Having a Happy Thanksgiving with Insulin
Scott Benner
What do you think about when I say the words mashed potatoes, stuffing or pumpkin pie?
Most people hear those words and think "mmmmmm, it must be Thanksgiving" but some of us immediately begin to wonder how many carbohydrates are in stuffing. Many of the people who live with or care for someone who lives with diabetes, begin to panic. Instead of family and football they begin to think about Thanksgiving as a day that is trying to defeat them, they immediately feel stress and either decide to, sort of just give up and "do their best" or search for the measuring cups focused on getting the carb counts of every tasty Thanksgiving treat exactly right. In my opinion; there is a better response.
When I'm giving my daughter Arden insulin at a meal I focus on two things - How insulin works in her body and about how many carbs are in the food she is eating. In an effort to keep this, if you'll pardon the pun, digestible... I'm going to break this post into individual thoughts on subjects.
Questions I ask myself before I begin...
Is it more important to know A. exactly how many carbs are in a scoop of potatoes or B. how long it takes for insulin to begin to effect the blood sugar and how long it lasts in the body? - Answer is B
Will the day include a lot of grazing, am I planning for set meal times or is it both?
Do I have a reasonable understanding of the amount of carbs in the foods that will be consumed?
Am I afraid of insulin? - Be honest with yourself
My Goals...
My blood glucose goals for Arden are simple, yours should be too...
I am trying to maintain the steadiest blood sugars as I possible can. I want to avoid spikes and significant lows.
I consider a BG over 150 (after food) a high blood sugar.
I do not want Arden's BG to fall below 75 but steady at that number is a huge win, especially today.
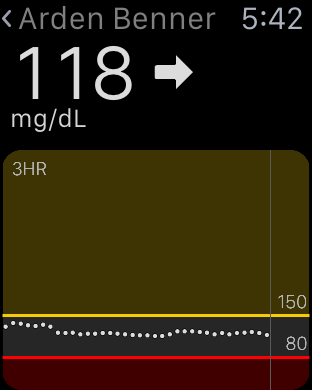
For CGM users: I don't want to see arrows pointing straight up or straight down. If I do, I've mistimed insulin, miscalculated carbs or (for pump users) would have benefited from extending my bolus. When we were non CGM users: If Arden's BG is above 150-160 forty-five minutes after your mealtime bolus, you probably didn't use enough insulin. More insulin, more testing.
I want to create a stress free, carefree and happy day without frying my brain.
Insulin...
I have two steadfast rules about managing my daughter's type 1 diabetes. Read them, memorize them, live by them.
1. It is far easier to stop a low or falling blood glucose then it is to return a high blood sugar to a safe range. In my experience most low or falling BGs can be stopped and steadied in a short amount of time, maybe 15 minutes. A high BG can take 3 to 5 hours to return to a safe place. I'll say it again. It is easier to stop a fall or a low then it is to effect a high. This thought guides everything I do with insulin.
2. If Arden's BG is high any time after a meal (140-150), I did not use enough insulin at the correct time. Two VERY important considerations in this sentence, they are AMOUNT of insulin and the TIMING of the bolus relating to when food consumption begins.
Before we move on I want to say this, these are my rules but you know as well as I do that diabetes will, on some random day, act in no way like you expect. That is a fact of living with manmade insulin. I refuse however to allow the fear of that random day to make me except high BGs on all of the other days. I would rather battle a low a few times a month then live with a daily average BG that is any higher than it needs to be. Bold with insulin!
Lets talk about giving insulin for a meal...
There are generally one of three situations I experience before a meal. 1. A higher BG then I want, 2. A lower BG then I want, 3. A BG in our comfort range. All of these may be steady, rising or falling.
Let’s have some examples:
Step one for each possible situation is to pre-plan. Don’t start thinking about insulin at 4:55 if dinner is at 5, if that’s what you are doing... I’m willing to bet you see a lot of high BGs after food.
If our dinner is at 5 pm, I want to find out what Arden's BG is at 4 pm.
