#267 Ask Scott and Jenny: Chapter Three
Answers to Your Diabetes Questions…
Ask Scott and Jenny, Answers to Your Diabetes Questions
Let’s talk about standard deviation and target range.
Let’s talk about Loop and absorption time to better understand food impact, glycemic index and extended bolus.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Pandora - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
This episode of The Juicebox Podcast is sponsored by in pen from companion medical. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. And to Always consult a physician before making any changes to your healthcare plan, or becoming bold with insulin. MDI users, this one's for you. How would you like to live your life less complicated? You can do that within pen in pen is a reusable injector pen that has its own smartphone app. They talk to each other through the Bluetooth. that Bluetooth is magic, isn't it? You know what the app does? I'm going to tell you a lot of battle over the next few weeks on these Friday shows. But for right now, dose calculator dose reminders reporting actually tells you if the temperature of your insulin has gone out of range. Not only that, it connects to your CGM. Ooh, I got you there tonight, an app on your phone that connects to your continuous glucose monitor that connects to your insulin pen. Now you want to know more about indepen don't you? Check out companion medical.com. Welcome to ask Scott and Jenny. In today's episode, I Scott and Jenny Jenny Smith from the diabetes Pro Tip series in defining diabetes. You know Jenny, Jenny works at Integrated diabetes. She's a CDE, a registered pump trainer CGM trainer dietician, she has type one. Her favorite candy is dark chocolate peanut butter cups. And if Jenny was a professional baseball player, she'd be Hank Aaron.
In today's episode of the show, Jenny and I are going to be taking questions from you the listeners. In this episode, we're going to talk even more about understanding standard deviation and absorption times for loopers. Now that absorption time for lupus thing, don't get confused and think if I'm not looping, this doesn't work for me. It's also going to be able to inform you about how to understand your extended boluses. Trust me, it's all about timing and amount.
mirdif asks one interesting journey after we did standard deviation in a defining diabetes. I get this question a lot now. So obviously we there's something we didn't say there. We caused more questions than then
Jennifer Smith, CDE 2:42
then I think I read this one, what three day
Scott Benner 2:45
target for standard deviation? And if you set your targets tightly for alert purposes, will it look like your standard deviation is greater? Will that not affect the value of murder? We did talk about this in the office? Because I've had the same thought. But I won't. Yeah, I'll let me go over it one more time in case we missed something in that episode.
Jennifer Smith, CDE 3:03
Yeah, so standard deviation really speaks to the variance up down. So even if you had your target set, let's say, in your CGM, you have your target set from 80 to 120, let's say a very tight target, okay. But you have this roller coaster that's happening this up, down, up, down, up, down, up down, you know, from, you know, on the low end, maybe in the 50s. And on the high end, maybe up to like the 120s, you're still you're going to have a higher standard deviation, because the variance even within that target that you're still meeting, you're still having a roller coaster. Now the standard deviation is going to get higher. If you have more variance, let's say even if you're your target is that 80 to 120. And you're going from 50 all the way up to 300. And way back down and way back up to 250 and back down, then the standard deviation is even going to be larger than it was with a roller coaster within a target. The aim for standard deviation. I'm always kind of cautious to say we're aiming for a standard deviation of this solid rock, you know, this one number. The lower the standard deviation, the better. That's that's the easiest way to say I mean, if you're looking at a standard deviation of 70, you've got a heck of a lot of variance you do. Your CGM graph probably looks like a roller coaster at an amusement park, right? That's not what we want to aim for. Even within a tight target. You still don't want all of this happening. You want more gentle rolling hills from you know within less or within a tighter range, right? That's going to bring the standard deviation down. So if you have you know, a target range set from 150 to 180. And you're meeting it and your standard deviation is 21. That's a beautiful standard deviation, but your target is leaving you high. Right? So you're doing a good job of keeping things to a minimum as far as excursions, but you just need to ratchet your target down to keep that same low standard deviation. So I hope that makes sense. I'm going
Scott Benner 5:29
to share what we do because it's by no means the rule but it's a place where I've become comfortable with living life and finding a balance. Right. So Arden's target is set at 70. And 120. I'd love to be between 7120 as much as possible, it's not as much a target as it is. alarms for me, like when do we have 120? So I know what to do, right. I love for Arden standard deviation to be lower than it is. But in honesty, I tried just not to go over 40 Like that's like, and that's not great. Yeah, but it's, it's I shoot for more like 35 I try not to go over 40 If you look at Arden's graphs, they're interesting in that 18 hours of the day, her blood sugar is like 80. You know, most of the time, there's two meals that are varying cause a variance Right. And, and she'll jump up usually, it's like 181 60, conventional pumping, I was able to get down a little more quickly. But we're doing now not as fast. But conventional pumping, I didn't have 18 hours of ad that was solid. So in my mind, it's a bit of a trade off, and I'm learning how to do the meals better. I think that you should think about standard deviation more in the context that Jenny put it in. You don't want it to be 70. Not good. Right. But if you're shooting for 20%, or something like that, probably not that realistic. So I've heard under 40. I don't know where I've heard that from is that a reasonable like Mendoza line for
Jennifer Smith, CDE 7:13
under 40? Absolutely. I mean, if you're really it, I usually with the with the people that we work with trying to aim for, you know, the 30s or without consistently running just way too low with little deviation, the 20s can be great, as long as like Arden is kind of hovering at that at with little deviation. Great. That would be awesome. You might be in the 20s. But you know, 30s is kind of where we aim. Overall, with a little bit lower or whatnot. Depending on what situation in life you might be at two, with the women that I work with through pregnancy, we aim lower, tighter overall everything.
Scott Benner 7:55
Let me give you an example because I'm looking at a live grant for art and for 24 hours, right? So in the last in the last one day Ardens a one C has been 5.8 with an average blood sugar of 119 that put our standard deviation at 42. Now if you go out over 90 days, Arden's averaged a one C is 5.6. Over 90 days, her average blood sugar's still 115. But her deviation will probably go up. It does. So it goes it says 45 Over the last 90 days now we are still learning some things and so we have some more prolonged blood sugar's but for instance, in the last seven days, her standard deviations 38. Right. So as I get better at it, you know, over the last 90 days, because you know of this loop thing, you know, you see it come down, I will get the deviation consistently under 40. I think it's going to be more consistently like 35 Once I figured out the meals, but then, you know, I think Jenny's Right. Like once you have the tools in place and things are working. I see standard deviation not as a target. I see it more as See, I don't want to call it a report card, because I don't mean it like that. But I think of that more something you look at later to say, oh, things are getting better, not something right day to day. It's like a comparison
Jennifer Smith, CDE 9:19
almost to say this is where I was this is where I am now. Oh, it looks like it has improved.
Scott Benner 9:26
I would look at if you're looking day to day, I just look at average blood sugar, and I try to keep it lower. And then I look at at deviations like high high deviations. Obviously I don't want a low blood sugar. So I don't have a lot of problems with lows. But I don't want to see big spikes that lasts too long or big spikes. Right. So Meredith, I hope that answers some question and then I'm about to tell you something about in pen. And I think I should first warn you it's possible the information could blow your mind. So I don't know what you want to do put a hat on or hold your hands in the side of your head or something like that, but When you Bolus within Penn say you're having some food, right? And you look at your plate and you're going 10 times, you decide that's 35 carbs, you go into the in pen app, tell it 35 carbs, and it tells you how much insulin to inject, right? Hold yourself tight now because the here's the rest of it. Now pen users, no, you have to prime your pen a little bit. So you prime the Impend, and then dial up the insulin that the app tells you, let's say it tells you a 3.5 units, you inject those 3.5 units, the in pen actually can see the difference between the prime and the 3.5. And it doesn't. So you know, I'm saying like, when it's calculating how much insulin you have, it's not saying like 3.5 plus the priming amount of insulin it know, how does it know? The fascinating, right, like just boom, I don't understand. I mean, for a pen user, or somebody who's doing injections, this is an incredible leap. Your insulin on board is being kept by an app on your phone. And it can see the difference between the priming of your pen and the Bolus. Get out of here. You obviously need to know more companion medical.com. There's links in your show notes at Juicebox Podcast comm. And one more thing, starting I think next week, maybe the week after these ads are actually going to be a conversation within pen user and world champion, paddle boarder, Fiona wild. Fiona is going to tell us what she loves about it. And it's enough of me telling you what I can, you know, read in a PR kit. Let's hear from a real user. I'm wondering about carb types, oh, entering into a loop. I get confused about what to put when I'm eating a combo meal. For example, what if I'm having pizza and fruit or a burger and veggies or, you know, like yogurt fast carbs plus protein? She said I thought maybe since Jimmy was a dietitian too. This might be something she can help decipher how to Bolus for different combinations. So what Matty's bigger question is and how this will work out for the rest of you is she's really asking about absorption time, I think in loop right, to
Jennifer Smith, CDE 12:15
an glycemic index to a conventional pump system. Yeah, in game
Scott Benner 12:19
conventional pump system, it's going to be glycemic index. And the idea of extending boluses or temporary or something like that. So it's, it's crap, slightly different tools, same reason. But to give people context, you don't listen, who don't use the looping system, you will tell the loop Hey, I'm eating 35 carbs now. And then you have to tell it how long you expect it to be in your system, how long you expect it to take to absorb is that one hour, 30 minutes, two hours, three hours, like that kind of thing. If you get that absorption time wrong, when you put the setting when you put the carbs in the loop, it really big causes a lot of high blood sugars when you get it wrong the wrong way. So do you have any thoughts on this? Because I'd actually love to hear them. I'm gonna sit back and listen like a listener for a second.
Jennifer Smith, CDE 13:03
It's a very good question. I think that the icons that are within the fast moderate and slow groupings, if you are a looper and using them are defined by like a glycemic index nature, right there fast ones are going to get absorbed pretty quickly loop says they're two hour moderate or like a three hour really slow, which would be like high fat, really high protein kind of meal would be a slow absorption, right? icons like a lollipop, a taco or pizza. Okay. Now, most mixed meal, she brings up a good question. Most mixed meals that are a content of carbohydrates, and protein and fat and healthy fiber. Good example being something like grilled chicken, steamed veggies, and maybe like quinoa or brown rice or something like that, right? That's a good mixed meal, a three hour absorption would be a good place to start. It's mixed. You've got a little bit of everything. Now, on the flip side of that, let's say you have like a thumb size of grilled chicken, one broccoli spear and a plate full of brown rice. Hmm. Question time there is based on the content, right the content but the portion that's the glycemic load. It's not only glycemic index, but it's the amount if you've got a plate full of high index carb that you're eating, very minimal little other things that's no longer a combination meal. That's more like a two hour that's like it's fast now rice is as an example in this can be a can be a bad example because some people's experience with rice can be longer impacting same thing with pasta. Some people get really quick impact from pasta some people get really like long drawn out. And I mean if I went into it further, some of It has to do with cooking method and again what you eat with it and whatever. But in a simple answer, most combination meals that are not heavy simple carb should be about a three hour absorption for our absorption would definitely be those Merle meals like she's saying, let's say I'm eating a big old cheeseburger and french fries but I'm also having an apple on the side, that's still a fairly long digesting meal. A trick or a tip that might work it let's say you're eating the apple First eat the apple, put it in as a 15 gram you know kar Bolus absorption two hours. And then when you go ahead and Bolus for the rest of the combo meal, or go ahead and rest as the rest as a four hour absorption. That way, you're kind of addressing both types of food and the way that they may be being digested because of how you've kind of eaten them. Whereas the apple at the end of the meal sitting on top of the burger and the French fries and whatnot. Group it in and to for our absorption.
Scott Benner 16:10
I was gonna I was gonna say to rice so at home. I only use a basmati rice. It's okay, and that does not impact Arden nearly like if we were to go to a Chinese restaurant, she was just going to grab like white rice, right? It's just it's easier. You know, bread with no high fructose corn syrup. Great way to cut yourself a break. And pasta, I use dreamfields It does not hit Arden nearly like other pasta does. Both in intensity and time. So there are sort of ways to like cheat around it with certain foods and what you said about about cooking methods I just made I just made another another note for myself about something we could talk about in the future. Because that's really interesting.
