're like, Oh, like this is I'm really bad at this is how it feels. I mean, they felt like that way to me, at least when I saw Dexcom for the first time. Yeah, you're making me think that Dexcom should make an ad where they're like, Dexcom better than a plastic hat to PN?
Emily 11:44
Yeah, they should
Scott Benner 11:45
capture the 60 year old market. No problem. People would be like, Oh, they know about the plastic cat. Yeah. So so. Are you? Well, it sounds like you're not. But I would say that. The first hump you have to get over is to not see the data as like a report card, but just see it, like big picture, step back from it. Don't look at it minute to minute hour, look at it over 24 hours. So you can kind of get a feeling for like, Is my Basal right. You know, like, that's where I would start. Because, yeah, you know,
Emily 12:20
I don't even have enough. I have to my endocrinologist appointment is hopefully coming up soon. They haven't actually called me back to make the appointment yet, but hopefully, they'll be able to give me more information because I don't really know what I kind of know what Basil is, but I don't know. How to cook with that. I mean, no,
Scott Benner 12:48
no, I do. I was just gonna say you are from a time period of diabetes where no one let you adjust your your insulin, right? Yep. Yeah, you just go to the doctor and they tell you like, Oh, we're gonna make it. We're gonna make it eight now. Like, that's pretty much it. You go. Okay, that number is eight now. And you just go with it. What is your agency's been like over your life?
Emily 13:10
Oh, I'll tell you a story. I was seeing this diabetic nurse practitioner. And she said, You know, I think my last test had been at like 9.2 or something. So she says, Would you like to try this? drug? It's not. It's for type two diabetics. It's a shot. You take it when you take your insulin. And it's supposed to really help with control. And I'm like, sure. Okay. And so I took it for three months. And what it did was it made me so nauseous. I never ate. I was constantly throwing up. I why I stuck with it for so long. I don't know. But my blood sugar numbers were pretty great. And so then I went in, and I told her that I wanted to get off of it because I was literally throwing up every day. And she's like, Oh, okay, well, your numbers are really good. You're down to 6.5, which is ideal. And so she tried to talk me into staying on it because I wasn't eating and so I had lost all this weight. And my numbers were down.
Scott Benner 14:30
That's not a perfect I can't believe I can't believe that ideal was the word that was used because it's not ideal if you vomit constantly and that's why you lose weight and why you can't write why your agency is lower because you're not eating and there's no food your system. Exactly.
Emily 14:44
How can I even got a little certificate in the mail saying your agency is perfect well done, and they spelled my name wrong. I don't like your My name is right there like it's in the list.
Scott Benner 14:58
So Emily asked her Hearing that you were vomiting your way to a six a one C on some medication that clearly did not jive with your body. Well, they sent you a certificate of achievement in the mail and spelled your name wrong. Yes. Well, that's that's a copay well spent for you. Did you keep taking it? Or did you stop?
Emily 15:19
I stopped? Yeah.
Scott Benner 15:21
I have to tell you I would not. It's an interesting thing, that generational thing with diabetes because if somebody gave my daughter something, and it made her throw up, I'd stop giving it to her immediately. Like, I wouldn't care what they said. You know what I mean? But it's interesting that you persevered with it, how long did you do it for?
So I just checked out my link dexcom.com forward slash juice box, and somebody at Dexcom has spruced it all up. Thank you. Dexcom. It looks fresh and new. I was immediately greeted by a handsome photo of Nick Jonas, who, as you may know, has type one diabetes. After I swooned for a moment, I scrolled down, who do I see Miss Patti LaBelle, Patti LaBelle, seeing her gave me a new attitude, if you know what I mean. Here's the point. If you're using insulin, type one or type two, the Dexcom G sex is going to be a friend for you, you're going to be able to see your diabetes as it's happening. That's the speed, direction and number of your blood sugar. Is it 89? Is it 120? Is it 150? Is it 240? Is that rising? Is it falling? Is it rising quickly? Is it rising slowly, etc, etc. So on and so forth, so forth, so forth. Speed direction number, you see that on the Dexcom receiver if you like or you can see it on your supported iPhone or Android device, this is a big deal. To see your blood sugar without a finger stick to see it in real time to be able to set alarms and alerts. I want to know when my blood sugar goes under 80. No problem, you can get that you want to know when it goes under 60 you can get that you want to you want to know when it rises above 121 4150 to 100. Wherever you set those alerts. The Dexcom is gonna give you the little beep beep and let you know when it's happening. On top on top, on top of all these alerts and alarms, the Dexcom also allows you to share your data with up to 10 people if you'd like that means your kid could be at school and 10 family members. I mean, you probably don't know 10 People but I mean, you know I'm saying it could be up to 10 Could be your school nurse. It could be your husband or wife, a sibling, a friend an adult could have their friends looking up to 10 people can take a look at your Dexcom right on their phone if they like. Head over there today. dexcom.com forward slash juice box see Nick Jonas's smiling face. Learn more about the Dexcom G six, find out if you're eligible for that free 10 day trial of the Dexcom g six@dexcom.com. Forward slash juice box. On the pod is a tubeless insulin pump. It's a tubeless insulin pump that my daughter has been wearing for like 14 years now. been wonderful. She's had it on every day. You can check it out and try it for yourself. And on the pod.com forward slash juice box. Here's what you may be eligible, you'd be good. But I can't talk. Here's what you may be eligible for a free 30 day trial of the Omni pod dash. That's crazy enough. You can also head over and learn more about the new Omni pod five. That's an algorithm based system that makes dosing decisions for you in conjunction with your Dexcom G six. Are you kidding me? The future is now baby and it's here. Omni pod.com forward slash juicebox Get started today, learn more contact Omni pod and say hey, you know I'd like to try Okay, get to trial. He even think they'll send you out a like a little we haven't talked about this in a while. But I think they still do this. You can get a single pod like a dummy pod doesn't actually work. Just if you want to try it on aware to get a vibe for how it feels. All of this is at your fingertips. The internet is at your fingertips, you use your fingertips that's at your keyboard, and then you type on it. The va.com forward slash juicebox if you're looking for an insulin pump, in my opinion, you should look at the Dexcom. If you don't like it, it's cool. But I mean a free 30 day trial gives you plenty of time to figure it out. omnipod.com forward slash juicebox dexcom.com forward slash juice box links in the show notes of the audio player you're listening in right now. And links at juicebox podcast.com. Let's get back to Emily. And trust me. There's a lot more to talk about with Emily. Three months. No kidding.
Emily 19:48
And well. I would call her and tell her that I'm throwing up she's like well try staying with a little longer. It may just be taking you a while to get used to it. So I kept thinking it's not like I called her every week. She kept telling me to take it. Yeah. But you know, after the first week, she said, well take it a little longer see if you still have it. And I just kept thinking, well, maybe next week, it'll get better. What was the drug? I wish I could remember the name as long ago, right? It's i It's one of the ones that's has a commercial on it now. But every time I tried to look for that, like, they didn't give me the they gave me the off brand.
Scott Benner 20:25
Oh, you were using a generic of it? Yeah. And they didn't try. They didn't even try moving into the drug. Just generic only.
Emily 20:36
Oh, that well, that was Walgreens fault.
Scott Benner 20:39
You have it the doctor can say no generic substitutes. I'm saying like the doctor never stepped up. Did the doctor know you were taking the generic? Do you think
Emily 20:49
the Nurse Practice Nurse Practitioner was the only one I was seeing. And I honestly didn't, it didn't occur to me that it would matter.
Scott Benner 20:57
Gotcha. Might not have I'm just saying I was wondering if that was the that would have been the first thing I said if I was the doctor. So I was wondering if it got said to you. Alright, so. So this is pretty much your setup, like this is how it's going. You're Are you your Dexcom and MDI are Dexcom in a pump.
Emily 21:16
MDI MDI,
Scott Benner 21:18
would you ever use a pump,
Emily 21:20
my doctor keeps trying to get me to take a pump. But my I had a Dexcom, about 10 years ago. And I had a very bad experience with it, which I'm not having this time around. But it was with the the insert, I don't remember the name of the three pieces. But the the piece that you carry around with you, as opposed to the recipient,
Scott Benner 21:49
I'm sorry, the central know the receiver, the part that you carry to look at your numbers on the receiver, right? The receiver
Emily 21:56
was set so that it would be but certain times you couldn't change the beeps. And it was just constantly beeping. And I got so frustrated, because it would wake me up for no reason, if you like your blood sugar is on its way up, like I know. And I couldn't turn it off. And so I just said, No, I'm not going to do that anymore.
Scott Benner 22:18
Emily, you have gotten no help. Because those alarms are custom are customizable. You can change them.
Emily 22:24
Well, the one I'm on now I'm on the GS six, you can customize it except for what it deems is your lowest low
Scott Benner 22:31
5050 BMC. Yeah,
Emily 22:35
I consistently wake up at night, well, before I was on it, I consistently would wake up with my blood sugar being in the 30s. And I'd be pretty much coherent. And I would just get up and I'd eat something and I'd go back to bed.
Scott Benner 22:52
So, so Emily, there's a lot going on here, you are about to learn a lot with this Dexcom I tell you, first of all, please stick with it. Like unlike the drug that made you vomit, I think you're gonna have a good outcome with this. I stick with it because it sounds to me like you are using insulin in a way that is making you low at times. You don't need to be that I mean, 30 is just, I mean, 30 is a pretty big mistake somewhere. You know what I mean? Like, I don't know if it's with your meal or with your Basal insulin like I couldn't possibly tell you from here. But have you listened to the Pro Tip series of the podcast?
Emily 23:31
A couple. A lot of them. A lot of the the podcasts I've listened to just happen to be about things that don't really apply to me. At least I haven't I haven't heard ones that apply to me yet. But I, I listen to a lot of different kinds of podcasts. So I have to admit that I don't listen to yours on a regular
Scott Benner 23:58
route. So I'm gonna send you a specific list of management ones that might help you get your Basal insulin dialed in, and then give you ways to think about giving yourself insulin at mealtime. Because Because you shouldn't be at 30 like and I don't think you have to be you know, so I think somebody needs to help you a little bit and get you get you going in the right direction.
Emily 24:22
Well, I can tell you that. Now I'm I'm on a human log and Lantis at least four shots today. Because the Lantis is I use a pen so the Lantis is separate. And what I will tend to do is I'll be hungry, so I'll try to figure out how many cards I'm going to take. And I was given at one point, the ratio that I'm supposed to use. And so I'll figure out the carbs. And then I'll take my insulin and then I'll end up about halfway through getting or, like I have a really small stomach. And so I never finish a meal. And so the hardest part for me is figuring out how much I think I'm going to eat versus how much I do eat. And when I should be taking my insulin, so they said, Well tried take your insulin afterwards. And so then I do that
Scott Benner 25:23
not okay. So, again, the input, the information that people come back at you at is interesting, where they skip over the common sense and go right to the dumb idea. I've seen that this has now happened twice in your stories. It happened throughout my life, right? So yeah, so here's, here's a thought, if you don't know how much you're going to eat, why don't you Bolus half of it as a Pre-Bolus? And then if you finish it, put the rest of it in. Like you're not afraid of the needle. I mean, you've had years you don't get about, oh, I just cursed. You don't care about injecting? I imagine, right? Yeah, no, right. So do half upfront, give yourself a reasonable do you Pre-Bolus your meals at all?
Emily 26:03
You mean, take my insulin before I
Scott Benner 26:05
yeah, like but yeah, you do. But like 15 minutes, five minutes? How long do you do?
Emily 26:12
It's usually about five minutes. Okay?
Scott Benner 26:15
There's a whole world out there you don't know about I'm excited. I'm excited to send you these episodes. I'm gonna list them at the end of your episodes so people can hear them. But when we get off, I'm going to just send you an email with a list. Okay. Okay. All right. And I think that you'll be able to get your IP. So, Emily, this is interesting. For me, I didn't realize we were going to talk about this before we talked about the other thing. So in my mind, everything about type one diabetes is how you use insulin. And everything about the insulin is the timing and the amount, meaning you need to use the right amount at the right time. That can mean your Basal insulin Volantis for you. And that can mean your mealtime insulin. Both things need to be measured and used properly. So the first thing you're going to kind of work on is getting your Lantis, right. And your Lantis should be holding your blood sugar stable at a number, whatever your number is that you want. Like if you want to be 90 all the time, if that's your goal, if you want to be 120 all the time, if that's your goal, like whatever your goal is, there's an amount of Lantis that you can take that away from meals away from meal insulin, and away from exercise. Your Atlanta should hold you with that number. You should have enough of it in there to hold you steady. You should think of the Lantis as sort of like a giant unseen force standing over your top of your blood sugar pushing down with its palms, holding your blood sugar stable at a number not letting it rise up past that. That's its job. Now once you have that, right, you need to move on to understanding how to polish your meals right.
Emily 27:54
Did you say pushing down with its paws?
Scott Benner 27:57
With its palms? I'm sorry? Oh, yeah. Just like try to imagine Lantus being a giant. I don't know, like a god. Okay, well, I'd
Emily 28:05
like to think of it as a giant bear now.
Scott Benner 28:07
Okay, fine. I'm with you. All right, I thought I heard pause. And we I'm going with you. And this is a bear. Okay, it's a bear 10 times the size of you. And your blood sugar is this. I don't know, unforeseen ocean that's trying to float up too high. And the bear is just pushing it down, pushing it down, pushing it down, but not too far, just keeping it where it wants to be. That's what your Basal job is. It's to hold you stable at a number. Okay. And then once you do that, that's sort of not a variable anymore for you. Because you know, your Lantis is set up well and doing its job. And then you come along and look at your meal and say, Alright, this meals, 30 carbs, and you look at your insulin to carb ratio, you put your insulin in, in enough time. I call this a Pre-Bolus. I think it's a pretty common phrase write in enough time so that when the action of the insulin starts to work on your blood sugar at the same time, or very similar timing, the food starts to work as well. So think of the meal as a tug of war. So on one side of the rope, put the insulin and on the other side of the rope, put your your food. Now, if you inject your insulin and begin to eat right away, the insulin is not going to start working for probably 1520 minutes, maybe if you're lucky. And then it's not going to be at full power probably for 30 minutes, like when do you usually see a peak like 45 minutes maybe? Right and then, but the food hits you much quicker than that. So now you've put the insulin in, you've started the timer on the insulin and you've told the food go ahead and pull on the rope. While the food is now has a huge head start it's pulling on that tug of war rope and that flag is going more and more on the on the food side and your blood sugar is getting higher and higher. And you're seeing that now for the first time in your life. because you're really wearing a Dexcom. So even if you start eating at a 90 blood sugar, you put in the food you put in the insulin 10 minutes later, the your 90 is 100, then all of a sudden it's 105, then the arrow flips up diagonal, now it's 110 115 121 25. And then the arrow flip straight up, this sounds familiar, right, and then your blood, your blood sugar starts flying up. And now it's, you know, 30 minutes later, your blood sugar is 190. And the insulin is really kind of feeling itself now and it's at full, it's at, it's more full power, and it starts to pull down. So now the insulin is finally pulling on that rope. And then that arrow goes from straight up to diagonal up to level, because that are, if you can think of the insolence got a hold of that rope, and it's finally pulling back, and it's pulling that arrow back around. But at this point, you only gave yourself insulin for the food, with a 90 blood sugar as your math. But now your blood sugar is 190. There's momentum on the side of the of the blood sugar on the side of the food. This insulin you've used is not nearly enough. And that's one thing that happens to you. The other thing that happens to you, I bet is that that whole process happens, but you don't finish your meal, and then the food, then the insulin comes online overwhelms the number and crashes you back down again, Does that all make like sound like stuff that's happened to you?
Emily 31:22
It's like, you're reading my pancreas,
Scott Benner 31:26
I have to tell you, those other podcasts you listen to, are gonna have to go on the back burner for a while I'm late because we are going to get you straightened out. Okay. So
Emily 31:35
let's see. That's the whole reason I wanted to talk here because my therapist said, you know, the whole way you're dealing with everything as far as diabetes in chronic pain and stuff has to go back to the grief that you've dealt with. Since you were 10. And on, tell me about it. And, you know, my grief. Does a grief when you're diagnosed as a diabetic, because even if you don't understand it, you do understand that you no longer get to eat as many double stuff Oreos as you want. There's a loss there. There's a, you know, a loss about, well, now I have to start thinking about everything I'm gonna do for the next hour, day, week, month, year, I have to sort of plan everything out, like my friends make fun of me, because I'm one of those people who has a purse that has something for every possible thing that could happen. Because that's what diabetics have to do.
Scott Benner 32:45
Well, Emily, not that people with diabetes don't need to be prepared. But I'm going to assert that it's more of what you have to do than what some people have to do. So my daughter is 17. She's had diabetes, and she was to yesterday afternoon, she came home from school at one o'clock. She's a senior and she's got an early release. They apparently are not teaching them anything in her last year. And she comes home and hurt her day begins basically her personal day and we knew my daughter had plans to go out with her friends that like they were going to go to dinner. So my daughter comes home. She had eaten something at school, we had not spoken to her about it. She had given herself a little too much insulin. So while she was getting ready, she took care of that with a little bit of juice, got herself at about a 90 blood sugar, took a shower, put her makeup on and got dressed. Her friend came and picked her up, they drove to a friend's house. Three, four hours later, they were having dinner. They ate at a restaurant from like six to 730 they went back to the friend's house, they hung out all night did a sleepover and she walked back in the door today at 10am. I did not speak to my daughter since she left the house yesterday at three or three I think maybe two and I'm going to pull up her her Dexcom in front of me right now. Okay. And over the last 24 hours after my daughter fixed the little low that happened when she came home from school, which was about 65 her blood sugar is for a number of hours from three o'clock until 630. Her blood sugar was 88 to 91. And then it looks like she missed a little bit on her dinner. And she had a spike but she spiked to 140 and that only lasted for about a half an hour. And then over the next 738 3930 She came back down. She looks like she caught it with a little snack. The drop around nine o'clock, and then she leveled out. And by 10 o'clock she was 75 and for the next 12 hours she was basically between 85 Have and at one point she got to 110. And that's a pump and an algorithm and a CGM working together along with her knowing how to Bolus for her meals, and how to fix her low blood sugars without causing a high one. That's all she knows how to do. She fixed her low without causing a high, she Bolus for her meal. And other than that she's wearing an algorithm. She's wearing it on the pod that's running an algorithm. And it is giving her insulin and taking it away and keeping her basil exactly where she needs it to be. That is a world you could easily live in. It is not that hard to get involved. If you have insurance, it'll cover a deck sound, you can get a pump, you know? Or you can or you can learn. I'm sorry, I'm sorry. I'm sorry. I didn't mean to step on you. But where you could learn to do it with MDR? There are plenty of people who do.
Emily 35:49
Yeah, I think I mean, I was really burned at the beginning with the the lack of information I got, and then I just I have a complete mistrust of doctors. I stay away from them as much as I can. Because I've never had a doctor really tell me anything particularly useful. When I was 13, I passed my first kidney stone, although that's not what I thought it was. I stayed home because I thought I had cramps. And then I was passing the kidney stone which have you ever passed a kidney stone? My wife has? I have not? Yeah, they're really horrible. Especially without pain medication. And sorry, I'm Flemmi.