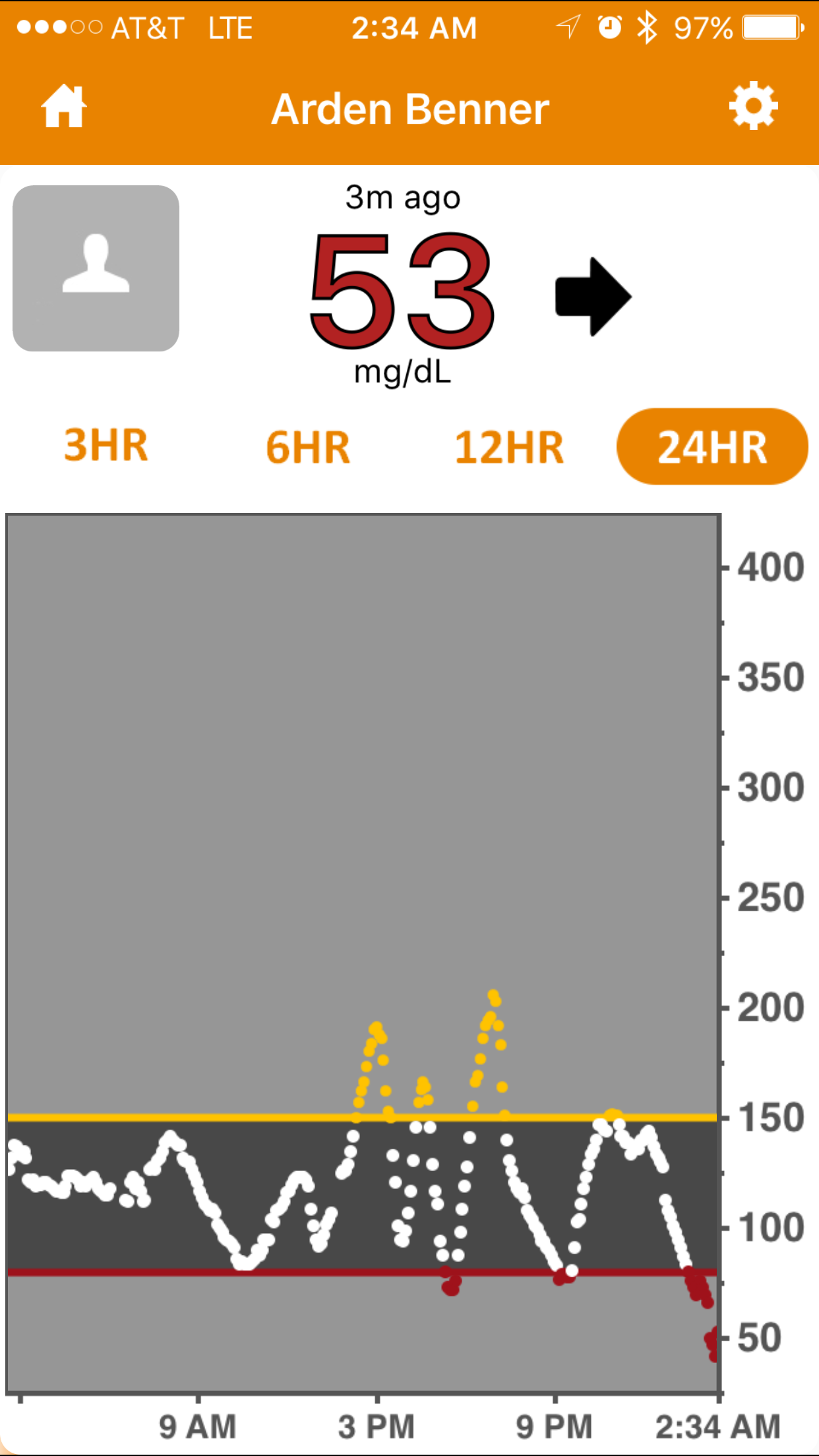
If Arden’s BG is 160 at 4 pm I would bolus for the 160 with the goal in mind of getting it as close to 90 as I could by 4:45 pm because (in this example) at 4:45 pm, I am bolusing for dinner. Here’s me counting carbs. Scoop of potatoes… eh 30. turkey 0, gravy, let’s call that 7, probably have two dinner rolls… I’ll call that 30, corn lets say 10, green veggies nothing. Okay that’s about 80, how much insulin is 80 carbs? Last thing I do is ask myself if the amount of insulin that 80 carbs indicates sounds like enough or too much? “Sounds like” means based on my past experiences with similar meals. If it doesn’t, I adjust it manually. One way or the other I’m hoping to have a 90 BG 15 minutes before the meal begins and I am bolusing with the thought that the mealtime insulin (In Arden) won’t begin to work for at least 15 minutes. The goal is for her BG to be 80ish when two things happen. 1. Her mealtime insulin begins to work and 2. The carbs from the food begin to have an effect on her BG. I want these things to happen at the same time when her BG is around 80. Then I watch the struggle between insulin and carbs play out on her Dexcom CGM. Most times this results in no spike and a steady BG for the next two hours. Adjustments (In Arden) may be needed around the two hour mark. More insulin, some carbs… one never quite knows.