Ask Scott and Jenny was brought to you today buy in pen from companion medical, please go to companion medical comm or click on the links in your show notes of your podcast player, or the ones you can find at juicebox podcast.com. For more information. Just think about what it would mean if your insulin pen could keep track of your insulin on board and so many other things. Just like a pump. The impact is fantastic. It's like that little train that just keeps going get any mean climb and Chugga chugga chugga that thing you don't I mean, it's like no stopping us. Now that's not the train. But if the train could sing, you know if the little engine that could could sing I imagine it would sing ain't no stopping us now. What would that even sound like? I'll leave you with that thought. As it fills your head all day long and torments you. You know what? That's not fair. You need to get that out of your head. Do this instead, think about this companion medical.com with links in your show notes for juicebox podcast.com
About Jenny Smith
Jennifer holds a Bachelor’s Degree in Human Nutrition and Biology from the University of Wisconsin. She is a Registered (and Licensed) Dietitian, Certified Diabetes Educator, and Certified Trainer on most makes/models of insulin pumps and continuous glucose monitoring systems. You can reach Jenny at jennifer@integrateddiabetes.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
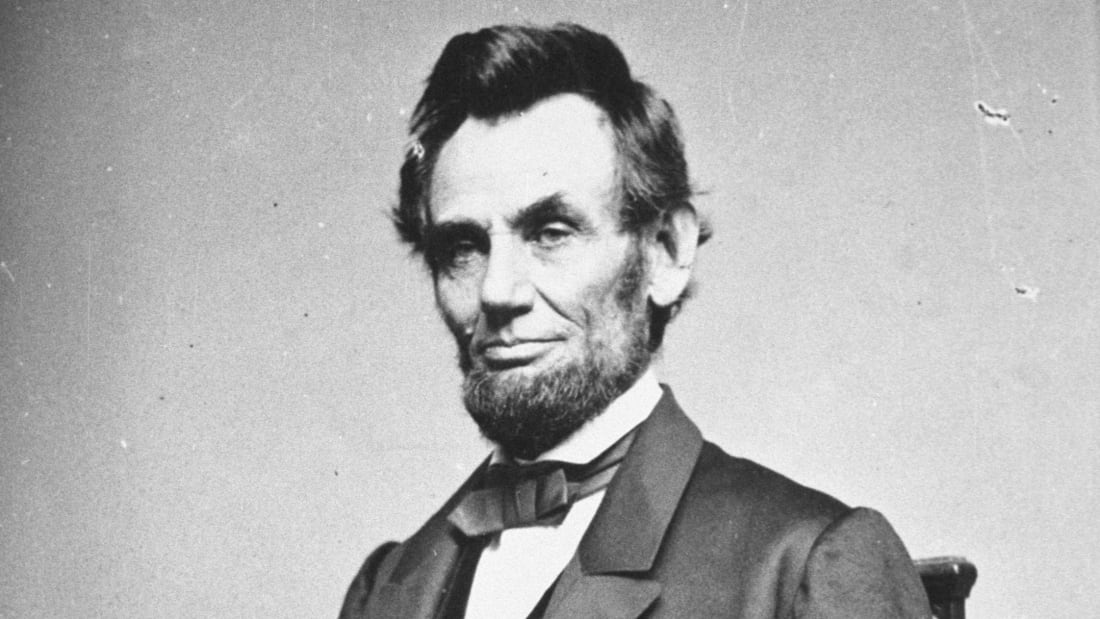
#266 Whatever You Are, Be a Good One
That’s an Abraham Lincoln quote…
Lincoln has type 1 diabetes, heart issues and a good mom.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Pandora - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Welcome, everyone. This is Episode 266 of the Juicebox Podcast. Today's show is sponsored by Omni pod Dexcom and dancing for diabetes. You can find out more about the Dexcom g six continuous glucose monitor@dexcom.com forward slash juice box. You can see what's going on at dancing for diabetes dancing the number for diabetes.com. And to get your free no obligation pod experience kit from Omni pod. That was the link Miami pod comm forward slash juicebox. There's also links in your show notes at Juicebox podcast.com. Once in a while somebody has to go over and above to be on the podcast. They use their phone in an airport waiting for a flight. A person has sat in their car in the summertime with the air conditioner off so the sound would be good. Talk to Tommy on his way home from the endocrinologist. But Stephanie, Stephanie really went over and above because Stephanie recorded almost the entire show, before I had a mechanical failure with a computer, and then she started over again, even though her life had gotten crazy. So this one's gonna be a little interesting for you because there's gonna be background noise sometimes once in a while you're going to hear Stephanie driving, you're going to hear children playing in a playground behind her but a law makes sense. And I believe that the situation that Stephanie is in while she's recording goes to her story. All right, I'm going to give you this rich tapestry of emotions and sound and feeling information. Right after I say nothing you here on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your medical plan. We're becoming bold with insulin.
Okay, um Arden's asking me about lunch. I'm sorry.
Unknown Speaker 1:51
She's like,
Scott Benner 1:53
she says, I'm not that hungry. So I'm like, What do you mean by not that hungry?
Stephanie 1:59
I think it's gonna be like the story of our episode.
Scott Benner 2:03
This one's gonna be it's gonna be interesting. So while I'm doing Arden's lunch, let me put everybody's mind in the right place for this episode. I have recorded I think about 280 episodes. You haven't obviously heard them all of this podcast. I've had no mechanical computer failures during the recording, ever. And Stephanie and I were probably about 15 minutes from being finished recording her episode when everything froze up and crashed and did not flash save the way it was supposed to in the way it's set up to. So we're gonna start over again now. But now as we're starting over, we're up on the time where I'm like, Oh, I know. I've set this one will be perfect. I'll finish right doesn't have to do Arden's lunch, and everything. So now everything's a little hodgepodge. In the time, Stephanie has left her son Lincoln, his preschool, where she hangs out outside to help manage him while he's there. And driven home to give the dog groomer, the German Shepherd. She is now headed back to the preschool. Are you back yet?
Unknown Speaker 3:05
Elma,
Scott Benner 3:06
almost 70s goes back to preschool. And then I'm going to finish up Arden's lunch here. And then we're going to start speaking again and we just need to get that out of the way because I didn't want you to feel weird. Like you had to talk like you hadn't said something before. So start over, everybody in on the on on what's going on, and we'll be able to work that way. So, while Stephanie's driving, I'm going to figure out what are the means by it's lunchtime, but I'm not that hungry.
Stephanie 3:32
Not for by
Scott Benner 3:34
And trust me, the answer I'm going to get back here is going to be unpleasant. I said, What do you mean by not that hungry? What will you eat? Maybe? And she said a little, which is a designation of an amount of food. And that doesn't help like snack on I'm not having the sandwich. Okay, well, you know what? I can I can work with that. Let's Temp Basal in grace. Let's go 50% 50 No, I'll tell you why. 95% for an hour, and Bolus right now I'm taking this sandwich out of the bag. Let me think of what's in there. Not many grapes but some blato cookie 12344 units or a couple of little chips five six, not the sandwich banana 7890 I'm gonna say I'm gonna do 11 units 70% now, the rest over Turn on any red Tell me when she's done eating. Tell me when you're done eating.
Unknown Speaker 5:06
What are you just gonna polish your half of what you would
Scott Benner 5:10
know. So there's more going on than you know. So Arden left this morning. I said, Boy, this day really is messed up is Arden left this morning I said, Hey, you only have 25 units of insulin left in your pump. So it'll get you to lunchtime, which is right now. And what I said was we'll be able to Pre-Bolus with your old pump, I'll be done recording the podcast and I'll come over we'll swap the pump out. And and you know, we'll, we'll keep going. Instead of that happening. Please take a moment to visit dancing for diabetes.com dancing the number four diabetes.com You can also find them on Facebook and Instagram.
Unknown Speaker 5:50
Instead of that happening.
Unknown Speaker 5:53
Luckily, I guess
Scott Benner 5:55
artists to school and decides that it's muffin day chocolate chip muffin day.
Unknown Speaker 5:59
Uh huh.
Scott Benner 6:00
So those muffins are like crazy that they have the school. So I had to do a really big bolus just for the muffin probably like 12 units in total. So we did that was two hours ago already. And so we went over and change the pump A while ago. So we don't need the we don't need a new pump. Now she has a new pump
Unknown Speaker 6:21
on the break.
Scott Benner 6:22
But she's a little I can't tell if I'm having trouble getting the pump site going. Or if it's the muffin. So she's like 150 and kind of stuck at 150 right now. So in a second I'm going to find out because the muffins pretty much gone at this point we're gonna find out if this Bolus doesn't get her going in the right direction, then it's a different issue, but we'll run it Yeah. And I don't think it's that way. I liked where we put that pump. It's and it's doing well. We've been using it and having luck. I just think that it was a new pump on top of an incredibly Carbo rific. muffin was probably that was bad timing. I'm honestly thinking keeping it at 150 is a is a hell of an accomplishment, actually.
Stephanie 7:03
Right? Yeah. Lincoln steady at 116 right now. So let's see if that juice bot that juice box catches up 10 minutes.
Scott Benner 7:11
Do you think he's gonna go back up?
Stephanie 7:13
Oh, yeah. Because he he went he bought, like starts falling he falls fast and hard. And so, um, there's many times where we've corrected and we've gotten really dangerously low, like in the 30s. And then it's just like, a struggle to get him to stay at 80 because I think it's really hard on your body to like recuperate when you're
Scott Benner 7:36
bouncing. It's tough for sure.
Stephanie 7:38
It's tough, hard, but you know, with him being so little to get his body to like balance back out. And and he doesn't talk so ask him how you feel doesn't really get anywhere. get us anywhere? No, yeah, for some reason Lincoln has chosen not to talk.
Scott Benner 7:54
Oh, so let's let's we're gonna reorient everything ready. Sorry. Everyone, this is Stephanie. Stephanie. Hello. Stephanie has four kids. her youngest, Lincoln has type one diabetes for about a year and a half ish. He has other medical things going on too that we're going to talk about for a second. Right now he's in preschool. And he had a bit of a bit of a falling blood sugar was falling really fast. And you gave him one or two juices for that falling butcher,
Stephanie 8:26
I he was on the playground actually. So I just like popped my head over the wall until the teacher he needed a juice. And she gave him a juice when he was 153 double arrows down because I mainly follow the arrows. And he was 109 double arrows down so I said I think you need to give them another one because I don't know if he was running around a lot on the playground that was like with the bazel that probably kicked in at the same time causing him to
Scott Benner 8:53
no job now he's 160 and stable but you're expecting to go back up and you're scared to put in again So know that at the moment.
Stephanie 9:00
Yeah, like I won't give them any influence right now. But if the arrow angles up, I will I just kind of I feel like a stalker at the school sometimes so they just hang out in the parking lot.
Scott Benner 9:12
Now here's my assumption, right? You're trying to give Lincoln some like normal thing he's gonna go to preschool and have a little bit of socialization and play and have fun and do the things you would have done with him had diabetes not come up? Correct. But you don't have enough comfort with they obviously they're a preschool they're not you know, they don't know.
Stephanie 9:32
In Arizona, the public schools offer preschool
Scott Benner 9:36
Okay, so it so it but you just don't feel comfortable with their knowledge about diabetes.
Stephanie 9:41
So he Yeah, so he's in a developmental preschool because he doesn't talk and so he there's a lot of AIDS and you know, great teachers and staff there, but because it is a public K through fifth preschool or school, they have a nurse on staff, but the nurse and I did not have A good start to him coming on the school campus. And so our last conversation was not nice. And I basically told her that she needed to stop talking to me and that she never had permission to touch my son or ever give him insulin. And even if he's an emergency situation, you are not allowed to touch him and just call 911.
Scott Benner 10:24
What what I'm so interested
Stephanie 10:26
with the ending of our, our last conversation, and since then she's quit.
Scott Benner 10:32
Did you Okay, assuming it wasn't you that made her quit, but she was probably having other problems as well. What led to her? What led to you guys having that conversation?
Stephanie 10:42
Until when Lincoln Lincoln started school in November, because when they turn three, the day after they turned three, and they can start school. I planned on staying at the school Never did I ever intend on like just leaving and be like, I'll be back in three hours by. Um, so I just like lightly touched up with the nurse like how I treat him, which is kind of like I, I just kind of treat as needed. Because he's so little, he doesn't talk and you know, the amount of food that he eats is, is, you know, like what a bird eats all the time. He was he was 89 and steady when I dropped him off the first day, but I was like, and they were about ready to go on the playground. So I was like, I'm going to give them some applesauce before he goes on because 89 unsteady on a 301 playground is a little low for me. And I don't know how he was going to respond to being at school, right? So I was watching it with the applesauce. And I figured maybe he brushed it like 150. And it went to like 190 200. And then like, before I even knew it. He was like 400 like high until the oh my gosh, this was so fast. But I think it was an adrenaline that like kicked in new new thing, big playground, lots of kids who's running around screaming. And that was like my very first experience with him being in a school with the gentleman and I didn't know. And so I told her that I'm gonna go give them a half correction. So I just gave him one unit as like because they This is a false rise. Like he's going to come back down. And she, so she was like, freaked out that he went that high. And I think well, you wouldn't have known this. If he didn't have his CGM on. It's just the technology we know. So now we can fix because I'm pretty sure any other type one diabetic, you know, they either rise or fall with adrenaline, you just don't see it. And so that was the day. Basically it kind of like I took them home. And as soon as we got home, he was 130 unsteady. Like it was just an hour that it took for him to level back out because it wasn't food. It was the adrenaline. And I wake up at six o'clock in the morning with this voicemail, and it was nurse Cathy, that I wasn't allowed to bring Lincoln back to school, that she's uncomfortable with him being in school with those blood sugars, and she feels that I don't give him adequate care. Oh,
Unknown Speaker 13:09
uh huh.