Scott Benner 36:40
You're fine. I have an edit thing later, I'll listen back to this, no one will ever even know you cough. Don't worry about
Emily 36:45
okay. You can change this to say I'm Flemish, if you want. And so I called my mom at work. And I said, Mom, you have to take me to the doctor, I'm in so much pain. I'm pretty sure this is because I'm a bad diabetic, I'll do whatever you want. Just get this pain to stop. So she didn't it didn't occur to her that it was a kidney stone. It didn't occur to anybody that it was a kidney stone. They got me to the doctor, the doctor said, Well, have you been testing your blood because by now, blood testing had come out where you did these big strips, and you had to put like, half a gallon of blood on it. And then it would show you a color scheme. And I didn't do those because I didn't. I just didn't want to. I had sort of no one ever explained to me how that would be any more helpful than the urinalysis test. So I get to the doctor, and I'm still in a lot of pain. And he says, Well, what are your last blood sugar has been? I'm like, I don't know, I haven't tested on and he's like, why haven't you tested them? And I said, because I can I feel I can feel if my blood sugar is gonna go low. And he's he slams his fist down on his desk, and screams at me. Sorry, you're fine. And to a 13 year old, right? Like he went all he got credit for dinero in my face. And so I left that never getting help for my kidney stone, which I then eventually just passed.
Scott Benner 38:26
They didn't they just let you leave the hospital. They had me leave the hospital? Because you didn't test your blood sugar. They didn't check on the pain. Yeah. Emily, where did you grow up?
Emily 38:38
Northern California.
Scott Benner 38:40
Wow. Um, listen, let me say something to you. I didn't think this was gonna go this way. But I am sorry for all of the bad information that you have gotten over the decades. But I wanted to tell you that, that doesn't exist anymore. If you don't want it to the information is easy to come by now. It's literally in that I'm gonna give you basically, I don't know, 15 episodes of this podcast, if you listen through them, and marginally understand what you're listening to your agency will be in the sexes. It's it's the technology is so much different. But I think for you, if faced with that information, I think the 40 years of somebody or everybody may be letting you down. You just feel like maybe it's not possible, or is it? Or do you feel like it's too late because it's not too late. And it's incredibly possible? Like you should go into my private Facebook group and see that there are 20,000 people in there who are all either learning or doing and their blood sugars are not the way you describe. They are not living lives the way you think it has to be. Because you have diabetes. You just grew up in a bad time with type one, but you're still here and you're young, and it doesn't need to be like that anymore.
Emily 39:59
Well, I Appreciate that, and I will listen to the podcasts. Here's the kind of thing that I grew up with. I was diagnosed in December of 1980. And I turned 11, the next month in January, and we got a diabetes forecast magazine. Does anybody still get that?
Scott Benner 40:23
I don't know. But I was in at once. Oh, congratulations. I don't I didn't feel that exciting.
Emily 40:30
I had my doubts about this whole diabetes thing. When I saw there was a cover article that had the headline, I'm a diabetic, or maybe it was my daughter was just diagnosed diabetic. Can I still get a Christmas tree? Wyatt. That's what I said. And I, I it confused me. I'm like, why wouldn't we? Why wouldn't you get in? I knew enough about diabetes to know that Christmas trees have nothing to do with diabetes. And so anything I ever saw was either super, super scary. make no sense at all, or was super tweet like that? Just the sort of not
Scott Benner 41:18
helpful? Yeah. Exactly. The diabetes space is full. Yeah, yeah, I don't I don't do. So I'm just telling you there's a it's timing and amount, use the right amount of insulin at the right time. Your Basal right, you'll learn to Pre-Bolus for foods, you'll learn the difference between different foods glycemic index and, and load just meaning that, you know, 10 carbs of watermelons not going to impact your blood sugar the same way 10 carbs of white rice will. And then you stay flexible after that. And bunch of other stuff. It's a 681 say just good basil. Get your Pre-Bolus together understand how much insulin things need. That's pretty much it. Like there's not much more. I mean, listen, that's an unfair statement. There's a lot more to it. But that's the base of the that's the base of the building right there. You got to get that right. And then after you get that, right, the rest is a learning experience that you'll actually have time to learn because your experiences won't be so horrible. Like, you know what I mean? Like there's a difference between something going wrong and your blood sugar spiking to 140 which is what I described with my daughter's dinner last night, and something going wrong and you waking up in the middle of the night your blood sugar's 30. Like one of those things is an emergent disaster. And one of those is like, Oh, I got my Bolus a little wrong here. You know, so like, when you're constantly in the disaster, you can't see the lessons. You only mean like when you're running from the from the bear through the woods, in the woods or on fire? That's not the time to think the forest is a deforestation probably caused this, you know, like, this is the time to think I gotta run from the bear and the end The woods are on fire. I don't want to burn down. You're always constantly flight or fight, I would imagine. Yeah. And you need, you need to get you into a more calm place where you can actually watch something happen and say to yourself, oh, Emily, hmm, I Pre-Bolus 10 minutes here, and I spiked a little bit and then didn't get low later. I bet if I changed that Pre-Bolus to 15 minutes for this meal, the spike wouldn't happen. And I wouldn't get low like you can be a little more thoughtful about it when you're not running for your life.
Emily 43:27
Does that make sense? Yeah. Well, I think part of the reason I react the way I do to pretty much any sort of problem is, you know, my basically, I was diagnosed diabetic when I was 10. My dad died when I was 12. And so my fight or flight reaction is stuck at that age. So I feel like I don't quite under you know that. It's still a 10 year old me who was trying to fight with this diabetic stuff. Yeah. And is just so shocked. You know, I thought I was gonna die. My whole family joke that I would be the first one to die because of the diabetes.
Scott Benner 44:12
bunch of comedians who grew up with their Emily. Oh, yeah. Oh, yeah.
Emily 44:15
And so the fact that I've made it to 52 is so shocking to 10 year old me.
Scott Benner 44:23
Well, I'd start taking that as a sign if I was who am I? Am I dumb? I forget what those people said. And I'd get busy living. You know what I mean? There's a lot here.
Emily 44:37
The diabetes hasn't stopped me from doing anything except my mom sat me down. When I was in high school and said, you realize that you're going to have to have a job. The minute you get out of college because you need to have health insurance for the rest of your life. And she explained to me what insurance will do you know, once you get off insurance now this is a preexisting condition and you can't get on insurance again. Unless you have a job that recognizes you know that we'll give you health insurance. And then for six months, you're paying, you know, millions of dollars for your insulin, even though back then it wasn't as expensive as it is now.
Scott Benner 45:23
Yeah, device, get a job have insurance. I think that's valuable advice for a person that was type on.
Emily 45:27
Yeah, no, I'm really glad I know it. But having to do that kept me from doing what I really wanted to do. Like I ended up. It took me five years to graduate from college because I had to have a full time job as well. Because my mom stopped supporting me, and which was fine. I was an adult. But then, I had to start temping so I could get insurance. And I wasn't able to do I wanted to move to New York and become a comedy writer.
Scott Benner 46:04
And you got a job to make sure you had health insurance.
Emily 46:08
Yeah. Instead, I started temping at a just marketing company. In San Fran, well, I had a whole bunch of temp jobs. And I started working for this marketing company. And that got me into databases. And now I do it stuff, which I mean, I'm okay at and I guess it's okay. But I sure would rather be
Scott Benner 46:31
doing something different, or at least at least trying the thing you were hoping to do. Yeah. Well, you talked in your note to me about grief. And you said that obviously being diagnosed was hard. And then your father passing soon after was hard. Did it keep coming after there? Or were there two were these two things just very present with you constantly growing up?
Emily 46:54
Well, my family didn't know the rest of my family. My mom and my two other sisters didn't know how to grieve. My dad's loss it so it got buried under about, you know, 15 miles of crap. And my mom ended up like, right when I felt I needed her most let alone my other sisters. My I was 12, my middle sister was 16. And my eldest sister was 90, and hang on a second. Okay. Because my mom wasn't expecting this, I think she sort of reevaluated her life, and realize that she was going to start spending her life for herself and not for her children. And she found this friend who was 12 years younger than her and they just started, you know, running off on trips and doing things like that. And I don't actually have a problem with her having done that. But she didn't allow us to grieve. She just said, Okay, move on with your life. I'm moving on with my life. And, you know, I barely saw my mother. Well, I wouldn't say barely. But she, she wasn't around as much as say, my friend's moms. And the last conversation that I remember having with my father was one that he was accusing me of, because my blood sugars when I did test them were high. He, he had the memory of my urinalysis being high, he had decided that I somehow had found a way to go to 711 and buy candy and I had it hidden somewhere in the house, which was not true. And that was the last interaction. I remember having with him before he died. How did he pass? He had a heart attack. He was a US only 49. And he was a five pack a day smoker, meat and potatoes guy, so it's not a shock.
Scott Benner 49:08
Certainly drinking or drugs going on in the house with your parents? No, no. Interesting. Okay, so your dad dies, your mom flips out. Do you remember your mom being a panic before your dad died or to just really get to her?
Emily 49:21
I think she didn't know how to deal with it. My entire extended family I've talked to like, I'm really close with my cousin. And she talks about how her family you know, our whole extended family doesn't know how to grieve. You just kind of you're supposed to push things down. The only the only thing you're allowed to do at family functions pretty much is laugh. We're all very happy, goofy and not recognizing the problems that everybody has. Which has caused several divorces and just weird
Scott Benner 49:58
things not going well. Right. And for you, the for you. I mean, let's be honest. Right? You feel abandoned?
Emily 50:06
Right? Yeah. Even though I mean, I wasn't really abandoned. It just felt like that.
Scott Benner 50:10
Yeah. And well, you don't have to stick up for anybody I understand what we're talking about. Don't worry. I know they didn't leave you on purpose. But I'm saying you the end result is you feel abandoned. Your dad left, he died, your mom left, she kind of went and took care of herself. And you may she might have physically been there, but she wasn't helping you. And you were only 12 years old at that point. Right. Right. Yeah. And so you grew up 1213 1415 1617? Probably with your older sister helping you more than anything else, then you go off to college. In the middle of being at college, your mom lets you know she's not paying for you anymore. Right? Right. Yeah. So that's an abandoned feels. That'll make you feel abandoned as well. And then you abandoned your dreams to take care of your diabetes. Right? So you hate diabetes. And you're probably not thrilled with your mom. But she didn't leave you leave you so I'm assuming you write that off in your head. Are you mad at your dad?
Emily 51:12
I'm getting there. Now. I romanticized him for a long time. But I took it all out on my mom, because she was the one that was there. And she talked about being abandoned by your mom. She drove me I went to UC Santa Barbara. And so she drove from the Bay Area down to UC Santa Barbara. And for some reason, she had decided that she was just going to turn it's like six hours, six and a half hours, right. And she decided she was going to do the drive all in one day. So we got up super early. Everything was already packed, drove down there. unloaded my stuff. And then I turned as I put the last box down, I turned around, she was already in the car, starting it up and driving away. And she yelled out the window. Right when you get work.
Scott Benner 52:03
Were you guys broke?
Emily 52:05
No. Well, okay. i We there were more money problems. And she led on she just didn't tell me. Right. So you know, if she had told me if she had told us we could have
Scott Benner 52:17
you know, understood maybe? Yeah. Was your mom a nice person?
Emily 52:24
Absolutely. Yeah, she was a nurse. That's why they caught my diabetes super early, because I started showing symptoms over Thanksgiving, and then was in the hospital by the second week of December. So I still don't have knock on wood. Very many. You know, I've never been gone into ketoacidosis. As far as I know. Okay. Certainly never been hospitalized for it. I by optic nerve is still perfect. My kidney values are fine, except for the stones. I don't have you know, I don't have all the things that are supposed to happen. You haven't
Scott Benner 53:17
had any you haven't any, like ill effects from diabetes yet.
Emily 53:21
Yeah, that I would have expect to happen by now, given the fact that I haven't even bothered to really pay attention.
Scott Benner 53:29
When did you start to pay attention? When did you actually start testing your blood sugar?
Emily 53:35
In 1999, I moved up into the Pacific Northwest and saw a doctor and they said you know there's much better insulins that you could be on there's there's much better things that you could start doing. And so they gave me a book blood testing monitor, whose name I'm forgetting off the top of my head. It's the freestyle freedom like where you can have alternative blood testing sites. So I started using my forearm rather than my fingers because I could never handle the fingers. Okay. And so once I could do that, I started testing my blood more.
Scott Benner 54:24
So Mm hmm. Basically, when 18 years without testing your blood sugar, and then I getting that timing right about 18 years. 81 Yeah, I
Emily 54:34
was 3020 years.
Scott Benner 54:36
20 years. Okay, that's 20 years you didn't test. And then for the last, you know, the last chunk here, you've been paying more attention. So in the last 20 years, have your agency still been in the nines?
Emily 54:49
Um, the mid 80s. Low 90s.
Scott Benner 54:54
How much effort do you put into diabetes every day? Not a lot. Not a lot. Okay. So it's, it's not. I see. Do you know other people with type one? No, no, you don't know anybody else with it? Well, my sister
Emily 55:11
I did. I didn't know her. She was also not a good diabetic. But she hadn't been diagnosed she had it way before she was diagnosed with it. Because she was on her. She was in college, and she was on her summer bikini diet and eating like 500 calories a day. So it wasn't as obvious. You know, she was losing weight, which she thought well that this diet is working right. And she thought she was paying a lot because she was drinking so much water. She thought she was drinking so much water because she had. Yeah, she was supposed to drink eight glasses of water a day or whatever. Yeah, it all
Scott Benner 55:51
covered each other. Do you guys ever talk about your diabetes? The two of you?
Emily 55:56
We would complain about it. She died in 2014. I'm sorry. Okay, well, so let me get the overall grief thing out of the way. So you can understand. Okay, so I got to college in 1987. Pass a couple of kidney stones moved back up to the Bay Area in 93. And my middle sister starts to be antagonistic towards me, because we each got an inheritance from our grandmother. And I used mine and took a trip and backpacked around Europe, whereas she was married. And so she bought a house. And so she was mad that she didn't get to go to Europe. And so she, we never talked about this, but that's how I sort of felt about it. She was just always kind of, she had I was staying in her house. For about three weeks or maybe a month, I was working three different temp jobs until I could get enough money to move out. And then I caught walking pneumonia. So while I was out with walking pneumonia, my sister thought I was making that up. So she, if this sounds so much more Maury Povich than it really was, but she had my mom kick me out of her house. She my sister had my mother kick me out of my sister's house.
Scott Benner 57:32
Okay, I understand.
Emily 57:34
Which I didn't know you can do that. By letter. I didn't get to talk or basically what am i Mom writes, you know, you've always been the funniest, but also the most selfish, like this really harsh letter. And so I we, we kind of had a falling out after that, although it would kind of go up and down in 2012, so I moved to the Pacific Northwest Northwest and my eldest sister was in Pacific Northwest already. And in 2012 My mother dies, surprisingly, like no one expected it at all. So that threw us all for a loop. And then two years after that, my middle sister dies. They're not sure of what we would have had to pay like 1100 bucks for an autopsy. And we didn't
Scott Benner 58:43
know I was married with the house one, right?
Emily 58:46
Yes. Okay. And she's the one who also had diabetes. So when you have diabetes, and you die, they assign you we always used to joke that oh, you know, we get in a car crash they're gonna blame it on the diabetes right? And well, she was also on several different pain meds because she had terrible complications. She had a tracheostomy because of all the throwing up. She did, because she had What's that stomach disease when your stomach doesn't gastroparesis? Yes, she had gastroparesis. Her kidneys were basically shot. And so she died at the age of 47. It sounds
Scott Benner 59:37
like she was doing less day to day work on her type one than you were for sure. Well,
Emily 59:43
actually, she actually. I don't I don't know whether she was doing more or not. We never discussed it. But she had just always had because her diabetes had been noticed. Her diabetes had taken hold much earlier before she was diagnosed, that it just came with more crap. Like, I think even if she had a pump and the best everything in the world she still would have gotten gastroparesis, she still would have gotten the neuropathy. Um, yeah, I
Scott Benner 1:00:20
mean, I don't know how to say for sure what people what what things people would develop or not develop based on their care. I can tell you that I think if you get good care immediately, and you keep a onesies lower that that lowers your chances of these things happening but certainly it's not a not a foolproof system. But it sounds like a lot went wrong like it to me. I mean, a layman from the outside. It sounds like your sister's a onesies were really high. And it was just ravaging her in a number of different ways.
Emily 1:00:52
Yeah, she she would go into ketoacidosis. Like, every three weeks. Yeah. And well, the problem was that her doctors would fight with each other through her, like her diabetic doctor would say you need to do A, B and C and her her kidney doctor would say no, no, you need to do XYZ. In the meantime, she's in so much pain, and neither of them are giving her any pain medication. So finally she gets an okay, she's changes hospital and she moves up to, to Pacific Northwest. So all three sisters are together after mom died. And she lived near my other sister. And she was on disability. And so my eldest sister found her apartment and my niece was going to go over and just sort of help her out. You know, clean the cat box for her and stuff like that and hanging around and make sure she was okay. And within a month, my niece went over there and found her dead on the floor. And we don't know what killed her. But because she had a bottle of you know, legally prescribed methadone. They decided that oh, she she Odede.
Scott Benner 1:02:23
Was she a recovering heroin addict? Nope.
Emily 1:02:28
Methadone is a common pain
Scott Benner 1:02:30
is common for pain. Yeah. Oh, I didn't realize that. Yep. Okay. And it's really
Emily 1:02:35
good. I'm on it, too. And it's really good. It gives you it helps with just standard. Just the lowering of a pain
Scott Benner 1:02:46
changes your threshold.
Emily 1:02:47
Yes, exactly.
Scott Benner 1:02:49
What, what are you on it for?
Emily 1:02:51
I have chronic pain in my hips and legs and shoulders. My shoulders basically are like, stuck in Frozen Shoulder syndrome and have been for four years now.
Scott Benner 1:03:04
Well, that's a complication of type one frozen shoulder? Yeah, yeah, that's what they've told me. Are they? Did you get it looked at like by somebody who thinks they can treat it? Or are they just treating the pain?
Emily 1:03:17
Um, well, I have a pain management doctor that I also am seeing a physical therapist, I have a PHP, I'll be going to see an endocrinologist. Um, my pain is pretty well managed now.
Scott Benner 1:03:33
Okay. Do you have any considerations about like, maybe if you brought your agency down and got your variability a little stable, like your stability better than maybe some of your problems might alleviate? That would be great. Yeah. Because there have been people your age that have come on that I've talked about that. People with, with significant type one, complications, who were on their way to others, and then they found the podcast and got their agency down in some of those complications. I'm thinking of one person now whose vision was going and then he got his blood sugar down and stable and his vision stabilized.
Emily 1:04:13
Oh, well, yeah, that, that totally makes sense.
Scott Benner 1:04:15
Yeah. Do you understand? Like, why high blood sugars cause problems like this?
