Living Between the (Diabetes) Lines
Scott Benner
Three questions that every person living with diabetes asks themselves...
How high is too high? How low is too low? How do I find the balance between long-term complications and having a seizure.
Each of us has been given a range to aspire to. When Arden was first diagnosed, the doctor told us that we should be trying to keep her blood glucose value between 110 and 200 - "let's try to keep her A1C under 8.5", they said.
And so that became my goal.
Then one day they told us that we should lower the high range value to 190, at our next visit we agreed to try 185. The low range number was never touched. I understood what was happening even though it was never articulated to me, our BG goals were adjusting based on the vibe that our Endo got from us at each visit. She was evaluating our ability to handle spikes, lows, meals and overnights. I was being lovingly manipulated.
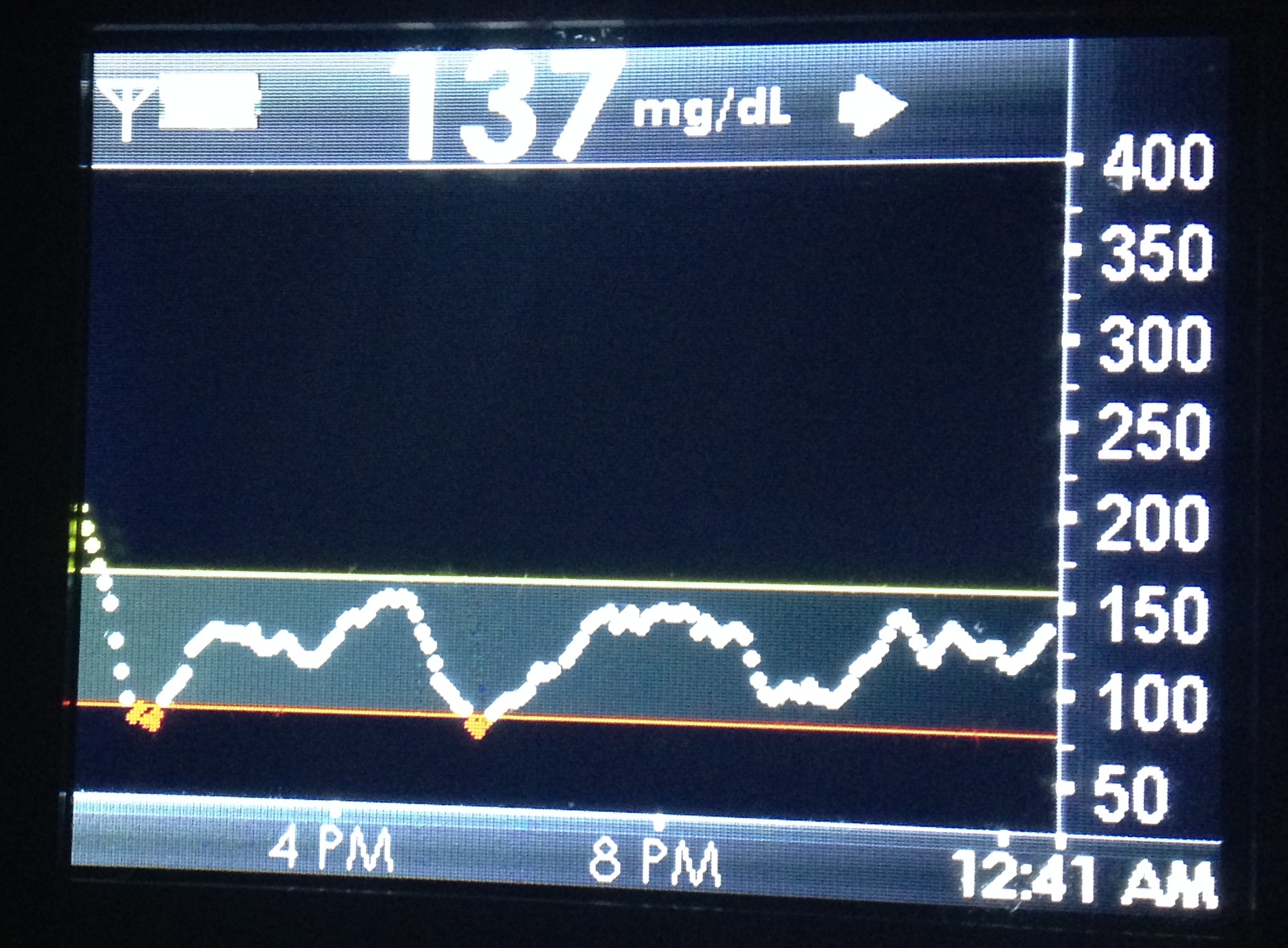
Then one day we discovered CGM technology and that little screen gave me something that I never had before, a visual representation of our goal. Now there was a line that I was trying not to cross. In the past when our goal was 190, 210 didn't seem like a huge miss and on the low end... even though we were trying for 120, 100 seemed so perfect that we didn't mind being a little low; besides many people, who don't have diabetes, regularly have a BG of 85 - of course they don't have man-made insulin in their system that doesn't know when to stop removing sugar from their blood.
I was living between the lines but I think the lines were holding me back...
I say holding me back because Arden's BGs were, for the most part, existing between them. I'm not talking about unforeseen spikes or unexpected lows. Highs and lows happen, you correct and move on, but you don't let them impact your impression of the graph. A few blips don't discount the rest of the day. Look at how the BGs are when you are blousing correctly, counting carbs accurately, when your basal rate is properly set. In those hours I was content if the graph line was mostly stable and in between 180 and 120.
It took me quite some time to figure this fact out, but the comfort that I felt when we achieved BGs that were between those lines, was holding me back from trying to do better. I had been lulled into a state of acceptance.
The lines were also providing a false sense of security. Even though they were arbitrarily set by a person that I only see four times a year, I was treating them like gospel. Finally I wondered, "if I can successfully keep a BG under 180 why could't I keep it under 170? Hell, why couldn't I shoot for 140?".
So I moved the line and do you know what happened?
I kept her BG under 160. Then I got brave and moved her low threshold to 100. Today, Arden's low alert sounds at 85 and her high is set at 160, but this summer I'm going to move that to 150.
All of this doesn't work if you punish yourself for going outside of the lines. I am telling you, do not do this if you can't handle seeing the graph climb above, or below those lines - don't add stress to your already stressful day. Before you attempt to move the lines you must find peace with being on the other side of them, you have to come to grips with the idea that nothing in life is controllable to that degree. Here's how I found my peace with that truth.
I was happy if Arden's BG was 180 all day because someone told me that number was okay. Her BG still spiked, it still got low but for most hours of each day her BG was 180. Today, most hours of the day come with a BG of around 140. She still has spikes and still gets low but most hours are spent in our new range. It took me a while, but now I can see, there is no difference in how I manage or what I do; the only thing that has changed is my expectations and the way that I react to them.
When I expected 180, I got 180. When I expect 140, I get 140. I'm learning to except 90... one day I'll learn to expect it.
When you're ready, move those lines... the ones on your CGM or in your log book, and the ones in your mind and heart. Expect what you want, except what you achieve and never stop moving the lines that life sets. Define your own reality.
Don't forget to read my disclaimer, I am not a medical professional and I am not dispensing advice... just telling stories on the Internets, the WWW, the information highway - you get what I'm saying. Please also don't forget that high and low ranges are never one-size-fits all. While Arden feels fine when her BG is 85, you or your child may not.