Unknown Speaker 13:10
Because though we,
Stephanie 13:13
because he jumped up,
Scott Benner 13:14
but you're saying that the applesauce was so like, so he's at 89 you put the applesauce in the applesauce has no time, even though it's like, like sugar water. It the jump was so immediate that you thought this couldn't be from that even know. Right. Right. Okay. And so you got to see something else you try it you addressed it sounds like you did well with it and came back to a nice number. So yeah, so she saw something she didn't understand and decided that it was your fault that she did that she didn't understand it. I got Yeah,
Stephanie 13:46
which I never gave her permission to. Like, I was like, I'm not gonna let just hand this all this stuff over to you and expect you to understand. Like, I'm gonna stay here, I'm gonna, you know, treat him and make sure things are fine. Like, I'm not gonna set my son up for failure, the first day of preschool.
Scott Benner 14:03
And I'm sorry, was it your intention? This hasn't been long, right? Like, how long ago was this?
Stephanie 14:09
This started like November.
Scott Benner 14:11
Okay, so a few months ago. So what was your intention back then? To find? I don't know, like some sort of like a, like a nice balance with this, this nurse and to eventually for you to not be the person who's sitting in their car, or were you always thinking I'm just gonna stay here and take care of this. What was your plan there?
Stephanie 14:29
Well, my intention was like after, you know, giving them brief, like education classes on how to handle it. I would just stay close, like, I live like seven minutes from the school and there's grocery stores and stuff. So I would stay really close if needed. Because he only goes to school for two and a half hours, three hours, like not a lot was going to happen. But if I would call and say I think he needs a bolus, give him X amount of insulin, I would just expect them to do it. But it just didn't work out that way. And so that morning, I actually went to the district office and sat there. And I was like, I'm not leaving until someone talks to me like, This isn't how this works. Like, she can't tell me I can't bring my kid to school. Like he gets adequate care. Like he has a good a one. See, he's three. And this was his first day I was I didn't know how he was going to respond. Like, it's going to be trial and error for a few months, because I don't know how it's gonna work. And so basically, they said, you know, they're going to talk to the nurse, and they're going to work it out with, you know, the districts because they've never had a parent that didn't want to follow doctor's orders. Is what they told me. And because I don't want them to follow the doctor's medical plan.
Scott Benner 15:50
And so what happened, because I think this happens to a lot of people, the doctor gives you a pretty basic like 15 carbs, 15 minutes correction, like those, like, you know, kind of just, you know, basic ideas. And you went into look, we have a way we do this, and I, you know, I'd like to make it happen here. And wow, that wow,
Stephanie 16:08
the I'm sorry, the medical plan is like when you go to any doctor, you only correct every three hours, right? You don't stack insulin. And if he's low, you know, you give him you know, 15 carbs, you wait 15 minutes, which we all know is either too much or like it takes longer than the 15 minutes to respond to the 15 carbs, depending on what it is. So they had another executive meeting and it was me the nurse and two directors in this meeting. And during this break that I didn't take Lincoln the school, the nurse called his endo, and had like a very detailed conversation with the team at the hospital and I was really offended and I felt very violated by that. Because I was like, the doctor doesn't care for my son. This endocrinologist has never given my son a shot of influence. He has no idea how my son responds to insulin on a day to day basis. The endo doesn't tell me how much to give my son I make that choice, not the endo. How dare you guys have a conversation with the doctor without me on the phone? He doesn't know anything. But I think they take that as me being like, like disrespectful or argumentative towards the doctor's care. Yeah, because I didn't, I was like, that's not what we're doing. You're not going to give my son and son and that was never like your net. And she wanted a vial of insulin on at Campus. It's like, no, he has a parent. I'm not not giving you a vial of insulin.
Scott Benner 17:46
You know, it's funny. Six months ago or so, our dad started getting treatment for like a shoulder like a chronic shoulder injury. And, you know, there was some getting set up with a note for Jim, like, she goes in the gym, she just doesn't kind of use her right arm while she's in gym. She said to me the other day, she's like, you know, playing one handed. I'm an incredible wiffle ball player, I was like, congratulations. But But in the beginning, I guess the nurse didn't understand the orders completely at school.
Unknown Speaker 18:16
Oh,
Scott Benner 18:18
and I get this like, like phone call from her. And she's like, Hi. I didn't quite understand the orders from the doctor. And I was like, oh, what don't you interested? Because Oh, it's okay. I know people at that practice. So I called over there and got it all straight. I was like, You can't do that.
Unknown Speaker 18:32
I was like, never legally allowed don't like never
Scott Benner 18:35
do that. Again. She's just trying to kind of honestly care what you were trying to do. And you might this bit may have been the most well intended thing in the world. I'm like, you don't call my kids doctors and talk about them. Like, that's not okay.
Stephanie 18:48
And I don't know why people would think it would be, you know, I know mad. And I called the American Diabetes Association, because I wanted to understand the legal rights, like of the school and of my son and as his care like his parents. And they said, because once I dropped my school off on a public property, or like a government property, the care provider, which is the nurse is allowed to call another care provider, which would be the endo to have a conversation about my son's diabetes, it's legally allowed. I was so upset. by it.
Scott Benner 19:25
I don't know if that's, you know, that's fine. Like if that's if that's allowed, legally, it's fine. I still told the nurses like don't ever do that again. Like if I know something asked me. And if I don't have the answer, I will find out for you. But you're not getting involved in this and he knows why that's such an odd leap to make I because you know, I too Is it infers, it infers that you don't understand. So she needs to go around you to the person who really understands. And I think we all know and diabetes specifically, you're very much more likely to understand And then somebody else, you know, you know
Stephanie 20:02
that Yeah. And that's what I told her. And so this last, you know, this meeting, she told me that basically, I had only been doing this for a year. And then I really probably didn't understand it. And you know, she had been doing it longer, and which she was a cardiac nurse. So it's totally different than a endocrinology appealed. And I basically was not very nice. And I was like, I think you just need to stop talking. I'm going to stop you right there. And don't ever touch my son, ever. He's never, you're never allowed to give him insulin. You're never allowed to do a finger poke on him. I will, I will stay close to the school, I will monitor his needs. And if there's ever an emergency, don't touch him and call 911. And that was the end of our conversation. Really? Yeah, no, it was done. Third day of school, never again. And I was really heartbroken. Like, I didn't take them back to school for two weeks. It just like ripped off so many scabs. And it really like sent me in like, not, not a depression, but I was just so offended by the whole process. Like her calling has ended her saying I didn't know what I was doing. Like her questioning the care that I gave my child like it like, like, do you know how many sleepless nights I spend watching this Dexcom? Because I don't I didn't know what it was doing. And I was trying to figure it out and learn and oh, it it really like, put a dagger in my heart for a minute.
Scott Benner 21:31
And by the way, a year with a three, a two year old with diabetes is worth 10 years of being a cardiac nurse and understanding diabetes. I mean, because we all know how well doctors and nurses handle blood sugar's when you're in the hospital to begin with, is that that's probably her idea coming from a hospital setting, which is, like you said, and I yeah, every every three hours will check and you know, as long as he passes out, we're good. And that's you know, yeah.
Stephanie 21:58
And I told her I was like, I lived in the cardiac Grubbs for a year because Lincoln had open heart surgery when he was eight months old. And I told her like cardiac is nowhere near comparable to endocrinology, like diabetes and Lincoln's open heart surgery are in two different worlds like, and and I'm blessed that Lincoln's open heart surgery was was a very good success. And it went well. And he recovered and hopefully Fingers crossed, he won't need another one. But I would do another open heart surgery before doing diabetes any day hands down.
Scott Benner 22:34
It's quite it's because yeah, that's, that's a telling statement. It really is.
Stephanie 22:40
I mean, diabetes is literally a minute by minute or deal. You know, cardiac, at least what Lincoln experienced, you know, we dealt with the lasix and the cardio angio like we didn't he didn't have cardio angio but echocardiograms all all the time and the constant monitoring of his blood pressure and all that stuff. I'd rather do that then the diabetes any day. Yeah.
Scott Benner 23:03
Well, it's a lot. It's a lot of work. And at least there's consistency with some of that other stuff, right? That always open to interpretation, or I wonder how it's gonna go this time. And I do have to say, especially with a smaller kid, the fluctuations are just, they're never ending sometimes. And and they really do test your they test your Will you know what I mean? Like, you're like, Oh, I figured this out. And then it changes, you know, Google. Yeah, right. Thanks. Yeah.
Stephanie 23:30
I mean, then the nights where he's like, steady, and he's like, 130, the whole night. I'm like, it was a miracle. And the next night, it's like, alarms are going off every other direction. And I can't figure it out. And I am afraid to give him too much of a correction. And then as it
Scott Benner 23:44
gets bigger, by the way, like that'll, you know, he puts on body weight and everything like that all gets so much easier. What are your expectations for his speech? Is it something that's new things coming? Or is there like, Is it a physical issue? Or if he's just not ready to talk yet? Or do you not know?
Stephanie 24:01
I really don't know. Like, some my five year old husband is autistic. But he's like high functioning. He can talk and communicate any socializes and he just has more like this and three sensitivity issues. But he was delayed speech as well. So of course, they're constantly checking to see if he has autism, or that's a question that's in the air right now. But I really believe that Lincoln doesn't because his cognitive thinking is there. But I don't know. He just, it's something that he can control. Like, he can't control a lot of things right now, like how he feels or the, you know, the site changes and the finger pokes. Or if, if he's just like, No, I'm not talking.
Scott Benner 24:49
It's an I mean, how, in your estimation, what's the timeframe for you to start getting a feeling for what that is? Or do you know we didn't know
Stephanie 24:58
well with autism? I mean, I knew at a year and a half that something was different. husband didn't talk, but it was more vocal like he made sounds for the things that he wanted. Like he wouldn't say soup, but he would slurp like, I need soup. And like he had sensory issues. So like he didn't want to put shoes on and didn't wear clothes. And like it was more of that combative stuff, where Lincoln doesn't care. And Lincoln can put puzzles together. Lincoln can sit and watch a movie Lincoln can, like do memory and match games. He just doesn't talk.
Scott Benner 25:34
Yeah. So if he was speaking even a little right now, you don't think these questions would be up in the air?
Stephanie 25:40
Yeah, I don't I don't think that they would ask me as often as they do. They think that there's, you know, a sign for autism. If he was saying more words, but he just and he may, he says five words. Ouch. Ouch. It's one of them. When he gets like a site change. Every Blue Moon he'll say No, mom. He doesn't really say dad, he said Spider Man three times. And that was it. And that's pretty much it. Like he just does not talk at all,
Scott Benner 26:08
which spider man got him to say Spider Man was doing the spider verse.
Stephanie 26:13
He was spider man for Halloween. And he said it three times. And then that was it. He never said it again.
Scott Benner 26:18
Well, that yes, we did that. I have to ask was that a moment? Like, oh, he's gonna start talking. And then he just stopped?
Stephanie 26:24
Yeah, I mean, I was so excited. jumping up and down. I'm like, we're gonna, we're gonna move on from this, we're gonna start talking. And that was it. He never said again. I was like you a little brat. So I think he knows how to talk. I think he just is like, What for? And I do think that maybe he's a little delayed from like, all the medical trauma that he's been through, you know, open heart surgery. And then he's had the two procedures last year, and then the procedure this year, and then the diabetes was kind of found in all that mix. You know, his poor little bodies been through a lot in order to survive.
Scott Benner 26:59
And so what Stephanie is alluding to, and it's not fair to her, because we're having two different conversations, one of them it's not recorded one that is but so Lincoln had to have out his tonsils and adenoids. Right, that one, and he had so many cavities, I guess that you he had to be pulled over for a dental thing, right?