Emily 1:04:23
I'm in a very vague way I sort of pictured in my head as if Hi. I always picture my body's being sort of a cartoon. And so you know, like my optic nerve. High blood sugars. High blood sugar to me is like a cotton ball surrounded by steel spikes. So as it rubs up against the optic nerve, it shreds it. It's a sort of a weird No, no,
Scott Benner 1:04:57
it's not weird at all. It's how I think about it too. I I think of it as there's a certain amount of sugar that belongs in your blood. And that at the molecular level, sugar is jagged, just like you would see table sugar, but smaller. When you pack too much of it in your blood, you're basically being scraped or sandblasted from the inside out. Right? And, and all you need to do for that to stop happening and to give your body a chance to heal is to get a adequate, but not too low or too high level of sugar in your blood and find some stability, you don't want to be rocketing up and down, up and down. That's really bad for you as well. Right? Yeah, I. So Emily, in the last years, last couple of years, well, just the other day, actually, a company named Omni pod came out with a algorithm pump that will make your, you know, insulin dosing. Well, it adjusts your insulin as you go along during the day, you still have the Bolus for your meals. There's also a company named tandem that has a pump that does the same thing. Control IQ. Medtronic has a pump that does the same thing. There are three pumps on the market that do this, two of them work with your Dexcom control, like you on the pod five, like these things, if you got them on with even like reasonably good settings, I think your blood sugar would would level out, I think your agency would go into the sixes and stay there. And you know, then you'd really just have to worry about you know, your bolusing for your meals properly. counting your carbs, right understanding the different impacts of different foods and Pre-Bolus say a little bit. I really think there's a lot of success very available to you and everybody else, not just you. But you got to go get it like you have to. I mean, you got to go to a doctor and make them do it. Don't wait for them to suggest it to you. If that's what you want to do. But you're also at the same time you're battling all this grief. Right? You're in counseling. I guess how long have you been doing that? Um,
Emily 1:06:59
well, I saw one therapist for about 15 years, and then she retired. And so I've seen I've been seeing the one I'm have now for a couple years. Is it helping you? Um I'm having a slightly harder time adjusting to my new person. She's great. She's a little more in your face than I'm used to.
Scott Benner 1:07:31
What's the goal for you and you go to therapy?
Emily 1:07:33
Yeah, see, that's the problem. My goal when I was seeing my first person was to basically just express my grief and my rage and everything else in a safe space. And then prescribe antidepressants because I've been diagnosed with severe depression, surprise, surprise.
Scott Benner 1:08:01
How is your Shiva for your thyroid levels checked?
Emily 1:08:04
Oh, yeah, I'm on thyroid meds too. I'm on Synthroid Synthroid. Yeah,
Scott Benner 1:08:10
what's your TSH when it gets checked? Do you know it?
Emily 1:08:14
I don't know it off the top of my head. I get really bad about taking. I was only told recently that you're supposed to take your thyroid meds before you eat and right first thing in the morning like
Scott Benner 1:08:30
not not with any other medications or food. Right? Yeah. So you've been taking it? It's not been helping you? Right? Yeah. So one of the things that you might find with an unregulated hyper, you have hypothyroidism or Hashimotos. Have they told you? Oh, hypo. Okay. So with hypothyroidism, depression is one of the things that you that you get from having an unregulated thyroid very possible that could be from that. So taking your thyroid medication every day, at the same time, letting it stay in your stomach for an hour or, you know, at the you know, without putting anything else in with it. You might see an improvement just doing that for two weeks. And then continuing on but I mean, I'm saying in the first two weeks, you might see a real benefit that you have. Are you cold all the time? Does your hair fall out? Do you have dry skin?
Emily 1:09:24
I have dry skin, but no, my hair is okay. I'm not always cold.
Scott Benner 1:09:32
regulating your thyroids a really big deal. It also makes your blood sugar management easier. There's a whole series in the podcast about thyroid so you might like this podcast, you'd be surprised.
Emily 1:09:45
There's only so much self improvement I can do before I start to rebel because remember, I'm between 10 and 12 years old.
Scott Benner 1:09:54
Yeah, well, and we I don't know a lot about the psychology of people. Um, I'm certainly no expert, but I will tell you this, if you don't do something different, it ain't gonna end well. So, you know, you might as well like, I mean, if you're gonna find something to take serious, I would think that your that your physical health would give you the best chance. I would think that having solid physical health is attainable for you. I don't hear anything about you that says that you couldn't accomplish that. And then you would give you more time to work on your on your mental health. And you might, you might have an easier time with that when your physical health is is there. I mean, high blood sugars make people you know, it's altering in your mind. And low blood sugars are as well vacillating up and down blood sugars are hard on you. I think you I think you take your Synthroid every day, I think you listened to a few episodes of this podcast to figure out how to get your your insulin like regulated a little bit. And you might see a really different person 30 days from now, looking back at you. Are you up for that? Do you think? Or are you just gonna like like this thing on fire and ride it out to the end?
Emily 1:11:13
I don't know. I haven't decided yet.
Scott Benner 1:11:17
Well, that's up to you. But I'm like, No, but I mean, everybody in your life has gone, right?
Emily 1:11:22
Yes. After my middle sister died, and my niece found her. Two years after that my eldest sister died of a very rare cancer called gastrointestinal stromal tumor.
Scott Benner 1:11:41
Emily, I would take the fact that you're still alive as a sign that you're supposed to be here. I mean, because everything around you is a show due respect. Yeah. I mean, it's a it's a dumpster fire. And, and you're, for some reason, standing up in the middle of it, and you're okay. And you're at the very least alive. And I don't know, like, I mean, it's a really weird thing, because I'm not judging you at all. Like, if you just want to sit back and be like, I got a crappy hand dealt to me, and I'm just gonna ride it out. I wouldn't know. I mean, I couldn't blame you. You know what I mean? I don't know what you've been through with it. Maybe it's more than you can overcome. But, I mean, I think it's obvious that, that this path is going to end poorly. I mean, you've seen that with everybody in your life, basically. You might as well try a different path. I mean, what do you got to lose? Really?
Emily 1:12:35
Well, that's true. It's just a, I don't have a keep to itiveness that, you know, I get on these kicks where I'm like, Alright, I have found the solution. I'm gonna do this. And then like, after a week, I lose interest. And I don't know if that means. I don't know what that means. Or where I got that from. You know, my dad always thought it was because I was lazy. My mom always thought it was because I was lazy.
Scott Benner 1:13:01
I think my play pop psychologist with you. I would think it's because that somebody has sent that expectation out for yourself. So you're just trying to you're just trying to prove them right? I think you're just i All that sounds like nonsense to me. Like you're a reasonable person. You were here when you said you were gonna be today, right? You get your insulin, you buy your your CGM, as you go to your doctor's appointments, you get up in the morning you eat every day, you're, you do plenty of things you don't I mean, I feel I should get a cookie for that. Well, good, then have one I don't give it. Like definitely have a cookie like, like, feel good. Pat yourself on the back all day long. If you want to, I'd wear a shirt that says Emily rocks. That's fine with me. You know what I mean? But what I'm saying is, is that if you grew up with a father telling you for too, you know, for two years, every time that that test came back, hi, it's because you're lazy. First of all, no offense to your father. He didn't know what he was talking about. Either. It either did the medical community at that point? You were a child. So you're being told every day you're doing something wrong. In fairness, you didn't know what you were doing. So it's not like you were actually doing something wrong. It wasn't even willful, you're just doing what you were told to do. It was ending the way it was always going to end. Because you were set up for failure to begin with. And then along comes this person to tell you it's your fault. So they don't have to feel bad about it. Because what he really is thinking is, oh, I'm failing this little girl. But I'll put it on her. So he puts it on you. Then your dad dies, and your mom puts it on you. Right? And then life puts it on you. And you're just you're just living a self fulfilling prophecy of of you're trying to make them right. I'm lazy things don't go right for me. My sister died. My other sister died. My mom died. This is my lot in life. I'm gonna die. Here I go. I don't think any of that has to be true. Well, I will die. Well, it doesn't need to be today. You're 52 Well, no,
Emily 1:14:56
I don't think it's going to be today. Yeah, like let's
Scott Benner 1:14:59
like let's Let's get into this. Like, I'd like to see you back on this podcast 10 years from now be and look at me still here, baby. You know, seriously like, and I'm telling you, the only thing you need to do is understand a little better how your insulin works. Take your Synthroid on time. Do it every day. Don't don't I mean, look, if you're going to tell me that I'm going to get bored, then there's nothing I can tell you in return. I don't think there's anything your therapist is going to tell you in your return. You got to you got to prioritize you, and you got to stop listening to ghost voices tell you you're bad at this. That's how it seems to me, but I've only known you for an hour, 10 minutes, 17 seconds. So
Emily 1:15:36
it's still it's up? 17 seconds there.
Scott Benner 1:15:39
That's where I really started understanding.
Emily 1:15:41
Yes. I was gonna say something, and now I've just forgotten. Okay, well take your time.
Oh, my mom told me something really weird when I was, like, 30. She died when I was 32. So we were at a family function. And she she said, oh, did I ever tell you the plans that your dad had for you? And I said, plans. And she said, Well, he had decided that after graduation, you are going to go to school at UC Berkeley, which was laughable because my grades would never let me get into UC Berkeley. But they had both gone to UC Berkeley. And you would live at home until you met your husband. And then he would hand you over to your husband. Not that my dad was one of those religious people who thought you know, the man is the head of the house kind of crap. But he thought that I would need to be watched over my entire life. And so he would do the watching over until my husband did. And that floored me.
Scott Benner 1:17:09
Emily, would it hurt you to know that I think it would have been better if you were born and then left in the woods to your own devices? Well, I think if you would have grown up feral you might be in a better situation.
Emily 1:17:26
See, but my parents were both great. I don't want Oh, they were doing the 70s that they weren't
Scott Benner 1:17:32
Yeah, looking. I was born in the 70s to trust me, I know what you're talking about. Like, nobody was thinking about anything very deeply. You know, it's people were not, you know, if your kid wasn't dead, you're taking care of them. You know, the, the idea of you go to go into college was like a great thing. You know what I mean? Get out of here, we're not paying for you anymore, you know, be gone with you. You'd probably the only thing I think that you could hear today that would make you cry is that I'm considering after talking to you getting in a car and driving two hours to take my son something he needs a college. And I would think that, like that seems like something that no one would ever do for you. And, and it's just that I've made a decision to like, I've made a decision to be the kind of parent I think you wanted to have. And you got the kind that that you know, either got sick and died or was like, Oh, I'm gonna get sick and die one day, I better have some time for me and they stopped making time for you. You know, but you could do it for yourself. Do you have kids?
Emily 1:18:36
No, no, I have never really wanted children. And then
Scott Benner 1:18:42
that's cool. Like, I mean, are you married? Are you with anybody? You by yourself? I
Emily 1:18:45
am. I am married. I'm actually married to someone I went to high school with although we weren't dating at the time. But yeah, we just weren't interested in kids. I like cats better. And then I just thought my genes are not the genes that should get passed on. Respectable the future
Scott Benner 1:19:04
respectable decision. I wouldn't. I wouldn't say anything bad about that. Can we put this guy in charge of the Synthroid. I like him having a job in this.
Emily 1:19:12
Oh, he can tell when my blood sugar's low way before I can.
Scott Benner 1:19:16
I want him to charge to the Synthroid. I want him in charge of the Synthroid, I want you taking that Synthroid every day for 90 days. And then I want you back at your doctor to get a blood test to see where your TSH level is. And if you're, if your TSH is over two, I want you to tell the doctor I want my TSH to be two or below. And then let's get my medication. Right so that happens. And in those 90 days, too, you start taking a little better care your blood sugar's I'm telling you you're a different person after this is over.
Emily 1:19:43
Okay, well, I will tell him he gets up. We both work from home, but he gets up about an hour before I do. So I'll just tell him to wake me up and make me take my
Scott Benner 1:19:53
pill, stick that thing in your mouth, drink a little water. Make sure you have enough and then whatever. And that yeah, that hour over be perfect. I seriously, nothing wrong with needing help getting this going. You know what I mean? Nothing wrong with that. Let him help with that. And, you know, we'll tasked you with listening to a couple specific episodes of the podcast and see if you can't figure out how to use your insulin a little more effectively. This all makes sense to you. Are we gonna get off this? And you're gonna be like, Yeah, screw that guy.
Emily 1:20:22
No, I mean, I feel very motivated at the moment.
Scott Benner 1:20:26
Good. Well, great, then that's it. Let's leave you right here, then. Let me not let me I've done my job. There's no more talking to do. Excellent. I do want me to tell you the episodes I think you should listen to.
Emily 1:20:39
Um, weren't you going to email them? I don't have anything to write.
Scott Benner 1:20:44
We're just making the podcast. You don't have to write it down. Don't worry. Okay. Okay. Yeah, we just want the pelota here. You know what I mean? Yes.
Emily 1:20:50
Oh, sorry. Yes, please. i Please tell me them right now.
Scott Benner 1:20:53
See, look at you're getting a no. All right. So I think there are a number of different places and ways to begin. Do you? Are you comfortable with terminology? Do you think you know, the terms that you need to know for diabetes? Because if not, I have one? Yes, you do?
Emily 1:21:15
I think I think so. I mean, I was on one of the Facebook groups for a while until I realized that it wasn't the face group for me because it was mostly people talking about taking care of their diabetic children. And I didn't feel like I really had fun. I can't tell anybody how to take care of their diabetic child.
Scott Benner 1:21:36
May I, Emily, you're thinking about that backwards. So it doesn't matter if their kids are adults. By the way, there are a ton of adults in there. They're just quieter. They don't They lurk more than they talk. But the point is that taking care of a five year old diabetes, taking care of your diabetes, at its core is pretty much the same thing. So I let the let the other stuff go just look at the focus. But if I said to you, Bolus, you know what a Bolus is, right? Yes. Okay. Basal.
Emily 1:22:06
Bolus is the current that you you are based on that give you getting the most Okay. Basil is the kind you take would be taking your short acting insulin Bolus is belonging acting.
Scott Benner 1:22:19
You have those backwards. Okay. Okay, so Basil is your Lantis. Bolus is your humor log. So just having said that to you, I'm going to tell you that there's a series of very short episodes called defining diabetes, I'm going to send you that list. Okay, okay, there's three, five minutes long, they're going to pick terms and they're going to define them for you, it's not going to be boring. And then you'll you'll kind of have this idea of like these, these things that are going to come up in these other episodes. Once you have those, you move on to the Pro Tip series. And the Pro Tip series is just going to walk you through basically how I think about taking care of my daughter's blood sugar, it's going to be me, and the CDE named Jenny. Jenny's had diabetes for like 33 years. She's delightful. She's from the Midwest, right? So you can't help but love her. And I don't think they're boring. They're going to it's going to be one of the episodes is going to be how to start over one's going to be about MDI about Pre-Bolus thing about insulin pumping. And then some other ideas, some variables that might impact you how illness exercise, how those things might help, you might might impact your decisions. That's it. There's, there's not many there. I think if you listen probably to the first like 10 or 10 or so you should be in a better situation. So I would have you listened to the defining diabetes first than the Pro Tip series. And then if you like them, or you see them helping you, that's when I say just jump in. Because even if you think about your episode right now, like, if I asked you when this is over, what's this about? You're gonna say, I got diabetes, when I was younger, I've had a lot of grief in my life, and I'm struggling, right, except there's a ton of management conversation in this too. And that exists in every one of those conversations. So sometimes just hearing people talking about it, normalizes it. And that makes it feel you know, like it's not work it just I don't think of diabetes as work like you don't put much effort into diabetes you said but you don't get a return. I probably put about as much effort into it as you do. And my kids a once he's in the fives. And she doesn't have any diet restrictions. She had like some pasta and bolognese sauce last night when she went to that restaurant.
Emily 1:24:35
Yeah, but did she have a Christmas tree?
Scott Benner 1:24:38
Every year? Every year Emily, I swear to you, that's a wonderful, I wish I could find out what the hell that was about. Like you can have a Christmas tree with diabetes. Shame on anybody who wrote that episode. That article by the way.
Emily 1:24:51
That was not that was a joke in my family for years.
Scott Benner 1:24:57
Well, it should have been that's ridiculous. Alright, so hold on, I am actually creating. I am going to create an email to you right now. So that I said I literally don't forget, because I'm so hungry. When I get done here I am 100% gonna go eat something. Okay, do you feel okay about all this? Is there anything you want to talk about that we haven't talked about?
Emily 1:25:21
I just want to end on a funny story, if I may, please. Okay, so we took a trip to San Francisco, once my, everybody in my family it because I was like a, I think 11. And so we all went to Fisherman's Wharf, there was a favorite restaurant, my family would go to, and I was sitting, my mom would usually give me my insulin. When I was 11, just because it was easier. I mean, I could do it myself if I want to do but she just wanted to. So I was sitting sort of next to the wall, and my three, two sisters were sitting next to me. So it wouldn't really easy for me to get out and go to the bathroom and shoot myself. So mom, we had ordered our meal, and mom's like, Okay, I'm gonna shoot, you shoot, you now. Just get under the table. And I'm like, Get under the table. She's like, Yeah. And I'm like, okay, so I get under the table, and I stick my arm out. And she shoots myself, she shoots me, and I pop up. And the weight person is there ready to put my food down. And so she had a way person had shown up while I was under the table, saw that I wasn't there, turned around, picked up my plate and went to put it down, down. And then I was there. And she nearly jumped out of her skin. And we thought it was hilarious.
Scott Benner 1:26:50
Well, I'm, I'm sad that they made you get under the table to get your get your insulin, but at the same time, I think the story is hilarious. Yeah,
Emily 1:26:59
that is the kind of person my mother was she just caused very funny things to happen.
Scott Benner 1:27:04
So Well, it sounds like she was lovely. It sounds like in general, you guys were overwhelmed with diabetes. And we're not getting any help. And I hope that somehow this has been helpful to you. Yes, I really.
Emily 1:27:16
And I would like to add to anybody listening. I did and do love everyone in my family. So well, the little things that I'm talking about.
Scott Benner 1:27:26
Yeah, for context. Look, look, I have to thank you for your honesty, because you really were able to come on and tell stories that, you know, didn't shine people in the brightest light all the time. But you there's no need to say. I mean, to me, there's no need to say what you said. Because I don't think that what you said is an indication that you didn't love and respect and care for your family. I'm just saying that. You know, sometimes people are outmatched by the things they're asked to do in life. And sometimes those things impact children. And you were around some people who got outmatched a couple of times, unfairly points even to them. And then it just had the impact on you that it had. And it's not fair to you either. So you don't need to. It's not just because that's how their life went doesn't mean that that's how your life needs to go. I guess. If there's one.
Emily 1:28:15
Do you still think this is an an after dark episode? Oh, yeah. This
Scott Benner 1:28:19
is very sad. I'm incredibly sad. You're a little girl who? Listen, let's not go over it again. But no, I think it fits well. In the after darks. Have you heard any of the after darks?
Emily 1:28:33
Yeah. The one that caused me to write my email was the one with the woman who was a recovering heroin addict.
Scott Benner 1:28:43
Yeah, that one's tough. They're all tough. Have you there's a ton of them. There actually, are, I think of some of the best podcasts that we have. Because like yours, people come on, and they, they've gotten to a point where they recognize that they're going to be incredibly honest, because that's what people need to hear. So I appreciate that you did that very much.