A steady and in range BG gets the same pre bolus. Again, I want the struggle between the carbs and insulin (insulin pulling the BG down, carbs pulling it up) to happen as close to the 70-80 range as possible.
If Arden’s BG is low or falling an hour before dinner I only want to bump it ever so slightly. I don’t want it rising or high at 4:45. On the lower side is a great way to approach a meal - But you still have to pre bolus. I can’t say to myself, “her BG is 80 at 4:45 pm so I can’t pre bolus”. I have to trust the process, I have to trust that new insulin won’t cause a low for at least the amount of time that I believe it takes for the pre bolus insulin to begin working.
In the end, I can count the amount of times on one hand that a meal has gone well without a significant and well timed pre bolus. Only you know how long it takes for insulin to begin working in you or your child, so adjust accordingly with great deference to how long it takes the food to begin to effect the BG.
Remember, it is easier to effect a low than it is to correct a high....
I know there is a ton of other variables that I haven’t discussed. What if my child is too young to properly assume how much they will eat… in that situation I'd pre bolus half and then get the rest of the insulin in as soon as I could confirm that the food will be eaten. Easier with a pump sure, but even when you are injecting... it’s either two shots at dinner or one shot at dinner and another an hour later while you are battling a 300 BG. Which sounds better to you?
Arden has a CGM which makes all of this so much easier. I can see when she’s falling 5 minutes before we eat and hand her a roll. I can see the speed and direction that her BG is moving. No doubt what I am talking about is easier with a CGM but it is not impossible without one. Pre bolus (or inject), test 45 minutes later, test again 2 hours later. Stay on top of the BG.
Don’t fall prey to the drama! Don't ell yourself that, “I did what the endo told me” or “I counted the carbs, what else can I do”. That's all bull%$#&. You can do plenty with a positive attitude and a calm reaction to the things that don’t go as planned. Keep it easy in your mind; BG too high, need more insulin. Too low, need more carbs.
Is it a grazing day? Try using a temp basal rate. Perhaps an increase of (maybe) 30% to start, then adjust as needed. Don’t be afraid to let it run all day and don’t forget that the effects of a new basal rate may not be visible on a BG for 30 minutes to an hour. Also, when you stop a temp basal, it will take that much time to return to a level that you are accustom to.
I won’t let a BG that has gotten crazy high ruin Arden’s day... I crush it with insulin. Then test often or watch my CGM closely - sometimes both. If it falls too far or too fast, I catch the fall with a fast acting liquid carb. I give myself enough time to treat the fall without having to over treat - stay off the rollercoaster! Sometimes the hardest thing to do is to just wait and retest, I know, but that is how you will avoid chasing highs and lows all day. At some point you have to say to yourself, "we need to find a plateau and start over".
Last things and this is important. Lots of insulin is going to be used today. Watch your overnight BGs closely. Look for lows, unexpected falls and even high BGs from those carbs that just won’t digest and be gone. No telling which reality you’ll experience over night. Best to be on the look out. Give yourself a chance to battle on a level playing field, don't begin Thanksgiving with a pump site that is failing or on it's way out. Get your tech going and stable before the stuffing hits the table.
Wishing your family a very Happy Thanksgiving… don’t forget my disclaimer nothing you read here today is to be taken as advice, medical or otherwise. I’m just telling the story of how I manage my daughter’s BGs. Okay, thats enough diabetes talk for me today, I have to got make the stuffing!