Stephanie 27:22
Like, I don't know. I mean, I don't know if it is diabetes related because the dental stuff started before we knew he had diabetes. But he just was born with very little enamel. And so his teeth were just like deteriorating in his mouth. But then we were diagnosed with diabetes, and then the tonsil surgery, and then the diabetes, or the dental kind of got pushed back a couple months. And so by the time that we could get into the hospital and get clearance through endo and cardiology, he had four of his front teeth removed and eight root canals. Yeah, and then we just had another person. Yeah, and he just had another dental procedure two weeks ago. And it's always an ordeal like we're always admitted in the hospital that night before to check a monitor blood sugar. And then, you know, they take him back and put them under anesthesia and do like a deep cleaning. And they did two more work now.
Scott Benner 28:20
So she's Yeah, he has been through a lot. Honestly, he needs spider man.
Stephanie 28:26
Yeah, he needs a spider man and his wife.
Scott Benner 28:30
Well, okay, so I'm gonna try to like revisit this a little for you because Stephanie did something that I think is pretty great. So she found out that that her son needed open heart surgery prior to his type one diabetes. She looked around locally did not find a doctor that she thought was was, you know, the right person to do the job. And tell tell them how you contacted a doctor all the way in Boston and you're way out on the west coast. I like this idea. I want to make sure that I don't forget to mention the ease of use of Omni pod every once in a while and and today's gonna be that day. This past weekend, my family went to visit our son at college. So you know, we stayed in a hotel and you know, everything was a little kind of packed in and rushed around every once in a while you were going from here to there and working out of bags and stuff. So one morning we got up and I said to Arden I said hey, you see there's only like 30 units of insulin left in your pump. We're gonna have to change at some point this morning. But we were going to visit my son was doing some sort of a run or something and we were going to see that first. We thought the pump was gonna make it the answer was gonna make it to lunch, except that my son's event kind of got stretched out which led us to a snack and then all the sudden the pump needs to be changed. Arden changed her insulin pump standing at the back of like the tailgate of my car. And it may be took two minutes. I think that was it. A little cooler with some insulin it took the insulin out filled up the pump prime the pump, suck the pump on, push the button, injected the canula and finished cleaned up. That was it. We literally did it in a parking lot with people streaming by I don't think anyone noticed. That's how quick and seamless the process is. If you want to find out more about the on the pod, you should go to Miami pod.com Ford slash juicebox. And at that link, you can ask on the pod to send you a free no obligation pod experience kit, where you can actually try the pod on for yourself. Now you don't have to try it on standing behind your car in a parking lot. You could probably do that your house. But if you wanted to, you could. And I don't think anyone would notice my omnipod.com forward slash juice box.
Stephanie 30:45
After we were told that link, you know, it's time for Lincoln to start preparing for open heart surgery. We were given two referrals locally. And you know, good old Google. I did a lot of research on the doctors here and just decided, you know, that wasn't the road that we wanted to go. So we picked out three hospitals it was going to be la Philadelphia, and Boston and Boston being number one because there's number one pediatric cardiology Hospital in the world. And so I got just enough digging, and I did some background search and found this thoracic surgeons email and I emailed them and said, Hey, this is my son. He needs surgery. These are the things he needs fixed and repaired. Can we schedule surgery with you? And within like a week, he responded back and he's like, yeah, I have July 13. Open. And I was like booked. And we just hopped on a plane. And we were in Boston for nine days while he was recovering from
Scott Benner 31:48
like Expedia for open heart surgery just now. Yeah, click on this link here. And they'll get back to me with their offer. And then we'll go forward. That was there really is great. It Yeah, it
Stephanie 31:58
was it was. I mean, it was a blessing, because the surgeon actually only had to do a partial open heart surgery. So he didn't have to open his whole sternum. And he was only in surgery for like three and a half hours. And when he came out, he recovered. And I mean, he was only in ICU for like 24 hours. So and then we just went down to the recovery forum hosted ago.
Scott Benner 32:25
How long ago was that surgery?
Unknown Speaker 32:27
July 2016?
Scott Benner 32:29
It's the follow up like for something like that? Do you still have to follow ups? Or is he finished?
Stephanie 32:33
We do know. So what they did, Lincoln had three holes in his heart, one of them being very large VSD. They repaired those, but the biggest concern was he had it's called a muscle bundle. So basically, like it's all these like fiber endings that kind of make like a web inside your heart or consider like a cyst. And it was blocking one of his valves. So they had to go in and cut into the heart, muscle and tissue and remove that cyst and digital app. So the biggest fear was damaging, like the electronic operating system of the heart. And so if they did, you know, dug too deep or missed a spot, I mean, he would have needed a pacemaker. So that was kind of my fear of finding the best of the best that I could find to remove that. But it can always grow back. It could grow back. Yeah, so we get an echocardiogram done, like between 10 months and a year. Now, we just go back to the cardiologist and make sure that, you know, the holes are staying closed, and there's no tissue damage there and that the bundle isn't growing back.
Scott Benner 33:44
Wow, that's a that's a lot to go through. And then how long after the surgery, did the diabetes pop up?
Stephanie 33:52
Um, so we celebrated a year, you know, celebration with Lincoln surviving the open heart surgery. And then kind of immediately after that, he started just getting like not acting himself and kind of being sick. And so that was like, I'd say, July, August. And then in October is when I think the DK said and he was really sick. And so, the week of diagnosis, I actually had taken him to five different doctors, and just pretty much begging them to look at my son. I took them to the cardiologist, I took them to the EMT, my pediatrician even took him to like quick care. took him to one other doctor. I couldn't I can't think of who it was, but I was like something is wrong with my son. He's vomiting. He smells funny. I'm like smell I would put his face in their nose and I'm like, smell him. He smells funny. He had this really bad yeast infection which we had never experienced before with him. And just all the telltale signs like and nobody caught it.
Scott Benner 34:58
Yeah, but but now You didn't know what those signs were you just know. really sick. This is obvious somebody told me What's wrong?
Stephanie 35:06
Yeah, I thought I really thought because he was scheduled to have the tonsils and adenoids removed that it was just a really bad like strep infection or some type of infection with the tonsils and adenoids because they were so big. And he kept having the chronic ear infections. And, but then I started getting scared. That was that infection affecting the heart. And so that's why I took them to the cardiologist. And they did like, you know, their little scan and they're like, No, he's fine. There's nothing wrong with the heart. And so actually, Thursday night, I was sitting on the couch with them after he just threw up all over the house. And I got, I got him a smoothie, which was probably full of sugar. But because his tonsils were so bad, he was choking on everything. So I thought, well, at least if we get you a smoothie, you'll get hydrated and get some calories in you because he had lost so much weight. And I was just sitting there and I had this like, inner voice. Tell me, Stephanie, this is bad, and your son is going to die if you don't get him help. And I kind of like brushed it off. And then the next morning I woke up and he was panting, his breathing so heavily. He couldn't he stood up and fell down. And I was like, Oh, no. So I immediately like just threw him in the car. And as I'm driving to the hospital like that, just sheer panic is coming over me again, because I'm like, Oh, please don't be the heart Even though we just went to the cardiologist. And how am I going to get him to Boston for the surgery, and I get we, once we get to the hospital, we're automatically like, put in a room because of his history. And the PA Watson and I told her like, I need you to listen to me. My son is going to die if you do not help me. Something is wrong with him. He smells funny. So I go through all these symptoms, and it's vomiting but no fever. And you know, he's been on antibiotic and nothing's helping. And she's like, Okay, well, let's run some blood tests. And we'll see what that says. So the first panel came back. And at this point, we had been there for five hours, and he had been fasting. And she's like, well, that panel came back fine. And, you know, there's really nothing so it's just he probably just needs that surgery to have his tonsils removed. And I was like, No, like, You're not listening. Get another physician in here. I'm not leaving something is wrong. And she's like, Okay, well, let's wait for the second panel to come back. in about five minutes later. There were people just like wide eyed buzzing around the room. And they're like, we're gonna do some more tests that didn't come back. Right. And I'm like, and I keep asking like, what do you mean didn't come back? Right. What What's going on? And, you know, your immediate immediately thinking horrible things. I'm thinking cancer, I'm thinking like, some infectious disease, like I never once did, I think diabetes until they checked his blood sugar. And it said, 310 and I kept looking at them like, what does this mean? Like, what is a normal blood sugar? What are you looking for? And, and then like a whole team of like, official, like big time doctors came in, and they're like, your son is a type one diabetic. And we're emitting into ICU right now, because he's NBK.
Scott Benner 38:06
That's it, you got a double extra stress, he died.
Stephanie 38:13
I will never forget that moment. Like, I was hyperventilating. My husband had just gotten off work. So he met me there. I gave Lincoln to my husband. And I was like, I'll be right back. And I walked out in the parking lot. And I vomited. And I just like fell to the ground, because there's just like, we just like survived open heart surgery. And like, we just did all this stuff. And now this like, it was so like, it knocked me to my knees, because there's a cow, we gonna deal with this. And that was Friday. And on Tuesday, my son was diagnosed with autism. So in one week, like our whole world, just like crashed, even even going back, it's still super emotional, because, like, we're just spinning out of control.
Scott Benner 39:01
Everything else going wrong at the same and at the same time. So you're telling me that a year after heart surgery on a Friday, you find out first of all, you you go, you're you're running the doctors, begging them to help nobody's helping you finally say to yourself, alright, I'm going to go to the hospital, the hospital, the hospital tells, you know, the whole time you're there, you're thinking, this is something to do with his heart. This is really bad. You know, it's taking you back to the other spot. They tell you nothing's wrong, you persist. They come back, they say diabetes. And then and then 1234 days later, your other son's diagnosed as having autism.
Stephanie 39:38
So my son was diagnosed autism four days prior prior.
Unknown Speaker 39:42
Oh my god. Hmm.
Stephanie 39:43
So on a Tuesday, my son was diagnosed with autism. And we kind of already knew like, it wasn't a secret but just to have that like it verbally said to you, your son has autism and has ADHD like he has like a bunch of diagnosis. And so that's our own They're sudden, and then on Friday, you know, meanwhile we're dealing with the autism. You know, Lincoln is like dying. Like there's he's just deteriorating minute by minute. And so find him in the, in the Children's Hospital and they say that to us. So yeah, it was. It was a rough. I think I walked around in like a cloud for a good month or two because I just didn't know how to how to handle life grieve and process all this stuff going on.
Scott Benner 40:30
Well, I think it's even more impressive that you figured out the diabetes on the heels of the autism because you could have easily said to yourself, I you know, I there's no more here like, I can't keep looking for problems in my life. I have enough and and, you know, but I guess he just was so bad off at one point, you're like, like, I don't care what anybody is saying. He's obviously dying. Yeah.
Stephanie 40:51
Yeah, no, I knew he was in a bad play. I mean, just looking at him. You know, like the panting and he couldn't hold himself up and like, everything if he bone was like, protruding out of his body. And, and I mean, it was very obvious that he was gonna die.
Scott Benner 41:08
Remember Arden, like those in the hours prior? I remember Arden, prior to diagnosis. I remember her like when she was walking like that feeling like she was dragging herself. Like there was just a forcefield in front of her like, she could barely get herself to move forward. And then she'd stopped frequently while she was walking like this was just too much for now. Yeah, it's really terrible. But you are, I don't want to say but because it's, that's not something you just give away. I don't think emotionally and move forward. But are you having any luck kind of moving past that part? And?
Stephanie 41:41
Oh, yeah, I mean, every time it you know, I think that definitely is, you know, ulimate that I don't think I could ever, like get over like being a parent. Like, there's a couple moments in life that you just look back on that just, you know, knock you to your knees again. But we're good. Like we've traveled Lincoln's been to Mexico, we go to California, I have taken him on a couple trips. We've definitely mushed forward.
Scott Benner 42:08
Please don't forget to visit dancing for diabetes.com. And check them out on Facebook and Instagram. That's dancing, the number four diabetes.com.
Stephanie 42:22
I kind of hit that rut. Nothing was really happening. And I was just really struggling in the summer because I couldn't figure out how to manage diabetes with our hot summers and putting him in the car when it's 110. outside his blood sugar would tremendously drop. I couldn't figure out the pools. And I was just like, so bummed. I'm like, Okay, this is not as easy as I thought it was going to be. And so I just kind of hibernated in the house. And then I took a weekend to go hang out with my best friend in San Diego. And as I was driving there, I was like, I'm going to listen to a podcast, and then that's when I pulled up your podcast, and it just kind of re charged me laughter I listened to one episode, it's like, oh, my gosh, I got to go home, I could fix this. I know how to do this now. And so thank you. Yeah, it really, it just kind of feels the fire, right? Like, I just needed that community of friends. And and even though you're, the people that you put on, aren't my friends, but it really feels like I have a team supporting me and people's ideas to bounce off.