Well, I'm gonna thank you for listening first, and I'm gonna thank Emily for telling her story. And then I'm gonna thank Dexcom and Omni pod for sponsoring this episode of the podcast. So here, I guess I don't have to do it. I pretty much did it. dexcom.com forward slash juice box, go check out the Dexcom G six. See if you're eligible for the 10 Day Trial Get started today. Omni pod.com forward slash juice box may be eligible for a 30 day trial of the dash. You can check out the Omni pod five, two. And what else you can get started with my link Omni pod.com forward slash juice box when you support the sponsors. You're supporting the podcast so thank you for using those links. Speaking of the sponsors, I almost forgot that I am contractually obligated to say this For full safety, risk information and free trial terms and conditions, also visit omnipod.com forward slash juicebox. All right, now we'll get to the other stuff. All the episodes that I spoke about with Molly are available at juicebox podcast.com, diabetes pro tip.com. Or you can join the private Facebook group, and then scroll to the top and click on the feature tab where they're listed for you. These are going to be the diabetes pro tips. This will be the diabetes Pro Tip series, The defining diabetes series and there's a lot else there's a lot else that's not English, there's a lot more, check out those lists in the Facebook page or on the website. If you're enjoying the podcast, please tell someone else about it. Please, please, please share the show. It's how it grows. And it is really growing. And it's because of you. And I can't thank you enough. Oh, what else? Seems like there should be more but this about an hour and a half in you probably get a little tired of me by now. So maybe I'll just let you go. Does that seem fair? I'll bring up a bringing another podcast very soon. You can check that one out too. Before I go, let me thank somebody in the Canada for leaving a really wonderful review of the podcast says I do not listen to podcasts. That's actually not what it says. It says I did not listen to podcasts before my daughter was diagnosed type one in February 2022. Now I listen to the podcast religiously and find that I have learned so much about good diabetes magic management, from the pro tip episodes, the pumping episodes and the ongoing exploration of how others with type one manage their disease. I am less than six months out with my kids diagnosis and feel like a mini expert on how to manage her disease and how to teach others about how to manage it. Isn't that lovely? That's all the way from the Canada that's a foreign country. Did you know The Internet even worked like that? I want to thank whoever JoJo jammer is by the way JoJo jammer cool name for leaving this wonderful review takes a few minutes to leave a well thought out five star review that helps other people see the podcast and think maybe I'll give this a try. So if you're looking for ways to promote the podcast, leaving a great review is one of them. telling a friend is one. Tell your doctor. You can go out the window if you want. I don't think it's going to reach anybody but do that. And while I'm thanking people here at the end. Do you know the there'd be no way for you to know I've never said this on the podcast I don't believe I think we're up to like six states in the United States where somebody has a Juicebox Podcast license plate, a vanity plate, like someone they say like juice box or juice box. Like stuff like that. I tried to show my children because I thought it was really cool. And they were like what what are people doing? I was like, I don't know, isn't this really great? They love the park so much. They did a plate for their car with it. Anyway. It'd be cool if you guys all did that. So couldn't you free time or whatever. Go get a different license plate. I'd like to have like a collage of all 50 states and not for nothing. There are license plates on cars and other countries too. So you know what I mean? Anyway, if you do that, thank you. It's very cool. It's heartwarming, but if you definitely do it, send me a picture, please. All right. Now I'm really leaving. I'm out of here. What do I have to say at the end? Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#696 Double Transplant
Michele had a kidney and pancreas transplant.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 696 of the Juicebox Podcast.
On today's show we'll be speaking with Michelle who's had diabetes for well over 40 years, but most recently has had a kidney and pancreas transplant. She's here today to tell us all about it. While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin. If you're looking for the diabetes Pro Tip series that begins at episode 210 In your podcast app, you can also find it at juicebox podcast.com diabetes pro tip.com, or a complete list of the Pro Tip series and other series on the private Facebook group Juicebox Podcast type one diabetes up at the top in the featured section. If you're enjoying the show, please subscribe in a podcast app and tell a friend
this episode of The Juicebox Podcast is sponsored by Ian pen from Medtronic diabetes, vn pen is a reusable smart insulin pen that uses Bluetooth technology to send dose information to a mobile app. And I'll be telling you more about it later in the program. You can also go to in Penn today.com. To find out more. If you have type one diabetes, and are a US resident or are the caregiver of someone with type one, please go to T one D exchange.org. Forward slash juicebox. Join the registry, complete the survey. And just like that you've helped people with type one diabetes and supported the Juicebox Podcast, they're going to ask you incredibly simple questions about type one, you'll know the answers, they're not going to be difficult. The entire thing will take less than 10 minutes. It is completely HIPAA compliant and absolutely anonymous. T one D exchange.org. Forward slash juicebox.
Michele 2:32
I am Michelle. I have been a type one diabetic for 45 years. And in May of this year, I had a kidney pancreas transplant. So that's why I'm on to talk
Scott Benner 2:47
I Michelle 45 years. All right. This is oddly going to be easy. Because it's 2021. So I just take 20 away, right? And now I'm down to 25 years, then I take the one away down to no way then I'll take 20 More away I get down to 1980. And what am I left with five? Did you were you diagnosed in 1975 76? Close? I was feeling pretty good about that. All right. That's, you know, I was born in 1971. Wow, how old are you?
Michele 3:22
I am 59 years old.
Scott Benner 3:26
You weren't born that much before me. 1962. So I'm just gonna say that a little bit.
Michele 3:33
I'm proud to be this old. I'm lucky to lift as long as I have.
Scott Benner 3:38
I'll tell you right now that I know you're saying that because you have diabetes. Right? Right. And when you're diagnosed, I don't have diabetes, I feel the exact same way. I got up this morning and I was like, I had my pants right. And my back is stiff as it always is. And I think to myself, Do I like Go for it? And just like pick my leg up like a person and stick them through? Or do I lean on something just to make sure I don't stumble?
Michele 4:07
That's pretty sad, but understandable.
Scott Benner 4:13
People want to understand they get older, right, Michelle? Exactly. Okay, gives them something to look forward to. I look forward to having to consider putting your pants on.
Michele 4:26
Struggle some days.
Scott Benner 4:28
I am determined to to fix this somehow. I don't know what I'm gonna do. I'm thinking about different exercises to strengthen. I'm trying different stretches but I just My back is hurt since I was like 20 years old. So I would like that to stop one day. I would just like to get up one day and not think about that. But I'm complaining to a person who had a couple of their organs pulled out and replaced with organs. So why don't I stop that and ask you a little bit about what it was like to have diabetes for 45 years.
Michele 5:00
Well, I was diagnosed at 14. So that was interesting. Because if you're, you know, getting right into those teenage years, and now something's wrong with me, which was very shocking, because I had been held healthy, pretty healthy up to that point. So, you know, I diagnosed spent a week in the hospital went home, I only saw a primary care physician. And I would see him once a year. So he would do a fasting blood sugar. And send me on my way for with my one shot a day of beef, pork insulin. So it went on like that. Boy for probably 10 years or so. Up, a friend of mine was diagnosed. A couple years later, she was she was a semi close friend, but not real close. And she came back from being diagnosed and was like, you know, you have a lot to do. And I'm like, not really take a shot today. That's pretty much it. All I have to do. So I went on for many years really, kind of living a normal life. With this one shot a day that I had to
Scott Benner 6:25
do, yeah. But what was testing like, then, like, how were you measuring success? Or where were you not?
Michele 6:35
I basically was not. So they showed us how to do the urine test. But to me, it made no sense at all to do that, because I couldn't do anything about it. So if it came back, hi, what do I do? There's there was really nothing I could do. They didn't really talk about increasing insulin or decrease in insulin. You know, they had me on the one shot today. So it was very interesting.
Scott Benner 7:02
So you could see you take this injection, and then their advice was to do the urine test strip, and then, but then no matter how the test came back, there was no next step.
Michele 7:15
Exactly. Exactly. So I had to eat at certain times during the day because you'd have those peaks and valleys for the insulin. But I'm a pretty relaxed person. So I wasn't on a strict schedule. It was more if I felt like I was need to do something. I would eat something my mother would make me breakfast every morning. So I would have breakfast right away. But beyond that, I pretty much lived a normal life.
Scott Benner 7:43
Okay. All right, and how long with high blood
Michele 7:46
sugars? Yeah, of course.
Scott Benner 7:48
You were were those urine tests usually high?
Michele 7:53
When I did them, but I quit doing them pretty quickly after diagnosis. I didn't really pay attention.
Scott Benner 8:04
I hear you. So I get that. How many years do you think that you did that just didn't just did that contest and did your doctor ever up your insulin like based on like weight gain or age or anything?
Michele 8:18
I just saw him once a year. And I don't remember him adjusting it. It was always like you're doing fine. Keep doing what you're doing. And like I said he was a primary physician. I didn't even know about endocrinologist at the time. So he diagnosed everything from diabetes to cancer to everything in between. Okay, and
Scott Benner 8:46
let's say Say that again, for me, you saw him
Michele 8:50
from 1976 to probably through college. Okay. So ad one, ad two,
Scott Benner 8:59
so he's not an endocrinologist. He's just a row. Okay.
Michele 9:03
And just a primary care. What general practitioner,
Scott Benner 9:07
what other issues did you have during that time?
Michele 9:10
Um, really? None?
Scott Benner 9:11
None. Okay. All right. So he just didn't do anything. You just kept injecting staying high and Japanese thing. winded. I'm like, I'm guessing that the technology changed somewhere and you changed with it or No,
Michele 9:23
I changed influence. I went to the you know, the synthetic insulin versus a beef pork. When that was available. I saw my first endocrinologist in the 80s because I went to was going to grad school. And I lived with my brother and sister in law and my sister in law was a nurse. So she recommended seeing an endocrinologist, which I went to his reaction was pretty much if you don't fix this, you're gonna die. Okay, and I, because he had me start doing finger tests, like at that point, the finger testing was available. So I would do it. And he had me doing it three times a day. And it was always in the two hundreds. But again, he didn't tell me what to do. And it was a little bit longer till they had that sliding scale, where if your sugar's this, take a shot, if it's this take a shot. So he didn't really give me a whole lot of information. So go ahead. Did you?
Scott Benner 10:33
Do you remember having any feelings about the information that you had gotten prior from the other doctor at that moment?
Michele 10:41
It was kind of shocking. It was like, Oh, I'm supposed to be doing something differently. I didn't know I had, I really didn't know. And but I thought I was doing what I was supposed to be doing. I, you know, do my show today and go on with life. I was went all through college that way. Did my shot a day if I like, spent the night at my friend's house or something, I just go back in the morning and take my shot. So it was just kind of a, you know, crazy time, or you especially now with all the technology that's available
Scott Benner 11:14
and what you can see now. Yeah, were you in your mid 20s. At that point, when you switch the insolence.
Michele 11:20
I was mid 20s. And then shortly after that, I was diagnosed with retinopathy. Wow. So that really scared me.
Scott Benner 11:29
Yeah. When you first get the hay, you're gonna die. If you don't do something talk. Do you even believe it?
Michele 11:37
I was kind of like, yeah, yeah, yeah, whatever. Like, I've been living this way. All this time. No one's ever told me anything differently. But I did what he told me to do, like, I'm a rule follower. So he told me to do this testing. So I did change the insulin I did. So that was my life. But, you know, once the right not that the came out. And I was dating somebody. And at that point, it was like, oh, I need to do something about this, because I don't want to go blind. So, you know, had laser surgery in both eyes. And that was probably 87. And, but I haven't had any eye issue sets. So they have been stable since then. I've got a lot of laser burns in the eyes, but the eyes have been very stable.
Scott Benner 12:34
Okay. Okay. Wow. That's crazy. Okay, so you're, you're so you're still doing it now. So now you're testing and you see your blood sugar's higher. But it takes more time to even get to the point where doctors are talking about making adjustments once you see your blood sugar.
Michele 12:53
Well, right. I mean, we they had the sliding scale, so then I would use that. Okay,
Scott Benner 12:59
about that point, what point in your life? Do you think the sliding scale popped up?
Michele 13:03
That was probably 8586 8586.
Scott Benner 13:05
Okay. That's okay. But it all makes a lot of sense. I'm just thinking back to when my friend was diagnosed in like 88. And I'm just putting the pieces together kind of backwards from what you're saying to this at all, that all lines up for me really well. But so when the retinopathy laser surgery in the 80s? Yes. What was that like?
Michele 13:32
It was a bright light flashing in your eyes. I probably had three times on my right eye, two times on my left eye, they would give a shot to numb the eye, kind of underneath that in their eye. And you would see bright flashes of light. I didn't like it. But I didn't want to go blind. So, you know, I kept going back for those.
Scott Benner 13:57
Yeah. And that and that. Plus, I'm imagining your control started getting better as well.
Michele 14:04
Right. You know, just because now I'm seeing of endocrinologist, I'm seeing a regular doctor. Then I met my husband in 87. We got married in 88. So he was there through the timeframe of the laser surgery. And, you know, shortly after that, I started talking about having a baby. Now my endocrinologist was like, I don't have time for you. So he ended up sending me I'm in Cincinnati, he ended up sending me to University of Cincinnati hospital that had a clinic for diabetics. And they were it was a study kind of measuring the effects of high blood sugar and low blood sugar on children that were born. So I entered that study and the doctors there saw me all you know quite often, even before I got pregnant to get the blood sugar's more in line, but they were proud played a Wednesday was probably still in the eights and nines at that point.
Scott Benner 15:05
I am fascinated that you there was a time where you could say to a doctor, hey, I'm gonna have a baby. And I'm like, yeah, get out. I don't want to be involved in this. But also that he sent you to a study, do you think he sent you to the study? Because they're like, well, this lady is going to provide good data if she gets pregnant, or do you think this study was meant to help you?
Michele 15:27
I really think that he, I think he didn't have time to deal with me and my blood sugar's so he sent me the study so they could deal with me instead.
Scott Benner 15:41
Alright, Michelle, are you telling me that that that standard care wasn't very adjusted, and you were trying to figure out something greater?
Michele 15:51
I believe once I knew better, I believe I stayed on top of technology and things like that. When I was pregnant with my first son, the nurse there had started wearing an insulin pump. And she suggested I get on it. But at that point, I didn't know how those worked. So I had my first child in 91. So I didn't know how the pumps worked. And my belly was so big, like, how is that going to fit on my belly? Because it was Medtronic back then. So I didn't start that till probably 9394, maybe 90, maybe 95 on the Medtronic pump.
Scott Benner 16:36
Okay. Wow. That's a that's really a tale. And now and you're still just, I mean, did you did you end up having a baby?
Michele 16:45
I had two sons. They were both healthy, healthy. They were big babies, but, but I was a big baby. So I'm, I'm sure part of it with the diabetes, but part of it was just having the genetics to have big babies. My first son was 10 pounds, or nine pounds, six ounces. And the second one was 1013. But I was 11 and a half when I was born, and my mother was not diabetic.
Scott Benner 17:15
Any other diabetes or endocrine issues in your family?
Michele 17:20
Yes. So my brother, I'm the youngest of eight. My brother, who is eight years older than me, was diagnosed at 14 as well. But he kept it really private. And he saw the same doctor as I did. So he had to boil his insulin needles and, you know, reuse the needle every day. So it wasn't a big shock. When I was diagnosed. We were all tested, when he was diagnosed. And none of us had it at that point. But I kind of had a feeling in the back of my mind that I was going to get it someday. I don't know why. But so when I was diagnosed, I was unhappy, but it wasn't a big shock. But again, I didn't see him living a very different lifestyle other than, you know, taking his shot every morning. Well, yeah,
Scott Benner 18:11
there was a lot of like, just masked ignorance right about what was Exactly, yeah. How.
Michele 18:17
And the funny thing is, we're a very smart family. We're not dumb. So it just the information wasn't available. You didn't have Google, you didn't have your doctor wasn't telling you. You didn't know it just
Scott Benner 18:30
didn't exist yet. It just you were doing the best that that was available to you. Exactly. How is his health generally?
Michele 18:39
His is not as good. He lost a leg. And he has trouble getting around now. He's still alive. So he's eight years older than me. 67. But not very healthy.
Scott Benner 18:59
Okay. Did he ever make the switch like you did.
Michele 19:04
He finally he got on an insulin pump. Gosh, I don't even know 1015 years ago, but it was much later than I did. And then he did try. He stayed with Medtronic. And he did try their CGM. But really didn't use it very often. And I talked him into the Dexcom. And I'm not quite sure how often he is. He doesn't like to talk about itself. Yeah, so we don't spend too much time talking.
Scott Benner 19:39
I understand. Okay, well, I appreciate you sharing that with me though. That's it's valuable information for the for the big pick. So
Michele 19:45
that's one. Pretty much everyone. All my siblings have thyroid problems one way or another either low or high thyroid. I have a nephew with type one diabetes. And there's talk about an uncle that had diabetes, but there was it was never very clear about whether he was type one type two or what, how that was related?
Scott Benner 20:13
Sure. What about genealogy? Where are your people from?
Michele 20:17
We are from Slovakia and Poland to half of each interesting. Thank you. My grandparents actually came from those countries.
Scott Benner 20:27
My wife's mother grandmother, my wife's mother's mother is Polish, and she had celiac. And they call it the sprue.
Michele 20:40
That's a new one.
Scott Benner 20:42
I guess at some point, it was referred to let me check celiac sprue I think it's been kind of like rebranded as celiac disease. Yeah, but at some point, it was called celiac sprue pets. That was kind of the, the general term for it. And my, my, my wife's grandmother, who was a generally unpleasant person, just she, she'd be like, I have this sprue I can't eat that. And it kind of went like that. That's great. It really, it really hurt her at the end of her life, because she finally I think she finally gave over to the dieting but way late. And, and it just then she was so old that the dieting for celiac, I don't think she was doing it. Well, she just lost so much weight towards the end of her life. Right. But anyhow, okay, so that's a lot. But I understand I appreciate you filling me all in on it. Now let's get to the fun stuff. Michelle winters really get upside down. Because I'm assuming it happened at some point if you ended up with a transplant right.
So here you are a person who doesn't want an insulin pump, but would like more functionality than a regular old insulin pen offers. If this describes you, you are the exact right person to go to in pen today.com forward slash juice box and check out today's sponsor in pen from Medtronic diabetes, here's what you get when you buy the M pen. First of all, it's incredibly affordable. And that's important. Secondly, you're getting a Secondly, you're getting a well built insulin pen. And that too, is important. But here's where in pen separates themselves from other pens. The M pen has an app. And it speaks to the app with Bluetooth and keeps track of things like your current glucose, your dose calculator, active insulin remaining meal history, dose history, glucose history, activity log and reports. That's right, my friend. The in pen gives you some of the functionality that people get with an insulin pump. Active insulin remaining that's insulin on board, there is a thing you thought you could only get with an insulin pump. But it turns out, it's also available within pen from Medtronic diabetes, head over now to in pen today.com. To find out more, do a little scrolling. And you'll get to the part of the web page that says pay as little as $35 for the impact. This is an offer available to people with commercial insurance and Terms and Conditions apply, of course, but this could be you a $35 insulin pen that has a companion app that keeps track of things that you want to know about. Do you know the Impact app even allows you to manually log your long acting insulin doses and set up dose reminders for your long acting insulin? It actually does that. Isn't that crazy? Oh in pen, what have you not thought of? Here's a couple other little things the pen does. Are you wondering if the pen allows integration with the Guardian Connect system? Well, yes, it does. The integration is compatible with both iOS and Android devices. However, you should check your compatibility for both the Guardian Connect system and the M pen app prior to ordering. So go get yourself the in pen from Medtronic diabetes and have an app that shows your active insulin on the homescreen and allows you to Paris many impairments to the app as you want. This enables the flexibility for you to have one pen at home and another at work or school. Are you kidding me? In pen today.com links in the show notes of your podcast player and links at juicebox podcast.com. But I think you can remember it in pen today.com That's my link you go to that. Find out everything you need to know get started with the pen. In pen requires a prescription and settings from your healthcare provider. You must use proper settings and follow the instructions as directed or you could experience high or low glucose levels. For more safety information. Visit in Penn today.com
Michele 25:16
Okay, so I mean other complications along the way. I have had probably almost all my fingers operated for trigger finger. I had frozen shoulders and both shoulders over time. But see again, you know once once I got pregnant once I was past that I would stay up on technology. You know, I got the insulin pump as soon as I could I got the CGM as soon as I could switch to Omni pod is I think I got the CGM in 2011. Yeah. Got the Omni pod in 2013.