Scott Benner 43:26
That is very nice to view to say, I appreciate it. A lot of people think their stories aren't valuable. But I'm like, eventually your story will be part of the fabric of why people listen to the podcast, and they will get something from it, you know, and there's no way to you you kind of don't get to decide what your story is to somebody else. And you just putting it out there is the best way to go. I'm I'm thrilled that you found it. And then it's been it's been this valuable for you.
Stephanie 43:51
Yeah, like, I feel like, you know, we were through because he had those two procedures really early on in the year last year, right after being diagnosed. And so every procedure changed, his insulin needs drastically. And so it would take like, I don't know, three weeks to figure it out. And then we get in a good spot. And then he would see the procedure done again. And so then or he gets sick or, you know, something like that. And so it took me a while. And so when I found your podcast, I think is a one fee was like 9.8, which was a lot of work on a little kid that doesn't talk with all of this stuff going on. And and we just had an endo appointment in February and you 7.5 so I'm pretty proud of it. It has been. Yeah, it's been a lot of hard work. And he just had his procedure in February too. So I mean, I want to get them lower, but I think it's hard with a three year old who doesn't talk and you give them food and he falls asleep. So first,
Scott Benner 44:50
let's say first of all, two things. That's a great number. You know, for anybody, not just for your son who you know is young and doesn't talk and you know, the That's just that's a fantastic accomplishment. So, you know, having a goal of being lower, is really going to be about you making like fine tuning adjustments about him growing and getting bigger, you know, being more communicative, like all the things that it's going to take, you know, to start, like cranking that number down. But you're, you shouldn't feel like, you shouldn't feel like, wow, I need to get lower you should, you know, I think that I guess the way to put it as is that people always say like, I want to lower my eight, one, C, and I think no, you don't really you do, but you don't. That shouldn't be your goal, your goal should be to make small changes that keep your blood sugar from spiking, and from falling lows, that you don't have to re add food. Like when you do that, you get better and better at it as time goes on. And your agency as a consequence of that comes down. Like I always tell people, I never think about rnc one say, No, no, no,
Stephanie 45:55
I yeah, and I understand that part of it. But it's just kind of like, validation that all your hard work is like it's actually showing and it's bettering his health, like,
Scott Benner 46:05
I feel good, when we get the number, don't get me wrong. But in the day to day, management of Arden's like blood sugar, I don't think like I have to do this or hurry once he's gonna, like be something I just think of, you know, each, you know, a spike by spike below, just over that blood sugar is trying to go up. Now I'm gonna take care of that, you know, we're, like, we talked about at the beginning about doing a pod change over top of a carb heavy thing today, and now aren't eating and I'm still being aggressive, and we're holding their blood sugar at bay, it's at 180 now, but now she has a full meal in her room, you know, I'm not gonna, I'm gonna do my best to not let it go higher this week, we just added more insulin a moment ago, you didn't hear it happen, but we're gonna keep pushing until we can get it back. Get our level again. And I'll never think about this moment ever again, you know, like, it's gonna keep going forward. And if you keep making those addresses, that's how you get to where you want to be. You know, I know there are always people who listen and hear art and say, one see is lower, and think that our blood sugar must be constantly, you know, like, 85 or 90, and it's just isn't the case. It's 180. Right now, it's something, you know, timing of something just didn't go well, for us today. We're gonna get it out as fast as we can. That's it
Stephanie 47:19
right? And and I always feel like people always want to know, like, what's his number? And I'm like, well, it's number one, I could tell you, but in a few minutes, it's going to change because we're going to go outside or he's going to eat and like, it's never about just what it is. At that moment. It's looking forward and making sure that in an hour, we're still going to be able to keep it balanced, or, you know, make minor adjustments, because it's not always the number that I'm concerned about. It's the direction of the arrows to that I really, I really follow.
Scott Benner 47:49
Absolutely. There's a Yeah, I mean, it's it's the speed and direction of your blood sugar. And how are you keeping it where you want it to be?
Stephanie 47:57
Yeah, and I think every, like, person's needs are different. Like, we just had an endo appointment, which I mean, I don't really understand, though, I heard you saying you don't know what the whole point of them is. And I kind of feel that way now right now. Like we go and he's like, you do this really hard. What you do is a lot more work. And I and I was kind of taken back because it's like, well, how else would you do it because if I only bolus Tim every three hours, like he would be all over the charts, but because I give him those micro boluses. So for him, you know, anywhere from point 10 to point five, you know, just these little bits, every you know, throughout the hour, like I'll do it two or three times as he's eating or as he's playing, you know, on the needs of adrenalin or the hormones or, and I'm like, but how else would you do it and I'm fortunate enough that I I work evenings so when I go to work my husband you know takes over so we don't really have a lot of caregivers and my father in law does it and we do have some babysitters that help and I don't allow them to give insulin but I always set him up kind of for success when he's not when I'm not with him and he's alone with someone I mainly just at that point, you know, have them treat as needed with lows.
Scott Benner 49:15
Can you believe how much help the Dexcom g sixes in Stephanie's life? between being the three year old and preschool and surgery and everything else that happened? Just amazing. You heard her say earlier. Most people's blood sugar's probably jump up the 300 and no one ever knows. How long do they stay there hours till somebody checks again. But you don't have to live like that with the Dexcom. The Dexcom g six continuous glucose monitor can tell you instantly that your blood sugar is not reacting the way you would hope
Unknown Speaker 49:47
or
Scott Benner 49:48
it can tell you that it is reacting the way that you hoped and provide sort of a comfort and a calm and ease and an ability to forget about diabetes for a while. No matter where Dexcom is helping you in your life. It was We'll help you. Right now today. Arden has a cold, it's just a head cold. It's nothing crazy. But she's requiring more insulin. And we've been able to let Arden live her life normally today. And by that I mean food, lunch breakfast or inside pancakes today already. Today off from school, she's downstairs now working on a little lunch. And even though she needs a lot more insulin today than she normally would her blood sugar's 140, I'm looking at 146. And it's coming back down a little bit. But it hasn't gotten any higher than that. Now, if I would have just used the regular amount of insulin that we normally use in these scenarios, her blood sugar would be much higher. But Dexcom told me, Hey, this isn't working. And I was able to readdress, I implore you, check it out. dexcom.com forward slash juice box, look into the G six continuous glucose monitor. That'd be the best thing you ever did. If you can't remember the links, they're also at Juicebox podcast.com. I can't agree more. I mean, honestly, to call it harder, I think what they're trying to say what I think that they're saying harder and meaning you're involved more often. But being involved, being involved less often, to me is harder, because it's difficult for me for my kids blood sugar to be 300. And then they'd be 50. And then to be 300. Again, like that's hard.
Stephanie 51:23
You know, and that's what we were experiencing doing that every three hours, like, you know, he'd be 300. And then I give him a unit and then he would be 50. And then I'd be treating the 50. And then we'd be 400. And it just never was like even in even if it's even in 200 you're learning to coast. Right? So if he even is what we're aiming for not this spike all over the place. And that was that? are the keys never balanced. I don't even know what you're talking about. Like to me never in a good spot.
Scott Benner 51:53
Yeah, right. To me. It's much simpler, and less, you know, taxing on my time and my thought to see a 130 diagnostic. Oh, let me just bump that back again. Anyway, oh, and then it would be to just put in insulin, close my eyes. Hope for the best test again, three hours from now let's see that because it throws you into that power every time you're like, Oh, geez, I did what they told me to do. And now his blood sugar's 300. And what am I going to do, because he's 300. But he's gonna be hungry again soon. So and you get into that horrible just that rollercoaster ride, which really is no better way to say it like your high and your low and it's up and it's down your stomach and your throat and your heart and your stomach and you like it's it's always like that. Yeah, give me five minutes where I have to say, All right Bolus extra here. Let me pay attention to it for a couple minutes. See if it stops the way I expect it to. And if it doesn't, we'll put in a little more. That, to me is so much easier, and a better way to live a more delightful way to spend your day. Yeah, they
Stephanie 52:53
feel better. I don't feel I mean, I feel better when I know that he's in a steady range versus like, this spikes all over the place. I mean, I literally start like, if I'm not with him, I'm calling my husband, did you give him influence? Did you give him mental and give him this much give him this like, and I don't stop because it's just like, no, like, it's just not gonna, it's gonna crash as soon as the insulin catches up, because there's nothing really backing that rise at that point anymore.
Scott Benner 53:16
Exactly. You're missed. And trust me again, please, as he gets older, as you get, you know, more body weight, all the things that come with growing, this becomes less and less a part of your day, to the point to the point where it just doesn't, it just doesn't happen the way that you're describing anymore, you'll find a balance.
Stephanie 53:34
I can't wait. I'm like, come on second grade, because you said you started typing Ardo when she was in second grade, until I'm like, in second grade, I'm gonna start texting him and telling him because I don't know, at this point, like if I could ever really trust the nurse, because they're all going to want to do the three hours and I'm just like, no, that's not how we're going to do this. Like,
Scott Benner 53:54
and even that, even that aside, even if you found a fantastic nurse, there's still going to be in that situation where like, well, there's certain times I go to the nurse's office. Yeah, you know, and so whatever my blood sugar is, when I get there is what it is. I mean, like you're looking at what's happening with Arden's lunch today is a great example of how texting is helping, like we really are in the middle of the it's a quagmire, like it's just there's too much. It's just such a messed up situation. You know, she needs a new pump. So we put the pump on but it she's already eaten something with a lot of carbs. And now we've done a pump change on top of a large carb heavy thing in our system. And we're trying to get it going in the right direction. But it's just it's we're not winning the battle at the moment. And before I know what happens, lunch happens. And so, you know, I thought we were there. We were at 150. And I was like, Well, I'm getting it, it's moving in the right direction. But it turns out I wasn't and then lunch happens. But if I just if I go back three hours from now and do whatever we did, do how much more insulin we've used since then, like Arden's blood sugar would quite simply be 450 right now If I waited three hours for her to go back to the nurse, and instead we're just in a sucky 190 blood sugar that's gonna take a little time to get down to huge difference being just having that communication.
Stephanie 55:12
Yeah. And so I'm going back to when Lincoln had his dental procedure. A couple weeks ago, there was the following endocrinologist that came in, and she was like, go, we're going over the protocol and, and it's a big battle every time I go to the hospital because they want to administrate insulin, I'm like, No, he has a pump on I monitor his insulin. Basically, you're here just to hook up the IV. That's why we're here. And they're like, Oh, we've never had a patient do this. They always are astounded by his technology like the Dexcom. And the Omni pod, which I'm just like, This isn't like new technology, I don't understand what Yeah. And they're like, we've never seen someone with all this technology on we don't know how to handle this, or the protocol. And procedures aren't up to date or current with technology, which I find very, very frustrating every time we go. And so the doctor came in, she's like, so if his blood sugar hits 300, we will take his insulin pump off and give him a shot of insulin. And I was like, why would you take his pump off? Right? It's probably going to go that high because of the anesthesia. And if it does, I will just pull this in with the pumps, and then we'll wait and it'll come back down. And she's like, so are you refusing medical care? No, I'm refusing you to take my son's pump off and give him a shot of insulin. Well, the pump could be the pump could be key, she told me and like, but the pumps working right now. And if the pump is king, so just take the pump off and put a new pump on. No, you're not you're not taking its pump off chill. She got really frustrated me. And she's like, so you're refusing medical care, as I guess that's what you want to call it. I'm refusing for you to take his pump off. There's no reason for his pump to come on.
Scott Benner 56:51
Feel free to call it whatever you want. And, hey, I'm refusing to accept your under your misunderstanding of why my kids blood sugar might go up. Isn't that amazing? Like if the blood sugar goes up? She left right to a mechanical failure of the pump is the answer. Not Yes. All the bazillion things that could happen to push his blood sugar?
Stephanie 57:09
Yeah, like he's going to surgery with dextrose running through his system. So yeah. And they they always like decrease when he goes in for procedure decrease insulin, or they shut it off. Because they don't want to do anything while he's in there. So yeah, when when he actually came out of the procedure, he was like, at nine with an arrow angle down. So I was like, you need to get that extra. So on him now, like he's gonna drop really quickly. And so with that, running through a system, and we weren't really bolusing, we were just letting the bazel run in the background, because I don't know how dextrose is good. Like, I don't know how much the bolus for that. So he did hit 300. And I gave him you know, a small correction not a full one, because I wasn't, I don't know what, there's nothing in his system that's really causing this high. And it was just the anesthesia and the dextrose. And probably the you know, trauma that his mouth just went through. And she came back in, she's like, should we give him a shot? I'm like, No, he's gonna come back down. It's just takes, it takes time for influent to work, you should know this, like, and he had all that dextrose running through the system, like, he's okay. Like, and I don't want to force him to have to drink juice again, because he just had a procedure done, like in his mouth, let's just let it be. And he was fine. Like, he came back down and everything was good. But every time I take him to the hospital, I get this, like pushback about his technology and the dexcom and the insulin pump. And I feel like I'm you, you know, you have to really advocate and really not argue but you know, be smart about it and just say no, we're not doing that, or no why question. Why are you doing that one time I took him in? He was 75 because he was vomiting and he kept vomiting like four or five times a one day and 75 and it couldn't keep juice in the lady came running in to put on an IV fluid. And I was like, No, you can't give him that. He's like he 75 if you have sugar dextrose Yeah, you can put that but you can't put you know, sailing on him right now. She's like, he's high. I think though he's 75. Like if you if you give him that you're going to bottom out in 30 minutes flat.
Scott Benner 59:11
Wow. It's just it's mind boggling to think of all the different misunderstandings that you've like, witnessed. And these Yeah, these people have enough power over you to then say, well go ahead and tell me you're refusing medical care. So I can chart that you're refusing medical care.
Stephanie 59:26
Yeah. And like, and it's like, but you don't understand the technology. Like you're not understanding me and I all I'm like, I'm afraid that it's like if there's ever an emergency and my husband had to take him because my husband never really does. You know, he usually stays home with the other kids or he's working. I do all of the medical stuff. Or the doctor stuff. Something Yeah. And the advocating he just he just says yeah, whatever she said cuz she'll kill me and you so do what she
Scott Benner 59:57
like and you think he would just go with the medical People because he wouldn't have another basis for understanding he would think, well, I gotta go with him. I don't know.
Stephanie 1:00:06
I think he would who was like, Oh, they said, hook them up for an IV. So they know and he'd let them do it and, and where I'm like, no. And I think I told them four times, no, you're not giving him fluid until his blood sugar is over 100. Like, it's 75. And he's, he's three, like, he doesn't talk, getting him to eat and drink on demand is not possible. And he has been vomiting all day. So if you have that extra fluid running in the background, I know what's going to happen. So water is just going to, you know, drain them. So I think the biggest thing of dealing with a chronic illness is just knowing your child or yourself and knowing that advocating for yourself is not necessarily being wrong,
Scott Benner 1:00:51
right? No, you have to you absolutely have to stick up and, and speak up. I want to know where at the end of the hour and you've basically spoken for an hour and 45 minutes outside. I appreciate that. But I want to just check on you sort of at the end here a little bit. All right. How are you doing? Do you stop and think about yourself? Or are you just gonna see how long you can keep all these kids alive before you drop dead? What's your plan?
Stephanie 1:01:15
No, um, you know, I still work and, and I really love what I do in I think that is like, because I'm a hairdresser. I've been doing it for 1415 years. And, and I get to go and socialize with my friends, basically people that I've done for a long time. And, and I think that is I mean, it's my saving grace. It's my escape. And we do my husband and I do do like, we switch weekends. Like oh, this is your weekend to go do girl time. This is my weekend to go do a guy's night. So yeah, we do a lot of mental escape. Like even if it's going to the movies by yourself on a Saturday like we we do give that each other that breaks because it is it's, you know, meant mentally exhausting, and especially managing for kids and to have them special needs is it's a lot. It's a lot of battling. I feel like I'm always battling a doctor and battling the pool. Yeah. And I'm just like, when is it going to be easy, but you know, I feel I'm I feel like I've always kind of been a warrior in that sense of where I just don't do that. I don't go left. Because you say go left for you.
Scott Benner 1:02:27
I'm glad. Are you excited about you? Have you said you have Dexcom you have on the hunt? Are you excited about the idea of them working together and making?
Unknown Speaker 1:02:33
Oh,
Stephanie 1:02:34
I am. So I am so excited. So I do I did sign up for dash. So I'm waiting for that to come out. And we are just now upgrading to the G six transmitter. So I'm really excited for that. But yeah, I'm ready for horizon to come out. And you went to the Phoenix summit, right? The jdrf summit?
Scott Benner 1:02:54
I did. I went out and I spoke I spoke three times in six hours at the jdrf summit in Phoenix. I
Stephanie 1:03:00
know, did you I think I shook your hand when I first walked in. But I felt like I was stalking you. Because I went to all three of your How do I do that? Let's
Unknown Speaker 1:03:09
get really good.
Stephanie 1:03:12
Yeah, you know, I feel like for you, it must be really challenging because so many people want to ask you questions. Like there was one lady that just went on and on about here. She was just like, so frustrated, and you kept trying so many times to be like, maybe I can't help you with a cure. But I can help you with your blood sugar. Like, do you want to talk about your blood sugar, but but I can't help you with a cure? And I was like, Can you stop talking and taking up his time? Like we're not we're not gonna talk about QA today? Can we talk about like blood sugar and bazel the scenes about that this
Scott Benner 1:03:41
would probably not get me invited back. So we're in this I'm sitting on a panel. My first one was a panel, right? And we were there to answer questions. And so you know, somebody raises their hand. And if you go to enough events like that, you'll see that there are some people there, they just really want to be heard. And there's no like they're not following along with what the rooms therefore what the people are there for. They just they want to say what they want to say. So she wanted to start, you know, chirping about, I was promised a cure and it's not, you know, like that. And so she kept you know, you think at some point, okay, they're gonna get it and they're gonna stop and you're gonna move on and get to everybody else. But she wasn't giving up. So I don't know if you caught me. But I leaned over to the person who was next to me on the panel, and I whispered in their ear, and I said this, one of us is going to have to stop her. Is it going to be you? Because if it's not going to be you, I'll do it. Oh, and she's like, No, no, I said, Okay, I will and you just have to know how to so I kind of I hate to say it, but I just kind of spoke over a little bit and stopped her and then try another question to get it moving it but she did chew up it. That's the problem with those things is that the time is not enough. And so yeah, this was um, you know, this was a situation where you had an hour to ask for people questions, and it would have been nice to let all the people answered there as many as it could. Instead, she chewed up on of time, my problem then in the next settings, is it in 45 minutes or an hour? The stuff I'm really there to say in fairness takes an hour or so plus, then it invites questions afterwards. So I'm always talking incredibly fast. And and you know, sometimes the further you get away from the east coast, and you're speaking quickly, you go south, you go west, people are like, Hey, calm down, buddy. And I'm like, No, you don't understand. I got to get a lot out here in a short amount of time. But, but I am glad you so I'm glad you like that. I really am. And thank you for
Stephanie 1:05:33
Yeah, yeah, no, I I went last year. And last year, I felt it didn't really, I felt really bummed that I wasted my Saturday going because it didn't really apply to little kids. There was nothing geared to little kids or just how to treat you know, how to change or, you know, treat bagels. And this year, I felt like with you being there, and then Forgive me, but the guy that did the triathalon marathons. Yes. Yeah. Right. He was there. And that was exciting to hear his accomplishments. And so so I think this year, they did much better. And I was really happy that they had a lot of, like, pediatric endocrinologist there. Because last year, they did it. And I was just like, well, what's the point of me being here? Because none of it was like, send your kid off to college. How did you sports? Like, none of it apply to having a type one topic? Not one. One thing? Yeah. Sounds like what's the point of us being here?
Scott Benner 1:06:24
What we got a lot of great feedback. I know, I got good feedback on my stuff. And and the jdrf has gotten back to me and said, they've gotten good feedback about the stuff that I spoke about live is there. So I think they'll I think that, you know, hopefully, they and other, you know, chapters will think more about letting people leave with real actionable tools, you know, not just like, Oh, you know, we talked about encapsulation. Well, that's great, that's 15 years away, if they cure if they figured it out today, encapsulations, 15, or 17 years off, or something like that, which is fun to hear about for five minutes, but not for an hour. And, you know, like, people need something they can take home with them and put into play, you know, and so yeah, that was my pitch. When people asked me to come out, it's like, you know, but I tell them is I'm gonna, I'm gonna speak about stuff, and give people a real chance to make an impact in their health and their life and their happiness and everything and,
Stephanie 1:07:17
and not be so afraid. Yeah. I mean, the I mean, the doctors, I mean, this just may be like, like you say, like, the don't die advice, but they really like been bound up with that in itself. Like fearful when you get home, you're like, I don't want to be responsible for killing this little kid.
Scott Benner 1:07:34
But when you don't, but you still need to understand how to use the insult. You can't just throw your hands up and say, well, well, I guess whatever happens happens. And so yeah, that's that I had a great time. I told them immediately, I thought they ran an amazing event. I thought it was incredibly well. Set up and organized. And it ran great. I said, I'd be thrilled if you want me to ever come back. I'd love to come back again. I thought they I thought they did a really great job. I was also equally as impressed with Southwest Ohio man they have they really do something great out there. Yeah. So you know, I'm up for anything. If you're interested in having me speak, reach out.
Stephanie 1:08:10
I would love to No, it was it was awesome. And I really liked that you were there because it was a different spin on what was available, what was speaking and so to have, have you out there who's not a doctor, and you're not a diabetic, but you're a caregiver. And that's what a lot of those people are, we're all caregivers. And, and we're here and we don't know what to do, like the constantly like looking for the next best advice or next idea.
Scott Benner 1:08:36
It's great to hear from other people and see what they do too, and see if you can incorporate some of it into your plan. So
Stephanie 1:08:42
yeah, and the one thing I do want to say to parents out there that have not or that are non diabetic, where your son CGM, or your child's old CGM for a week to see how a non diabetic blood sugar works, because when I did that, it totally changed my perspective on diabetes.
Scott Benner 1:09:00
Because people's blood sugars do go up.
Stephanie 1:09:02
They do go up and they go really down and like it bounces around and I'm like, oh, okay, well, if I'm healthy, I don't have diabetes, or pre diabetic and mine is mine doing it. So I mean, I went to 150 eating yogurt. And so now I don't really eat yogurt anymore. Because like, obviously, that's hard for my body, but just to see how it changes and how I like if I can change and feel things like I went to like six. All night one time when I was sleeping. I was like, oh, and I'm fine. And I'm alive. And yeah, so he's 75 and he's low sleeping. He's okay. Like, it's I don't really need I can shut the bazel offer, you know a little bit and let him go back up. But I don't need to wake him up and correct it and make it go to 150.
Scott Benner 1:09:43
Yeah, knowing knowing what you're talking about goes a long way to doing something it really does and a great way to do it. I've heard a lot of people say that and I haven't had the opportunity to but I would certainly if I could get a hold of the technology. That was extra. I would love to see that. You know, so yeah.
Stephanie 1:10:00
He was getting ready to expire. And we had to do once a week left on it. And I just downloaded the Dexcom app on my phone. I was like, Okay, I'm gonna try it and see what happens. And I was such a little chicken when I had to insert it myself, but
Scott Benner 1:10:12
did it and put it on someone else, right?
Stephanie 1:10:15
Oh, I had to count. I was like, Okay. 123. Okay, we will do it at 10.
Unknown Speaker 1:10:22
But well, thank
Unknown Speaker 1:10:23
you, Stephanie.
Scott Benner 1:10:24
Thank you. I really appreciate you coming on.
Stephanie 1:10:26
Yeah, so thank you, and I can't wait to hear more. Take care. You too. Thanks. Bye.
Scott Benner 1:10:33
So Stephanie is obviously a fighter. There's a lot going on in their life. And there was a lot going on this day. I appreciate you guys listening. I try really hard for the sound to be great on the podcast, but I just didn't want to not give you this episode. I feel like what Stephanie went through today recording the show once and having to record it again. Now in our car, outside of our son's school, it's just to me, it showed a tenacity that I wanted you to see. So hopefully you could listen through the background noise and and see what I was trying to show you.
Thanks so much to Dexcom on the pod and dancing for diabetes for sponsoring the Juicebox Podcast. Thank you very much to you, the listeners and everyone who's supporting and sharing the show. Don't forget this Friday, another episode of Ask Scott and Jenny will be available. If you're not following the show on Facebook, check out app bold with insulin on Facebook and on Instagram at Juicebox Podcast. Facebook's really great. There's a really big contingent of you guys in a private Facebook group. So you join the ball with insulin group and then ask to be put into the private side of it. Where there are thousand people helping each other with questions day to day stuff about basal rates and stuff like that. It's very cool. Very communal. I like it.