Scott Benner 25:51
So you selling you know, I tried to stay on top? Yeah, ya know, you did exactly what you hear me talking about, right? Like, I'm always saying, you know, pay attention to technology, you don't want to be using the last generation of stuff, you know, keep up with what people are doing, you know, don't switch just the switch. But when it makes sense, you got to keep up because, you know, as we move forward, better technology is going to equal better results and better results are going to equal better health. Right? Yeah. You saw that and you got to it, your your brother either didn't see it, or didn't care to see it one or the other.
Michele 26:29
And he was eight years earlier. So you know, a lot of damage had been done by the time the technology came around.
Scott Benner 26:36
Okay, so you still felt hopeful? You think when when this stuff was available to you, like I can still do something about this for myself.
Michele 26:44
I never thought I never thought I had a shortened life or anything like that. I really just thought, Okay, it's just another piece of me and something I have to deal with. As I move forward. Yeah. So so the eyes checked me. And then over time, it's been a slow progression with the kidneys. So you know, you get a test at the endocrinologist, oh, you're you're creating levels that are higher than they should be. And that went on for years. And then, at one point, I finally said to my doctor, I'm like, should I be seeing a kidney specialist? And he's like, Yeah, you could do that if you want, you know, as the numbers were creeping higher and higher and the creatinine levels.
Scott Benner 27:30
Michelle, test me. Oh, nephrologist,
Michele 27:33
nephrologist. Yes,
Scott Benner 27:35
thank you, Grey's Anatomy, go ahead, keep going.
Michele 27:39
So I saw him and I'm not quite sure how many years I saw him, but I'm still feeling good through all this time. And I didn't really, I really never felt bad. You know, I still exercise I still do all the things that I'm supposed to be doing. I eat right. So then, at the end, January of this year, the GFR, which is what they look at to determine if you need to go on dialysis or have a transplant, it went to 20 or 18, beneath 20. So once it's 20, then you're eligible to get a transplant. So I'm still feeling pretty good. But I knew dialysis is can really be damaging to people. Yeah, so I went to four different hospitals and started just applying for transplants. So I contacted you when I was still in stage four kidney disease. And everything went pretty quickly. So I had to have a majority of tests. You know, you had to make sure your teeth are good. You have to make sure your heart is good. You have to make sure you get a stress test. A colonoscopy like every test in the world. MRIs, CAT scans, they've done every test on me in between January and May. May the end of May, I was finally listed at a hospital for a kidney pancreas transplant. Actually, two of the hospitals would list me one didn't want to because they thought I was too old. But the one I finally went with was really happy with the condition that I was in. They see they said they feel a lot of people younger than me that are in lot worse condition than I was. Okay, so I was listed. And three days later I got a call to get a pancreas kidney transplant.
Scott Benner 29:53
Huh? No, it was so quick. Show. Let me tell you something. So have you heard me talking about my friend Mike? whose past? Yes. Okay. So when he realized he needed kidneys when he started doing dialysis, I would say to him, like, you know, are you on the list, you know, get on the list. And he would always say I can, it's hard. There's money, it's insurance. It's this. And he always felt like, like too big for him to conquer the process. And then you just described how important it was like you went
Michele 30:28
after this, right? Yeah, I didn't wait. But you
Scott Benner 30:32
just were like, I am going to go find out how to make this happen for myself. Exactly. Good for you. Wow. Okay. So
Michele 30:41
right, because the first couple of hospitals I called, they said, No, we don't do any kidney pancreas under over 50. If you're over 50, we don't do it. So then I started doing more research calling around asking, and one of the hospitals I actually went with, told me that they do, do pay increases over the age of 50. But they wouldn't listen to me for that. They would only listen to me for kidney.
Scott Benner 31:08
So Wow. So this is exactly what he used to talk about. Like they always sounded like some people say they'll do both. Some people say they won't, blah, blah, blah, like and so you just had to keep looking to find somebody to do both. Exactly. Michelle, do you not have diabetes anymore?
Michele 31:26
You know, I asked that question yesterday. I'm like, am I type one diabetics? So the answer is, yes, I am still diabetic, controlled with a pancreas transplant. But I have not taken insulin since the transplant.
Scott Benner 31:44
Yeah, that almost made me cry. Michelle, actually, hold on, it might still give it. Hold on, I gotta do that wavy thing that you see ladies doing? Why does that work? By the way, we need to hear up if you just put some cool air on your face. It slows it down. I don't know. I don't either. But trust me, I do it a lot while I'm making this buck. Wow, that's incredible. Good for you. Do the downside of all this is.
Michele 32:12
All right, so there's lots of pills. So over time, I'll reduce the number of pills, because I'm only five months out at this point. So I have to take pills for digestion. I'm told those will go away. Eventually, I take anti rejection pills. So I have three different anti rejection pills, they need to take twice a day. I was recently told I have a low white blood count, which could be related to some of the medicines that I'm on. So you have to be very careful. I am constantly washing my hands. I'm constantly using hand sanitizer, wearing a mask, in crowds, and so on and so forth. So it's not just a breeze. There's still other things you need to do. But I'm feeling better every day. I've got a scar from my chest bones down all the way down. That's healed well. And I think because I was in good health forehand, at least I'm considered myself in good health. I think everything's feeling well. And doing well. Wow, congratulations.
Scott Benner 33:26
All right. So I want to walk through it. You get you get it all set up, and you find a place that's going to do both. Is it fair to say that without the kidney transplant, like what would your life have been like?
Michele 33:43
I had already been tested for doing peritoneal dialysis. So they were already talking about putting the tubes in, which would have been doing dialysis at home every night for eight to 10 hours every night and then another session during the day. So that's taking fluid into your belly, letting it sit there and draining it out every night and every day.
Scott Benner 34:13
And that's not necessary. Even if you did that every night and every day for your whole life. It doesn't mean that things wouldn't continue to go backwards, right? Correct. Yeah. So it's not like you're not stopping it in that even though that sounds like a unpleasant way to have to live. It's not like it would never get worse than there you would continue on. On exactly,
Michele 34:33
which is why I wanted the pancreas because I'm hoping to slow down some of the damage caused by the diabetes.
Scott Benner 34:39
Right. And surgeons must have felt comfortable about it because they gave you the organ Right? Exactly. Yeah. Okay. All right. So when let's start with the day you find out you're gonna get the surgery. What happened? Alright, you when Michelle we've got you know, you're on the list, right? So right Once you're on the list, is it's a matter of matching from donors, I guess,
Michele 35:04
yes, it's a matter of matching the blood type, as well as any antibodies that you currently have in your system. And I don't quite understand all of that. There's a lot of and I've asked, ask people, and they said, it's just it's very, very complicated how they match people with a donor, and you want to be as close as possible to the match, so that you're not rejected. I was lucky to have a B blood type, which means I'm a universal receiver. I can't give to any other blood type than my own, but I can receive from all blood types. So that helped.
Scott Benner 35:45
Okay. And then what was the, the amount of time between? Yes, you can be on the list and hey, we have your stuff.
Michele 35:52
So that was a Wednesday? Yes, you're, you're formally listed. On Friday morning, I got a phone call at 8am. And I didn't answer it because I didn't know the phone number. But then my husband's phone rang. And he answered it, and they're like, Okay, we have a possible donor. You need to hold on and look for this phone number and answer the phone. And if it is going to be your donor, you'll have to come to the hospital to tomorrow morning. So Saturday morning, so you have one day to get your things in order. And in February, I had a new puppy born, so most of that day. So the puppy was born in February, I brought it home in April, thinking I'd have all this time to train her. And so most of the day on Friday, I was trying to figure out what I was going to do with her because my husband works. He can't take care of her. I was working from home, which was helpful because I you know, I could do training in between the times and take her for walks at lunch. So my kids ended up like taking her the day I went into the hospital and drove her up to my sister's house four hours a day so that she could hold on to her while I was recovering.
Scott Benner 37:19
Let's be honest, though. Did your sister do a good job training the dog?
Michele 37:23
She She did a great job. Are you worried she ever lessons? Yeah, no, she did. She's she's an animal lover. She's had animals all her life. And I knew she would do a great job with her.
Scott Benner 37:35
So it must have made your boys feel good to do something. Like kind of like wholesome for you as you were heading into surgery too. I would imagine Exactly. Yeah. How about them? Do they have any autoimmune stuff? The kids?
Michele 37:47
They do not I had them in testing. I don't think it was called trial net then. But because I was in that program. I followed up at the Children's Hospital with testing from for them early on. They hadn't had any antibodies, or whatever the things are called for markers.
Scott Benner 38:06
Michelle, do you think it would be absolutely ghoulish if me if I said trialnet.org forward slash juice box right here.
Michele 38:13
Go ahead, go right. Are you telling? I keep telling my son to have his son tested? And so yeah, I'm all for trial on it. But that was probably the beginnings trial net wasn't really an existence, I think when they started because it was 9193.
Scott Benner 38:31
Okay. Oh, yeah, probably not. You were just getting that testing through a different way. You probably knew a lot of things because of the stuff you did earlier in your life. Right with research.
Michele 38:41
Right? Right. I kind of stayed on top of that. So yeah, they did that we I took them to Children's Hospital for years after that, you know, having them get different kinds of blood tests along the way. And then my younger son recently went back and had more testing done. And he still did not have the markers.
Scott Benner 39:02
So I'm good for him. I'd be nervous too. If you are my mom you understand? Yeah, no kidding. Let's look one more time. Okay, I'm sorry. So now we've got the dog squared away and we're sitting around Are you sitting in your house thinking this isn't gonna happen or it like is it hard to feel hope? Is it I
Michele 39:24
thought, no way is this going to happen? Because I've read you know, my kidney groups on Facebook, I'm on kidney pancreas groups on Facebook and you know the time it takes to get tested and the number of times people have to go and wait at the hospital and then it doesn't match for some reason. So I went on Saturday we went got there at 7am sat and waited and waited and waited they had to go get the organs. They had once they brought the organs back they had to so as I understand it, when they To acquire the organs, they have to wait for the heart to be taken out first, and then the liver. And then so the other organs get taken first, and then the pancreas and kidney come out. So each doctor team, oh, okay does their own organs, so they fluid back. And then another doctor had to take a final look at the organs to make sure that they were still viable when they were back in our location. And I don't know who my donor was, I don't know where it came from. I don't have any of that information unless the donor family wants to tell me Can we?
Scott Benner 40:37
Can we ask you about guilt? Like two things? So did you feel like you were jumping the line? Because it was happening so quickly? And is it a weird thing to be happy about somebody passing away?
Michele 40:52
It is. It is it's, it's odd. But the way I kind of look at it is they were probably already on life support when I got the call. So if it wasn't going to be me, it was going to be somebody else. So that kind of helps me with the guilt of taking it from someone named Michelle, I'm happy it's me. Yeah,
Scott Benner 41:17
I don't think you should feel guilty. I'm just imagining that it has to be a natural reaction.
Michele 41:23
Right? I think if I knew more about my donor, I probably have even more feelings about it. But at this point, I'm just happy. I'm blessed to be able to been on that list at the time I was and been available. I asked them when I was called, is there a backup? And they said, a backup person. Like if I don't give it they will get it. And I was the only person I guess in the country that was a match for this organ.
Scott Benner 41:51
Good for you. I mean, yeah, it's amazing. I would, I would have been like this is nuts. Just because you were probably just resolved right? Like this may happen. It may not happen. It's going to take years.
Michele 42:04
Right? I thought I thought six months, I really thought okay, it'll be a while. Because if it's kidney only the weight per kidney only is like five years plus. Or you can do a live kidney donor, which you can get quicker. And I did have people that said that they would get tested. No one actually had gotten through the testing yet because they don't test them until you're formally listed.
Scott Benner 42:30
I want to know what to ask you so badly. If you believe the people who offered or not, or do you think they do you do? Yeah, okay. I do. I do you know what I mean? Right? Like, I'm not being a I'm not being a jerk. I'm just like, I wonder how many people just out of like, you know, like, are like, Oh, Michelle, I'll get I'll do it. Yeah, I'll do it. Like, you know, do you mean yeah, that's what I was wondering. Oh, this is this is all kinds of
Michele 42:57
friends contacted me because I put something on Facebook just I wasn't asking. I just kind of did my situation update. And two of my friends from grade school that I haven't really stayed in too much contact with over the years. Both offered to get tested. How did
Scott Benner 43:18
that make you feel? Like I imagined it's a it's a wonderful feeling. But do you question it like, Have you ever considered like, I don't know if I'd give my kidney to somebody.
Michele 43:28
I was so grateful. So grateful. It just amazed me how generous people can be.
Scott Benner 43:36
No, it's really fascinating to me. i That's those people. I'd like to talk to one of those people. Somebody somebody that just said yeah, you can have one of my kidneys. That's you don't I mean, like that's a special statement. Right? Exactly. Okay, so you're it's five years of the five years for just the kidney what was what was the expected length for both again?
Michele 43:59
They didn't really tell me but they told me probably within a year, I would find a match. Wow. Because because it's two kidneys or two organs versus one. And pancreas is aren't in as high demand as kidneys are. Oh, I
Scott Benner 44:14
see by asking for the pancreas as well. It moves. So most people are just looking for kidneys. Right? Oh, so by by matching to you we don't waste the pancreas. Exactly. I'm getting it now. Michelle, I'm really coming online here with this. Okay. So, okay, so you're in the hospital. They're like, wow, this is gonna happen. Do you freak out? Are you nervous? Do you have any second thoughts?
Michele 44:42
We waited all day long and I didn't think it was I I tend to think of the worst outcome so that I'm not disappointed. I'm more happy so we didn't really know you know, we're waiting waiting. There's really no word or problem. really their Gosh, at their at 7am, it was probably 12 to 14 hours before they finally came in and said, Hey, listen, we need to do an enema because you're about to go into surgery. I'm like, okay, so all day long, they did not have me eating, but they just wanted to make sure your system is totally clear. And then it happened so quick, like they put me on a stretcher, wheeled me back, my husband saying goodbye to me, as we're wailing back. And I was knocked out.
Scott Benner 45:38
Is there any, any concern about just not making it through the surgery beyond the general concern about being put under?
Michele 45:48
I think my husband was worried about that. I really didn't think that that was a chance. So I just naively, but I just thought, hey, I'm getting this done, and I'll be fine.
Scott Benner 46:01
Did you have that moment on the gurney? When you looked at him? You thought he thinks I'm gonna die?
Michele 46:07
afterwards? Not at the time, but after a couple three comments, and I'm like, Ah, he didn't think I was gonna make it.
Scott Benner 46:16
I gotta be honest with you. I had my appendix out in an emergency situation. And I was like, on the phone to people. Like, I gotta say, oh, no, it doesn't seem crazy to me, they're gonna put you to sleep and cut your body open. I mean, I know people do it all the time. But it's some some people don't react well to anesthesia. So you know, I was doing my diligence column, my call my peeps, you know, let everybody know. But this sounds like it happened super fast for you. How long was the surgery?
Michele 46:51
The original surgery was seven or eight hours. And then the doctor came back and something was too tight. So then I was in surgery for another two to three hours. So in he had to bring the whole team back in, because they had gone home went to bed. So he had to bring the whole team back in and had more surgery. Meanwhile, my husband is there in the waiting room, wondering what in the world is going on going on? And only getting, you know, bits of information back? Oh, we have to take her back in. didn't really explain why they had to take me back in.
Scott Benner 47:30
Let me understand the process seven or eight hours for the surgery come out. You're in recovery. And pretty quickly. They realize you have to go back.
Michele 47:37
Yeah. And I was not awake. I don't remember being awake during that time. So I didn't know anything about it.
Scott Benner 47:44
Okay, something was too tight. And then they can you you know, it's funny as you're talking about this. I'm like, how do they do that? How do they perform surgery for seven hours?
Michele 47:57
I know they had two different surgeons, one for the kidney one for the pancreas.
Scott Benner 48:03
I'm just telling you, I can't stand that long.
Michele 48:05
Yeah, exactly. If you like, some special people. Yeah, they can be called at anytime, day or night, and they have to come in and do the surgery. So they're very special people are go collect, you know, click the organs for more, they need to be collected.
Scott Benner 48:22
My mom has to have surgery next week. And my brother had already made plans to come in to be here a number of days prior to the surgery and after the surgery. And then they up and called us yesterday and said we need to move the surgery to the following week. And I said please don't do that. You know, like I my brothers. My brother's not a wealthy person. I don't imagine he bought refundable airline tickets. And you know, like, right, you know, stuff like that. And so she calls me back an hour later. And she goes, we're just going to do it the next day. And I said, Oh, that's wonderful. Thank you, the doctors just gonna tack it on to the end of his schedule. And I was like, Wow, what an amazing thing. You know, I'll just do one more surgery on Thursday so Bev son can fly in and see her before her surgery. And I was like, wow, yeah, some doctors are amazing. And some you don't get anything out of
Michele 49:12
and I think you know, they have a whole team of people. So I think you know, you've got the original the people coming in that are prepping you and the anesthesiologist and the you've got a whole team of people that do the the closing up afterwards. So I think everyone has their specialty that they stay in for some I'm sure they have breaks during those that 1011 hours
Scott Benner 49:34
still amazing. So you come out how long does it take you to come to and then what do they expect from you? They want you like nowadays they get you moving pretty quickly after surgery. But what was your process like?
Michele 49:46
I I was in the hospital for two weeks.
Scott Benner 49:51
About your I
Michele 49:53
had, like I had some problems. So I think most people are six to eight days. That's what they tell them. But I had some problems like at one point, I couldn't keep any food down. I got Botox in my stomach. Which was, you know, I joke that I got Botox, but it didn't make me look any better. I imagine what that was supposed to do is make your stomach more active to move the food through because I was having trouble keeping anything down. Then electrolytes were kind of out of balance. So I had to have fluid and magnesium and potassium and phosphorus and all those kinds of things added.
Scott Benner 50:34
Were you in danger? Or is this just things they had to do? It?
Michele 50:40
This was ask your question again.
Scott Benner 50:42
Were you in danger? Or were these just steps that needed to be taken? Because
Michele 50:46
no, I think this is it was pretty common. Okay. For the surgeries. Just did people have different kinds of imbalances after that type of surgery?
Scott Benner 50:58
Okay, two weeks, and, and when did the medications begin, right away, antirejection, all that stuff, right away, right away,
Michele 51:08
right away. And then for the first three months, they're really, really careful with you because you have so many anti rejection pills at the beginning. And they say really, within the first year, it's really important to stay healthy through that first year.
Scott Benner 51:24
Did you ever hear Nicole's episodes about her surgery?
Michele 51:28
I did. Yeah, I did. I've listened to you quite a bit. And I'm actually still listening. And I don't know why. It's kind of crazy. But I contacted you back in 2016. When I had my agency had gotten to 6.3. So I messaged you on Facebook. And you said congratulations. Then after that. I was volunteering with JDRF and trying to get people set up for booth at our JDRF tonns event. And I contacted you and you said you couldn't come out to get a booth. But you could maybe do flyers or something and you never sent them. And
Scott Benner 52:21
so I'm very busy. I'm a one man show here. I'm so sorry.
Michele 52:23
I know. Well, then then you came I think the next year or the following year and spoke at Cincinnati. JDRF. tell
Scott Benner 52:31
people how good I was.
Michele 52:33
You were excellent. Did you talk during the luncheon?
Scott Benner 52:38
I did I asked for that actually. Because while everybody's busy wanting their own little space. I'm like, I always think everyone there has to eat and they eat at the same time. So I get to talk to everybody if I eat if I speak during lunch. There you go. Yeah, it's a I remember that there's a big room. It was a really well run event as well. Exactly. Yeah. No, i i It's uh, as far as those things go, I think of that one is almost a gold standard. The person who runs that chapter is type A and the best way and that that event goes off very, very well. I you know, I met Chris Rutan there for the first time. I met him in person.
Michele 53:23
Yeah, I saw him speak when he was there.
Scott Benner 53:25
Did you Okay, yeah. Okay.
Michele 53:27
And then. So, so yeah, I was actually on a panel that day of adults with type one. So the night before they had that reception, and I met you briefly while you were there as well.
Scott Benner 53:44
Oh, at the home was someone's home. Yeah. What is? What is art asking me Hold on a second. I'm sorry. You're fine. She's like, can I call? Can I call who? Me? I'm sorry, this is out of nowhere. I'm trying to figure out what this is. She's had trouble with her loop app earlier. And I helped her through it. Okay, she's gonna call me let's find. Let's find out why together Michelle. I'm just gonna keep Okay. Well, I'm gonna take off one of my earphones. Hey, alright, what's up
Oh, are you home still
so, honey, the problem is there's a little bit of a there's a glitch in the loop app and I need to reset it. So we have to have your the Bluetooth has to be off for like 20 minutes before we do it. That's why I had you do it when you came home when you told me it was working okay, so it's not gonna work till we make this little adjustment in the timezone. It's a glitch in the app. So when are you coming home again? were you headed to a restaurant? Oh, okay, well shut your Bluetooth off. Bring the food home when you get here. Come right to me and we'll do the fix. Okay, and watch your blood sugar on your deck. Stop yourself. Alright, bye. Sorry, Michelle technology let us down there. There's a small glitch apparently in the version of the loop app that Arden is using. And if you try to change the insulin sensitivity, and the timezone in the app is wrong. It crashes the app. So anyway, I don't know if that sounds like gobbledygook to you or not. We should I lose you. Michelle. Michelle, the show my Hello Michelle. Hello. Hello. Hello. Michelle. What the heck? Alright, I'm gonna stop recording. Michelle. Michelle, Michelle. Michelle. Michelle. Hello. Hello, Michelle. Michelle. All right. I'm gonna send her a chat. And you hear me? Hello. This is the end. Aquarius? Why would that song pop into my head? On Aquarius. Michelle Deanna, I can hear her typing. And she's not answering me. See if I have a phone number for do. This is boring. There's no way I'm leaving this in. And yet every time I say I'm not going to leave something in. I totally leave it in
Alright, I've texted her. I said, Hey, it's Scott. I can hear you typing but you can't hear me. And then I said it out loud. In case you maybe would hear people do not want to make a podcast. It's a lot of work. And sometimes it's irritating. And annoying and weird. Why is she unable to hear me? Michelle? Michelle. Michelle. Michelle. Michelle. Michelle. Hello, Michelle. She is not here
all right. I'm gonna call her will she answer this while she thinks she's making a podcast? No, right.
Michele 58:47
I can't hear you at all.
Scott Benner 58:49
Oh, okay. Michelle. Huh? She can't hear me at all. Why would she not be able to hear me?
Michele 59:06
I don't hear you. Hey, Michelle. I
Scott Benner 59:08
know we're on the phone now. But I hear you fine. And you're not hearing me. So let me I hear you through the phone. Yeah, let me figure out why that is. I don't know why that would be on
Michele 59:19
mute somewhere.
Scott Benner 59:22
I'm looking that looks right. Nothing here changed.
Michele 59:29
The lower left hand mute my audios that
Scott Benner 59:33
No, I didn't mute anything. I actually was like, keeping you on. I was recording with you. I wanted you to hear the phone call. Like just because I thought I didn't know if it would be interesting for the podcast. Not like I'm not muted. I'm gonna mute myself now. And then unmute myself again.
Michele 59:50
I heard the first part of the phone call but then it went away.
Scott Benner 59:54
Wait, can you hear me now? Through your computer? No. That's insane. There's nothing different here. All right, well, that's no,
Unknown Speaker 1:00:06
I hear you now.
Scott Benner 1:00:07
Oh, okay, I'm hanging up the phone. Now you can hear me. Yes, that doesn't make any sense. But who cares? I'm sorry. So you, you didn't hear all that Arden's having problems. Her loop app has a glitch in it, and it crashed the app. So she's gonna have to come back here in a couple of minutes. You're gonna hear me fix the app again. But she'll be in person when that happens. So I don't think anything should change on the audio. Okay. Okay, I am sorry, that was so long. I forget where we were. But I hope you
Michele 1:00:40
I don't remember either. We talked about post surgery.
Scott Benner 1:00:44
You were going through your medications and and everything you were taking after post surgery, told me that you had some trouble digesting. And then
Michele 1:00:54
yeah, that was in the hospital.
Scott Benner 1:00:57
Sorry, we were in in Ohio. You were telling me about being there. And I was getting ready to ask you. Because you were talking about having seen the been listened to the podcast for such a long time. So why why are you still listening to the show?
Michele 1:01:12
Don't know? The stories are interesting,
Scott Benner 1:01:16
I guess. Yeah. Do you feel bad for not having diabetes anymore?
Michele 1:01:20
No, I don't feel bad. I do know that my body can attack my pancreas again, because I'm still have those more markers that I had before. Those don't go away. Yeah.
Scott Benner 1:01:34
Right. And so it is possible that you could just get type one again with your new pancreas. Right, exactly. Is that based on other transplants?
Michele 1:01:46
I haven't found them. People, like the hospitals will track transplants, like after one year after five years. And they don't do a great job of tracking things after that. Okay. Which is kind of interesting.
Scott Benner 1:02:03
Gotcha. Well, let's just say that would suck. And I hope that doesn't happen.
Michele 1:02:09
Me too. Me too. But I think the technology will be so much further by then. That it won't be such a pain.
Scott Benner 1:02:17
Yeah, well, I mean, you you really are pretty caught up where you are until all of this until you put your pump in a drawer, I guess. Right? So like retiring? Did you like fold it up and put it under your underwear or something like that? Or?
Michele 1:02:27
I wore the Dexcom for about two months afterwards? Because I was afraid it was gonna get the sugars were gonna go high. And then it ran out one time. And I'm like, I'm not putting that back on. Why should I wear it? Okay, so I quit worrying. It
Scott Benner 1:02:44
was pretty cool. It really is. How scary is it to have all this going on during COVID.
Michele 1:02:52
It's worse during COVID. Just I feel more isolated. I can't really it my problems are kind of like COVID, where you can't see COVID. And you can't see all the germs in the system. So you don't really know where it's safe to go and what's not safe to do. So if I'm in public, if I'm in a group of people, I'll wear the mask. If I'm just around a few people I won't. It's much more easy to find a mask than it was probably prior to COVID. Yeah.
Scott Benner 1:03:28
You go all the way using it again. And 95 mask? I do. Yeah, I would. Yeah, I put one over my eyes. If I was you, just in case.
Michele 1:03:37
I know. I work I work glasses most of the time. So I'm a little protected.
Scott Benner 1:03:42
I would wrap my whole head in one, just bubble wrap people would be like what's wrong with her and I'd be like, I just had a transplant. Get away from everyone get away from me. But the feeling of isolation is real. It's terrible. You know, so I feel free there. And you said the first
Michele 1:04:01
I just had a baby granddaughter. I have a three year old grandson and a newly born baby granddaughter, and I've gone over there and saw them. I wore my neck the whole time because I'm worried for her too.
Scott Benner 1:04:15
Yeah. But congratulations. That's lovely. Thank you. Good for you. How's your husband handle all this? Has he been helpful? Did he do like is he like, standard guy thing? Does he stand in the corner and wait for you to need something? Or has he kind of jumped into action?
Michele 1:04:31
He he tries to be helpful. I mean when I was in the hospital. So the hospital was two hours away from Cincinnati. And I had to go two times a week after I was released from the hospital. So I actually had my top four brothers and sisters are all retired and they spent a week to 10 days with me and driving me back and forth because I couldn't drive for a while and But he would when I was in the hospital, he would come home from work, drive the two hours, sit with me for two to three hours, drive home. And then you know, wake up the next day do the whole thing again. So he runs his own business. So he doesn't have the luxury of just calling in sick, you know, he's off to do the work.
Scott Benner 1:05:20
Somebody got paid for those pills.
Michele 1:05:22
Exactly. Do you and I'm still working. So I carried the family insurance, which is good.
Scott Benner 1:05:30
At this point. Yeah, good for you that you're able to work through the they gave you would you take like FMLA little medical leave, and then come back start
Michele 1:05:39
short term disability for the first three months. And then I came back and they're allowing me to work for from home for six months, because the hospital requested that I do that. Excellent. How do you like working from home? I love working from home. So I've been working from home for a year and a half now. And it's awesome.
Scott Benner 1:05:58
I have to admit, I enjoyed myself. I don't know like the best probably is just very, you know, I don't know how interesting this is to people. But I love that I can get up in the morning, do a bunch of my work, record an episode, go, you know, grocery shopping, if I have to then come back and start working again. Like it's so it's so nice not to have to do stuff like that. At the end of the day when you're exhausted. It's so much easier to work until you're tired and then stop at the end. I do find that I work too long. Because I because my job's at home. Yes, but But I do like the knot. I do like that part of it like getting to break up the day. I do wish I had to move around more though. And that that. Well, that's right.
Michele 1:06:43
I did get my puppy back. And she has way more energy than I ever expected. So I get out at lunchtime and take her for walks. I'm up to like, I don't know, a mile and a half a day taking her for walks. So that's good.
Scott Benner 1:06:57
How long did your sister have the puppy?
Michele 1:07:01
About three months? Wow.
Scott Benner 1:07:02
Did she have trouble giving it back to you?
Michele 1:07:05
I think she was ready for me to get her get her back.
Scott Benner 1:07:09
So not attached. She's like, Please somebody come kick this
Michele 1:07:12
off. She was shocked at the puck he still remembered me. But she did. We met about halfway and picked her up. And she still remembered me and came home and is very attached.
Scott Benner 1:07:25
That's excellent. Good for you. Is there anything? We haven't gone over that I've missed? Because I don't understand the whole process?
Michele 1:07:33
I think we hit a lot of things. I don't I don't have anything that I can think of off the bat.
Scott Benner 1:07:41
Yeah, what is your moving forward look like? Oh, you thought it's something go ahead.
Michele 1:07:46
I was just gonna say the reason I wanted to why I didn't really want to be on the podcast. But the reason I contacted you was because you can't find anybody going through the kidney issues. Like there are a lot of people online but no podcast, no type one diabetes, talking about complications and things like that. And I wish I you know, I listened to Nikki, listen to her calls, but having people with real life experience is so difficult to find. So I broke down and said, Okay, I'll be on the podcast and contacted you and you're like, Okay, set it up.
Scott Benner 1:08:30
Let's go. I'm very grateful for this. And I agree with you there aren't I mean, listen, if you have a four year old that just got diabetes, I don't know how fun this is to listen to. But, you know, I think there's some solace that comes from the fact that you were diagnosed, you know, in the 70s, your care is nothing like care is now. But in fact, there are still people who don't, who don't pay attention and or don't have the tools or don't have the knowledge or whatever you want to say, to create, that you still can create this problem for yourself in modern times. You know, and so it's, it's good for people to know what could happen, you know, people who are like, Oh, my blood sugar is just 200 all the time. Well, that's what yours was. Right? You know, and,
Michele 1:09:16
and I was just naive. I'm sure there was more things I could be doing. You know, the more I talked to people or volunteer with JDRF there are people that have been diagnosed as long and knew more than I did at that time, right? Yeah, yeah, I just didn't have the the contact
Scott Benner 1:09:33
information just did not have access to the information. That's why I like to have people on to talk about all kinds of different things. Because I know there are some people are going to be like, don't you know, why are you telling me about complications, but it's so that you understand the big picture, and so that you can then apply it back to your life and think maybe I am missing out on something the way Michelle was missing out on something. Great. Did you enjoy Mike's episode about complications? Which one was that? Very recently it was an after dark about complications. Oh, yeah, yeah. I listen to that one. Yeah, that's the kind of stuff that has to be said once in a while, like you said, because nobody talks about like, I mean, I'm, I'm nearly 600 episodes into this, as I'm recording this right now, no one's ever no one has ever once contacted me and said, I want to tell you what it's like to be on dialysis. You don't think there are people listening to this show who have been on dialysis who are on it now. And no one's ever reached out and said they want to talk about it. And I understand that, but I'm saying there are plenty of people out there that might benefit from hearing from those people as well. Exactly. Yeah. I'm glad you did this. Thank you.
Michele 1:10:42
You're welcome.
Scott Benner 1:10:43
Let me just ask you a couple more questions, and I'll let you get back to your life. So moving your your new lease on life, moving forward, is your it's about staying healthy, staying away from being ill taking your pills, but what other milestones are you looking forward to or having to reach?
Michele 1:11:03
I want to start traveling again. So we're possibly doing something in February, we'll see. I still have to make reservation. So we'll do that. I'm spending more time with my grandkids that's on the top of my list.
Scott Benner 1:11:20
You want to travel somewhere warm?
Michele 1:11:21
I want to retire soon. But it's kind of out of the picture right now. It's I carry the insurance. And I'm too young for Medicare set. Well, I actually I'm on Medicare for three years, but my insurance is primary and Medicare secondary for 30 months. So how did you get on this early because of the end stage renal disease. So as soon as the transplant hit, I'm eligible for Medicare for three years. Gotcha. Okay, that only takes me to age 62. So it's still another three years in between till you can go on or I can get insurance.
Scott Benner 1:11:55
Right, right. I understand. Wow, that's a little scary to me. Yeah. But you'll you'll, it sounds like it. Listen, I gotta be honest with you, Michelle, you kick an ass. So I don't imagine you can't get any of this done. You took the bull by the horns about 16 times in this story. And ended up getting everything you needed. So I'm really impressed with you. Seriously, thank you. Yeah, thank you. Good for you. All right, I'm gonna, I'm gonna say thank you and let you go. I really appreciate this.
Michele 1:12:27
Okay, thank you. I appreciate all that you do. Oh,
Scott Benner 1:12:30
it's my pleasure. It really is. Hold on one second. I'm gonna say goodbye to you like privately. Okay.
A huge thanks to Ian pen from Medtronic diabetes for sponsoring this episode of The Juicebox Podcast, head over to Ian pen today.com. To find out more, you can also find those links in the show notes of your podcast player, the one you're listening in right now probably at juicebox podcast.com. Don't forget if you're a US resident, please go take the T one D exchange. Survey. Take it from me t one D exchange.org. Forward slash juicebox. Thank you very much for thinking about doing that. Alright, so we thank them pen. We thank you. Who do I thank you. I will thank you in a second. We asked you about the T one D exchange. What else should I say to you before I let you go? I don't have anything. Oh, my goodness, my mother, where are my manners? I want to thank Michelle for coming on the show and sharing her story. How crazy is that? That she got that transplant so quickly. Absolutely stunning story. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. Oh, I'm sorry. You know what I Michelle sent me a note later she said when we were talking about other autoimmune stuff in her family. She neglected to talk about her sister who had Ms. She said it progressed very quickly. And she passed from it at age 48. Her sister was six years older than Michelle. She asked me add that and I wanted to wanted to do that for Okay, so again, thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. If you're enjoying the show, please subscribe or follow in a podcast app like Apple podcast, Spotify, Amazon music, wherever you listen in an app. If you're enjoying the show, tell a friend about it. Or an acquaintance or anybody you think might enjoy it. Tell your doctor about it. Tell somebody Thank you. This show grows when you share it with people and that's why I asked you to do that. Alright, that really is that now I'm gonna go I hope you have a good day.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#695 Allergic to Insulin Part III
Morgan has type 1 diabetes and is allergic to insulin.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 695 of the Juicebox Podcast.
Today we're going to be speaking with 17 year old Morgan and her family. Morgan has type one diabetes, and she is allergic to insulin. Please remember, while you're listening today that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your healthcare plan, or becoming bold with insulin. This is a standalone episode, but if you really want the full context, you should also listen to episode 504. Allergic to insulin with Sasha and episode 578. Allergic to insulin part two, with Dr. McCann, Who is today's guest, Morgan's doctor. Hey, if you're at type one who is a US resident or a US resident who is the caregiver of someone with type one, please go to T one D exchange.org. Forward slash juicebox. Join the survey take during the survey. Join the registry, take the survey. support people with type one while you support the Juicebox Podcast T one D exchange.org. Forward slash juicebox. This episode of The Juicebox Podcast is sponsored by the Contour Next One blood glucose meter. Learn more and get started today at contour next one.com forward slash juice box, you can use the meter that my daughter uses. It's small and convenient, and very, very accurate. Contour next one.com. Forward slash Juicebox. Podcast is also sponsored by touched by type one. They're an organization helping people living with type one diabetes. They're touched by type one.org. They would love for you to check them out and find them on Facebook and Instagram. All right, I'm gonna hit record. And then I just need to test everybody. So just Morgan just say hello.
Morgan 2:18
Hello.
Scott Benner 2:19
Perfect. Go ahead doing Kyoto. Hello. Excellent. And then of course, Jennifer. Hello. We are all being recorded. Just lovely. All right. Okay. Let me wrap my head around how we're going to do this. Usually I just tell somebody to introduce themselves. But why don't I do that a little bit. Oh, hold on a second. Before we get going. Whoever's computer's making the sounds is that a PC or a Mac? PC PC? Do you know how to stop it? Because I only know how to stop it on the Mac.
Dwayne 2:56
I was just adjusting the volume, so I won't be doing that again.
Scott Benner 2:59
Okay, all right. Oh, I thought it was like you got an email or something like that. All right. You know what? Let's just do it the way I usually do it. So let me tell you this. You don't need to use your last name. As a matter of fact, unless you really want people to know who you are. Don't. That's up to you guys, though. I don't care. Honestly. Why don't we just sort of go around the horn like Jennifer, go ahead, introduce yourself.
Jennifer 3:26
My name is Jennifer. We are living in Texas. We've lived here for three and a half years before that. We lived in Utah. We have a daughter that's type one diabetic and she's allergic to insulin.
Scott Benner 3:42
Okay. And that's you right, Morgan? Yeah. How old are you?
Morgan 3:48
I'll be 18 on September. Oh,
Scott Benner 3:50
my daughter's gonna be 18 in July. Are you going away to college?
Morgan 3:54
No, I still have senior year. Oh, no
Scott Benner 3:57
kidding. Oh, well, then you're gonna have a good time. And Dad's here, right? Yeah. Go ahead. Introduce yourself.
Dwayne 4:05
Hi, I'm Dwayne. originally born in Texas. I had moved to Utah for several years. Before I met Jen and the kids and we ended up getting married. And when my kids are here, we have, you know, six kids all together. And then we move back here for work and close with my family. Oh, that's
Scott Benner 4:26
amazing. So, Jen, you have how many kids of your own? I have four for Morgan the only type one? Yes. Is there any other auto immune among your children or your side of the family? Celiac? hypothyroidism, anything like that? Nope. Just the type one. Okay. And Morgan, how old were you when you were diagnosed?
Morgan 4:51
I was seven. Oh, okay. Well, this
Scott Benner 4:54
is gonna be interesting, isn't it? I'm gonna give a little backstory now. So I did an episode with Sasha who was right, allergic to insulin. And not long after I put the episode up. I got this email from a doctor who has since been on the show, so you can share her name Morgan, what's her name?