Support the podcast, buy some swag!
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#265 Ask Scott and Jenny: Chapter Two
Answers to Your Diabetes Questions…
Ask Scott and Jenny, Answers to Your Diabetes Questions
Does bathing affect blood glucose levels?
How do you handle alcohol?
How do you crush a high?
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Pandora - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
This episode of The Juicebox Podcast is sponsored by in pen from companion medical. Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. And to Always consult a physician before making any changes to your healthcare plan, or becoming bold with insulin. MDI users, this one's for you. How would you like to live your life less complicated? You can do that within pen in pen is a reusable injector pen that has its own smartphone app. They talk to each other through the Bluetooth. that Bluetooth is magic, isn't it? You know what the app does? I'm going to tell you a lot of battle over the next few weeks on these Friday shows. But for right now, dose calculator dose reminders reporting actually tells you if the temperature of your insulin has gone out of range. Not only that, it connects to your CGM. Ooh, I got you there tonight, an app on your phone that connects to your continuous glucose monitor that connects to your insulin pen. Now you want to know more about indepen don't you? Check out companion medical.com Welcome to ask Scott and Jenny. In today's episode, I Scott and Jenny Jenny Smith from the diabetes Pro Tip series and defining diabetes. You know, Jenny, Jenny works at Integrated diabetes. She's a CDE, a registered pump trainer CGM trainer, dietician, she has type one. As a matter of fact, if it was the mid 70s, Jenny would be the Bionic Woman of diabetes care. She'd be Jamie summers. And for all of you who don't get that reference, I hate you for being young.
In today's episode of the show, Jenny and I are going to be taking questions from you the listeners. In this episode, we answer questions about bathing and whether or not that affects insulin drinking and how to handle it. And the third thing not lying to you, I cannot make out my handwriting. Oh, you'll have to figure that one out. I mean, it's only like 20 minutes long. You can do it. I wish I was kidding. That is what just happened. Right? You're ready.
EDAA EDA is editor right EDA at its at a let's call it says this is interesting because I think we kind of gone through this in our exercise episode recently. But she said okay, another doctor rule. When we got diagnosed, we were told not to take a shower and our past post insulin intake is I read this one is that is that true or false? My son's eight years old needs a shower every night. But sometimes we have to alter our night routine because he was given insulin. This is interesting because I think this is a great example of doctors trying to give you boilerplate answers to life's questions. And now doesn't consider that for the rest of time in memoriam Ed his kid is sitting around dirty not go into because he had a snack you know, I get the overall. So I've never really seen it Arden showers in her blood sugar doesn't get low is that because our Basal is right. And she doesn't have too much insulin in her body when she gets in the shower. What is that about it? Because I've seen it happen to where she jumped in the shower and her blood sugar falls?
Jennifer Smith, CDE 3:26
Yeah, it's it's really I mean, it has to do with the fact that in a shower unless you're literally taking like a Polar Bear Plunge which you're in the Midwest, you do in the middle of winter, right, that I guarantee is not going to cause your blood sugar to fall.
Scott Benner 3:42
You guys now have a great image of what Jenny looks like going from her shower to her towel to her bed.
Jennifer Smith, CDE 3:50
So, overall warmth to a site that's infusing insulin warmth creates, you know, it causes the blood vessels to move closer to the surface of the skin. And since that's where we're kind of infusing insulin, you get more vasculature, you get more circulation, I guess is the easier term so that your insulin actions speeds up. So you can get drops in blood sugar now, does it happen for everybody? No, it doesn't happen for everybody. The warmer the water, the longer the time that you spend in the water, etc. I know myself, you know, I mostly take showers now i with two little kids, they really don't have time to lounge in the bathtub for like three hours and read a book so
Scott Benner 4:39
Calgon commercials a lie, Jenny. It's a
Jennifer Smith, CDE 4:41
lie. It's totally a lie. Sometimes. In fact, I've said I need a Calgon moment my husband like sort of laugh in the background like I seriously
Scott Benner 4:50
fight. You know, now that he knows he could be replaced by dark chocolate peanut butter cups.
Jennifer Smith, CDE 4:57
Actually, yeah. Forgot I told you about
Scott Benner 4:59
that. Yeah, get in line and just laugh when Jamie says lamb.
Jennifer Smith, CDE 5:05
So yeah, you know, if I spend five minutes in the shower, I definitely don't see a change in my blood sugar now is my and I were Omni pod. So my pod is not like soaking in warm fits, you know I'm moving around in the shower, not just letting the shower water hit specifically that place. But for a kid who might be taking a bath, whether the if maybe the pump site is completely submerged in the water, if they're like my six and two year old who loves to like, play in the bathtub until it's literally like frigid, Ice Cube cold. And then they scream when they have to get out of, you know, if that's the case, it may be a reason that doctor is being I've never heard that a doctor actually even bring that up. So I think it's interesting that their doctor mentioned that
Scott Benner 5:51
at all a lot. I've seen this a lot. So,
Jennifer Smith, CDE 5:55
but really, yeah, I think it's interesting. But you know, it's, I think it's a preventative for hey, let's, let's not have you have low blood sugars just because you're taking a bath, but quite honestly, you know, if he's taking a bath, and you're doing an injection and his upper arm, technically, the bath unless he's laying down in it shouldn't cause a drop in blood sugar. Again, timeframe is also a difference there. I have noticed the difference. If I've been sitting in like a hot tub. I'm usually on vacation. If we do that I try to have my pat on the back of my arm so I can kind of hang my arm out of the hot tub and not like boil my insulin or anything. But even so just the warmth of sitting in that much, much warmer environment. I have definitely seen my blood sugar come down. So that's it's not odd. Your doctor was certainly not, you know, just blowing smoke. Yeah.
Scott Benner 6:52
For clarity to you're not saying that we don't want to heat the insulin up because it works better. When the insulins warm. You're saying that when your cells are warm, just like we talked about the exercise.
Jennifer Smith, CDE 7:01
So absorption is faster and Yeah, exactly.
Scott Benner 7:06
Okay. I like that one. This one's interesting, because I said to someone recently, I have to find a real like professional like drinker to come on the show and talk about how to Bolus for booze, right? Because I don't know but you live where it's called. You must have to get liquored up to get through the winter.
Jennifer Smith, CDE 7:27
So much. So people probably do.
Scott Benner 7:30
So Jim says what's general best practice considered for bolusing? For booze? I generally don't Bolus with my adult beverages. But what but I'd like your take on this. And then and then Emily came in and said, Yes, I gave up beer for more than a decade because it was so difficult to manage my blood sugar. Lately, I've been allowing myself one beer, but I tend to nurse it. So should I do a Bolus and extended Bolus or Temp Basal? So what are you? I am not a drinker at all, and I don't have diabetes. So I'm out on this one.
Jennifer Smith, CDE 7:59
Yeah, it's very, it's a good question. So in in general, have an alcoholic beverage that has carbohydrates in it, you will require insulin to cover the carbs in it. That's we're not talking about alcohol part of it yet just the carb part of it. So a beer. Most beers in fact, the lighter the beer, like the pale ales and those kinds, they tend to in 12 ounces have somewhere between like 15 and 20 grams per 12 rounds. The darker the beers like the stouts. And the Guinness kinds of things, they tend to actually have less carb, usually only about like 10 to 12 ish grams per 12 ounce. So there's a little card for you, beyond what you'd have to Bolus for. But if you are not a college, beer slam drinker in two seconds to see how long you know how quick you can actually get it down in competition with somebody else. If you're nursing it and it's a social drink. My assumption is that you're probably drinking a beer over let's say 30 Or maybe even 60 minutes. Let's It depends. She brings up a good point. Yes, extended Bolus is absolutely very beneficial there, especially if you're drinking the beverage on an empty stomach with no food with it was that mainly because food would help with the overall just it helps with the absorption that your body is also working on digesting the food and the beer or the alcoholic beverages sort of being absorbed and digested kind of along with the food. So you have less impact of like the alcohol component up front. So you have less tendency to have that drop first, even with a beverage that has carbs in it. But again, in a in a no food environment, just drinking a mug of beer. Essentially an extended Bolus would be a good idea, let's say over 30 minutes even over 60 minutes just depending the other types of alcohol let's say you're just doing something like gin or vodka, or something that really doesn't have a carb component to it. There's no reason to Bolus for it since there's not a carb piece to Bolus for. But does that mean that you shouldn't consider the impact of alcohol at all? No, in fact, conventional pumpers, the typical recommendation that we give is, when you've finished drinking, let's say you've consumed three beers or three, you know, drinks with vodka, that are carb free, or whatever it is, at the end of drinking, the goal is to take your Basal down a decrease of 40% for two hours per drink consumed. So at the end of the night, if you've consumed three alcoholic beverages, three times two hours would be six hours, you would decrease your overall Basal by 40% for six hours. And that helps to decrease the chance of lows, which are the end result of alcohol being processed in the body as a first response of the liver, the livers, that's one of the livers many, many, many, many, many jobs is to process the alcohol out because it's seen as kind of like a toxin, right? So in that same form, then the liver output of what your Basal insulin is supposed to be covering, if not outputting, that drip drip of glucose, that your body is supposed to be being covered by the Basal rate. So if you have lower output, you're not going to need quite as much of that Basal and the alcohol content to then cause low blood sugars.
Scott Benner 11:44
I had no idea. Yeah, and I here's one thing I do know that I can add, even though it wasn't asked, glucagon doesn't help you. When you've been drinking, is that right? Or is it not? It's,
Jennifer Smith, CDE 11:55
it's, it's not as effective, it can be less effective. Yes, because again, the liver is first word, especially if there's a fair amount of alcohol in the system, being one glass of wine. It's very wise if God would be fine, but you know, you've had several drinks and whatever, and you're kind of like tipsy and the glucagon would definitely have an impaired detail.
Scott Benner 12:18
And that's because your your liver is busy with other things, and it's depleted in the glucose. So if people understand or not, glucagon releases glucose from your liver, it's not a magic thing that brings your blood sugar up. It's not it's not Yeah, I don't know if everybody understands how it works. So if you're a power drinker, looking at your friends right before you pass out and saying hey, if I have a seizure, mix this up and stick it in my butt not going to be the only guy and I don't mean in the button
Jennifer Smith, CDE 12:45
all up right, right. It's better to call the better to call the EMTs and you know even in that case, you know, like you brought up earlier with the glucose you know, kind of in the cheek even at that point, something like honey or like a glucose gel if the person is actually carrying something along with them squeezing it in their cheek and actually getting it you just massage their cheek is gonna get absorbed and it'll help the blood sugar you know, faster so those are good options but yes, you know, overall, sure carb needs to be accommodated for in beverages especially if you're drinking the fancy you know, my ties and whatever they are Bahama sunflower, whatever Bahama breeze or whatever. Exactly. A there's a fair amount of carbon those.