Morgan 5:15
I'm Bonnie McCann,
Scott Benner 5:20
you call her body?
Morgan 5:22
Occasionally. Nice.
Scott Benner 5:25
She's very nice. I had the opportunity to talk to her a number of times. She was on Episode 578, which is called allergic to insulin part two. And Sasha was on 504 allergic to insulin. So I did not know until I heard about Sasha, that this happened to people just absolutely crazy. She came on, she explained what was happening to her. And I just I don't know, I was stunned by it. So Morgan, I want to start with you a little bit. Can you tell me when this began? And how it impacted you? Do you know how old you are when it started?
Morgan 6:00
Yeah, um, probably a year or so after I got diagnosed, it started starting to get painful and getting really large lumps and swelling where shots were done. It was just getting bad for it and got progressively worse.
Scott Benner 6:21
So you would say that almost 10 years ago this began. Yeah. And it was only with your fast acting insulin.
Morgan 6:29
Um, no. It was also my long acting.
Scott Benner 6:32
Really. Okay. So whether it was basil or or your meal and your Bolus insulin, you were getting painful sites. Bumps, was there itching or burning or anything like that?
Morgan 6:45
Definitely burning. Yeah. Okay,
Scott Benner 6:47
so Wow. And there was never a break. You never once gave yourself like an injection. You were like, Oh, it didn't happen. This time. It was consistent. Okay. What's the level? You must be like the toughest girl in Texas, right? Like you? Do you like fall over and bump yourself and be like, it's nothing. I just keep going. How do you go? Yeah, right. I mean, how do you? I guess it happened to you when you were little. Right. So So Jennifer, can you can you tell me a little bit about the first time this started to happen, it must have been a panic. Um,
Jennifer 7:24
well, the thing is, is that was kind of progressive. So at the very beginning, you know, of diagnosis, it was injections, but she was so little, she was getting small amounts of insulin. And a year after we got her on the pump, and started doing the pump, but as she, you know, got older, needed more insulin, it started to have reactions of pump sites being read red, inflamed, painful, itchy. And so, of course, we went to the mode of it must be, you know, the adhesive. So then we are trying barrier wipes and different methods, you know, MSB adhesives, then, you know, she wasn't having issues with other things like the Dexcom, she was having issues with the adhesives and stuff like that. So then we thought, well, it must be the catheter, you know, a plastic, so we went to metal, or vice versa. And either way it it still was having reactions. And we thought, Well, maybe it's the how Gauahar wipes because, you know, it's kind of, you know, abrasive. So, we were cleaning sites with, you know, water and soap before putting a site on just to see with that, and that wasn't working. And I remember talking to a nurse on the phone and asking her, you know, could it be the insulin? And she's like, That can't be. And I said, Okay, well, all of these reactions that she's having, is this normal. And she's like, No, how long? Oh, okay, what else?
Scott Benner 9:42
Thanks for your input. Jen. How long do you think from when it began the just the reading and the soreness to when you said to a nurse, hey, could this be the insulin How long did it take you to get from point A to point B on that?
Jennifer 9:55
It was probably a year and a half. Try different things, and it it, you know, not changing. It wasn't changing. And so I remember them deciding to do a different insulin, just to see if it, you know, would be. So different reactions
Scott Benner 10:20
and we're not throwing anyone under the bus here because Morgan's not just allergic to one insulin and not the others or something like that. So, so what what insulin did you start with? What was the first experience?
Jennifer 10:30
The first, the first insulin that she had was Novolog.
Scott Benner 10:34
Okay, then what you go to?
Jennifer 10:35
Yeah, you know, regular. And then we tried? Sorry. It's like, are these insulin?
Scott Benner 10:50
Sorry? Do you try Humalog? Okay, yes. And then when that didn't work? Did you keep switching? Or did you say to somebody I'm telling you to think and so on.
Jennifer 10:59
So we switched again. And we went to we saw an insulin called the P drug pager hadn't heard it before.
Scott Benner 11:07
It's the one my daughter used this, by the way for years. Yeah, my daughter's been using the future forever. And then then when that didn't work for you, just so being really serious once you get into this situation, and I sort of want to hear about this, from everybody's perspective, you're basically being told the oxygen your breathing is burning your lungs, but you can't stop breathing? I mean, is that incredibly difficult to make peace with?
Jennifer 11:36
It? It was it was difficult. Because, you know, I was, I was willing to try anything, anything, you know. So, pump sites were horrible after three days. So then they switched it every two days. Every one day of you know, having to change her sights and hopes that, you know, she wouldn't have a reaction. Yeah. And after 24 hours, you know, the doctor that she was seeing at the time, he's like, I've never seen a pump site like that before.
Scott Benner 12:10
Okay. And that was like, Well, great. Yeah. It's almost like taking your car to the mechanic. And you know, they don't know how to fix it. And they just start saying, like, well, we're just gonna swap this part and see what happens. And, and so do you get hopeless? Oh, yes. Yeah. Yes. Morgan, can I ask you like, did you ever skip insulin or anything like that to avoid the pain?
Morgan 12:35
Um, I would try to a lot. Yeah.
Scott Benner 12:38
Is this I mean, did you did you go to therapy for this Morgan?
Morgan 12:43
Um, not to have recently have we tried it?
Scott Benner 12:49
Yeah, I mean, it just, I'm, I don't know like, I know you're on the spot here. But can you put it into words what it's like to use something when you know it's going to hurt.
Contour Next One blood glucose meter. It's tiny, it fits well on your hand. It has a bright light when you're using it at night. The screen is easy to use, and the accuracy is out of this world. The Contour Next One blood glucose meter features Second Chance test strips. So if you should head into that blood drop and get some blood but not quite enough, and you go back in again, go get yourself some more blood, it does not hurt in any way the accuracy of the test, you're not going to waste test trips with the Contour Next One, like you may with other blood glucose meters. Contour next one.com forward slash juice box. That's where you go to find out more about it, where to buy the meter. There's little Linky link there for online purchases. Or you can learn about the meter and then go ask your doctor. Buy it right there on the website. There's so many different ways to get an accurate meter for yourself. You don't have to just use the meter someone gave you. I know it's easy to believe that they're all the same, but they're just not the Contour. Next One is super accurate. It's easy to use, easy to carry in your diabetes bag, your purse or your pocket. Check it out. That's all I'm saying to do contour next one.com forward slash juice box. If you want to get really fancy the Contour Next One pairs with an app on your phone so you can keep track of your blood sugar tests and other such information. Don't forget to head over to touched by type one.org right now and check out what they're doing. They've actually got a little thing coming up this summer I'm going to be speaking at so go pick around their website and see if you can't get yourself some tickets. Last little bit here T one D exchange.org. Forward slash Use box, go take that survey, please. And if you're looking for the diabetes Pro Tip series from the Juicebox Podcast, they begin at episode 210. In your podcast player, you can also find all the information you need to listen on the Facebook page for the podcast Juicebox Podcast type one diabetes, we're at juicebox podcast.com. Let's get back to Morgan and her family now.
Can you put it into words what it's like to use something when you know it's going to hurt?
Morgan 15:42
Very difficult, and a lot of trying to convince yourself that it's worth it.
Scott Benner 15:50
What are you convincing? I don't mean to be morbid, but are you convincing yourself that being alive is worth it.
Morgan 15:56
Um, at times, the pain would get very extreme to where I didn't want anything to be touching me. Not even like air going on me. So it was a lot to just be there. But then also, hey, you got to do more because your blood sugar's high or a need to do more, because you want to eat, right?
Scott Benner 16:21
And I'm imagining, tell me if I'm wrong. But when they started saying like, move your pump every 24 hours, all it did was make more sore spots on you, right?
Morgan 16:29
Yeah. Okay. The sore spots also lasted for like days. So you'd move it? And then it would be trying to find another spot in between parts that already hurt, because they hadn't held yet.
Scott Benner 16:43
Did you have the extra burden? Were you trying to hide them from other people? So they couldn't see them as well?
Morgan 16:48
Um, occasionally, yeah, I would, because I didn't want my friends and other people to see how red and ugly it would look. So I tried to focus the shots in the sights, where people would have it covered by their clothing.
Scott Benner 17:14
Yeah. Did you ever try change? I mean, did you ever go to the extreme of changing your diet significantly?
Morgan 17:20
Um, I try to eat a lot the US or avoid snacks? What?
Scott Benner 17:25
Were you able to avoid this turning into an eating disorder?
Morgan 17:30
Um, yeah, for the most part.
Scott Benner 17:33
Good. Okay, that's very cool. It's just, it's already difficult, as you know, you know, I mean, this. It's funny, funny, in an awkward and odd way. But this description of like, every injection is a hill to climb. And you know, something to get over. It's it really is how diabetes is anyway, even without the you don't I mean, even without the pain and the the allergic reaction. So you're adding, I mean, you're just multiplying it, right? It's just, yeah, that's insane. And you were so young for a while. I imagine it got more difficult as you got older and became kind of more self aware. Yeah. 100%. Okay. So when you were younger, you were just doing what you were told. And it hurts. Yeah. Did you ever? Like Jennifer, did she ever tell you? No, she ever just say I'm not doing this?
Jennifer 18:30
Actually, Morgan has been an amazing, you know, diabetic, you know, if you could be one like she, she never complained. Do you know? I mean? Yes, she would tell me, Mom, it hurts. It hurts. I don't want anything to touch it. But yet, she never told me. I don't want to do this anymore. Like, you know, I don't want to have you give me an injection. She was just, you know, okay, this is what we have to do. And I, I've always been one to try and be positive that, you know, I am all for, we're gonna find an answer. We're gonna, you know, we're gonna do this. And then it was also, you know, she, she would ask, you know, why me? And it would be, we're going to have an answer. And we're going to be able to help somebody else. This is, you know, we're going to do this. And so I hope that I was one that never gave up hope for her. You know, if she didn't have it, that I could give it to her.
Scott Benner 19:44
Okay, that's amazing. Can I ask you to be a little more honest? Did you believe it when you were saying it?
Jennifer 19:51
Um, at times, it was difficult. I can't tell you how many times I was crying for her. Um, which, if anybody knows me, I cry over everything I can cry when I'm happy, mad, sad, you know, but it's just one of those things of seeing your child go through something which, you know, you see that with diabetics, you know, I wish I could take this away from my child, but then to see them in constant pain and have no answer. It's, it's very, it's very hard to be positive. But, you know, I've always been determined that I'm going to help her I'm going to find something we're going to do this. So,
Scott Benner 20:43
Morgan, were you aware that this is how your mom felt? Yeah. Did that make you feel bad? Like guilt?
Morgan 20:50
Um, yeah, occasionally. always felt sad or upset with myself, even though I knew I wasn't the one causing her to be hurt.
Scott Benner 21:05
Are you allergic to anything else? Morgan? No, not that we know of even like, you don't get bad hay fever, anything like that at all? I don't think so. No kidding. Wow. Morgan, that's just some I was gonna curse. I'm sorry. We all don't know each other that well, but just some really bad luck. How terrible. Can I ask Dwayne, you have an interesting perspective, because you're not Morgan's natural father, but what's it like to sit back and watch this happen?
Dwayne 21:39
Well, I did work as a pharmacy technician for a long time. So the concept of somebody becoming allergic to something wasn't really new to me. Because everyone's body reacts differently. You know, this person is allergic to penicillin. These people are not, you know, so, you know, I just went into automatic mode and like, Okay, let's try different syringes, different manufacturers, you know, just went through the whole process of what I was trained on when I was a tech, and it's been rough. You know, I, last summer, I went to wake her up, and she's lying on her floor. And you know, that's the first time and she was unresponsive to and so that was really nerve racking. And it's like, I want to help her to make her feel better. And, you know, I keep coming up with ideas. Well, to me, let's try some lidocaine on that spot. We'll see if that helps with with this. You know, try some ibuprofen. Right, so Benadryl, you know, just went through all those steps and just trying to find a way to help ease her discomfort with all this was just, you know, disheartening, because? Nothing. Until recently, have we been able to find that solution?
Scott Benner 23:02
Yeah. Morgan, what were you on? Why are we on the floor? Were you in DK? Um, yeah. Were you not taking your insulin?
Morgan 23:10
Um, no, we had been my blood sugar just got to the point of it not absorbing any of the insulin and getting so high.
Scott Benner 23:19
Oh, from the inflammation at the site, you weren't getting good. Oh, I see. Oh, that's scary.
Dwayne 23:25
That's why she had to move the pump site every day, is because you get that tissue swelling, and just heard your absorption at that spot. So you have to move it to another spot, but then that that slow moving insulin finally hits her system. And so she would go into Ultra lows sometimes after being high, because she gets like a Bolus along with her. The other shot at new site.
Scott Benner 23:50
It's just like a cruel joke. We're gonna I wanted to ask, Oh, God, I had a question for you. I think it might have just fell out of my head. Because that was upsetting. And I'm still recovering from Jen, you almost made me cry about five minutes ago. So I had your voice broke once I'm like, I'm gonna cry. So Oh, my question for you, Morgan is is kind of simple. Maybe you will know the answer. And maybe you won't. But did you? While everybody's working so hard to try to figure this out for you? At what point? I'm guessing you gave up at what point did you just go along passively because they were trying like When did you stop believing anything was ever going to help?
Morgan 24:32
I'm probably after our first time with testing out to see the different area actions to all the different insulins that we had. We had gone to this one allergists and I remember just going to get it tested. And just giving up because the reactions didn't show from how a little mountain diluted They were. And I just remember, quitting I was done
Scott Benner 25:03
just didn't matter. Like, no matter what insulin it was, or how much or how diluted you were having the same reaction at every spot. Yeah. Wow, I'm so sorry. How long ago was that?
Morgan 25:15
Um, two years ago or
Scott Benner 25:19
eight years after this started? Yeah. Well, Morgan, you've got a hell of a college essay. And you, I'll tell you, you're gonna, you're gonna get accepted anywhere you are anywhere you want to go. That's really, it's crazy. So. Okay, so you're seeing a doctor in Dallas, and she hears Sasha on my podcast, and then contacts me and asks me if I can set her up with Sasha. And that all happens. You get a phone call, like an excited phone call from a doctor
Morgan 25:56
or no, like, we go into my appointment, and she's ecstatic. And I have no reason or clue why.
Scott Benner 26:06
Okay, yeah. And she's just like, you're probably like, Listen, lady, this is I hate this place. So why are you? She just told you what, what did she tell you?
Morgan 26:17
Um, that she had listened to your podcast, and gotten in contact with you to get in contact with Sasha. And learned about all this information about what she was going through what they've done and all that stuff.
Scott Benner 26:34
Okay, and were you like,
Morgan 26:38
I was very shocked. Didn't know what to say? Or how to react mainly. Right? I was just surprised to hear that there was someone else having reactions like I was.
Scott Benner 26:50
Yeah. And then did you? Did that make you feel hopeful? Or were you still like, this probably isn't going to work for me.
Morgan 26:57
I was a bit hopeful. Yeah.
Scott Benner 27:00
So So Sasha was doing? Gosh, she was doing that whole, like, getting that insulin from she had like, like a device she had to get from overseas. And it was like a big insurance problem, like this whole thing. Is that what you thought you were going to be doing at that point?
Morgan 27:17
Um, I didn't know what we're going to do. But I knew that there was other opportunities now.
Scott Benner 27:24
Yeah. Okay. I gotcha. So in the end, you're using so I guess, your your Basal insulin, or use your your you still you're still using a Basal insulin? Yes. And, and are you having an allergic reaction to
Morgan 27:40
it? Um, to this one. Now, right now, I'm using what's called receiver. And it's seeming to work pretty well. And I don't seem to react to it.
Scott Benner 27:50
Excellent. And for your meals, what are you doing? I use a Frezza for instance, you are using an inhaled insulin. Okay. Do you like it?
Morgan 28:01
Um, yeah, I mean, it's not painful. Super easy to do. So
Scott Benner 28:06
as soon as I asked if you liked it, Morgan, I was like, that's the worst question I've ever asked on this podcast ever. Obviously, you like it, but I meant, like, was, I guess what I mean, was, was it a big shift from injecting for meals? Like what was the learning curve? Like,
Morgan 28:22
I'm more so learning of when I need to take it, because it reacts a whole lot quicker. But it also gets out of your system a whole lot quicker. Okay. Are you just adjusting to that is?
Scott Benner 28:39
Yeah, well, what about the process of like, how do you I've never had anybody really explained it to me before. I don't think like he just kind of isn't like an inhaler. Like you see people use
Morgan 28:50
Yeah, it's practically just a little inhaler. It comes in set capsules of units. So there's 12 unit, eight unit and four unit. And based on how much you're eating, you'll put in one of the units and then you'll just inhale like you would for asthma,
Scott Benner 29:09
right? Are you experiencing much more stability? I mean, I would imagine you are like a you have more stable blood sugars now? Um, yeah.
Morgan 29:18
For my blood sugars which like always around in like three hundreds and up but from since starting this my blood sugar's normally are a lot lower than that. So
Scott Benner 29:32
can you tell me if you you don't have to share if you don't want to, but like, what was your a one see a year ago and what what is it now?
Morgan 29:40
A year ago, it was like 13. And our latest appointment was like 9.1 or something like that. Wow.
Scott Benner 29:50
You're kind of just learning how to have diabetes, aren't you? Yeah. It just It occurred to me like this whole thing has been it It stopped the process that everybody else goes through of, of, you know, getting over the sadness and learning how to use insulin and you know, that kind of stuff like Pre-Bolus in your meals and all the things that you need to learn to have find stability, and Laurie one sees, and you'd never had you were always in a in a firefight, basically, you never got, you never got to the part where you got to sit down and like think about it.
Morgan 30:24
Not really, yeah, that's amazing.
Scott Benner 30:26
Do you feel better that your agency is lower? 100%? Yeah. Jen, do you see a difference in her personality?
Jennifer 30:35
Yes. You know, first of all, with her agencies, she hated hated going to appointments, because every time we'd go, they'd be like, Okay, we got to work on the same one, see, we got to, you know, do better. And it you know, because of that, they would add more insulin, more insulin. And her ratio used to be where she would get one unit for every three carbs. And, of course, excuse me, her insulin, or her agency just wasn't coming down. She she had, I think, the highest that she had, you know, after diagnosis, her agency was 14. And, you know, it just couldn't have hated that all our work that we were doing was not shown on paper. And all they could see was a onesie 14. You're not doing it here. We
Scott Benner 31:44
no one ever said no one ever said, Hey, there's inflammation here. There's reasons why the insulins not working.
Jennifer 31:50
No, no, no, it wasn't until it wasn't until we, you know, found. Dr. Bonnie McCann Crosby is before that. Nobody, you know, I took dozens of pictures, we'd show them, you know, her injection sites pump site, then it'd be like, Oh, that's bad, okay, but they didn't ever say anything like, oh, this could affect your body, you know, you know, absorbing the insulin. And she'd go, like, at least once a year, she'd be in DKA and had to go to the hospital. And it'd be like, You got to work on your emergency, you got to do more insulin. And it wasn't until we were in the hospital for DKA. And Dr. McCann was the attending physician, and she came in. And of course, I'm like, these are the pictures. This is what's going on. This is you know, and she was one that was okay. Okay. And she had left and Morgan's. Like, I like her. And I was like, Okay, we'll go to her. So we switched over to Dr. McCann. And she was the one that actually looked at these sites. She took pictures she, you know, was genuinely interested in helping us find an answer. And so when we having her a Wednesday be at 9.1 we're ecstatic and I do see a difference in her person every
Dwayne 33:33
time we would go to a doctor or she was in the hospital, you know, they have rotations for rotating shifts and everything we just have any doctor that we were in the room when they came in, say, Oh, by the way, can you look at this, you know, maybe you have a wound care specialist allergist come by take a look at this and try to tell us what's going on here.
Scott Benner 33:50
Yeah, just hoping if you sent it to enough people, someone would recognize it. Right?
Dwayne 33:54
Yeah, someone would come in and go right away. Oh, yeah. It's because of this. It's a little
Scott Benner 33:59
demoralizing that it never happened, isn't it? You know, it's just it's crazy. That Well, I mean, it's rare and all but somebody should have been able to make the leap. You know what I mean?
Dwayne 34:13
And the last time that she was in is when we started for SEMA she tried Lantus lever mirror basil guard and then finally the in the hospital they put her on recibo we're like okay, this one works.
Scott Benner 34:27
So that one so why would imagine just getting on on a Basal insulin that wasn't causing you a problem probably started to bring her a onesie down and and create some stability. You were a CGM Morgan. Yeah, I do. Actually, is that like, before? This was that CGM just basically like depression on a screen for you.
Morgan 34:49
Um, yeah, I wouldn't like looking at it at all. constant reminder that my blood sugar was never worked supposed to be
Scott Benner 34:58
told me if Even though I mean, it's obvious to everybody, and I'm assuming to you as well. And you've said already that this is not your fault, right, but it doesn't stop it from feeling like that, does it?
Morgan 35:11
No, not at all. Okay.
Scott Benner 35:16
You actually, so how long have you been using the is it by the way? I'm sorry? Is it a Frezza? Or is that how they say it? Freeze? Okay, how long have you been using our
Morgan 35:26
Frezza? Um, it will be a year in September
Scott Benner 35:29
year in September. So now you can look at your CGM and start making more thoughtful decisions about using insulin. Yeah, yeah. And a nine. Let me ask you a quick. Do you mind if we talk about management for a second? Do you guys should? Yeah, Jen, you don't actually listen to this podcast, right? No, I do. Okay. All right. So let me ask you a couple of questions about your basil. How much do you take a day?
Morgan 35:55
Um, I take 32 units in the morning and then 56 At night
Scott Benner 36:01
of Joseba. Wow. So you are still pretty? Is that a resistance to the insulin? Have they ever checked you for insulin resistance?
Morgan 36:13
I'm not sure. No,
Scott Benner 36:16
they haven't, they haven't. So 30 to 56. Really. So eight onto I'm I'm mapping over here, which is not my strong suit. Sorry.
Dwayne 36:28
So we just went through around of having her text me whenever she did a Frezza how many units and I would put in the text messages and the time and date. And I built a spreadsheet on that and sent it to document cans office, they looked at her Dexcom stuff from their size, so they can see where she was at, at that time and date and make some adjustments based off of that. Yeah.
Scott Benner 36:55
Hey, overnight. Morgan, do you? Do you sit stable somewhere? Does your blood sugar sit stable? Overnight?
Morgan 37:05
Sometimes
Unknown Speaker 37:07
Do you this morning,
Morgan 37:10
this morning.
Scott Benner 37:12
So the way I talked about using insulin here and basil still Basil is that basil is kind of the most important part, it's the foundation and the building block of your of your management, right. And that away from meals, like you know, so away from meal insulin, which would be a present in your example, and away from active food in your stomach. So once your food is empty, your stomach is empty. If your Basal is doing its job, well, you are stable at the number you mean to be at, which means if you want to be at 100, you should be stable at 100. If you want to be at 90, there's an amount of basil that should hold you stable at 9120, etc. And so it's just very interesting to me. I mean, that's I don't think of insulin as a lot of insulin or a little bit of insulin I think of insulin is you use the amount you need. But performer perspective. I'll just do it. My daughter I think weighs like 135 pounds right now. And she's eight, eight teen, and she gets about a unit of basil through a pump an hour. So she's using about 24 units of basil a day. And it's an hour away from, you know, away from meals and active insulin. Her blood sugar sits pretty stable between 90 and 110. But yours isn't doing that. Is that right? No. So I would listen. I'm not a doctor. I'm actually maybe the farthest thing from one. But I would I would wonder if there isn't. If something's not happening, where you're, you're, you're seeing some resistance to the Joseba Yeah, and I don't know, I don't know what they would do about it, obviously. Because I wouldn't know if it's inflammation from you know, from the other stuff that we've been talking about. Or if you actually have I don't know, like, I mean, I know you're definitely type one. I'm not saying that but I wonder if you have insulin resistance on top of it or what's your diet like for the course of the day?
Morgan 39:13
I don't normally eat breakfast right now, um, lunch? Normally it kind of varies not very much than either and then dinner it's kind of a lot more
Scott Benner 39:30
Yeah, but nothing like you're not eating like like I don't know you're not having potatoes with rice and a cheeseburger like like you know like you're not taking in like like a like a ton of carbs a day. No no okay, but super interesting. Wow, okay. He caught me by surprise when you said when you gave me this receiver number it caught me by surprise. It's not that not bad. You understand what I mean? Like it just Yeah, it was more it was just more than I expect you to say. I think maybe Are you embody in conversations about this?
Morgan 40:07
Yeah. We're constantly going back and forth, or emails changing and tweaking intake for it and stuff.
Scott Benner 40:15
So let me ask you a question. If your blood sugar was sitting at like, let's just say 200. Right? And you haven't eaten in a couple of hours, you're just looking at a higher blood sugar. If you take the A Frieza a Frezza. Oh my God, why can I say it? If, if you do that, and say you drive that 200? Down to 100? Right? You correct that number? Yeah. Does it float back up again? Or does it stay down there?
Morgan 40:40
Um, normally floats back up.
Scott Benner 40:42
Yeah, that's basil. That so that's, that's, that's a weakness in the basil. Yeah, that's interesting. I don't know. I'm sorry. I don't obviously know how you're gonna get that accomplished and worked on but that I think that's your goal. I think if you figure that piece out, I think that nine a one C turns into a six a one say? Yeah, you know, oh, are you excited that that might happen?
Morgan 41:06
Um, yeah. We're always excited when it gets down.
Scott Benner 41:11
This is such a, this is a such a, an amazingly uncommonly happy story at the end. I mean, it took forever for you to get to it. But I mean, you really were in a position where you didn't think this was going to work out. And it just did. Do you ever have sadness that it took, like that, that a freeze have existed before this? And you didn't know?
Morgan 41:34
Occasionally? Yeah, it's hard. Not this gets you down thinking how many years you've dealt with this? And it could have been fixed. You're known?
Scott Benner 41:43
No, I hear you.
Dwayne 41:45
is expensive. It's, you know, FDA approved for 18 years of age and higher. So the manufacturer card because the doctor really prescribing this off label doesn't offer doesn't the savings card doesn't work at the pharmacy for her. So, you know, it's one month supply for her. It's a couple of grand Wow, during the ductable season, so as that's not not going to be for everyone.
Scott Benner 42:11
Right? Yeah. Hey, Morgan, hurry up and get to be 18. Yeah, did you ever try contacting the company directly?
Dwayne 42:22
And tell I know Dr. McCann contacted them talk to I think their medical director and stuff and because she was under 18. She wanted to talk with him about any risks associated with it but haven't talked with. We haven't reached out to them and talk to him about getting any assistance yet.
Scott Benner 42:41
Well, Morgan, I would think you would be a perfect candidate to be a sponsor of of that insulin. For sure. Your your your story is a is. I mean, your story is that that insulin was your only saving grace. Yeah, you know, like that one simple thing. You know, that company almost stopped making it a few years ago. Isn't that crazy? Like they had not imagined? Yeah, wow. Oh, I just thought of that. Give me chills. Okay. All right. So, okay, more than other questions. What do you enjoy doing? What do you think about going to college for that kind of stuff.
Morgan 43:17
Um, I like working with kids. That's what I do. Mainly a lot. I work at a daycare, actually, and work with preschoolers at school for one of my classes. I'm really good at math. And I'm dance to that and probably will go into mathematics for college.
Scott Benner 43:36
Do you think you'll do education? Or do you think you'll go? Possibly? You don't want to be a math teacher? Is that what you're thinking?
Morgan 43:45
It depends on the grade.
Scott Benner 43:49
What how, what age of child do you imagine would be the best to teach math though?
Morgan 43:56
Um, probably third grade. Yeah, cuz that's when they're learning multiplication. And it's still like it's honest.
Scott Benner 44:04
Yeah, it's a good age for kids. So they're kind of I don't know like you don't realize it till you see it but they're like they're they have enough like common sense that not be complete lunatics and they haven't been hit with all those hormones yet, so they're kind of nice. Yeah, right. Jen. Remember when the kids were nice? Well, this is amazing. Is there anything I'm not asking you that I should be like if I miss something about this story?
Morgan 44:31
Oh, not put a No I did. Okay.
Scott Benner 44:35
Jen, how about you? Can I Can I ask a year after this happened now? Is there been a an increase in your in your mental health like has this been a relief? That's hard to put into words? Yeah. Yeah,
Morgan 44:51
definitely. Definitely have a whole lot more motivation to do things. Before you. It was hard. Hard to do things because they felt like there wasn't a point because at some point, you know that your body is just gonna give out. But now with having more energy and my body actually accepting the insulin, I feel like I'm able to do a whole lot more.
Scott Benner 45:16
Yeah, Jim was there ever in your head that this high a one C was going to, like, hurt her and other ways, at some point. Excuse me.
Jennifer 45:28
So, you know, it just frustrating that you kept seeing it going up. And but, you know, she'd go into DKA. And, and every time that she was in DKA, you know, she was responsive, she wasn't feeling good. She went in, you know, but last year was, was the scariest. And, you know, seeing your child lay on the floor unresponsive and having the paramedics come in to get her and having to do a CT scan to make sure that her brain is okay. And going into the hospital room. And she is completely out of it does not know where she's at, and is trying to take off her, you know, her IV 's and stuff because she's wanting to get out of bed. And it just is, you know, a moment that I will never forget. And hopefully we'll never have to go through again,
Scott Benner 46:41
doesn't sound like you're going to have to, and it's good.
Dwayne 46:45
And in the last year, you know, when she started at Frezza. She went into clinic, we have the allergies there in Dr. McCain's office as well. They get a chest X ray just so they have a baseline in case of presence starts having any impact in their lungs. We go to Texas Children's Hospital, which is great as five minutes up the road. She's seen a cardiologist and kidney doctor just get a baseline on some of her systems to make sure that you know, diabetes doesn't start to impact those.
Scott Benner 47:22
Yeah, it's really interesting actually turn the way you answered my question. Because I and I'm not trust me, I'm not being critical. I was trying to lead you into thinking about long term complications about diabetes, but you're so mired down in this fight, I think that you can, you don't have the bandwidth to look deeper than what's happening right in this moment. And and that became really evident when you were answering the question, I thought, wow, like, there's this poor family, their situation is so immediate and constant, you guys, you don't have the luxury of thinking a month away. And, and now you do all of a sudden, is that, that that that must be a pretty nice change, I would imagine
Jennifer 48:06
that it is a nice change. And also like, so I'm in the middle of getting my master's program, or getting my master's in social work. And, you know, just this last semester, I had some amazing things, you know, even happened just recently because I was looking for research, and came across an article about a boy who was allergic to insulin. And I reached out to the author and asked him to, you know, forward the email on to the mom in hopes that she would contact me. And she did. And they they have a Facebook group is called insulin allergy and hypersensitivity awareness. And in there, there is a group of seven moms, all with kids who have allergic reactions to insulin. And it was just another thing of Oh, my goodness, okay. She's not alone. She's not alone.
Scott Benner 49:25
Right? Whether it's, I'm sorry, whether it's seven people or 7000 people, it's such a big deal to know you're not by yourself.
Jennifer 49:33
Right? Yeah. And that's what I kept telling them. I'm like, Oh my gosh, we're not alone. We're not alone. You know, you wouldn't wish it on anybody. But I am so thankful that we have now come into a community that completely understand. And so you know, that is one of my main goals with getting my master's degree is I just want to be able to help Morgan you know, the best way I can. But then to be able to help others who, you know, come into this life of feeling alone.
Dwayne 50:16
Yeah, I The reactions are the same across the board. I mean, Sasha, who was on your other podcast, she said that I believe that the insulin was eating away at the tissue of her skin Morgan gets bruised and redness and pain. Another one Jen was telling me about from this new Facebook group that she found was as like a BS thing where it gets raised and read and painful. So these reactions are carbon copy, right? You need to these fake these patients, these kids yeah,
Scott Benner 50:48
it's insane. Like Jen have those other people tried a Frezza.
Jennifer 50:54
So other ones they have not. I know that one of the patients. She was, you know, whenever she tried a Piedra, she would stop breathing. And so they have not tried a Frezza. You know, so and I think that they're all younger patients. They are now all younger than more than the oldest one turns 18 in March. So Morgan is now the oldest of this group. And so, you know, with FDA, you know, not having a friend approved for under 18. I don't think any of them have tried. I
Scott Benner 51:37
say well, okay. Hey, Morgan, are you do you know, Sasha? zyk? You guys hook up online and meet?
Morgan 51:43
Um, no, not personally.
Scott Benner 51:47
So, listen, as we wrap up here, I just want to tell you more than I know, my name is not great, Scott. It's kind of like it's not a great name. I've lived with it my whole life. But I do feel like if you have a baby ever one day, like I should get some fairly strong consideration for baby names. Do not think big. But I wanted to, I wanted to seriously tell you just kind of like to put some perspective in this for you. You're almost 18. And eight years ago, when you were 10. I started this podcast. But back in 2007, I started writing a blog a year after my daughter was diagnosed. I wrote that blog for years, I eventually started a podcast. And my idea was much like what your mom is talking about with with what she's working on, as I just really wanted to help people. And at some point, it became very obvious that I really understood how to use insulin, and that my daughter's outcomes were very repeatable, and that I could explain it to other people, and then they could have those outcomes. And then the podcast sort of just grew from there. Like, I'm just sitting in an extra room in my house right now. And, and I made a thing. I don't know, in 2007, that turned into a different thing in 2015, that in 2021, led you to find somebody who helped you with your thing, like it's, it's kind of magical and almost hard to believe, you know what I mean? Like, it's, it's crazy. What year were you diagnosed?
Morgan 53:20
Um, 2012 2012
Scott Benner 53:23
Wow. So six years after my daughter was diagnosed, you got diabetes. And I started a blog because I was trying to raise money for the JDRF. And I could I was having no trouble raise. I was having no luck raising money. So I started writing to people, and in like, this kind of email thing. And then I realized that was bothering them. And I found Morgan, this is gonna sound particularly odd to you because you're young. But I found a program that let me put my words on the internet and make a make a blog, which was not a thing back in 2007. Really? And all these years later, you don't have sores on your body anymore. is very cool. I don't know. I'm very excited. I'm I'm proud of you. And if I'm being honest, Morgan, I'm a tiny bit proud of myself right now. And I'm looking for just even if you buy a dog, and you name it, Scott, I think that would be appropriate.
Morgan 54:17
Okay, totally. I got you. Thank you audit. My pets. Yeah, you
Scott Benner 54:21
know what I'm saying? Like nothing big and you take a picture of it, you send it to me go look at Scott. Even if it's ugly, it's fine with me. I don't care. Really. You guys are terrific. I really can't thank you enough for taking the time to do this. Especially coming up on a holiday weekend. But your story is amazing. I do want to just make sure one more time. Like I didn't miss anything, right? No, you feel good about this. Yeah, I feel really great about I'm super excited for you, Morgan. I can't. I mean, as you're talking, as all of you are talking, I am sitting here thinking like this poor girl's life must have been drudgery. Like just wake up have every morning and just drag your ass through another bad day. And now I just, I just feel like you, the last year of your life has probably felt like, like heavenly, you know, you have a lot of perspective for a person your age, it's gonna serve you well as you as you become an adult. Do you ever feel like that around the other kids? Do you ever look at them and think I know more about the world than they do?
Morgan 55:25
Um, occasionally, especially my peers, you can just tell if some of them
Scott Benner 55:30
haven't been through anything, right? Yeah. Do you have that feeling? Like there's nothing you can't do?
Morgan 55:37
I'm sometimes
Scott Benner 55:40
may I say something, we don't know each other. But you should feel like that. You've been through a lot more than most people go through in their entire life. And, and you're on the other side of it now. So you have this, you have this perspective, like you know about before, and you know about now and now's better. So, you know, you don't need my advice, but anything's possible. You can just dream it and do it. And it'll happen. You know what I mean? Yeah, that's so cool. All right. Well, thank you guys so much, Jen. I really appreciate you doing this. You sounded so nervous in the beginning. Are you okay? Now, Jim?
Jennifer 56:16
You know, I was nervous. And, you know, it's the whole thing of Oh, my goodness, we're actually getting our story out there. You know, we haven't been able to have, you know, major platform to do that. It's always just been in the moment, whoever doctor is in front of us. Look at this, please help us. You know, so it. Yeah, nervous, but I'm so grateful that we were able to come
Scott Benner 56:46
on. No, I appreciate it very much. I mean, in my mind, Sasha story, reach Morgan Morgan story could reach somebody else. And at the very least, if it can't find another person who's going through what Morgan was going through, I think it should serve very well to let let the other people listening, reset their level of gratitude. You know what I mean? Because this is, because Morgan, you got way more than your fair share of both. So, you know, everybody else, I think, will listen to your story and feel pretty lucky today. And I'm just super happy for your kid. Like, I am so excited that this worked out for you. Congratulations. Seriously, go learn some math and maths. Good. Morgan. That's a good thing. Yeah.
Morgan 57:30
I'm excited for you taking calculus. So, Dwayne, you
Scott Benner 57:34
sound like a good dude. Man. That's a that's a lot of kids over there.
Dwayne 57:39
Yeah. Scott, if you're if you're curious, we did look up a Frezza on YouTube. And the company does have video on there and how it's used and everything else and what the equivalents are between the inhaled and versus the liquid insulin. So, you know, check that out.
Scott Benner 57:56
Yeah, let other people find it and take a look. That's amazing. All right. All right, everybody, thank you so much.
Well, I'd like to thank Morgan and her mom and her dad for coming on the show today and sharing her story. I'd also like to thank our Frezza for existing and help him Morgan out. You guys want to help her, contact me, and I'll put you in touch with her. And if you guys want to buy some ads, I've got a podcast all about diabetes, you should give me a call. Speaking of ads, thanks so much to touched by type one for sponsoring this episode of The Juicebox Podcast touch by type one.org. And of course the Contour Next One blood glucose meter. Go check it out right now at contour next one.com forward slash juicebox links to the sponsors. And all the sponsors are in the show notes of your podcast player, and at juicebox podcast.com. If you're looking for community around your diabetes, look no farther than the Juicebox Podcast type one diabetes Facebook group. It has people with all kinds of the diabetes in there. Don't worry, not just type one, but lotta type two gestational 25,000 members. All in they're talking about something that you'd be interested in getting involved in, checking on or maybe just lurking around. I mean, just be like, see what people are saying about how they adjust their Basal insulin or Bolus for pizza, that kind of stuff. Juicebox Podcast, type one diabetes on Facebook. It's a terrific group. It's a private group. So you have to answer a couple of questions to get in. But after you do that, I think you're gonna like it there. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!