Scott Benner 13:33
I think that's from Bahama breeze. I'm such I have probably not Jenny No kidding. I have probably not had the total of a case of beer in my entire life. I just does not occur to me to drink. I don't know why just it's never struck me. Let's talk about the in pen from companion medical, first of all companion medical comm. That's where you go to find out when you get there, there's a little blue thing up in the top right corner says get in pen. If you want to just jump right to the good part, you just click on that. First, I should tell you why you should be excited. If you're an MDI user. This thing is the bomb diggity, you understand. It's gonna help you track your insulin. You know, all that fancy stuff that people with insulin pumps get, you could get that with your pen. Not only that, it talks to your continuous glucose monitor if you have one, and if you don't have one. It's all right. The app still works great. The app, of course is for iPhone or Android. It is completely free. And available right now on the Google Play Store. And on the Apple App Store is it they don't call the App Store, right. They called the iOS App Store. They called the App Store. I think it was called the App Store. It's on the App Store. Let me tell you a little bit about what comes in this app. First of all temperature alerts. It can tell you right it's amazing temperature alerts limit the chance of extreme heat or cold impacting your insulin. And if it happens, the app will let you know Reporting is amazing. The summary of your therapy is spelled out right in front of you. You can share this with care providers or use it as a big picture look to help you make decisions. Do you have trouble remembering to dose your insulin in Penn provides you with an optional dose reminder. Right so you can decide to set up a dose reminder can also remind you to check your blood sugar in pen will not remind you to make dinner. The app has a dose calculator. Now listen, I know a lot of you who are on injections wish you had this because they're on pumps and they're really helpful in pen has it right on the app dose calculator to help you take the guesswork out of dosing. You enter your blood glucose and what you intend to eat. And the correct dose is recommended. It takes an account recent doses to avoid insulin stacking impact it's currently available in the US you can head over to companion medical calm right now to find out if your insurance covers the impact. But even before you get your answer, head to the app store and get the app the apps free. The pen, you know, depends on free, I'm not gonna lie to you. Insurance coverage varies by plan, please visit the get Impend link at companion medical calm to submit your information and find out with a no obligation verification of your insurance benefits if you're eligible for the in pen. Here's a funny one. Because Jenny and I know what we did last week. Jessica, who's another top fan? Jessica, thank you for being a top fan on Facebook says how do we concur? Or how do we handle a fat protein rise? When we know the blood sugar will rise again due to like Chinese food or mac and cheese steaks, burgers, etc? How do we learn how much to give at that second rise? And this one's an easy one for me to answer. I get to say, Go back a month to the pro tip episode about fat and protein. So you probably have heard of an easy answer. Just like yay, we finally got one. We don't have to do anything for Jenny and I just recorded an hour about fat and protein. So we're not going to rehash it here. But you can go find that episode. Jessica will absolutely answer your questions. Let's pull this one might be more like for me. Finally, ask Scott. Oh, yay. Actually, let me say this before I move on. One of the nicest replies in this one that made me feel really good about you know what the podcast does is Jessica said, goodness, you all do such a good job of answering questions that I didn't even realize I had. So oh really great. Like I was like that's that's wonderful. Yeah, that made me feel good. That is awesome. Yeah. So okay, here we go. Scrolling. Megan. Megan says, when you talk about crushing a Hi, can you please give an example in a little more detail. For example, if my eight year old daughter finishes eating 45 minutes ago, had finished eating 45 minutes ago, and she's 220 double arrows up. I either miscalculated the Pre-Bolus, the insulin or both? I love hearing people like they're mimicking the like the words in the pockets really makes me feel like we're getting through to people. How would you determine how much to give? This is Jenny's gonna laugh? Because my answers gonna be so just basic. And if and in how much time? If she's still going up? Would you? How would you When would you determine to give another Bolus, same amount this time, etc. So she's talking about like, how to stop this like a blood sugar flying up? My daughter's let's hear Scott's response. Responses just give her more insulin? How much more? I don't know. But more than you used the first time, that's for sure.
Okay, so this, to me is one of those trial and error things. It's where you have to use the information that you have from the past to make a decision today. And oftentimes, it's information you don't see as valuable. That's why I always tell people, anything that happens. Anything that happens with diabetes is never a mistake. I know things don't go the way you want all the time. But if you you can't step back and go, Oh, I screwed that up, or that really didn't work. You have to break it down and say, Okay, here's what I did. Here's where I put the insulin. And this is how much I did. This is what happened later. That's the information that will tell you next time when my blood sugar's to 22 up how much insulin will stop this. And you know, like and so there is a bit of that Megan, I think that you have to do it's sort of pre work for you know, really kind of breaking down what you've seen in the past now. I can tell you how I do it. But the numbers are there meaningless to other people, right? Like how much insulin I would give Arden to stop a 222 hour show up first of all, Meghan and I don't mean to brag but I don't see a lot of two arrows. But but that I mean might be what you really need to look into like how are you seeing two arrows like how far off were you in amount or timing it could have it should be to arrow should say to you significant miss? Like I really missed somewhere. You know what I mean? Now
Jennifer Smith, CDE 19:59
I can bring in what due to what does two arrows mean? We have a CGM. And you're seeing two arrows. What does that mean? That's a rate of change of at least three points. Plus, per minute. Yeah,
Scott Benner 20:09
it's flying. So
Jennifer Smith, CDE 20:10
it's a quick rise, just to define that.
Scott Benner 20:14
It's at least three. By the way, I know we've all done the thing. We're Dexcom says 215. And then five minutes later, it's like, 227. You're like, whoa,
Jennifer Smith, CDE 20:25
right. Right.
Scott Benner 20:28
Right. So Right. There's two thoughts in here. Megan, first of all, the one is sometimes you know, sometimes the arrows can, you know, throw you off a little bit and I like to look at the pitch of the line. I know that sounds may be strange to people but a a more gentle rising more of like a slope. I describe it as for people have seen the prices, right. It's the it's the, the unity, who the guy goes up the thing and like you're guessing things, and then you know, the fall is little pickup, right? And the whole time you're watching it, you're like, Oh, the little like, is it Switzerland? Is that what I'm thinking of? I almost said Swedish, but that's the Muppets. So it's Switzerland, and he's going up the Swiss Alps, they're in this real steady climb, and you spend the whole game thinking he's gonna stop, he's gonna stop and he never stops, he falls off the edge and you lose. That's what happens when you watch that line to me like that slow growing, but steady upward line that went to me says Pre-Bolus was probably pretty good. Not enough insulin, right? And so because if your Pre-Bolus wasn't really good, you'd be shooting straight up, like, like, and so to me that the line is, the answer is helpful. Yeah. Is it? Is it going up? Quickly, but still on more of a diagonal? Or is it like shooting straight up shooting straight up? You missed on everything? How much more do you put in the back? Like, I don't know how to answer that question. But I would I I've always said on the podcast I start with, when I need more insulin, back in the day, I would Bolus, like what what you would consider to be like life saving foods, like they were going to be eaten. So if I had a juice box that had 15 carbs in it, I'd say to myself, how much would I Bolus for this juice box? If I wanted her Arden to drink it as an enjoyable thing and not drink it as a way to stop a low blood sugar? Whatever that answer is for insulin. I know I can put at least that much in, right because I can cover it real quickly with a juice box. But you're looking at a 220. So in my mind, you're stopping the momentum, you're stopping you're covering a number, you have to account for the amount that's still going to rise before the insulin kicks in, like so you can kind of do that calculation through your head and go Alright, well listen, I think like say 220, a unit of insulin would bring it to 20 back to 90. So I go, Okay, I need a unit for the number. Now. I got to stop the arrows too, right? So I'll stop the arrows that probably going to take a unit. And she's gonna go another 50 points before this thing even slows down because I'm two hours up. That's how I sort of do the math, math math for me. Right. So Megan, I can't tell anybody how much that is? I can tell you the answers more. And I can tell you that you can do it in a way where your safety is how do I catch it on the way back down again. And I think that this is scary for people in the beginning, especially probably with kids or adults who are by themselves. But there's so much to figure out about this. And when you do figure out how to stop one of these things, the information you've learned that leads you to stopping this and bring it back level without a low. It will help you for years. And all other aspects of diabetes. Like when you really understand how to manipulate the insulin and smack that that high blood sugar down. It's It's It's the stuff you'll use forever. I think a gentleman might have a technical answer for this.
Jennifer Smith, CDE 23:58
Oh, well, let me and maybe a little bit more technical, because I you know, from what we all figure out by by experimenting on ourselves, we do. I mean, that's you've figured out many of the things that work for Arden, because of like you said, you do something you see the impact. And next time you're like, Oh, it worked but not quite enough or it worked way too heavy. So let's dial it back or let's dial it up. And while there's not really math there, there is an intuitive math that you're kind of using, right? If you really are trying to use a math to work this issue out. One she's right in considering Well, what was the problem to begin with? Okay, if you're getting a pretty quick rise up, as you said, it's probably the timing of the insulin in the Bolus. My my assessment would also be it's likely that the insulin to carb ratio is probably not quite right either. I mean, if it's still 45 minutes later When the insulin really should be getting active if there wasn't much of a Pre-Bolus To begin with, if it's still shooting up with a double arrow, there was missed insulin there as well. Right? How much one good and very, I guess, conservative way, if you wanted a conservative, you know, look of how to address how much is plugged into the pump. And see what is the pump recommending for this 220 blood sugar. Now, the pump doesn't know that there's a rise still happening, it just sees a solid, like written in rock number, right? And so you can utilize that and see, well, the pump is recommending you know, for a kid, it might be recommending something like point to your thinking will point to God, it's like a drop in the bucket, that's totally not going to touch a double arrow up with a 220 blood sugar. Okay, so intuitively, you know, something isn't quite right there with what the pump is recommending, nor does the pump know that it's still ascending. It's such a crazy climb. So there's where you can learn by saying, Okay, I know what the double arrows mean, the double arrows mean at least a climb of three, possibly more points per minute. So in the next 30 minutes, if you have a double arrow, and you do nothing about it right now, in the next 30 minutes, your blood sugar could be 90 points higher if you did nothing, right. So if you plug that number in as again, a way to use the math that's already programmed in with all of the ratios into your pump to 20 plus 90 Gets you What 310? Yeah, right, if you plug in a 310 blood sugar, and you ask the pump now to say, okay, what are you going to recommend for a Bolus? Now to correct this, you were going to get a more robust recommendation. Right. So that's a conservative way, it's not quite as bold as you would attack it with. But if you're trying to learn, it's a more conservative math way of figuring it out. And learning from it. Okay, you took the extra that the pump now recommended. And now I'm watching and the arrows have kind of angled and oh, it's now plateaued. But this is like that. It's another like 60 minutes that it took, because you took this conservative amount, right? So next time, be more bold, right?
Scott Benner 27:19
Because that can very easily lead to actual stacking. Yeah, so the difference between No, and let's add stacking to our defined diabetes list to that's a good idea.
Jennifer Smith, CDE 27:29
That's a good one.
Scott Benner 27:30
So I, I got some feedback about the podcast once where this gentleman said to me, we the day I said, it's not stacking, if you need it, he said changed his life. But it's not stalking if you need it. So but if you put in, in this scenario that we've built here, if you put in a half a unit, and then wait 20 minutes and put in another half, and then get frustrated, and wait a half an hour and put it in a unit, and now it's fit five, or you know, and next thing you know, you've put in three, four or five units over this hour and a half period, that is that you are going to get low later. But if you actually needed, say you actually needed three of those units. If you took it all up front, right, it wouldn't you wouldn't be stalking you. Because now because the impact of the insulin would be lined up with the with the carbs and what the carbs are doing right now. So the action of the carbs, the impact of the insulin are going to be lined up against each other, they'll get to that fight we talked about, then they'll all kind of dissipated the same time. But But thinking about the idea that insulin you use right now is for later, you keep adding later and later and later it keeps layering over top of itself. Eventually those layers are all going to be on top of themselves at the end of this timeline. And that's where you get low. So I like crashing up front because it also stops stacking it stops slows later. And if you are drifting low after crashing a high blood sugar, they are much easier to catch without loads or rebound highs if you haven't stacked Yeah, if you haven't checked if you stack Absolutely. Now you're stuck guessing how do I feed this insulin and not? Which one
Jennifer Smith, CDE 29:04
is actually which dose was actually causing the drop? So how much do I use to treat
Scott Benner 29:09
yourself a problem is what you've done. Yeah. A huge thank you to in pen for sponsoring this episode of The Juicebox Podcast. I hope you've enjoyed to ask Scott and Jenny as Jenny and I have enjoyed bringing it to you. Don't forget to find out more about in pen go to companion medical.com There are also links in your show notes and at Juicebox Podcast comm I'm going to take the rest of this time to remind you that I have a Facebook page. It's called bold with insulin. It's on you know Facebook, because that's where you keep the Facebook pages. Now there's a public page you can go to bold with insulin but once you're there is also a discussion group right? You got to kind of answer a couple quick questions that get in there so we know who's in there. And there you're going to find listeners from the show just like you talking about ideas about management supporting each other. It's very cool. You should check it out. I'm also on Instagram at Juicebox Podcast the Twitter if any of you are still doing that. Where else I don't know. Pinterest. I'm really I mean, I'm gonna be honest we I don't put anything on Pinterest last thing thanks so much for your wonderful ratings and reviews on Apple podcasts or wherever you listen means a lot I really do like them I say it means a lot a lot. A lot a lot. A lot. I say I say it a lot so I don't want you to think I don't mean it because I really do I say it a lot because I really mean it. I want you to know I also now wondering how many times I can say a lot before the music ends. Oh Joe, jeez, almost forgot. Check out Jenny at integrated diabetes.com Or there's a link in the show notes to her email address but integrated diabetes.com is where you can find Jenny Smith. Let her do the Voodoo that she do on you do a lot
About Jenny Smith
Jennifer holds a Bachelor’s Degree in Human Nutrition and Biology from the University of Wisconsin. She is a Registered (and Licensed) Dietitian, Certified Diabetes Educator, and Certified Trainer on most makes/models of insulin pumps and continuous glucose monitoring systems. You can reach Jenny at jennifer@integrateddiabetes.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!